Published online Apr 16, 2024. doi: 10.12998/wjcc.v12.i11.1980
Peer-review started: January 22, 2024
First decision: February 28, 2024
Revised: March 1, 2024
Accepted: March 21, 2024
Article in press: March 21, 2024
Published online: April 16, 2024
Processing time: 80 Days and 5.7 Hours
This case report presents the rare occurrence of hematochezia due to an internal iliac artery aneurysm leading to an arterioenteric fistula, expanding the differential diagnosis for gastrointestinal bleeding. It emphasizes the importance of considering vascular origins in cases of atypical hematochezia, particularly in the absence of common gastrointestinal causes, and highlights the role of imaging and multidisciplinary management in diagnosing and treating such unusual presentations.
A 75-year-old man with a history of hypertension presented with 12 d of hematochezia, experiencing bloody stools 7-8 times per day. Initial computed tomography (CT) scans revealed an aneurysmal rupture near the right internal iliac artery with suspected hematoma development. Hemoglobin levels progre
In cases of unusual gastrointestinal bleeding, it is necessary to consider vascular causes for effective diagnosis and intervention.
Core Tip: Lower gastrointestinal bleeding (LGIB) is one of the primary causes of morbidity and mortality in middle-aged and elderly individuals. Hematochezia is a primary manifestation of LGIB and is often associated with ulcers, tumors, and vascular malformations. Here, we report a very rare etiology, which can be attributed to an internal iliac artery aneurysm invading the proximal rectum causing an arterial fistula to the rectum, resulting in massive hematochezia. We hope that this case serves as a reminder that hematochezia may stem from less common causes.
- Citation: Li F, Zhao B, Liu YQ, Chen GQ, Qu RF, Xu C, Long Z, Wu JS, Xiong M, Liu WH, Zhu L, Feng XL, Zhang L. Hematochezia due to rectal invasion by an internal iliac artery aneurysm: A case report. World J Clin Cases 2024; 12(11): 1980-1989
- URL: https://www.wjgnet.com/2307-8960/full/v12/i11/1980.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i11.1980
Lower gastrointestinal bleeding (LGIB) is one of the primary causes of morbidity and mortality in middle-aged and elderly individuals[1]. Hematochezia is a primary manifestation of LGIB and is often associated with ulcers, tumors, and vascular malformations. The terminologies "pseudoaneurysm", "false aneurysm", and "pulsating hematoma" are synonymous, each referring to a specific vascular anomaly characterized by a defect in the vascular wall[2]. This defect culminates in the formation of an extravascular hematoma, which maintains open communication with the intravascular space[3]. An internal iliac artery (IIA) aneurysm is the result of localized dilation of the iliac artery. This may be caused by structural weakness in the arterial wall, typically due to atherosclerosis[4]. The aneurysm may be asymptomatic but can cause serious complications upon enlargement or rupture. Isolated internal iliac artery aneurysm (IAAs) are rare, and rectal bleeding as the primary symptom is even more uncommon. Here, we present an unusual etiology of massive hematochezia attributable to an internal IAA, leading to an arterial fistula to the rectum.
The patient had hematochezia for 12 d and slight abdominal pain.
A 75-year-old man with hematochezia presented to the emergency room in October 2022 due to a 12-d history of hematochezia. The patient’s stool was bloody and dark red. He produced bloody stools approximately 7-8 times per day, approximately 100 mL each time, with no accompanying symptoms of fever, vomiting, or abdominal distension. After visiting a local clinic and receiving antibiotic treatment, there was no significant improvement. Since the patient’s onset, these symptoms have recurred repeatedly. Three hours prior, the patient experienced an increase in the frequency of bloody stools, accompanied by abdominal pain.
The patient was diagnosed with hypertension 8 years ago. Initially, the condition was identified during a routine health check-up, during which the patient presented with persistently elevated blood pressure readings, averaging 160/95 mmHg. His medical history indicated a gradual increase in blood pressure over the years despite the initiation of antihypertensive therapy. The patient had been on a combination of levoamlodipine besylate and hydrochlorothiazide for the past 8 years, and his blood pressure was partially controlled. He says he usually takes his medication as directed, but sometimes he does not follow the recommended diet and exercise guidelines.
He had no personal or family history of artery aneurysm or any specific disease.
Upon arrival, his blood pressure was 165/107 mmHg, and his heart rate was 109 beats per minute. Abdominal examination revealed slight abdominal distension and a relatively soft abdomen. Tenderness was present in the lower abdomen, with no rebound tenderness or muscle rigidity. Vascular examination revealed normal arterial pulsations in both lower extremities, with no edema or muscle atrophy present. Digital rectal examination revealed normal anal sphincter function, with the rectal mucosa being soft and smooth. Insertion of the finger was unobstructed, and no narrowing or palpable masses were detected. Upon withdrawal, the glove was stained with blood.
Laboratory tests revealed a decrease in hemoglobin (Hb) (7 g/dL), an elevated white blood cell count (12.6 × 109/L), an increased percentage of neutrophils (88.2%), and an increased CRP level (22.7 mg/dL). There was no evidence of hematuria, with 0-4 red blood cells per high-power field observed under the microscope.
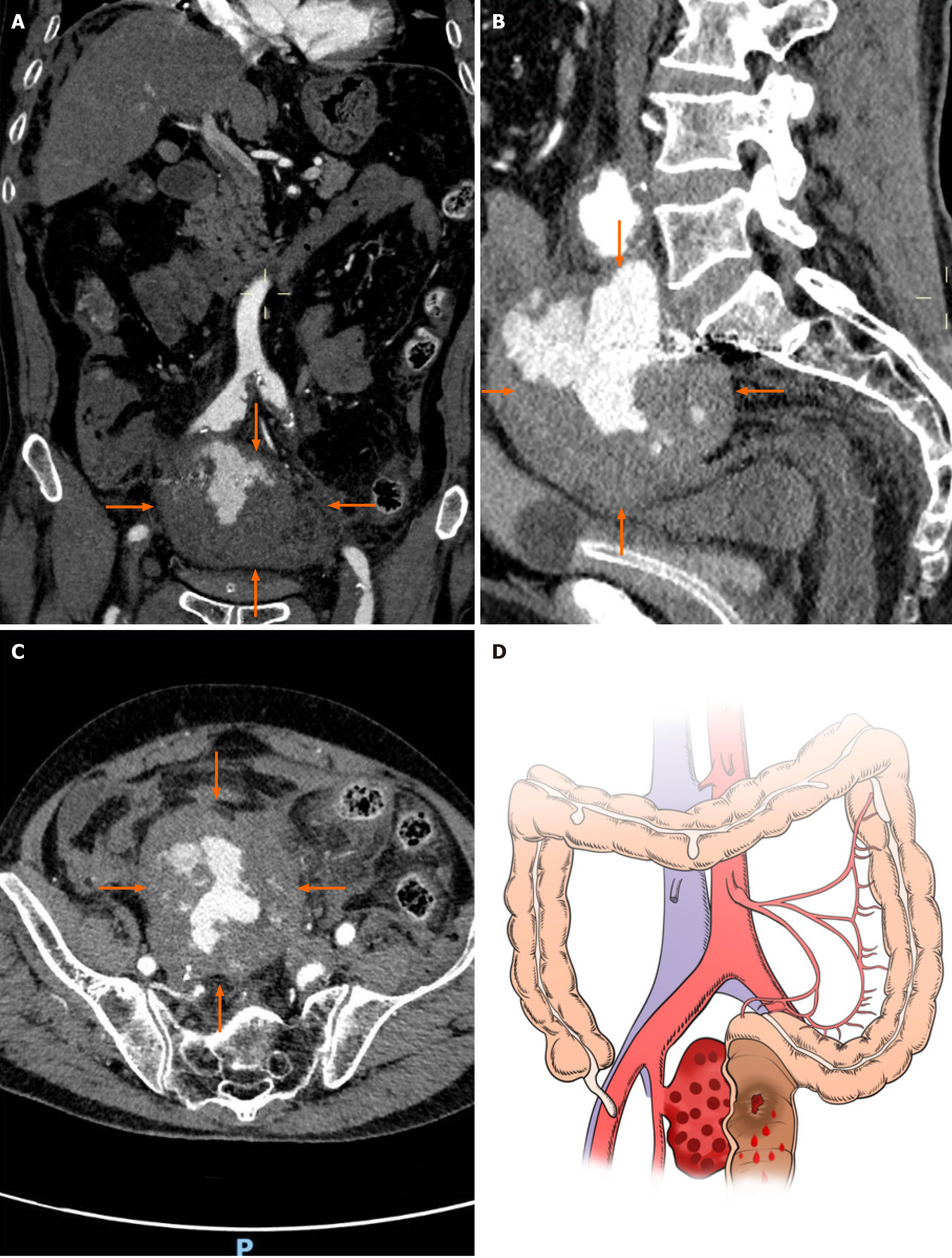
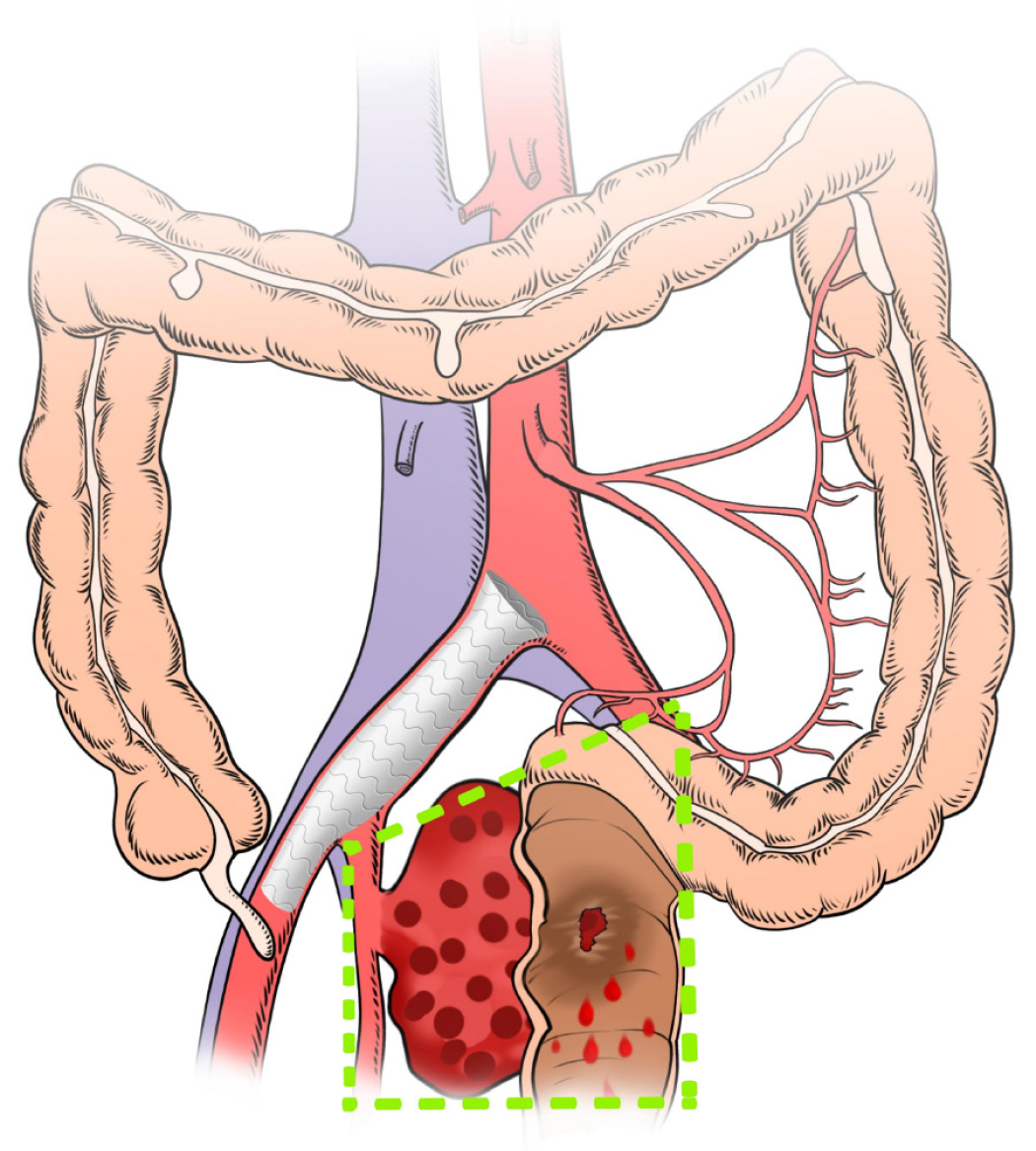
The chest X-ray, electrocardiogram, and cardiac ultrasound examination revealed no abnormalities. The patient underwent an enhanced computed tomography (CT) of the entire abdomen and pelvis. CT (Figure 1A-C) revealed an oval-shaped mixed-density mass on the medial side of the right IIA measuring approximately 9.5 cm × 8.5 cm × 7.0 cm. An enhanced scan revealed contrast agent entry inside, closely related to the right IIA, suggesting the possibility of aneurysm rupture and hematoma formation. Imaging also showed signs of hemoperitoneum and peritonitis. An illustration (Figure 1D) shows that the rectal wall was invaded by the right internal IAA, which led to rectal bleeding.
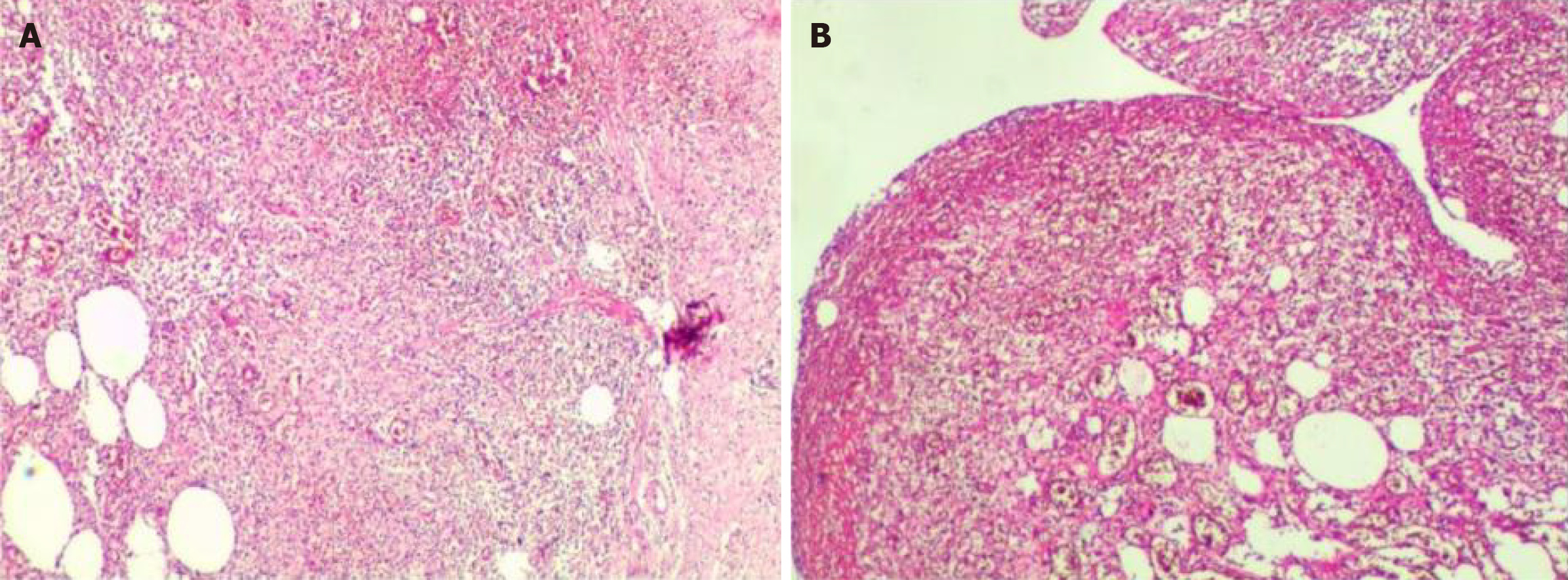
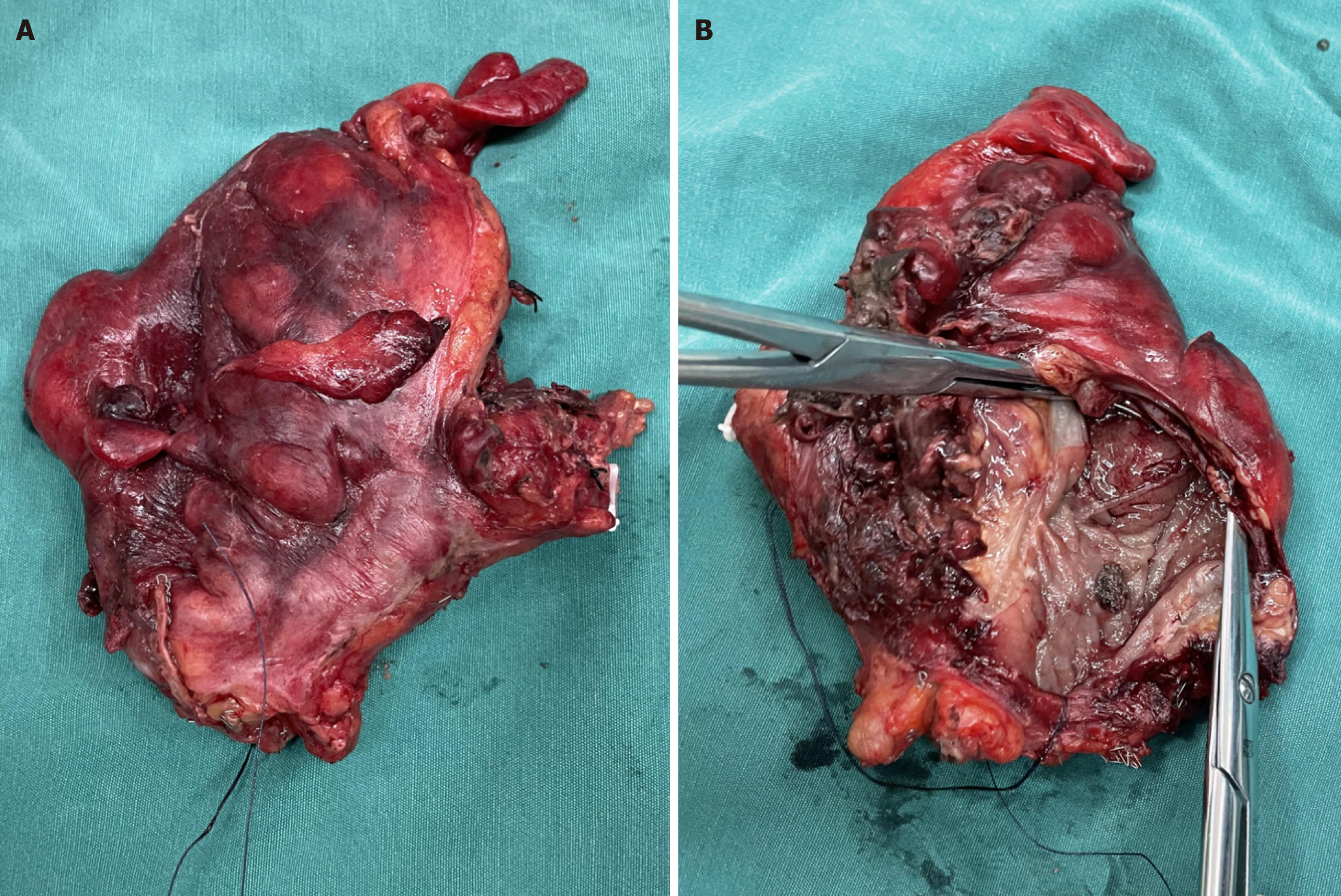
The patient was ultimately diagnosed with an internal IAA rupture and rectal perforation. Pathological examination of the aneurysm wall revealed hemorrhage and fibrous exudation (Figure 2A). Rectal pathologic examination revealed ulceration with perforation, mucosal edema, submucosal and serosal purulent inflammation with bleeding and necrosis, consistent with changes related to intestinal perforation. Ulceration was noted at one end of the rectum, while the other end was free of disease (Figure 2B). Additionally, reactive hyperplasia of the perienteric lymph nodes (17 in total) was observed.
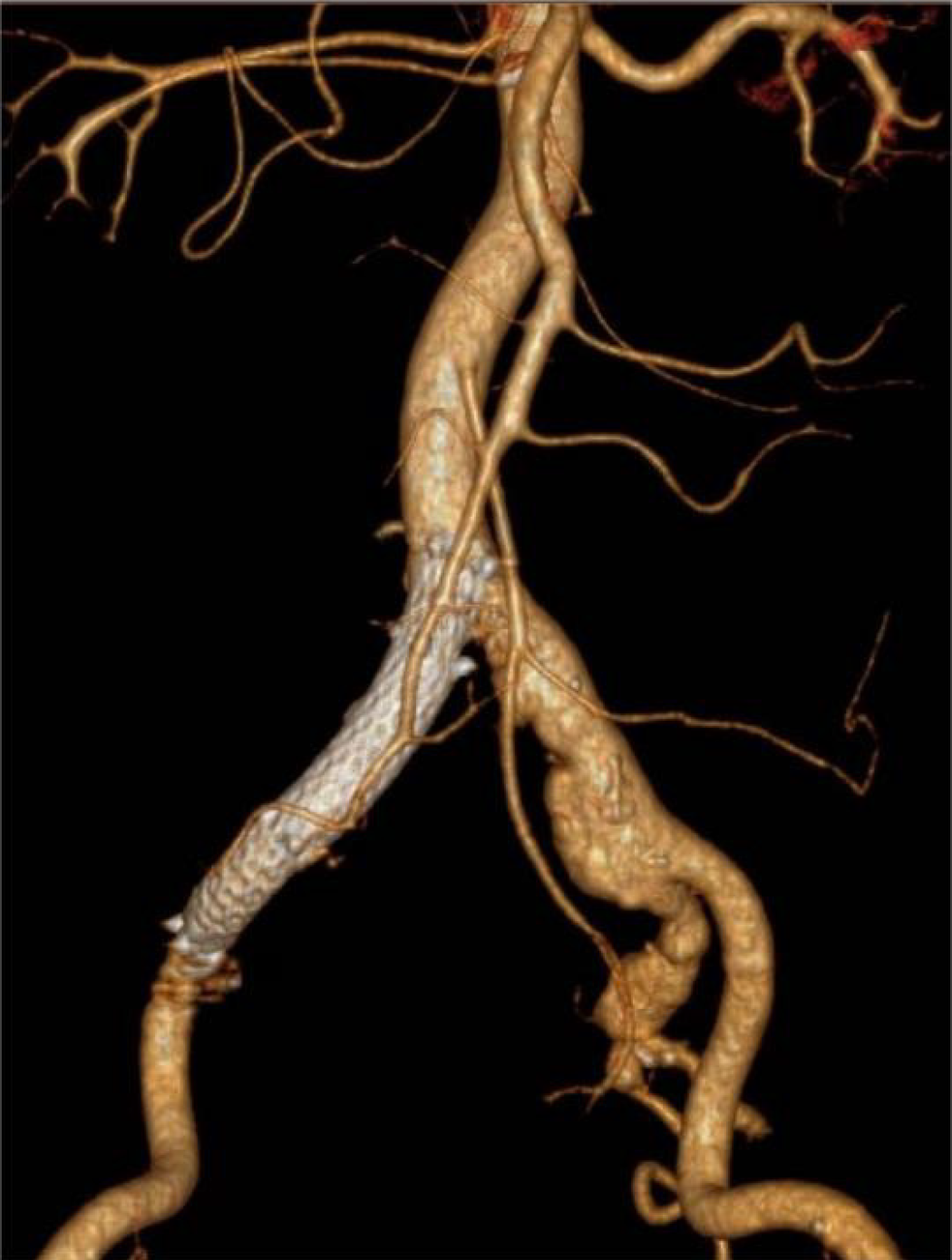
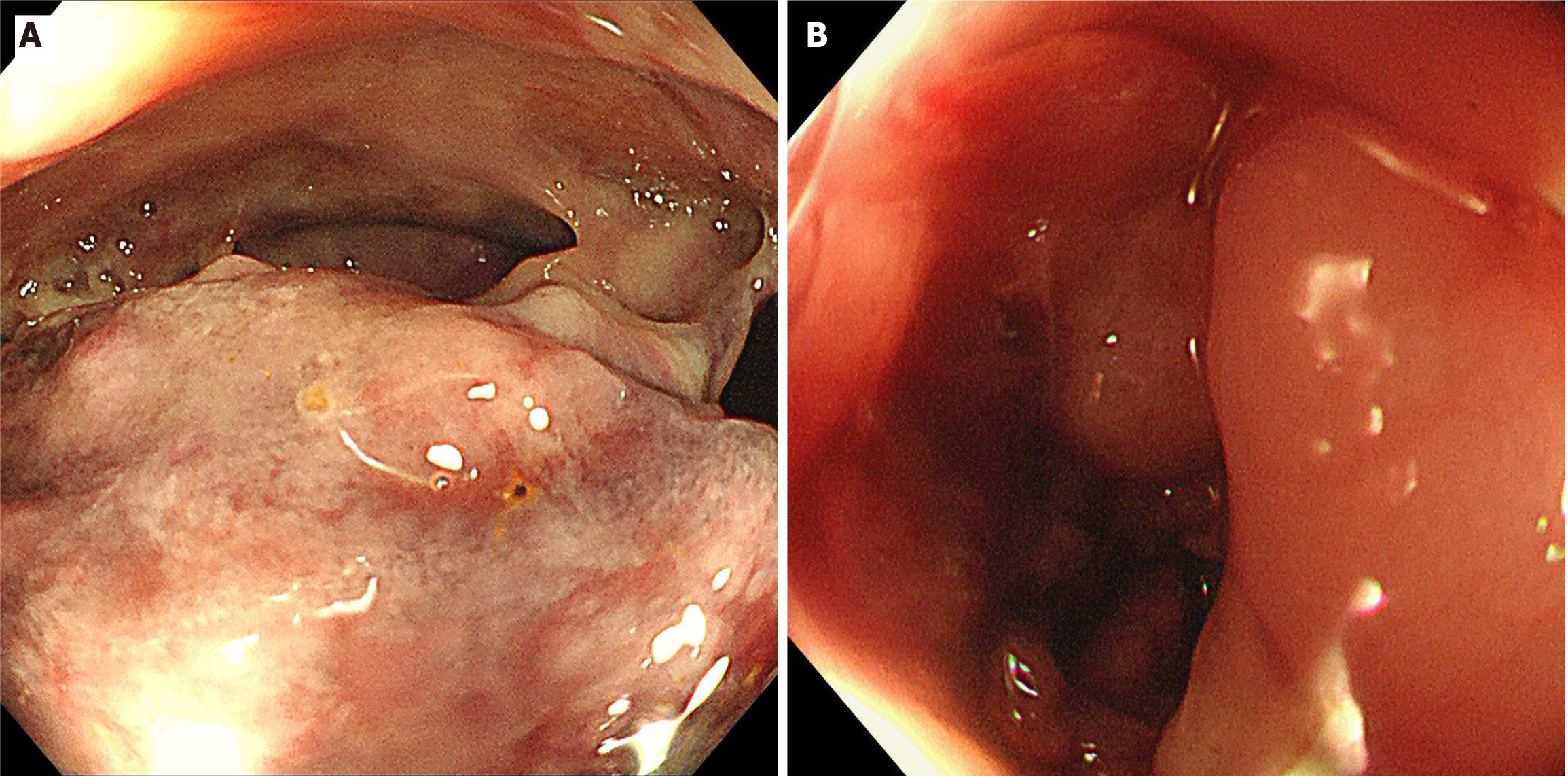
After reviewing the enhanced CT results, the emergency department physician consulted with a vascular surgeon. Following a thorough assessment of the patient’s condition, the vascular surgeon decided to perform arterial angiography, place a covered stent into the iliac artery and perform a balloon angioplasty operation under local anesthesia (Figure 3). Two days after the operation, the patient's vital signs were stable, but he reported minor rectal bleeding and mild abdominal pain. For a more definitive diagnosis, the patient was subjected to a colonoscopic examination. Colonoscopy revealed a large neoplasm invading the pelvic cavity approximately 16 cm from the anus, covered with a turbid coating, blood clots, and purulent secretions, with bubbles visible on the surface, suggesting the possibility of a rectal neoplasm with perforation (Figure 4A). After the patient was transferred to the gastroenterological surgery department, an exploratory laparotomy was performed. During the surgery, a hematoma formed by the rupture of the internal IAA was found in the pelvic cavity on the right side of the rectum. The hematoma, approximately the size of an apple, contained a large amount of abscess and stool, giving off an intense malodorous smell. The tumor originated laterally from the right internal IAA and invaded the wall of the rectum on the medial side, communicating with the intestinal lumen. After successful removal of the hematoma and resection of the aneurysm, intraoperative colonoscopy was conducted and revealed a perforation of 0.8 cm in the rectum located 15 cm from the anus and surrounded by neoplastic growth and purulent secretions (Figure 4B). Combined with the intraoperative observations, it is clear that the perforation was located at the site where the hematoma invaded the rectum. During the operation, we decided to perform partial resection of the rectum, followed by intestinal anastomosis and prophylactic ileostomy (the extent of surgical excision is shown in Figure 5). The excised rectal specimen is shown in Figure 6. The surgery was successful, and the patient was discharged from the hospital 7 d later.
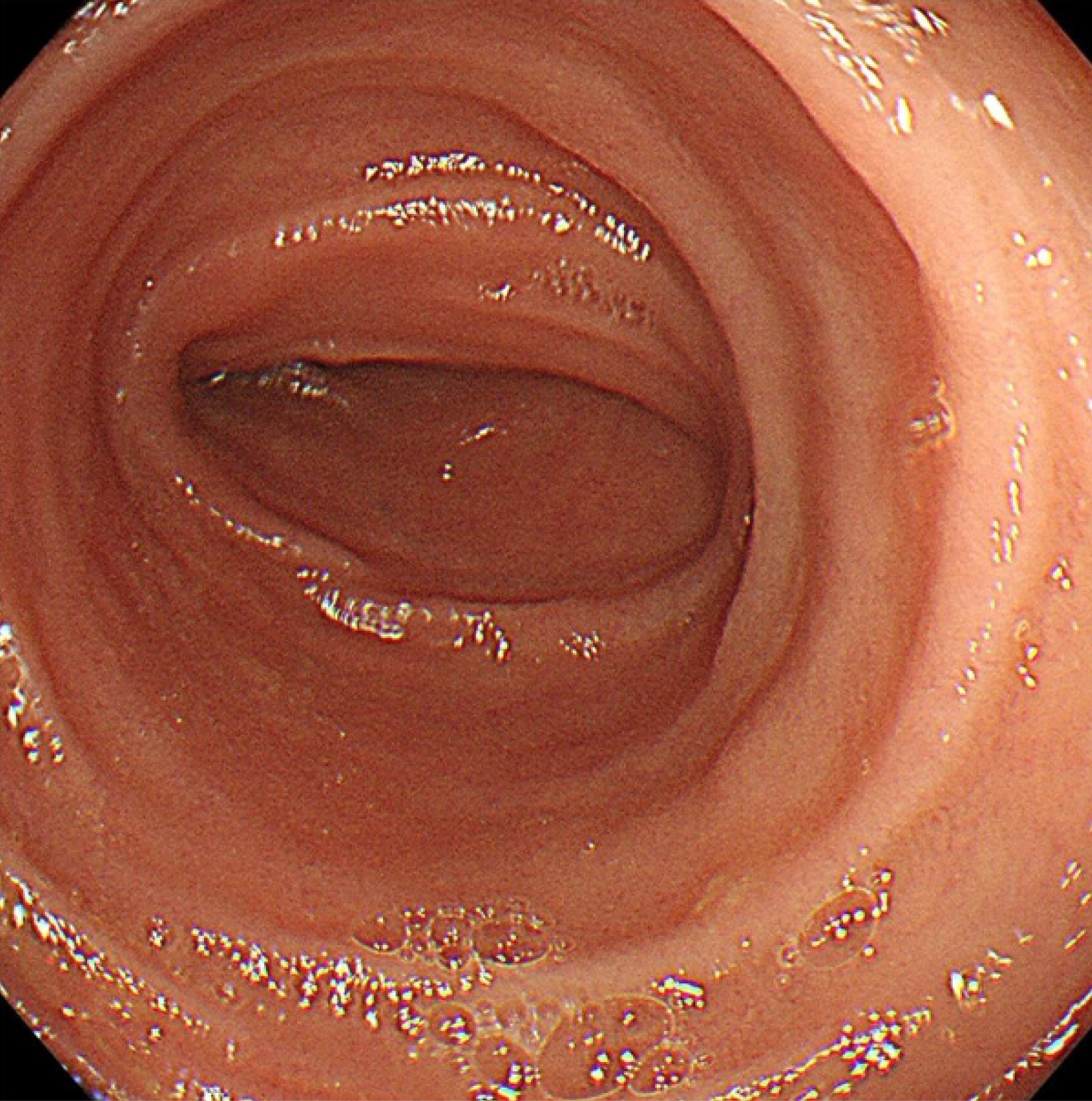
After being discharged, the patient recovered well and did not experience any additional episodes of hematochezia. Six months after discharge, he underwent follow-up enhanced CT of the entire abdomen. This investigation revealed no significant abnormalities, corroborating the absence of recurrent or residual vascular disease. Moreover, during the same follow-up period, a thorough colonoscopic examination was performed, which revealed a normal anastomotic site, with no intestinal stenosis, ulceration, or mass formation (Figure 7).
IAAs represent a distinct subset of vascular abnormalities characterized by localized dilatation of the iliac artery. The pathogenesis of IAAs typically involves degenerative changes in the arterial wall, often associated with atherosclerosis, leading to weakening and subsequent dilatation[5]. IAAs are markedly more prevalent in older populations, predominantly affecting males older than 60[6]. The exact incidence of IAAs is challenging to ascertain due to their relative rarity compared to aortic aneurysms. Studies suggest that IAAs constitute approximately 2%-6% of all abdominal arterial aneurysms[7]. Specifically, the common iliac artery is most commonly involved in approximately 70% of these aneurysms, while the IIA is involved in approximately 25% of case[8]. IAAs often coexist with other vascular abnormalities, especially abdominal aortic aneurysms. Approximately 10%-25% of patients with abdominal aortic aneurysms also present with IAAs[9].
Unruptured IAAs have a high risk of rupture and are associated with high mortality rates. The literature indicates that the mortality rate for patients with ruptured untreated IAAs can reach 80%, underscoring the importance of early detection and intervention[10]. In addition to the risk of rupture, IAAs are prone to thrombus formation and embolism, further increasing the mortality risk[11]. The risk factors for IAAs mirror those for atherosclerotic diseases and include hypertension, smoking, and hyperlipidemia[12,13]. If left untreated, IAAs are likely to rupture, which can lead to life-threatening hemorrhage or, in rare instances, adjacent organ invasion[14,15], as noted in the current case involving rectal bleeding.
Very little is known about the occurrence of an IAA invading the rectum, and few case reports on this topic have been published. This invasion can lead to gastrointestinal symptoms such as rectal bleeding, often leading to misdiagnosis or delayed diagnosis due to its nonspecific presentation.In the complex case of a 75-year-old male with hematochezia, a series of diagnostic and therapeutic interventions were performed. The initial enhanced abdominal CT scan revealed an aneurysmal rupture near the right IIA. A patient's progressively decreasing Hb levels indicated active bleeding. Emergency interventions included arterial angiography and iliac artery stent placement under local anesthesia, which are crucial for stabilizing the patient's condition. Despite these measures, the patient continued to experience minor rectal bleeding, which led to further investigations. A colonoscopic examination revealed a neoplasm in the proximal rectum and potential perforation. Surgical intervention, consisting of exploratory laparotomy, hematoma removal, partial rectal resection, and ileostomy, was performed. The pathologic findings were consistent with complications arising from aneurysmal rupture. With respect to initial management, a prompt response to the patient’s hemodynamic instability and the use of arterial angiography and stenting were appropriate and effective approaches. These steps are in line with current best practices for managing aneurysmal ruptures, where immediate stabilization is critical. In terms of surgical intervention, the decision to proceed with exploratory surgery following persistent symptoms was necessary. This approach allowed direct visualization and management of the complications associated with aneurysmal rupture and rectal neoplasm.
This report describing a rare case of an IAA invading the rectum and causing hematochezia has significant implications for clinical practice, particularly for vascular surgery and gastroenterology. The findings underscore the need to consider vascular etiologies in patients who present with gastrointestinal bleeding, especially in those of advanced age or with other risk factors. These presentations, though unusual, demand a high degree of clinical vigilance and a broad differential diagnosis.
The successful resolution of this complex case underscores the importance of an interdisciplinary approach involving specialists from emergency medicine, radiology, gastroenterology, and surgery. This collaborative effort is pivotal in managing such multifaceted cases, where the interplay of different organ systems and pathologies presents unique diagnostic and therapeutic challenges. Moreover, this case holds substantial value in informing clinical practice guidelines. This study provides insights into the management of rare and complex cases, highlighting the necessity for these guidelines to be adaptable and inclusive of atypical presentations and complications. The dynamic nature of such cases calls for comprehensive guidelines that are also sufficiently flexible to accommodate the nuances of individual patient presentations.
We are aware that there are several challenges and limitations in the management of this case. These challenges not only highlight areas for improvement but also underscore the complexity inherent in managing such atypical and severe vascular pathologies. First, early detection is challenging. One of the primary difficulties encountered in this case, and generally in similar cases, was the early detection of IAAs. The asymptomatic nature of these tumors, coupled with their deep pelvic location, often results in a delayed diagnosis. As observed in this case, the aneurysm was identified only after significant symptoms had developed, indicating a late stage of the disease. This delay in detection underscores the need for more proactive screening measures, especially in high-risk populations such as elderly individuals or those with a history of vascular diseases. Second, the unpredictable growth rate of these aneurysms presents another significant challenge. In this case, the rapid expansion of the aneurysm leading to rectal invasion highlights the dynamic nature of these aneurysms. This unpredictability necessitates a highly flexible and individualized approach to treatment, which can be difficult to standardize across different clinical settings. The development of predictive models or markers for aneurysm growth could potentially aid in more effective monitoring and timely intervention. Finally, uncertainties in the treatment of IIA aneurysms, as observed in this case, underscore the need for more extensive research and clinical trials. The management of IIA aneurysms also presents unique challenges. In this case, the rarity of IIA aneurysm invasion into the rectum added to the complexity of choosing the appropriate treatment strategy. The less defined treatment protocol for IIA aneurysms, due to their rarity, poses a challenge in developing a standardized approach. This uncertainty calls for more extensive research and clinical trials to establish clear guidelines for the management of such rare yet severe aneurysm presentations. Addressing these challenges requires concerted effort in research, clinical practice, and guideline development, focusing on early identification, understanding the natural history of aneurysms, and refining treatment protocols for rare and complex vascular conditions.
This case report not only provides a roadmap for managing a rare and complex medical scenario but also contributes to the broader understanding of interdisciplinary management of IAAs with gastrointestinal complications. This highlights the importance of integrating advanced imaging, prompt surgical intervention, and collaborative care in the treatment of such patients. Furthermore, the uniqueness of this case contributes valuable information for future research and educational endeavors in vascular surgery and gastroenterology. In particular, this study elucidates the management of IAAs with gastrointestinal complications, a relatively unexplored area. This case study could lead to advancements in both diagnostic approaches and therapeutic strategies for similar complex clinical scenarios. In summary, this case not only enhances the current clinical understanding but also serves as a guide for future explorations and improvements in patient care.
This case report of a rare IAA invading the rectum and resulting in hematochezia illustrates several critical aspects of vascular and gastrointestinal disease management. This highlights the need to consider vascular causes in elderly patients presenting with gastrointestinal symptoms, particularly when these symptoms are atypical. This case report not only elucidates the complex nature of managing IAAs but also highlights key areas for improving early detection, understanding the natural history of aneurysms, and refining treatment protocols for rare and complex vascular conditions. Addressing these challenges requires concerted efforts in research, clinical practice, and guideline development.
In conclusion, this case report is a significant contribution to the current literature on IAAs and their rare complications, offering important insights into their diagnosis and management and the need for ongoing research. Clinical guidelines should be developed to better address such complex medical situations, thus improving patient care and outcomes in similar cases.
The authors express their gratitude to the individuals who participated in this study.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Piltcher-da-Silva R, Brazil S-Editor: Zheng XM L-Editor: A P-Editor: Guo X
| 1. | Vora P, Pietila A, Peltonen M, Brobert G, Salomaa V. Thirty-Year Incidence and Mortality Trends in Upper and Lower Gastrointestinal Bleeding in Finland. JAMA Netw Open. 2020;3:e2020172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 2. | Moy Petersen JC, Vidal Insua JJ. Images in clinical medicine. Pseudoaneurysm after transradial coronary angiography. N Engl J Med. 2015;373:1361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Wolfgang GL, Barnes WT, Hendricks GL Jr. False aneurysm of the profunda femoris artery resulting from nail-plate fixation of intertrochanteric fracture. A case report and review of the literature. Clin Orthop Relat Res. 1974;143-150. [PubMed] |
| 4. | Crea F. Focus on translational vascular biology: new therapeutic targets in hypertension, aortic aneurysm, and atherosclerosis. Eur Heart J. 2023;44:2645-2649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 5. | Fossaceca R, Guzzardi G, Di Terlizzi M, Divenuto I, Cerini P, Malatesta E, Di Gesù I, Stanca C, Brustia P, Carriero A. Long-term efficacy of endovascular treatment of isolated iliac artery aneurysms. Radiol Med. 2013;118:62-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Chithra R, Sundar RA, Velladuraichi B, Sritharan N, Amalorpavanathan J, Vidyasagaran T. Pediatric isolated bilateral iliac aneurysm. J Vasc Surg. 2013;58:215-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Goksel OS, Gok E, Onalan MA, Güven K, Capar G, Cinar B, Alpagut IU. Endovascular Repair of Iliac Artery Aneurysms: A Single Center Experience in 10-Years. Heart Surg Forum. 2019;22:E088-E091. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Steenberge SP, Caputo FJ, Rowse JW, Lyden SP, Quatromoni JG, Kirksey L, Smolock CJ. Natural history and growth rates of isolated common iliac artery aneurysms. J Vasc Surg. 2022;76:461-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | Ruiz T, Alslaim HS, Frischmann D, Agarwal G. Endovascular management of isolated iliac artery aneurysm. Ann Vasc Surg. 2023;90:55-56. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Laine MT, Laukontaus SJ, Kantonen I, Venermo M. Population-based study of ruptured abdominal aortic aneurysm. Br J Surg. 2016;103:1634-1639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 11. | Guo Y, Yang B, Cai H, Jin H. Hybrid repair of penetrating aortic ulcer associated with right aortic arch and aberrant left innominate artery arising from aneurysmal Kommerell's diverticulum with simultaneous repair of bilateral common iliac artery aneurysms. Ann Vasc Surg. 2014;28:490.e5-490.e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Shu X, Li Z, Wang W, Li X. Endovascular treatment of bilateral common iliac artery aneurysms using bifurcated-unibody stent grafts. Ann Vasc Surg. 2014;28:1790.e5-1790.e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Lobato AC. Sandwich technique for aortoiliac aneurysms extending to the internal iliac artery or isolated common/internal iliac artery aneurysms: a new endovascular approach to preserve pelvic circulation. J Endovasc Ther. 2011;18:106-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 99] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 14. | Kang J, Chung BH, Hyun DH, Park YJ, Kim DI. Clinical outcomes after internal iliac artery embolization prior to endovascular aortic aneurysm repair. Int Angiol. 2020;39:323-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Yang M, Li L, Liu Y, Su Q, Dong Z, Li G, Jiang J, Ding X. Therapeutic management of isolated internal iliac artery aneurysms. J Vasc Surg. 2020;72:1968-1975. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |