Published online Apr 26, 2024. doi: 10.12998/wjcc.v12.i12.2116
Peer-review started: January 8, 2024
First decision: January 23, 2024
Revised: February 13, 2024
Accepted: March 25, 2024
Article in press: March 25, 2024
Published online: April 26, 2024
Processing time: 99 Days and 3.5 Hours
Angioleiomyoma is a rare and benign stromal tumor typically found in subcu
This case report detailed the discovery of intestinal angioleiomyoma in a 47-year-old male presenting with abdominal pain that had persisted for 3 d. After suspecting hollow organ perforation, surgical intervention involving intestinal resection and anastomosis was performed.
The report underscores the significance of early surgical intervention in effectively treating angioleiomyoma while emphasizing the pivotal role of timely and appropriate measures for favorable outcomes.
Core Tip: Here we report the first case of angioleiomyoma in the small intestine with a complication of perforation. This type of complication is extremely rare as the last published report of a perforation complication related to angioleiomyoma was published 30 years ago in Russian.
- Citation: Hou TY, Tzeng WJ, Lee PH. Small intestine angioleiomyoma as a rare cause of perforation: A case report. World J Clin Cases 2024; 12(12): 2116-2121
- URL: https://www.wjgnet.com/2307-8960/full/v12/i12/2116.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i12.2116
Angioleiomyomas are a vascular subtype of leiomyomas, categorized as benign smooth muscle tumors. The tumor itself is characterized by inclusion of vessel and smooth muscle cells[1]. Angioleiomyomas mostly arise from the wall of a vein. The majority of cases occur at 30 years to 60 years of age, with female predominance and location in a lower extremity[2]. Although, angioleiomyomas have been found in different organs[3-5]. Within the gastrointestinal tract, occurrences of angioleiomyomas are exceptionally rare[6]. This case report presents the inaugural instance documented in the English literature and details a patient who exhibited hollow organ perforation attributable to angioleiomyoma.
A 47-year-old male presented with lower abdominal pain and diarrhea.
The patient reported that his symptoms started 3 d prior to presentation, with both gradually progressing over that period. He also reported having a fever that would go up to 39 °C for 1 wk.
The patient had a medical history of controlled hypertension for many years.
The patient’s personal and family history was unremarkable.
The physical examination revealed the following: Body temperature, 36.7 °C; heart rate, 105 beats/min; respiratory rate, 18 breaths/min; and blood pressure, 125/80 mmHg. The skin and mucous membranes were free of yellow staining, rash, bleeding spots, liver palms, and spider nevus. Chest breathing was normal. However, the tenderness over the low abdomen and rebounding pain was mentioned.
Laboratory tests indicated elevated C-reactive protein (335 mg/L; normal range: < 5 mg/L) and increased creatinine (1.81 mg/dL; normal range: 0.64 mg/dL-1.27 mg/dL).
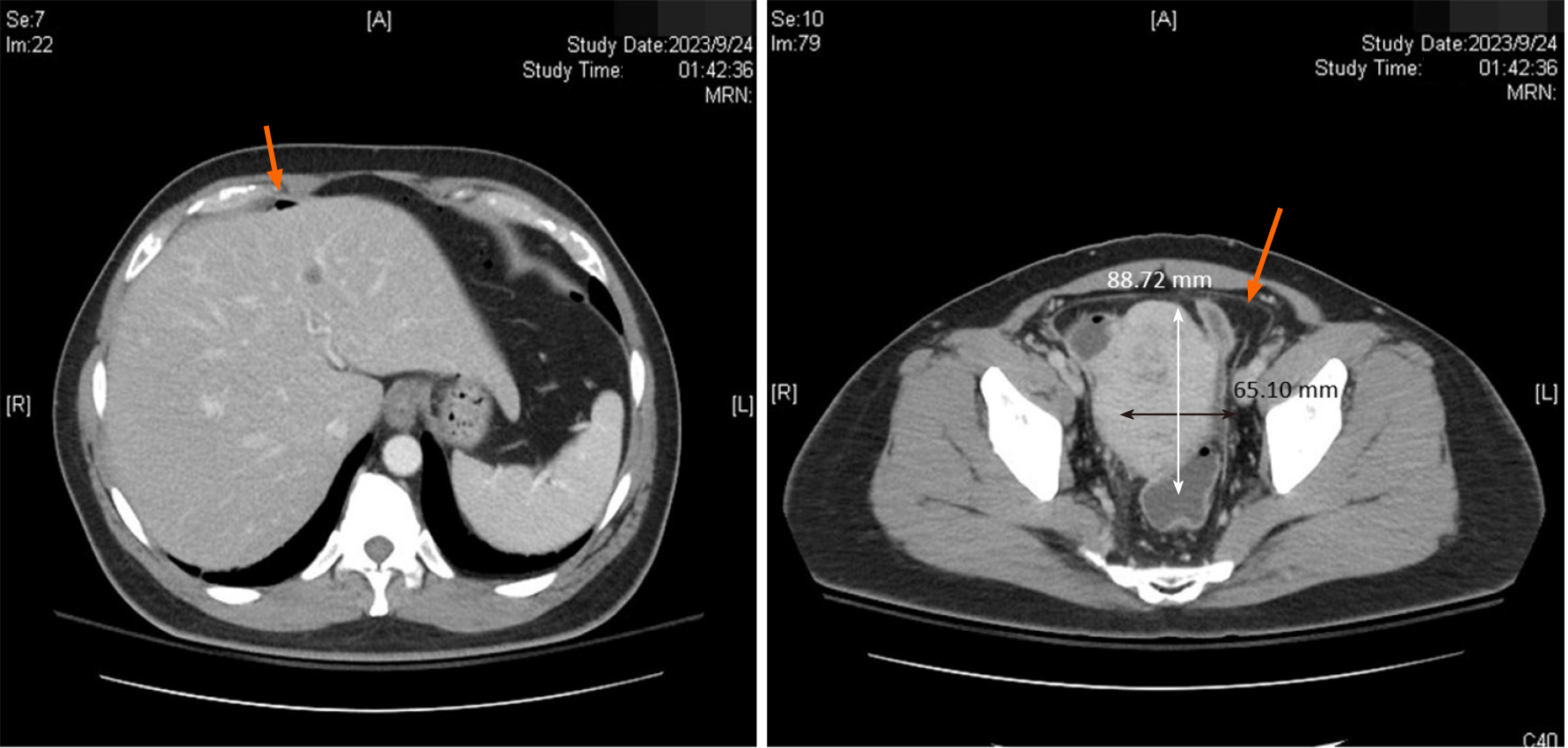
Computed tomography (CT) showed pneumoperitoneum and a mass over the pelvic area (Figure 1).
Ileum angioleiomyoma with complications of perforation and pneumoperitoneum.
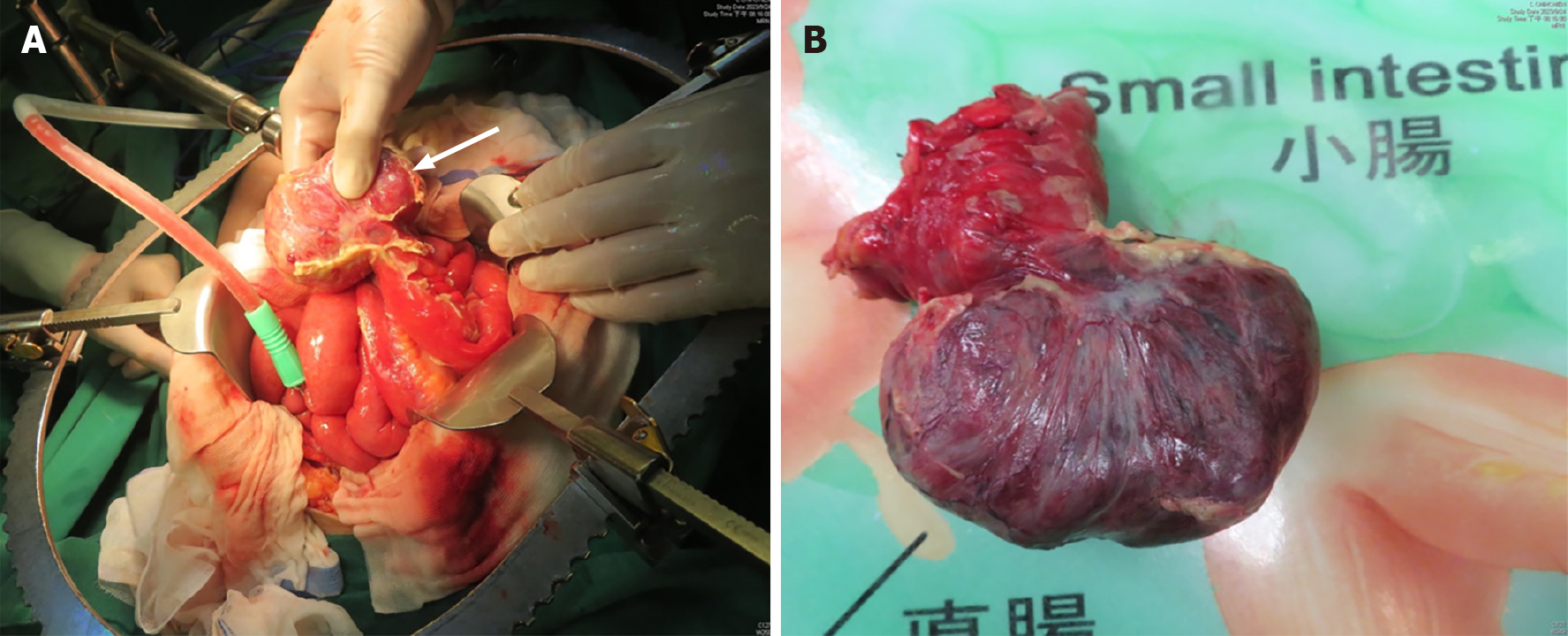
We initially suspected a perforation associated with sigmoid colon cancer. Therefore, surgical intervention was initiated approximately 7 h after admission. An exploratory laparotomy revealed a tumor, measuring 8 cm × 5 cm, located 70 cm from the ileocecal valve. It was surrounded by an abscess formation (Figure 2). A thorough examination of the stomach, intestine, and colon did not reveal additional perforation. The tumor was excised followed by end-to-end anastomosis.
Postoperatively, the patient was transferred to the ward for continued care and was discharged 2 wk after the operation. The patient returned to our clinic for follow-up after 2 wk without complaint of abdominal pain, nausea nor vomiting. The immunohistochemical analysis of the resected specimen corroborated the diagnosis of angioleiomyoma.
Leiomyomas are most frequently located in the uterine myometrium (95.0%), followed by the skin (3.0%) and the gastrointestinal tract (1.5%)[6]. In 1969, the World Health Organization defined leiomyomas as well-circumscribed benign tumors composed of bundles of mature smooth muscle cells. The World Health Organization classification includes three main groups: Solid leiomyoma; vascular leiomyoma (angioleiomyoma); and epithelioid leiomyoma (leiomyoblastoma)[7]. Angioleiomyoma, initially described by Stout[8] in 1937, commonly affects the skin and subcutaneous tissue of the lower extremities. Its presence in the gastrointestinal tract is exceptionally rare. Angioleiomyomas in the gastrointestinal tract occur predominantly in the jejunum (44%), followed by the ileum (37%) and the duodenum (19%).
Four distinct subtypes of angioleiomyoma have been identified[2]. The first type is capillary or solid angioleiomyomas. They are characterized by a rich stratification of smooth muscle cells surrounding a few slit-like vascular channels. This subtype is the most common. The second type is venous angioleiomyomas, which is distinguished by more vascular channels and walls that are thicker compared to capillary angioleiomyomas. The third type is cavernous angio
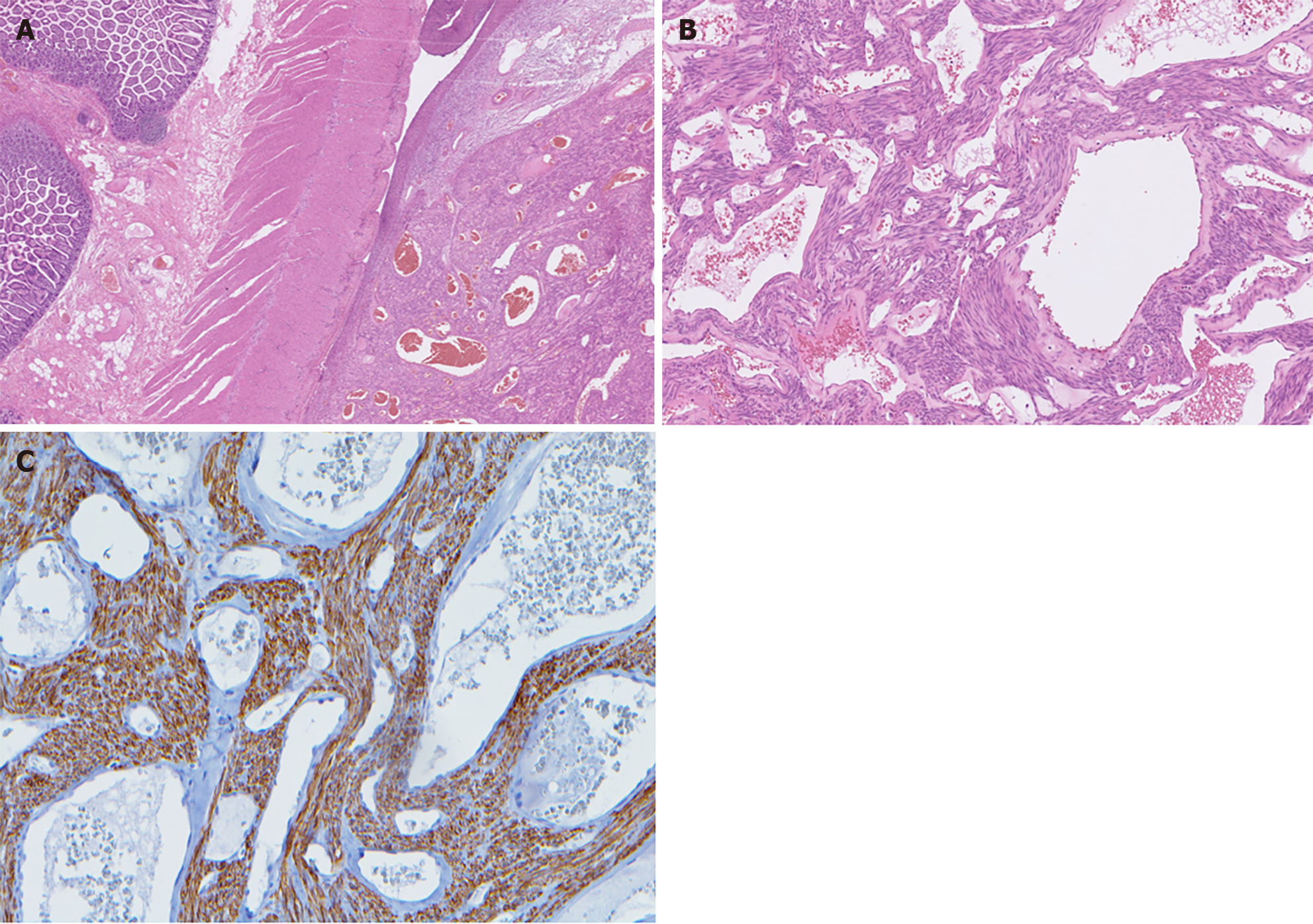
Our patient was diagnosed with cavernous angioleiomyoma based on histological findings. Sections showed ileal tissue with a well-circumscribed subserosal tumor composed of proliferative spindle smooth muscle cells bearing brightly eosinophilic cytoplasm and arranged in fascicles, punctuated by variable-sized vascular channels. The vessels were irregularly dilated with attenuated walls. There was also a lack of a thick muscular wall (Figure 3).
The clinical presentation of angioleiomyoma is diverse. Uncomplicated cases are typically asymptomatic. However, a limited number of reported cases exhibit rare clinical presentations. Therefore, it is challenging to establish comprehensive clinical features and complication rates. Only 10 cases of gastrointestinal angioleiomyoma have been documented in the literature. Table 1 compares these cases with our own.
| Ref. | Age, sex | Location | Complication | Diagnosis | Treatment |
| Valnicek[11], 1959 | NA | Small bowel | GIB | NA | NA |
| Gădăleanu and Popescu[12], 1988 | 31, female | Duodenojejunal flexture | GIB | Laparotomy | 2 stages: (1) Tumor vascular pedicle ligation; and (2) Resection |
| Sapelkin[13], 1989 | NA | Small bowel | Perforation | NA | NA |
| Pidoprigora et al[14], 1995 | NA | Small bowel | GIB | NA | NA |
| Sadat et al[9], 2007 | 58, female | Ileum | GIB | Angiography | Resection |
| Nakatani et al[15], 2010 | 45, female | Ileum | GIB | Capsule endoscopy + double-balloon enteroscopy | Resection |
| Turan et al[16], 2010 | Age not known, female | Ileum | Intussusception | CT | Resection |
| Stanojević et al[17], 2013 | 40, female | Rectum | Prolapse | Clinical | Tumor excision |
| Gachabayov and Mityushin [18], 2016 | 21, male | Jejunum | GIB | CT | Resection |
| Shao et al[19], 2018 | 42, male | Jejunum | GIB | Double balloon enteroscopy | Resection |
| Our case | 47, male | Ileum | Perforation | CT | Resection |
Gastrointestinal bleeding is the most commonly reported complication associated with angioleiomyoma. Past cases have reported other complications, such as intussusception and prolapse. Notably, our case represents the first reported instance of angioleiomyoma-related perforation in the English literature.
In our case, preoperative imaging, specifically CT, revealed a lesion located in the pelvic region accompanied by pneumoperitoneum. We initially suspected malignancy-related hollow organ perforation. Despite the absence of tarry or bloody stool reported by the patient, CT indicated a tumor of 9.5 cm × 6.5 cm × 6.4 cm in size that was surrounded by abscess.
Surgical resection of the affected bowel segment is the typical treatment to manage the angioleiomyoma and any accompanying complications. Resection is typically followed by side-to-side anastomosis, which was also performed in our case. Given the initial suspicion of hollow organ perforation, a comprehensive inspection of the entire abdomen was essential to identify potential perforations caused by other etiologies. This thorough examination was crucial to ensure an accurate diagnosis and appropriate intervention.
In summary, small bowel angioleiomyoma is a rare occurrence. Perforation is also a rare complication related to angioleiomyoma. Nonetheless, early surgical intervention plays a crucial role in the effective treatment of angio
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ikura Y, Japan S-Editor: Che XX L-Editor: A P-Editor: Yu HG
| 1. | Beissert M, Kenn W, Schultz G, Keberle M, Eck M, Hahn D. Hepatic angiomyoma: CT and MRI findings. Abdom Imaging. 2002;27:40-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Hachisuga T, Hashimoto H, Enjoji M. Angioleiomyoma. A clinicopathologic reappraisal of 562 cases. Cancer. 1984;54:126-130. [PubMed] [DOI] [Full Text] |
| 3. | Matsuyama A, Hisaoka M, Hashimoto H. Angioleiomyoma: a clinicopathologic and immunohistochemical reappraisal with special reference to the correlation with myopericytoma. Hum Pathol. 2007;38:645-651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 77] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 4. | Brooks JK, Nikitakis NG, Goodman NJ, Levy BA. Clinicopathologic characterization of oral angioleiomyomas. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:221-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 74] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 5. | Jamiyan T, Kuroda H, Luvsan G, Munkhnyam T, Kakumoto A, Enkhbat B. Primary Hepatic Angioleiomyoma: A Case Report. Am J Case Rep. 2023;24:e938645. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 6. | Veeresh M, Sudhakara M, Girish G, Naik C. Leiomyoma: A rare tumor in the head and neck and oral cavity: Report of 3 cases with review. J Oral Maxillofac Pathol. 2013;17:281-287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 7. | Enzinger FM, Lattes R, Torloni H. Histological typing of soft tissue tumors. International histological classification of tumors. No. 3, Geneva. World Health Organization, 1969: 42. Available from: https://scholar.google.com/scholar?q=Enzinger+FM+Lattes+R+Torloni+H+Histological+Typing+of+Soft+Tissue+Tumours+1969+Geneva+World+Health+Organization+30+1+. |
| 8. | Stout AP. Solitary Cutaneous and Subcutaneous Leiomyoma. Am J Cancer. 1937;29:435-69. [RCA] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 154] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Sadat U, Theivacumar NS, Vat J, Jah A. Angioleiomyoma of the small intestine - a rare cause of gastrointestinal bleeding. World J Surg Oncol. 2007;5:129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Agaimy A, Wünsch PH. True smooth muscle neoplasms of the gastrointestinal tract: morphological spectrum and classification in a series of 85 cases from a single institute. Langenbecks Arch Surg. 2007;392:75-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 63] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 11. | Valnicek V. [Angioleiomyoma of the small intestine as a cause of severe melena]. Rozhl Chir. 1959;38:848-880. [PubMed] |
| 12. | Gădăleanu V, Popescu V. Angiomyoma and vascular ectasia of the small bowel as a cause of intestinal bleeding. Pathol Res Pract. 1988;183:519-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Sapelkin OS. [Angioleiomyoma of the small intestine complicated by perforation]. Klin Khir (1962). 1989;61-62. [PubMed] |
| 14. | Pidoprigora AP, Chmeruk SP, Fedorchuk LI, Shuldik SI. [Angioleiomyoma of the small intestine as a cause of recurrence of hemorrhage]. Klin Khir. 1995;48. [PubMed] |
| 15. | Nakatani M, Fujiwara Y, Kameda N, Okazaki H, Watanabe T, Tominaga K, Arakawa T, Noda E, Inoue T, Maeda K, Hirakawa K, Wakasa K. Angioleiomyoma of the small intestine detected by double-balloon enteroscopy. Gastrointest Endosc. 2010;72:187-8; discussion 188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Turan M, Karadayi K, Duman M, Ozer H, Arici S, Yildirir C, Koçak O, Sen M. Small bowel tumors in emergency surgery. Ulus Travma Acil Cerrahi Derg. 2010;16:327-333. [PubMed] |
| 17. | Stanojević GZ, Mihailović DS, Nestorović MD, Radojković MD, Jovanović MM, Stojanović MP, Branković BB. Case of rectal angioleiomyoma in a female patient. World J Gastroenterol. 2013;19:2114-2117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Gachabayov M, Mityushin P. Recurrent Midgut Bleeding due to Jejunal Angioleiomyoma. Case Rep Surg. 2016;2016:4569781. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 19. | Shao XD, Liang ZD, Guo XZ. A Small Jejunal Angioleiomyoma Detected by Double-Balloon Enteroscopy: A Case Report. Am J Case Rep. 2018;19:1126-1128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |