Published online May 16, 2024. doi: 10.12998/wjcc.v12.i14.2389
Revised: February 13, 2024
Accepted: April 3, 2024
Published online: May 16, 2024
Processing time: 121 Days and 6.5 Hours
Morgagni hernia (MH) is a form of congenital diaphragmatic hernia (CDH) characterized by an incomplete formation of diaphragm, resulting in the protru
A 76-year-old female with no history of prior abdominal surgeries presented for an elective colonoscopy for polyp surveillance. During the procedure, when approaching the hepatic flexure, the scope could not be advanced further despite multiple attempts. The patient experienced mild abdominal discomfort, leading to the abortion of the procedure. While in the recovery area, she developed increa
A MH is a rare condition in adults that can present as a life-threatening compli
Core Tip: A Morgagni hernia (MH), a congenital gap in the diaphragm, may only become evident later in life. Initially small, this defect enlarges over time due to increased intra-abdominal pressure. Although it usually remains asymptomatic, a MH can lead to severe gastrointestinal or pulmonary complications. We describe the case of a previously asymptomatic 76-year-old woman who underwent a routine follow-up colonoscopy. Unexpectedly, the procedure led to a colonic perforation due to a previously undiagnosed large MH. This rare complication emphasizes the need for endoscopists to be vigilant in suspecting and diagnosing potential intra-procedural complications associated with this condition.
- Citation: Al Alawi S, Barkun AN, Najmeh S. Previously undiagnosed Morgagni hernia with bowel perforation detected during repeat screening colonoscopy: A case report. World J Clin Cases 2024; 12(14): 2389-2395
- URL: https://www.wjgnet.com/2307-8960/full/v12/i14/2389.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i14.2389
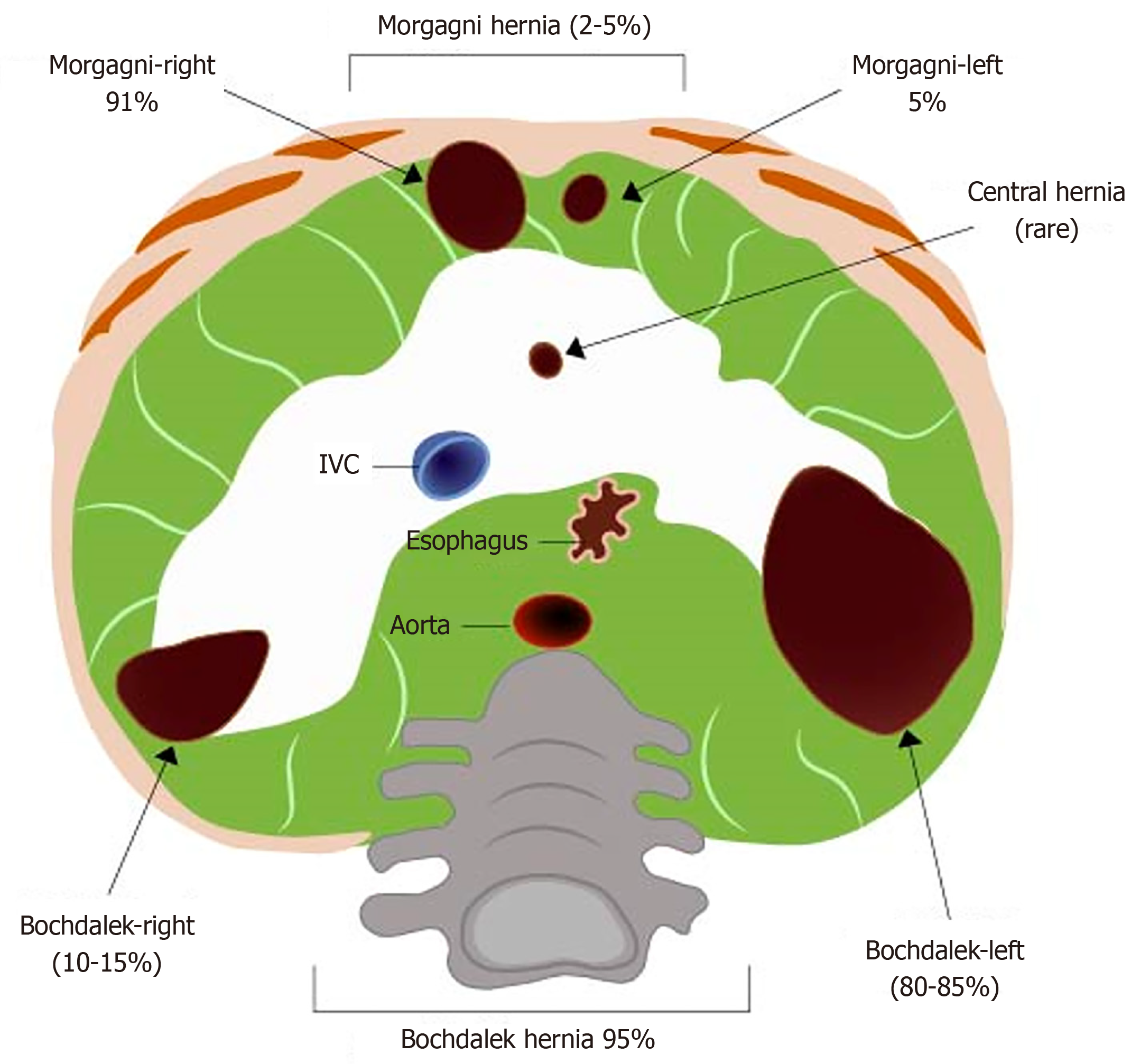
A Morgagni hernia (MH) is a diaphragmatic malformation of unknown etiology that typically manifests in the neonatal period[1]. It was first described in 1769 by the Italian anatomist Giovanni Morgagni[2]. MHs constitute a minority, approximately 2%-5%, of all congenital diaphragmatic hernias (CDHs) and typically present as either anterior-retrosternal or anterior-peristernal hernias[1-3] (Figure 1). The remaining cases of CDH include Bochdalek hernias, which are characterized by posterolateral diaphragmatic defects, with central defects being rare. These pathologies can be detected prenatally through fetal ultrasonography, which may reveal herniation of the bowel or liver into the thoracic cavity. This screening method has been found to accurately diagnose the condition in 50%-90% of cases[4]. When symptomatic, a MH commonly presents as acute neonatal respiratory distress or gastrointestinal pathology, usually due to obstruction and incarceration of herniated bowel loops. Pulmonary symptoms are likely attributable to intra-thoracic compression of the lungs by herniated abdominal viscera, resulting in disruptions in pulmonary blood flow during development[4]. Neonatal symptoms associated with congenital MHs include respiratory distress, inadequate oxyge
The patient presented for a routine follow-up colonoscopy. She was asymptomatic prior to the procedure, except for long-standing, very rare sporadic abdominal pain that did not interfere with her daily activities. There is limited literature on delayed presentation of MHs with bowel perforation during colonoscopy in asymptomatic adults. This case study highlights an uncommon manifestation of a MH in adults and the importance of being aware of this condition and maintaining a high level of clinical vigilance.
A 76-year-old woman reported experiencing increasing abdominal pain approximately 30 min after being transferred from the endoscopy room to the recovery area after a difficult aborted colonoscopy.
The patient was previously healthy with no significant comorbidities. She had been referred for an elective outpatient colonoscopy for post-polypectomy surveillance. The most recent colonoscopy, conducted 5 years prior, was normal and had not presented any technical difficulties. During the index colonoscopy, which was conducted with CO2 insufflation after conscious sedation with 50 μg of fentanyl and 1 mg of midazolam intravenously, the scope could no longer be advanced smoothly upon reaching the hepatic flexure (Figure 2) despite multiple trials and changes in position and technique. There was no abdominal wall or inguinal hernia noted on physical exam during the procedure. An internal hernia was suspected, but there was no history of previous surgery or trauma. During this part of the procedure, the patient experienced mild abdominal discomfort, but vitals remained stable. The procedure was aborted, and it was decided to observe the patient in the recovery area for an extended period of time to exclude a potential perforation. After 30 min in the recovery area, the patient developed increased abdominal pain, rated 8 out of 10 in severity, along with new dyspnea. The patient then mentioned for the first time that she had experienced recurrent pains of a similar nature, although not as severe, for several years; these episodes were infrequent, occurring once every 2–3 years.
The patient’s medical history included hypertension and a previous transient ischemic attack with no residual neurological deficits. She had undergone three previous colonoscopies. The first, in 1997, was normal. The second, in 2014, revealed a diminutive polyp in the sigmoid colon (tubular adenoma). The most recent colonoscopy, in 2017, showed no abnormalities. In 2002, she also had a sigmoidoscopy and barium enema, both of which were normal.
Family history was significant for colorectal cancer in her father at the age of 75.
During the episode of abdominal pain, the patient was fully alert and conscious, but appeared uncomfortable and anxious. She exhibited hypotension with a blood pressure of 72/53 mmHg and a heart rate of 68 beats/min. Her oxygen saturation remained above 95% on room air. Abdominal examination revealed no abdominal sounds, a rigid abdomen with diffuse tenderness and guarding, as well as rebound tenderness.
Acute blood tests showed a hemoglobin level of 134 g/L and a white blood count of 7.6 × 109/L. Other lab tests, including liver function, electrolytes, and renal function were all within normal ranges.
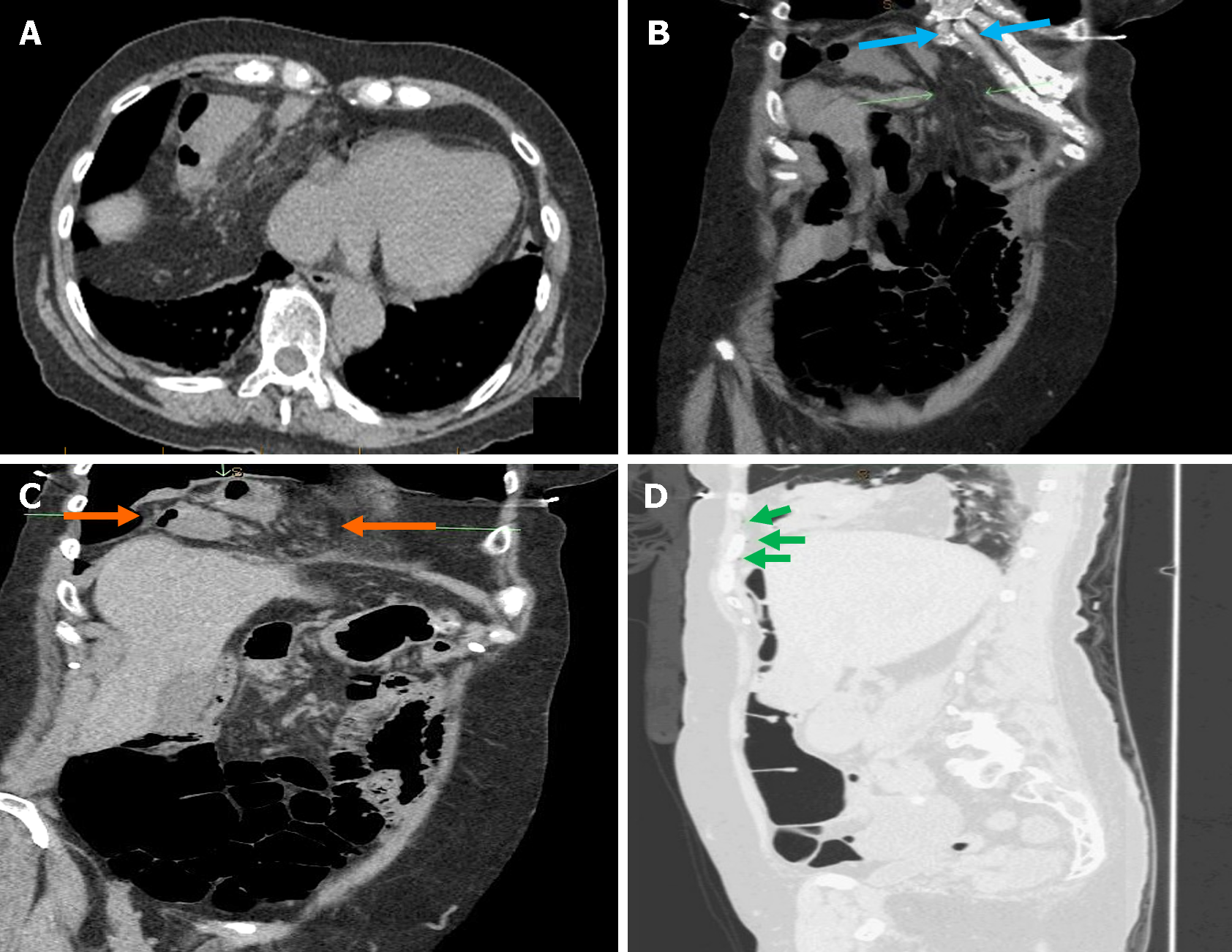
During the colonoscopy, the colonoscope was able to advance easily into the sigmoid colon but encountered limited progression into the transverse colon and hepatic flexure. The colon appeared tortuous with an intraluminal appearance resembling a volvulus. The procedure was terminated prematurely due to the inability to progress further. Upon scope withdrawal, submucosal hemorrhage and mucosal evidence of barotrauma were observed (Figure 2). A computed tomography (CT) abdomen revealed irregular wall thickening of the hepatic flexure and proximal transverse colon, which had herniated through a large diaphragmatic defect suspected to be a MH into the chest at the level of the right cardiophrenic angle. This herniation extended through the right major fissure to the superior segment of the right lower lobe. Surrounding fat stranding and a few extraluminal air locules were present, indicating a colonic perforation (Figure 3).
Colonic perforation after colonoscopy due to a large MH.
The patient was resuscitated with intravenous fluids, resulting in a rapid and appropriate hemodynamic response. The colorectal surgical team was urgently consulted. The patient was started on intravenous antibiotic therapy with cefazolin and metronidazole in preparation for urgent transfer to the operating room (OR). In the OR, a diagnostic laparoscopy revealed that a segment of the transverse colon was incarcerated into a retrosternal diaphragmatic hernia. There was no evidence of fecal peritonitis. Once the hernia was carefully reduced, a small antimesenteric perforation was observed on the serosa of the transverse colon with no significant signs of ischemia. A transverse segmental colectomy was performed with colo-colonic anastomosis. The diaphragm was inspected, confirming a small to moderate-sized MH in the retrosternal position lined by a large hernia sac, which was dissected and removed. Due to the presence of a colonic perforation and a secondary contaminated field, the hernia defect was closed primarily using interrupted non-absorbable sutures without the use of a mesh.
The patient progressed well postoperatively, tolerating clear liquids on postoperative day one, and was discharged home without any complications two days after the operation, resuming a regular diet. She had follow-up appointments two weeks and four weeks after the surgery, during which was doing very well. Pathology of the transverse colon revealed a small perforation with no signs of ischemia, serositis, polyps, or malignancy.
During the embryonic period and by the eighth week of gestation, the diaphragm undergoes complete development through the fusion of its components, including the septum transversum and the pleuroperitoneal membranes[6]. Failure of appropriate closure of the pleuroperitoneal folds between the fourth and tenth weeks postfertilization results in herniation of viscera into the thoracic cavity, causing disruption to normal development. The causes of unsuccessful diaphragmatic closure remain to be elucidated. One potential explanation is the disruption of normal mesenchymal cell differentiation during the morphogenesis of the diaphragm and other somatic structures by genetic or environmental triggers[7,8]. The occurrence of CDHs is primarily sporadic, with the majority of cases lacking an identifiable familial association.
The prenatal diagnosis of a MH can be conducted through detailed prenatal ultrasound or magnetic resonance imaging (MRI). In adulthood, the diagnosis may be made through various diagnostic imaging techniques such as chest X-rays, CT, MRI, or upper gastrointestinal and bowel double-contrast studies. Common imaging findings on a CT scan may include the presence of fat or soft tissue abutting the upper surface of the diaphragm, a distinctive posterolateral position on the hemidiaphragm with consistent density across the defect[4].
The majority of adult cases of MHs are asymptomatic due to the occlusion of the defect by the underlying liver or omentum, which effectively prevents herniation of intra-abdominal organs into the thoracic cavity[9,10]. Several studies have documented its manifestation in an adult population. In a recent review, 310 adult patients were identified with a MH, with 61% being female. The most commonly reported presentation included pulmonary and gastrointestinal tract symptoms. The majority of MHs were located on the right side (84.0%), as in the case of our patient, with the greater omentum and transverse colon being the most frequently herniated viscera[11]. Although there have been some cases of MHs presenting with bowel obstruction or perforation, to our knowledge, there has been only one other reported case of bowel perforation within a MH during colonoscopy[12]. Our patient reported experiencing rare, mild, and self-remitting episodes of abdominal and chest pain of unclear duration over years. These may have been the result of intermittent abdominal content herniation through a narrow hernia neck. The use of increased intra-abdominal pressure, colonic insufflation, and manipulation during colonoscopy may have paradoxically exacerbated the herniation and precipitated bowel perforation. Due to the widespread use of colonoscopy in the field of gastroenterology nowadays, the aim of publishing this case study is to raise awareness of MH when encountering unexpected difficulties during colonoscopies. After navigating the usual challenging sharp angles in the sigmoid colon and splenic flexure, observing a sudden volvulus-like appearance of the transverse colon lumen should prompt the endoscopist to consider a CDH. Presumably, any internal or congenital hernia could present in a similar fashion, and subsequent abrupt onset of abdominal symptoms or respiratory distress during or after the procedure should prompt further investigations. Examining the patient's prior chest or abdominal imaging for incidental findings of CDH and gathering a comprehensive surgical and traumatic history, particularly focusing on the thoracic region, may assist in proactively identifying the presence of a MH. This approach may heighten the suspicion of a diaphragmatic hernia, thus potentially allowing for preventive measures to be taken before the medical procedure, thereby minimizing potential complications.
MHs can be repaired through either transabdominal or transthoracic approaches using either open or minimally invasive techniques. There is a lack of consensus on the preferred approach[13,14]. The hernia defect is often repaired with the use of synthetic mesh due to the size of the hernias, constant tension on the diaphragm muscle, and poor muscle redundancy in that area, which can increase tension on the sutures. However, for smaller defects and increased diaphragmatic redundancy, primary repairs may provide satisfactory results with low hernia recurrence rates[15]. In our patient, we opted for a primary repair due to a colonic perforation and concerns about mesh infection. The defect was repaired with interrupted non-absorbable sutures, with satisfactory results. It has been traditionally advised not to remove the hernia sac in order to prevent massive pneumomediastinum[16]. However, in our patient’s case, we decided to remove the sac to adequately expose the diaphragmatic muscle edge and avoid using the sac for closure. This approach has more recently been found to reduce the likelihood of recurrence, while lowering the risk of fluid collection[17].
A MH is a rare congenital condition that can present in both pediatric and adult populations. While the majority of cases in adults are asymptomatic, some may present with severe, life-threatening symptoms. Thus, surgical correction is recommended for patients with acceptable surgical risk, even if they are asymptomatic. Due to its rarity, there is a lack of awareness in recognizing its clinical presentation. Colonic perforation is a serious complication of colonoscopy that requires both prevention and early detection and intervention if it occurs. The current case report is only the second published description of a MH complicating colonoscopy and leading to perforation. We share this experience along with recommendations to increase the suspicion of such an intraprocedural event, in the hopes that heightened awareness can lead to early diagnosis and the prevention of complications during colonoscopy.
The authors extend their gratitude to Ms. Fathiya Al Alawi for her contribution of design and editing expertise in creating and refining Figure 1. Additionally, the authors appreciate the efforts of Ms. Myriam Martel in collecting data for the literature review.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Canada
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Okasha H, Egypt S-Editor: Che XX L-Editor: A P-Editor: Chen YX
| 1. | Lim L, Gilyard SM, Sydorak RM, Lau ST, Yoo EY, Shaul DB. Minimally Invasive Repair of Pediatric Morgagni Hernias Using Transfascial Sutures with Extracorporeal Knot Tying. Perm J. 2019;23:18.208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (1)] |
| 2. | Mohamed M, Al-Hillan A, Shah J, Zurkovsky E, Asif A, Hossain M. Symptomatic congenital Morgagni hernia presenting as a chest pain: a case report. J Med Case Rep. 2020;14:13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 3. | Mitrovic M, Jankovic A, Djokic Kovac J, Skrobic O, Simic A, Sabljak P, Ivanovic N. Perforated Appendicitis and Bowel Incarceration within Morgagni Hernia: A Case Report. Medicina (Kaunas). 2021;57:89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Bianchi E, Mancini P, De Vito S, Pompili E, Taurone S, Guerrisi I, Guerrisi A, D'Andrea V, Cantisani V, Artico M. Congenital asymptomatic diaphragmatic hernias in adults: a case series. J Med Case Rep. 2013;7:125. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Stoll C, Alembik Y, Dott B, Roth MP. Associated malformations in cases with congenital diaphragmatic hernia. Genet Couns. 2008;19:331-339. [PubMed] |
| 6. | Kotecha S, Barbato A, Bush A, Claus F, Davenport M, Delacourt C, Deprest J, Eber E, Frenckner B, Greenough A, Nicholson AG, Antón-Pacheco JL, Midulla F. Congenital diaphragmatic hernia. Eur Respir J. 2012;39:820-829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 103] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 7. | Longoni M, Pober BR, High FA. Congenital Diaphragmatic Hernia Overview. 2006 Feb 1. In: GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993–. [PubMed] |
| 8. | Chandrasekharan PK, Rawat M, Madappa R, Rothstein DH, Lakshminrusimha S. Congenital Diaphragmatic hernia - a review. Matern Health Neonatol Perinatol. 2017;3:6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 108] [Cited by in RCA: 147] [Article Influence: 18.4] [Reference Citation Analysis (2)] |
| 9. | Supomo S, Darmawan H. A rare adult morgagni hernia mimicking lobar pneumonia. Turk J Surg. 2022;38:98-100. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Eren S, Gümüş H, Okur A. A rare cause of intestinal obstruction in the adult: Morgagni's hernia. Hernia. 2003;7:97-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Katsaros I, Katelani S, Giannopoulos S, Machairas N, Kykalos S, Koliakos N, Kapetanakis EI, Bakopoulos A, Schizas D. Management of Morgagni's Hernia in the Adult Population: A Systematic Review of the Literature. World J Surg. 2021;45:3065-3072. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 12. | Polat N, Kesici U, Kesici S, Yılbaş S. Morgagni hernia detected due to pneumothorax development during diagnostic colonoscopy. Turk J Gastroenterol. 2014;25:448-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Kuikel S, Shrestha S, Thapa S, Maharjan N, Kandel BP, Lakhey PJ. Morgagni hernia in adult: A case report. Int J Surg Case Rep. 2021;85:106286. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 14. | Nguyen T, Eubanks PJ, Nguyen D, Klein SR. The laparoscopic approach for repair of Morgagni hernias. JSLS. 1998;2:85-88. [PubMed] |
| 15. | Aghajanzadeh M, Khadem S, Khajeh Jahromi S, Gorabi HE, Ebrahimi H, Maafi AA. Clinical presentation and operative repair of Morgagni hernia. Interact Cardiovasc Thorac Surg. 2012;15:608-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 16. | Sharma A, Khanna R, Panigrahy P, Meena RN, Mishra SP, Khanna S. An Incidental Finding of Morgagni Hernia in an Elderly Female and Its Successful Management: A Rare Case Report and Review of Literature. Cureus. 2023;15:e42676. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 17. | Loong TP, Kocher HM. Clinical presentation and operative repair of hernia of Morgagni. Postgrad Med J. 2005;81:41-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 90] [Article Influence: 4.5] [Reference Citation Analysis (0)] |