Published online Apr 16, 2024. doi: 10.12998/wjcc.v12.i11.1954
Peer-review started: December 27, 2023
First decision: January 16, 2024
Revised: January 30, 2024
Accepted: March 19, 2024
Article in press: March 19, 2024
Published online: April 16, 2024
Processing time: 105 Days and 21.1 Hours
To retrospectively report the safety and efficacy of renal transcatheter arterial embolization for treating autosomal dominant polycystic kidney disease (ADPKD) patients with gross hematuria.
The purpose of this study is to retrospectively report the safety and efficacy of renal transcatheter arterial embolization for treating ADPKD patients with gross hematuria. Materials and methods: During the period from January 2018 to December 2019, renal transcatheter arterial embolization was carried out on 6 patients with polycystic kidneys and gross hematuria. Renal arteriography was performed first, and then we determined the location of the hemorrhage and performed embolization under digital subtraction angiography monitoring. Improvements in routine blood test results, routine urine test results, urine color and postoperative reactions were observed and analyzed. Results: Renal transcatheter arterial embolization was successfully conducted in 6 patients. The indices of 5 patients and the color of gross hematuria improved after surgery compared with before surgery. No severe complication reactions occurred.
For autosomal dominant polycystic kidney syndrome patients with gross hematuria, transcatheter arterial embolization was safe and effective.
Core Tip: In this manuscript, we report the retrospective analysis to evaluate efficiency and safety of transcatheter arterial embolization in autosomal dominant polycystic kidney patients with gross hematuria in the Chinese population and currently there is no relevant article published.
- Citation: Sui WF, Duan YX, Li JY, Shao WB, Fu JH. Safety and efficacy of transcatheter arterial embolization in autosomal dominant polycystic kidney patients with gross hematuria: Six case reports. World J Clin Cases 2024; 12(11): 1954-1959
- URL: https://www.wjgnet.com/2307-8960/full/v12/i11/1954.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i11.1954
Autosomal dominant polycystic kidney disease (ADPKD) is a genetic disorder caused by mutations in PKD1 and PKD2[1,2]. Its pathological characteristic is a bilateral progressive enlarged kidney filled with multiple renal cysts. With the development of disease, early renal dysfunction changes to end-stage renal disease (ESRD). ADPKD is also associated with external manifestations, such as hypertension, hepatic cysts, pain, infection and intracranial aneurysms[3].
Dialysis is recommended as the first-line renal replacement therapy in ESRD patients with ADPKD[4]. However, kidneys with cysts continue to enlarge during the dialysis period, leading to significant complications[5,6], including dyspnea, abdominal pain, lumbago and persistent hematuria. To treat these problems, nephrectomy and renal transplantation could be performed. However, its drawbacks, namely, high invasiveness, poor prognosis and relatively low efficacy, restrict its application[7,8].
Transcatheter renal artery embolization (renal TAE) is a minimally invasive therapeutic option that is used for relieving the symptoms and reducing kidney volume[9-11], and it is regarded as an alternative to surgery before renal transplantation. However, no previous studies have focused on the treatment of ADPKD patients with gross hematuria. The aim of this study was first to retrospectively assess the safety and efficacy of renal TAE in ADPKD patients with gross hematuria.
Assess the safety and efficacy of renal TAE in ADPKD patients with gross hematuria.
ADPKD patients with gross hematuria. The study population was composed of ADPKD patients who had undergone hemodialysis regularly at Zhenjiang First People’s Hospital. All patients underwent routine blood tests, routine urine tests and abdominal no-contrast computed tomography (CT) scans before and after renal TAE.
Kidneys with cysts continue to enlarge during the dialysis period, leading to significant complications, including dyspnea, abdominal pain, lumbago and persistent hematuria.
ADPKD is a genetic disorder caused by mutations in PKD1 and PKD2.
The pathological characteristic of ADPKD is a bilateral progressive enlarged kidney filled with multiple renal cysts.
All patients underwent routine blood tests and routine urine tests. All 6 patients who suffered from gross hematuria had ESRD. The hemoglobin and erythrocyte levels of all patients were obviously decreased. The levels of erythrocytes in the urine of the 2 included patients were obviously increased.
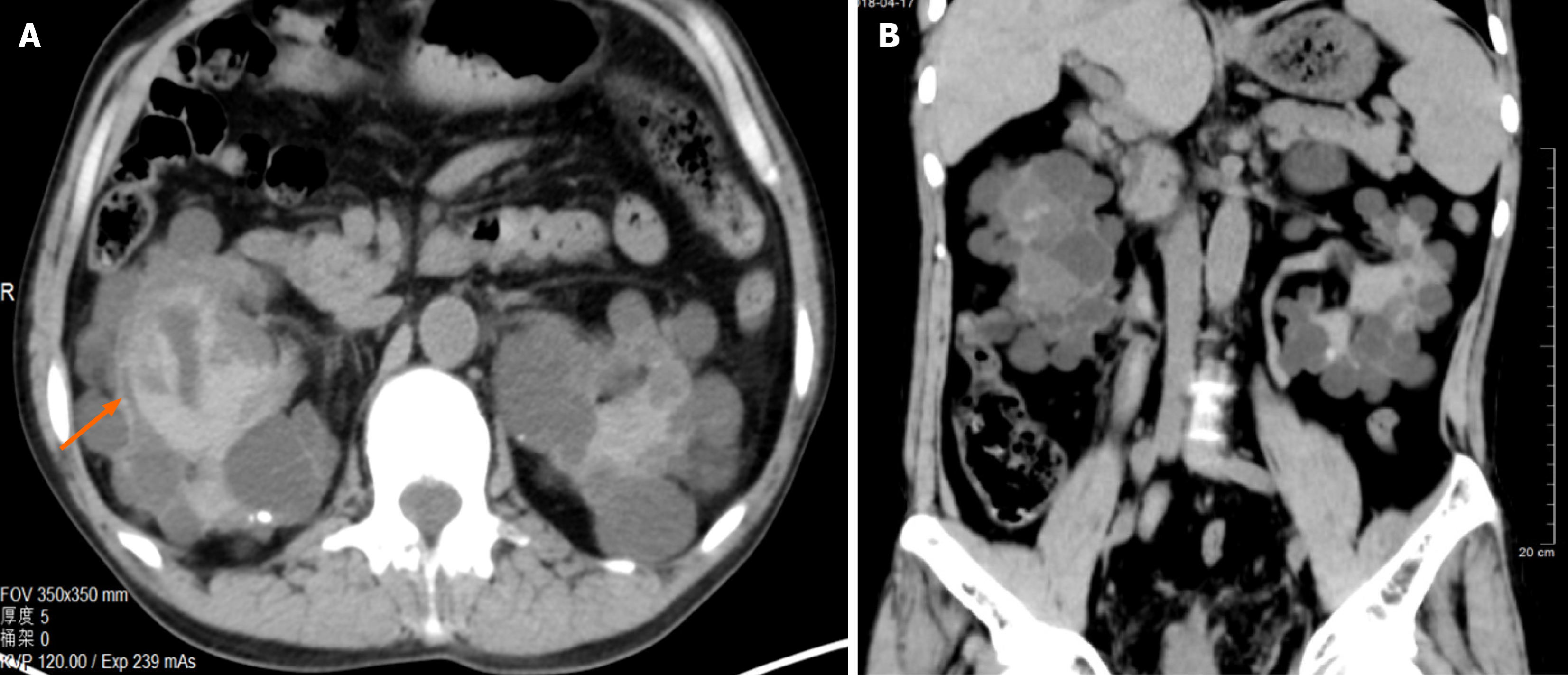
All patients underwent abdominal no-contrast CT scans. An abdominal no-contrast CT scan showed bilateral enlarged kidneys full of cysts of uniform size. Acute hemorrhage was found in the cysts (Figure 1).
Based on the laboratory and Imaging examinations. All 6 patients were diagnosed as ADPKD patients with gross hematuria.
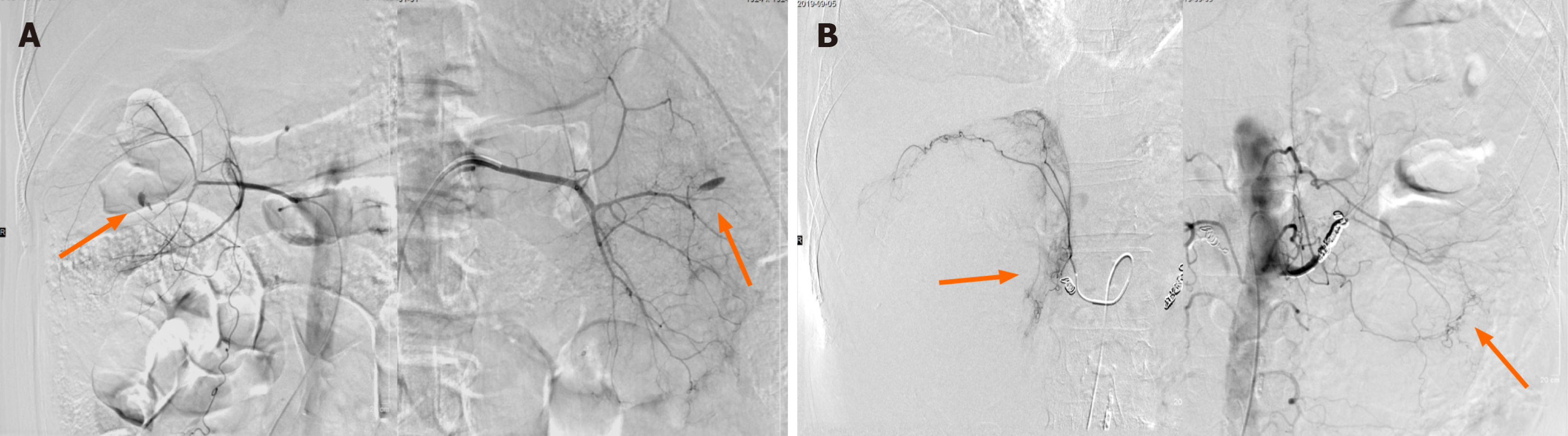
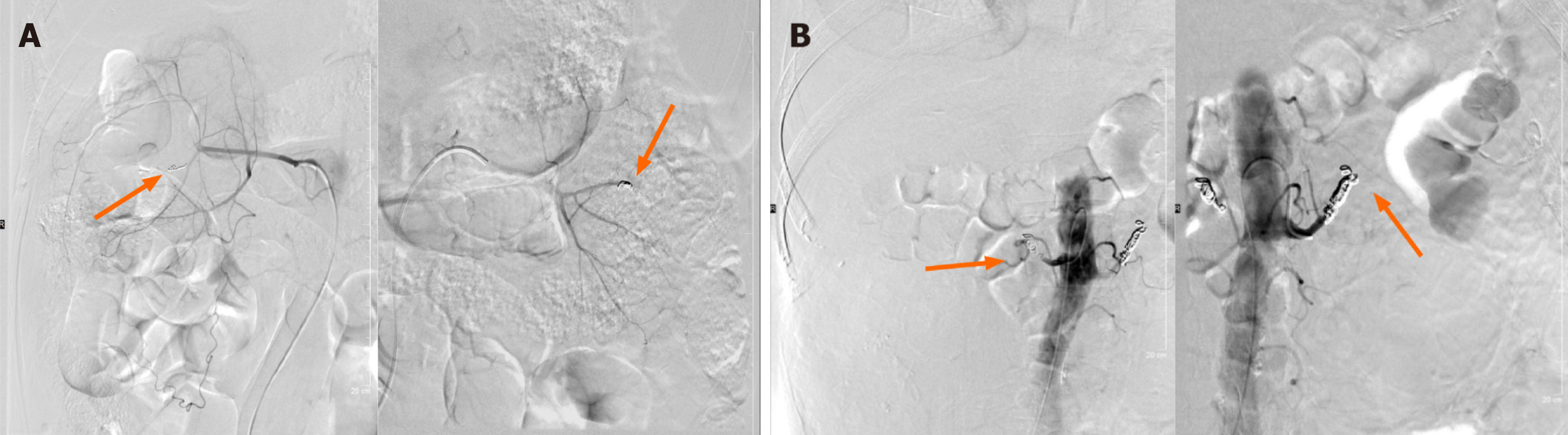
All 6 ADPKD patients underwent renal TAE successfully. Renal arteriography showed enlarged bilateral kidneys with thin arteries. Selective renal angiography revealed definite hemorrhagic positions in branches of the renal arteries (Figure 2A). For these patients, the branches of the renal vascular bed were embolized with microspheres from the gelatin sponge particle (GSP) in 3 patients (Figure 3A), and the bilateral main renal arteries and branches of the renal vascular bed were embolized with microcoils and microspheres from the GSP in 1 patient. Microcoils were found in the bilateral main renal arteries of 2 patients (Figure 2B). For these patients, embolization of branches of the renal vascular bed were performed with microspheres from the polyvinyl alcohol (PVA) or GSP, and embolization of the bilateral main renal arteries were performed again with microcoils (Figure 3B).
The 1st day after embolization, the gross hematuria in all 6 patients clearly faded. On the 3rd day after embolization, the erythrocyte levels in the urine of 2 patients decreased. Four patients refused routine urine tests. The hemoglobin and erythrocyte levels of all patients were increased (Table 1).
| Case | Sex | Age | Hemoglobin in blood in G/L | Erythrocyte in blood as 1012/L | Erythrocyte in urine as U/L | Embolic agents | Complications | |||
| Pre-operation | Post operation | Pre-operation | Post operation | Pre-operation | Post operation | |||||
| 1 | Male | 51 | 65 | 86 | 2.4 | 3.23 | / | Microspheres of GSP+ microcoils | Fever | |
| 2 | Male | 51 | 67 | 85 | 2.49 | 3.16 | / | Microspheres of GSP | Fever | |
| 3 | Female | 44 | 72 | 76 | 2.6 | 2.8 | / | Microspheres of GSP | Pain | |
| 4 | Male | 48 | 56 | 71 | 2.03 | 2.57 | / | Microspheres of GSP | Pain | |
| 5 | Male | 64 | 88 | 93 | 2.97 | 3.11 | 24376.2 | 8338 | Microspheres of GSP+ microcoils | Pain |
| 6 | Male | 64 | 73 | 81 | 2.56 | 2.73 | 42455.3 | 3855.5 | Microspheres of PVA+ microcoils | None |
No severe complications occurred from the beginning of embolization to discharge. Two included patients had fever (grade 1) without symptoms of shivering or chills. The highest temperature was 38.8 °C, and the temperature ultimately decreased to normal before discharge. Three patients had lumbago (grade 2), and the highest numerical rating scale was 4. Nonsteroidal anti-inflammatory drugs were used to relieve pain. No complications occurred in 1 patient.
Our results showed that renal TAE was safe and effective for ADPKD patients with gross hematuria. The color of the urine faded on the 1st day after embolization and did not recur during the duration of hospitalization. Five patients’ blood tests and routine urine test results improved on the 3rd day after embolization. No severe complications occurred in any of the patients. Fever and lumbago after embolization were grade 1-2 without the need for surgical, endoscopic, or radiologic interventions[12]. Ischemia, necrosis and swelling occur in organizations due to embolization of branches of the renal vascular bed; these conditions are called postembolization syndrome. Fever and lumbago are common complications after embolization in ADPKD patients with postembolization syndrome[13].
Gross hematuria is a common complication in ADPKD patients and can occur due to cyst bleeding, urinary tract infection or tumors[14,15]. Gross hematuria is limited and can be alleviated within 1 wk by using etamsylate. Moreover, renal TAE and nephrectomy are the recommended methods for treating this disease. Renal TAE has been gradually recognized in Asia as an option for patients with ADPKD who are not suitable for surgery[16,17]. Previous research confirmed that nephrectomy led to persistent hypotension and aggravated renal anemia[18], which may further increase the risk for ADPKD patients undergoing dialysis. However, renal TAE rather than surgery is not widely accepted in Western countries because of the higher rate of kidney transplantation in the West[11].
The materials and extent of embolization are considered significant factors for ensuring the safety and efficiency of renal TAE. Owing to the self-specifications of microcoils, which are common mechanical embolic materials, they are usually placed in main renal arteries to reduce the blood flow to the kidneys. Previous studies[19,20] have demonstrated that although microcoils lead to temporary vessel occlusion of renal arteries, later revascularization can lead to renal failure after surgery via microcoils alone. Renal TAE was also confirmed in 2 patients in our study. Since revascularization is the main cause of failure, embolization of the renal arterial bed by microspheres or liquid embolic materials is necessary[10,19,21].
With regard to embolization of the renal arterial bed, previous studies[12,19,21] confirmed that the use of liquid embolic materials (anhydrous alcohol) and microspheres of the PVA was safe and efficient. The use of microspheres from the PVA and GSP during embolization was also demonstrated to be effective in our study. Embolization of the renal arterial bed with anhydrous alcohol and microspheres could effectively restrain late revascularization through damaging endothelial tissue, coagulating proteins and inducing microvascular thrombosis and necrosis of perivascular areas[22]. In addition, serious complications linked to anhydrous alcohol and microspheres, such as ectopic embolism, were reported after renal TAE[23]. Such serious complications can be avoided by superselective arterial embolization and detection of nontarget arteries. Because anhydrous alcohol and microspheres are nonradiopaque embolic agents, we emulsified them with radiopaque material, such as contrast media, to monitor the direction of embolic agents. Previous research also suggested that nonradiopaque embolic agents could be mixed with iodized oil and that temporary balloon occlusion catheters could be placed in main renal arteries to prevent backflows of embolic agents[21].
For autosomal dominant polycystic kidney syndrome patients with gross hematuria, transcatheter arterial embolization was safe and effective.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Attur R, India S-Editor: Che XX L-Editor: Filipodia P-Editor: Guo X
| 1. | Gabow PA. Autosomal dominant polycystic kidney disease. N Engl J Med 1993; 329: 332-342 . [RCA] [DOI] [Full Text] [Cited by in Crossref: 721] [Cited by in RCA: 692] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 2. | Xu D, Ma Y, Gu X, Bian R, Lu Y, Xing X, Mei C. Novel Mutations in the PKD1 and PKD2 Genes of Chinese Patients with Autosomal Dominant Polycystic Kidney Disease. Kidney Blood Press Res. 2018;43:297-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Leonhard WN, Zandbergen M, Veraar K, van den Berg S, van der Weerd L, Breuning M, de Heer E, Peters DJ. Scattered Deletion of PKD1 in Kidneys Causes a Cystic Snowball Effect and Recapitulates Polycystic Kidney Disease. J Am Soc Nephrol. 2015;26:1322-1333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 56] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 4. | Li L, Szeto CC, Kwan BC, Chow KM, Leung CB, Kam-Tao Li P. Peritoneal dialysis as the first-line renal replacement therapy in patients with autosomal dominant polycystic kidney disease. Am J Kidney Dis. 2011;57:903-907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Torres VE, Harris PC, Pirson Y. Autosomal dominant polycystic kidney disease. Lancet. 2007;369:1287-1301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 957] [Cited by in RCA: 989] [Article Influence: 54.9] [Reference Citation Analysis (0)] |
| 6. | Yamakoshi S, Ubara Y, Suwabe T, Hiramatsu R, Yamanouchi M, Hayami N, Sumida K, Hasegawa E, Hoshino J, Sawa N, Takaichi K, Kawabata M. Transcatheter renal artery embolization improves lung function in patients with autosomal dominant polycystic kidney disease on hemodialysis. Clin Exp Nephrol. 2012;16:773-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Fuller TF, Brennan TV, Feng S, Kang SM, Stock PG, Freise CE. End stage polycystic kidney disease: indications and timing of native nephrectomy relative to kidney transplantation. J Urol. 2005;174:2284-2288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 68] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 8. | Lipke MC, Bargman V, Milgrom M, Sundaram CP. Limitations of laparoscopy for bilateral nephrectomy for autosomal dominant polycystic kidney disease. J Urol. 2007;177:627-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 59] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Suwabe T, Ubara Y, Sekine A, Ueno T, Yamanouchi M, Hayami N, Hoshino J, Kawada M, Hiramatsu R, Hasegawa E, Sawa N, Takaichi K. Effect of renal transcatheter arterial embolization on quality of life in patients with autosomal dominant polycystic kidney disease. Nephrol Dial Transplant. 2017;32:1176-1183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Suwabe T, Ubara Y, Mise K, Ueno T, Sumida K, Yamanouchi M, Hayami N, Hoshino J, Kawada M, Imafuku A, Hiramatsu R, Hasegawa E, Sawa N, Takaichi K. Suitability of Patients with Autosomal Dominant Polycystic Kidney Disease for Renal Transcatheter Arterial Embolization. J Am Soc Nephrol. 2016;27:2177-2187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Hoshino J, Suwabe T, Hayami N, Sumida K, Mise K, Kawada M, Imafuku A, Hiramatsu R, Yamanouchi M, Hasegawa E, Sawa N, Takei R, Takaichi K, Ubara Y. Survival after arterial embolization therapy in patients with polycystic kidney and liver disease. J Nephrol. 2015;28:369-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18532] [Cited by in RCA: 24728] [Article Influence: 1177.5] [Reference Citation Analysis (0)] |
| 13. | Cardella JF, Kundu S, Miller DL, Millward SF, Sacks D; Society of Interventional Radiology. Society of Interventional Radiology clinical practice guidelines. J Vasc Interv Radiol. 2009;20:S189-S191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 198] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 14. | Hooton T. Urinary tract infections in adults. Comprehensive Clinical Nephrology. 4th ed. Elsevier, 2010: 629-640. |
| 15. | Yao Q, Wu M, Zhou J, Zhou M, Chen D, Fu L, Bian R, Xing X, Sun L, Hu X, Li L, Dai B, Wüthrich RP, Ma Y, Mei CL. Treatment of Persistent Gross Hematuria with Tranexamic Acid in Autosomal Dominant Polycystic Kidney Disease. Kidney Blood Press Res. 2017;42:156-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Ubara Y, Tagami T, Sawa N, Katori H, Yokota M, Takemoto F, Inoue S, Kuzuhara K, Hara S, Yamada A. Renal contraction therapy for enlarged polycystic kidneys by transcatheter arterial embolization in hemodialysis patients. Am J Kidney Dis. 2002;39:571-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 63] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 17. | Park HC, Kim CW, Ro H, Moon JY, Oh KH, Kim Y, Lee JS, Yin YH, Jae HJ, Chung JW, Ahn C, Hwang YH. Transcatheter arterial embolization therapy for a massive polycystic liver in autosomal dominant polycystic kidney disease patients. J Korean Med Sci. 2009;24:57-61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Schwarz ER, Heintz B, Stefanidis I, vom Dahl J, Sieberth HG. The heterogeneous and delayed course of blood pressure normalization in hypertensive patients after bilateral nephrectomy with and without subsequent renal transplantation. Ren Fail. 2000;22:591-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 19. | Sakuhara Y, Kato F, Abo D, Hasegawa Y, Shimizu T, Terae S, Shirato H. Transcatheter arterial embolization with absolute ethanol injection for enlarged polycystic kidneys after failed metallic coil embolization. J Vasc Interv Radiol. 2008;19:267-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | Yamagami T, Kajiwara K, Yamanishi T, Minamiguchi H, Yoshimatsu R. Use of a micro-balloon catheter in transcatheter arterial embolization of the renal artery for recurrence of symptoms of autosomal dominant polycystic kidney disease. Acta Radiol Open. 2018;7:2058460118818849. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Sakuhara Y, Nishio S, Morita K, Abo D, Hasegawa Y, Yuasa N, Mochizuki T, Soyama T, Oba K, Shirato H, Kudo K. Transcatheter Arterial Embolization with Ethanol Injection in Symptomatic Patients with Enlarged Polycystic Kidneys. Radiology. 2015;277:277-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Kónya A, Van Pelt CS, Wright KC. Ethiodized oil-ethanol capillary embolization in rabbit kidneys: temporal histopathologic findings. Radiology. 2004;232:147-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Siniluoto TM, Hellström PA, Päivänsalo MJ, Leinonen AS. Testicular infarction following ethanol embolization of a renal neoplasm. Cardiovasc Intervent Radiol. 1988;11:162-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 0.5] [Reference Citation Analysis (0)] |