Published online Apr 16, 2024. doi: 10.12998/wjcc.v12.i11.1929
Peer-review started: December 11, 2023
First decision: January 25, 2024
Revised: January 31, 2024
Accepted: March 20, 2024
Article in press: March 20, 2024
Published online: April 16, 2024
Processing time: 122 Days and 4.8 Hours
Recently, a growing number of adolescents have been afflicted with mental disorders, with annual morbidity rates on the rise. This trend has been exacer
To investigate the impact of the COVID-19 pandemic on adolescent bipolar disorder (BD), along with the underlying factors contributing to heightened rates of suicide and self-harm among adolescents.
A comprehensive statistical analysis was conducted utilizing clinical interviews and self-reports obtained from patients or their guardians. Diagnostic criteria for BDs were based on the Diagnostic and statistical manual of mental disorders, international classification of diseases-11, and the National institute of mental health research domain criteria. Statistical analyses were performed using SPSS 26.0 software, with significance set at P < 0.05.
A cohort of 171 adolescents diagnosed with BD between January 1, 2018, and December 31, 2022, was included in the analysis. The gender distribution was 2.8:1 (female to male), with ages ranging from 11 to 18 years old. Major factors contributing to adolescent BDs included familial influences, academic stress, genetic predisposition and exposure to school-related violence. Notably, a significant increase in suicide attempts and self-harm incidents was observed among adolescents with BD during the COVID-19 pandemic. Statistical analysis indicated that the pandemic exacerbated familial discord and heightened academic stress, thereby amplifying the prevalence of suicidal behavior and self-harm among adolescents.
The COVID-19 pandemic has exacerbated familial tensions and intensified the incidence of suicide and self-harm among adolescents diagnosed with BD. This study underscores the urgent need for societal, familial and educational support systems to prioritize the well-being of adolescents and offers valuable insights and guidelines for the prevention, diagnosis and treatment of adolescent BDs.
Core Tip: More adolescents have suffered from bipolar disorder (BD) since the coronavirus disease 2019 (COVID-19) pandemic outbreak. A total of 171 adolescents with BD were recruited and analyzed from January 1, 2018 to December 31, 2022. Family-related factors and academic stress played significant roles in emergence and exacerbation of adolescent BDs. The COVID-19 pandemic exacerbated family relationships and greatly increased the occurrence of suicide and self-harm among adolescents with BD. This study aimed to focus the attention of society, families and schools to increase care about adolescents and also provide guidance and references for the prevention, diagnosis and treatment of adolescent BDs.
- Citation: Ye ZF, Hong YH, Yang JL, Tan MQ, Xie JM, Xu ZC. COVID-19 pandemic amplified mortality rates among adolescents with bipolar disorder through family-related factors. World J Clin Cases 2024; 12(11): 1929-1935
- URL: https://www.wjgnet.com/2307-8960/full/v12/i11/1929.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i11.1929
Bipolar disorder (BD), also known as manic-depressive illness, is a profoundly severe and complex chronic mental disorder characterized by recurrent episodes of significant emotional fluctuation. It manifests in extreme highs and lows in mood, along with altered behavior, cognition, sleep patterns and energy levels[1]. Clinically, BD presents with cognitive impairments, socio-psychological disturbances and persistent manic-depressive mood oscillations[2]. The precise etiology of BD remains elusive, posing ongoing challenges in the identification of consistent and reliable biomarkers for its diagnosis, understanding of its pathogenesis, neurobiology and treatment strategies[3].
BD ranks as a leading cause of disability worldwide, impacting at least 1% of the global population[4,5]. It affects approximately 40 million people, with an age-standardized prevalence of 489.8 per 100000 individuals[6]. The 20-year post-diagnosis mortality rate for BD patients exceeds 6%, which is more than 20 times higher than that of the general population[1]. Notably, about one-third to one-half of individuals with BD engage in suicidal behaviors, with up to 20% of these attempts successful[7].
The current authors research is focused on adolescents diagnosed with BD in Huangshi. Findings underscore a significant correlation between the coronavirus disease 2019 (COVID-19) pandemic and increased familial stress, which in turn has contributed to a rise in BD cases among such adolescents. Statistical analysis established a clear connection between the COVID-19 pandemic and a heightened incidence of suicidal and self-harm behaviors in adolescents suffering from BDs, predominantly influenced by family-related factors.
A total of 171 mentally disordered adolescents aged ≤ 18 years were recruited from January 1, 2018 to December 31, 2022.
The diagnosis of BD was established following the criteria described in the Diagnostic and statistical manual of mental disorders, International classification of diseases-11 and the National Institute of Mental Health Research Domain Criteria[8,9]. Participants included in the study were individuals under 18 years of age who met these diagnostic standards and had comprehensive medical records. Exclusion criteria encompassed absence of a BD diagnosis, incomplete data, or failure to fulfill the established diagnostic guidelines.
The assessment of factors contributing to BD, along with associated abnormal illness behaviors such as suicide or suicide attempts (M8) and self-harm (M9), was based on insights from previous studies[10,11]. These factors included family-related and genetic factors, school violence and academic pressure.
Data were statistically processed and analysed using SPSS version 26.0. Statistical significance was set at P < 0.05.
The monthly incidence of cases was compared before and during the COVID-19 pandemic employing the Mann-Whitney U test.
Binary logistic regression analysis (Forward LR method) was utilized to evaluate the impact of variables including the COVID-19 pandemic, family-related factors, academic stress and school violence on suicide and self-harm behaviors. A P-value larger than 0.10 indicated a lack of significant impact, leading to exclusion of the variable, while a P-value ≤ 0.05 signified a significant effect, warranting inclusion of the variable. The 95%CI for both P-values and odds ratios (OR) were also calculated.
Univariate logistic regression was employed to explore the relationship between the COVID-19 pandemic and the statistically significant influencing factors identified. Calculation of 95%CIs and ORs helped generate a comprehensive understanding of the relationships and impacts studied.
This study included 171 adolescents diagnosed with BD. Figure 1A illustrates the temporal distribution of these BD cases. Figure 1B highlights a marked contrast in the incidence of BD cases between the pre-pandemic and during-pandemic periods, broken down by month.
Of the 171 adolescents with BD, 126 were female and 45 were male, resulting in a gender ratio of approximately 2.8:1, as depicted in Figure 1C. The age at onset varied from 11 to 18 years, with an average age of 15.54 ± 1.62 years. The peak incidence was observed in 16-year-olds, as shown in Figure 1C.
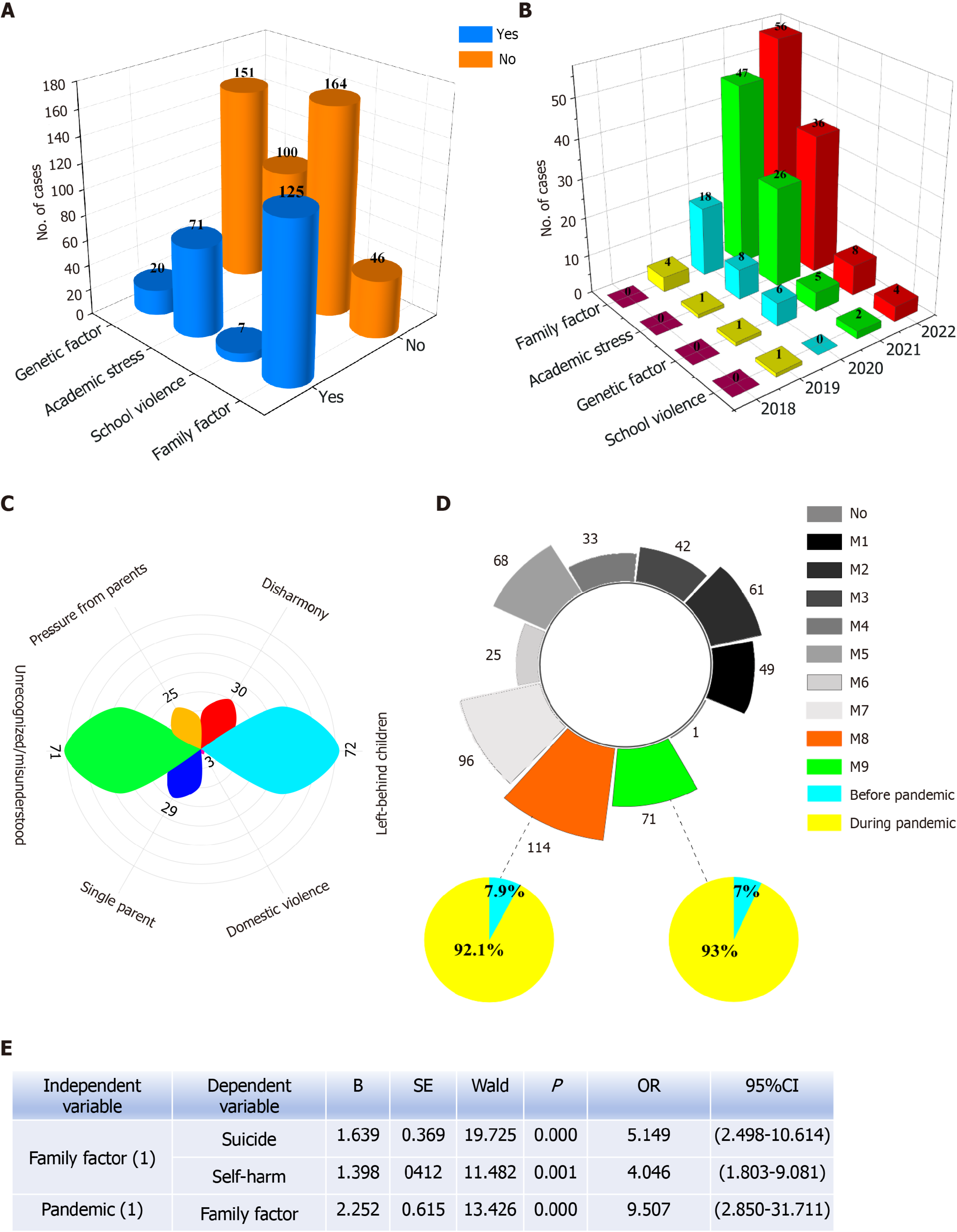
A significant proportion of the BD patients surveyed (125 out of 171, or 73.1%) identified family-related issues as a contributing factor to their disorder, as demonstrated in Figure 2A. Academic stress was reported as the second most prevalent cause, affecting 41.52% (71 patients). Genetic predisposition (20 patients, 13.25%) and experiences of school violence (7 patients, 4.27%) were also identified as influential factors in the development of BD, as detailed in Figure 2A.
When examining the distribution of BD cases in relation to potential contributing factors over the years, family-related factors and academic stress emerged as the predominant causes for the onset and aggravation of BD. An annual increase in the number of BD cases attributed to these factors was observed. Nonetheless, the roles of genetic predisposition and school violence in the development of BD should also be recognized, as depicted in Figure 2B.
Within the spectrum of family-related factors, being a 'left-behind' child was identified as a significant contributor in 57.6% of the cases (125 patients), and feeling unrecognized or misunderstood by family members was reported in 56.8% of these cases. Such findings highlight the major impact of family dynamics on adolescent BD, as shown in Figure 2C.
Abnormal illness behaviors encompass a spectrum of detrimental clinical manifestations arising from mental disorders, with the gravest instances exhibited as suicide and/or suicide attempts (M8), as well as self-harm (M9). Among the 171 cases of BD, 114 individuals reported experiencing suicidal ideation and/or making suicide attempts, while 71 patients engaged in self-harming behaviors, constituting 66.67% and 41.52% of patients, respectively (Figure 2D). Data analysis suggests the upsurge in suicide attempts and self-harm to the repercussions of the COVID-19 pandemic (Figure 2D).
Binary logistic regression analysis (Forward LR) revealed that family-related factors exerted a significant influence on suicide (P < 0.001, OR = 5.149, 95%CI: 2.498-10.614) and self-harm (P < 0.001, OR = 4.046, 95%CI: 1.803-9.081), whereas academic stress and school violence did not demonstrate statistical significance in their impact and were consequently excluded as causal factors. Subsequent univariate logistic regression analysis revealed a statistically significant effect of the COVID-19 pandemic on family-related factors (P < 0.001, OR = 9.507, 95%CI: 2.850-31.711) (Figure 2E).
This study included 171 BD patients, with a higher prevalence among females than males, possibly due to emotional sensitivity and hormonal fluctuations. Age analysis revealed a peak in patient numbers at 16 years, coinciding with the high school entrance examinations. The onset age predominantly ranged from 13 to 17 years in the studied cohort, with a significant number of patients being high school students, underscoring the strong link between academic pressure and BD onset.
BD incidence was linked to multiple factors, including familial dynamics, genetic predispositions, school bullying and academic stress. Academic pressure and family-related factors were significantly associated with BD in adolescents. A notable number of patients had familial ties, especially those who were either left-behind children or felt unrecognized and misunderstood by their families.
The prevalence of suicide and self-harm among adolescents escalated during the COVID-19 pandemic. A marked increase in the incidence of suicides and/or suicide attempts (M8) and self-harm (M9) was observed between the pre-pandemic and pandemic periods. Logistic regression analysis substantiated the profound impact of the COVID-19 pandemic on the rise in suicide and self-harm rates among adolescents with BD, primarily due to family-related stressors.
The COVID-19 pandemic has heightened BD morbidity in adolescents, with statistical analysis highlighting a robust association between pandemic-related family stressors and increased rates of suicide and self-harm in this group. Furthermore, the COVID-19 pandemic likely exacerbated family-related factors through enforced isolation and other restrictive measures.
Recently, there has been an alarming escalation in mental health disorders among adolescents, with annual incidence rates steadily increasing. The onset of the coronavirus disease 2019 (COVID-19) pandemic has particularly seen a surge in cases of bipolar disorder (BD) among this demographic.
This study aimed to examine trends in BD prevalence among adolescents before and during the COVID-19 pandemic. It investigates the escalation in abnormal mental health behaviors and identifies potential risk factors, such as family factors and academic pressures.
The primary goal of this research is to assess the impact of the COVID-19 pandemic on the incidence of BD in adolescents. It also seeks to understand the factors contributing to the increased rates of suicide and self-harm within this group.
For this study, data collection was conducted through clinical observations. The diagnosis of BD was based on the criteria given in the Diagnostic and statistical manual of mental disorders, international classification of diseases-11 and the National Institute of Mental Health’s Research Domain Criteria.
The study revealed that family-related factors and academic stress are pivotal in the onset and intensification of BDs in adolescents. The COVID-19 pandemic has further strained familial relationships and led to a significant increase in suicide and self-harm incidents among adolescents diagnosed with BD.
The study suggests that the rise in suicide and self-harm rates among adolescents with BD may be more closely linked to family-related factors than to the COVID-19 pandemic itself. However, the pandemic has potentially aggravated the family-related factors through enforced social isolation and other restrictive measures.
The study highlights that social isolation, a preventative measure during a pandemic, is closely associated with challenging household dynamics. Understanding the interplay between family factors and a pandemic is crucial for developing strategies to prevent adverse behaviors in adolescents with BD. Future research, including prospective randomized trials, is required to further elucidate this relationship.
Thanks to all the participants in this study for their kind support and coordination.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Stoyanov D, Bulgaria S-Editor: Liu H L-Editor: A P-Editor: Guo X
| 1. | Anderson IM, Haddad PM, Scott J. Bipolar disorder. BMJ. 2012;345:e8508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 152] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 2. | Harrison PJ, Geddes JR, Tunbridge EM. The Emerging Neurobiology of Bipolar Disorder. Trends Neurosci. 2018;41:18-30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 146] [Cited by in RCA: 146] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 3. | Ching CRK, Hibar DP, Gurholt TP, Nunes A, Thomopoulos SI, Abé C, Agartz I, Brouwer RM, Cannon DM, de Zwarte SMC, Eyler LT, Favre P, Hajek T, Haukvik UK, Houenou J, Landén M, Lett TA, McDonald C, Nabulsi L, Patel Y, Pauling ME, Paus T, Radua J, Soeiro-de-Souza MG, Tronchin G, van Haren NEM, Vieta E, Walter H, Zeng LL, Alda M, Almeida J, Alnaes D, Alonso-Lana S, Altimus C, Bauer M, Baune BT, Bearden CE, Bellani M, Benedetti F, Berk M, Bilderbeck AC, Blumberg HP, Bøen E, Bollettini I, Del Mar Bonnin C, Brambilla P, Canales-Rodríguez EJ, Caseras X, Dandash O, Dannlowski U, Delvecchio G, Díaz-Zuluaga AM, Dima D, Duchesnay É, Elvsåshagen T, Fears SC, Frangou S, Fullerton JM, Glahn DC, Goikolea JM, Green MJ, Grotegerd D, Gruber O, Haarman BCM, Henry C, Howells FM, Ives-Deliperi V, Jansen A, Kircher TTJ, Knöchel C, Kramer B, Lafer B, López-Jaramillo C, Machado-Vieira R, MacIntosh BJ, Melloni EMT, Mitchell PB, Nenadic I, Nery F, Nugent AC, Oertel V, Ophoff RA, Ota M, Overs BJ, Pham DL, Phillips ML, Pineda-Zapata JA, Poletti S, Polosan M, Pomarol-Clotet E, Pouchon A, Quidé Y, Rive MM, Roberts G, Ruhe HG, Salvador R, Sarró S, Satterthwaite TD, Schene AH, Sim K, Soares JC, Stäblein M, Stein DJ, Tamnes CK, Thomaidis GV, Upegui CV, Veltman DJ, Wessa M, Westlye LT, Whalley HC, Wolf DH, Wu MJ, Yatham LN, Zarate CA, Thompson PM, Andreassen OA; ENIGMA Bipolar Disorder Working Group. What we learn about bipolar disorder from large-scale neuroimaging: Findings and future directions from the ENIGMA Bipolar Disorder Working Group. Hum Brain Mapp. 2022;43:56-82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 93] [Article Influence: 31.0] [Reference Citation Analysis (0)] |
| 4. | Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, Petukhova M, Kessler RC. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch Gen Psychiatry. 2007;64:543-552. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1830] [Cited by in RCA: 1609] [Article Influence: 89.4] [Reference Citation Analysis (0)] |
| 5. | Merikangas KR, Jin R, He JP, Kessler RC, Lee S, Sampson NA, Viana MC, Andrade LH, Hu C, Karam EG, Ladea M, Medina-Mora ME, Ono Y, Posada-Villa J, Sagar R, Wells JE, Zarkov Z. Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Arch Gen Psychiatry. 2011;68:241-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1693] [Cited by in RCA: 1750] [Article Influence: 125.0] [Reference Citation Analysis (0)] |
| 6. | GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9:137-150. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 436] [Cited by in RCA: 2697] [Article Influence: 899.0] [Reference Citation Analysis (0)] |
| 7. | Bipolar disorders. Nat Rev Dis Primers. 2018;4:18009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 8. | Di Vincenzo M. New research on validity and clinical utility of ICD-11 vs. ICD-10 and DSM-5 diagnostic categories. World Psychiatry. 2023;22:171-172. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Clark LA, Cuthbert B, Lewis-Fernández R, Narrow WE, Reed GM. Three Approaches to Understanding and Classifying Mental Disorder: ICD-11, DSM-5, and the National Institute of Mental Health's Research Domain Criteria (RDoC). Psychol Sci Public Interest. 2017;18:72-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 280] [Cited by in RCA: 333] [Article Influence: 41.6] [Reference Citation Analysis (0)] |
| 10. | Xie J, Yan Y, Hong Y, Yang J, Bai M, Xia W, Zhang X. Descriptive and associated risk factors analysis of mental disorders among adolescents in Huangshi, China. Asian J Psychiatr. 2023;79:103405. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 11. | Zhang X, Yan Y, Ye Z, Xie J. Descriptive analysis of depression among adolescents in Huangshi, China. BMC Psychiatry. 2023;23:176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |