Published online Apr 16, 2024. doi: 10.12998/wjcc.v12.i11.1875
Peer-review started: February 9, 2024
First decision: March 2, 2024
Revised: March 5, 2024
Accepted: March 22, 2024
Article in press: March 22, 2024
Published online: April 16, 2024
Processing time: 62 Days and 4.1 Hours
In this editorial we comment on the article published in a recent issue of the World Journal of Clinical Cases. This article described a novel ultrasound-guided lateral recess block approach in treating a patient with lateral recess stenosis. The impact of spinal pain-related disability extends significantly, causing substantial human suffering and medical costs. Each county has its preferred treatment strategies for spinal pain. Here, we explore the lower back pain (LBP) treatment algorithm re
Core Tip: The treatment algorithm for low back pain in France, recommended by the French National Authority for Health, prioritizes early patient activity and minimal medication use. While it promotes daily function and non-pharmacological therapies for chronic cases, it may not adequately address acute pain, relying heavily on caudal epidural steroid injections. The fixed follow-up timeline may also hinder exploring alternative therapies for non-responsive or intensely painful cases. Despite these limitations, understanding the strengths and weaknesses of this approach could inform global adaptations, potentially improving patient outcomes and satisfaction across diverse healthcare systems.
- Citation: Boyer LE, Boudier-Revéret M, Chang MC. Protocol for lower back pain management: Insights from the French healthcare system. World J Clin Cases 2024; 12(11): 1875-1880
- URL: https://www.wjgnet.com/2307-8960/full/v12/i11/1875.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i11.1875
In this editorial we comment on the article “Novel approach of ultrasound-guided lateral recess block for a patient with lateral recess stenosis: A case report” published in a recent issue of the World Journal of Clinical Cases[1]. This article described a novel ultrasound-guided lateral recess block approach in treating a patient with lateral recess stenosis. The impact of spinal pain-related disability extends significantly, causing substantial human suffering and medical costs. Each county has its preferred treatment strategies for spinal pain.
Lower back pain (LBP) is one of the most common musculoskeletal disorders. More than 80% of the population experience LBP at some point in their lives, and 10%-20%-up to 40% in some reports-of acute LBP cases become chronic[2]. Thus, treating LBP is crucial; several treatment approaches have been implemented in clinical settings, with ongoing research on effective treatment approach strategies. Treatment approaches for LBP may vary globally due to differences in healthcare systems and the general perception of various treatments in each country.
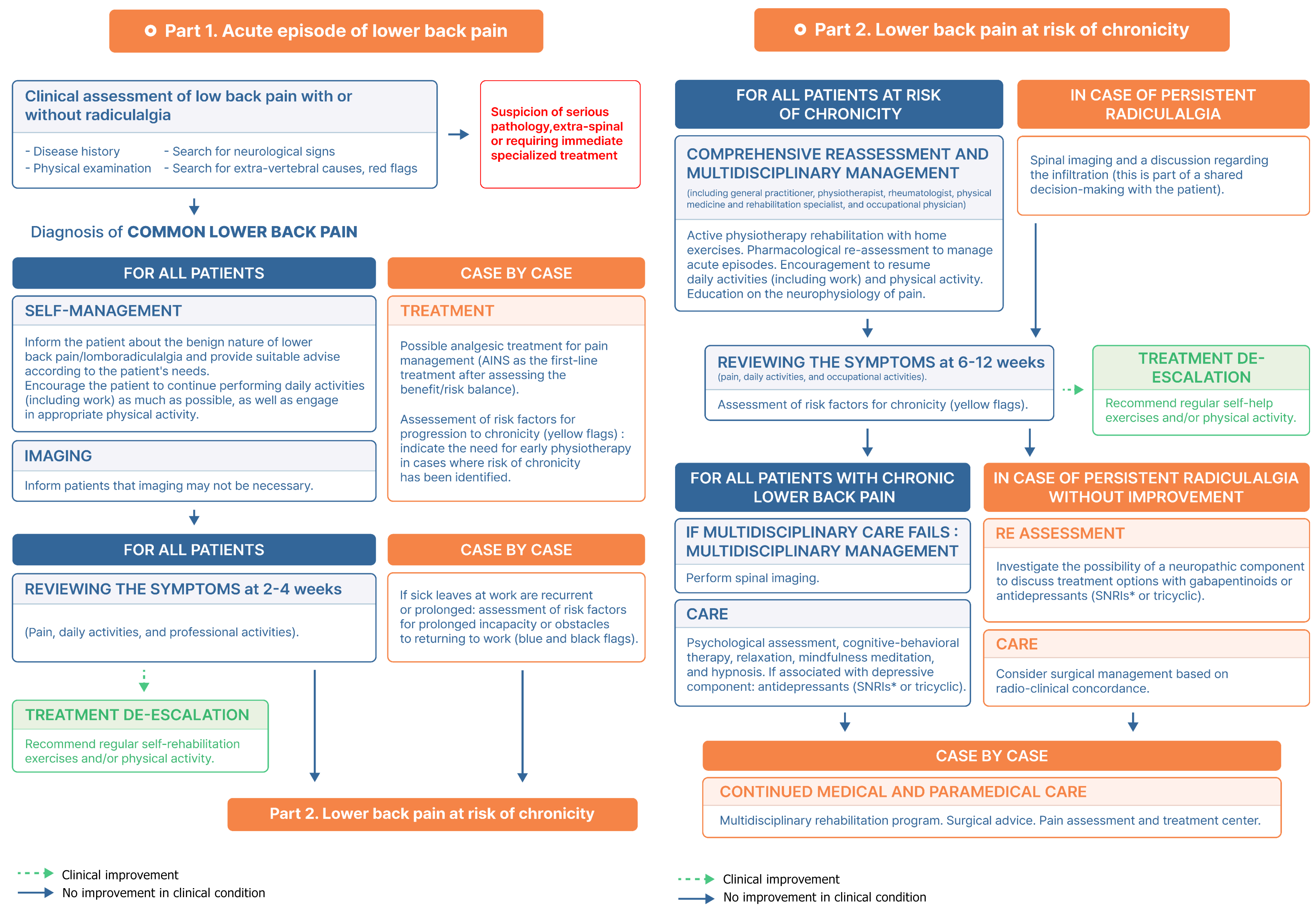
Here, we will explore the LBP treatment algorithm recommended in France. In France, the French National Authority for Health (Haute Autorité de santé) was established in August 2004 and has since been responsible for setting patient care guidelines and improving the quality of healthcare in France. We will examine the LBP treatment algorithm by this agency edited in 2017 and 2019 (Figure 1)[3].
The treatment algorithm recommended for patients with LBP in France can be summarized as follows: Patients visiting a clinic or hospital for LBP are encouraged to continue their daily activities as much as possible and are advised to engage in appropriate physical activity. Depending on the patient’s needs, pain management medications, such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs), may be prescribed for less than a week.
At the first visit, patients are informed that radiological evaluation is not always necessary, and clinicians do not conduct it.
Red flags are ruled out at each step to eliminate acute pathologies necessitating further specialized assessments and imaging (Figure 1).
A follow-up is conducted 2-4 wk after the initial visit. If pain persists, exercise and physiotherapy are recommended and prescribed. In addition, pharmacotherapy is considered for pain control. Yellow flags, factors of chronicization, are assessed (Figure 1). If radicular pain is present, a radiological evaluation is performed, and epidural caudal injection may be considered.
Another follow-up occurs 6-12 wk later. If pain persists, spinal imaging tests are conducted and a multidisciplinary approach is implemented, as well as addressing blue flags to assess the barriers to return to work (Figure 1). The family doctor can refer to a specialist or a pluridisciplinary center for back rehabilitation can be considered. This approach can include a psychological assessment, nutritionist, cognitive-behavioral therapy, relaxation techniques, mindfulness, and hypnosis. If depressive symptoms are present, the use of antidepressants is considered. For patients with radicular pain, gabapentinoids or antidepressants [serotonin norepinephrine reuptake inhibitors (SNIRs) or tricyclics] may be considered, as well as stepping up with infiltrations. If necessary, symptoms are evaluated in correlation with radiological images; surgery may be considered.
There are several positive aspects of this treatment algorithm. First, it encourages patients to continue their daily activities. Most clinicians are aware that patients with LBP should not necessarily be on bedrest and that they may continue with their daily lives without straining too much; however, they may not explain this to the patients unless asked. Therefore, making this a clear part of the treatment protocol would ensure clinicians consistently inform patients about the safety and benefits of maintaining normal activities.
Second, the algorithm is designed to limit the excessive use of oral medications and spinal injections. It recommends NSAIDs at the first visit only when necessary; spinal injections are considered only after an initial period if required. These measures help minimize potential drug side effects and complications of spinal injection, thus encouraging natural healing processes. Moreover, such measures may lead to reduced medical costs.
Third, for chronic cases, the algorithm recommends performing psychological assessments and using antidepressants when necessary, allowing for the treatment of depression that is common in many patients with chronic LBP. By suggesting treatments such as cognitive-behavioral therapy, relaxation, mindfulness, and hypnosis, the algorithm not only addresses the emotional aspects of chronic pain, but also helps to decrease dependency on drugs and injections. Additionally, the use of gabapentinoids or antidepressants (SNIRs or tricyclics) is recommended only for chronic pain with radicular symptoms, which can reduce the incidence of side effects associated with these medications.
While the treatment algorithm for LBP in France has these advantages, there are also some keys disadvantages to be considered.
First, it may not address the patient’s pain aggressively enough in the early stages. This approach overlooks the acute discomfort caused by LBP, and the resulting impact on daily life and work. In cases of severe pain, a more proactive use of medications or spinal injections early on could alleviate suffering, while earlier imaging could allow for more proactive treatments, such as spinal injections, in cases of significant herniated lumbar discs, thus reducing patient suffering[4]. Early aggressive treatment could prevent the pain from becoming chronic; treatment success rates are typically lower once pain becomes chronic[5].
Second, recommended infiltrations are predominantly caudal epidural steroid injection in cases of radiculalgia. Other injection procedures are not recommended and not usually conducted in clinical settings in France. Current recommendations do not endorse transforaminal or interlaminar epidural steroid injections due to concerns over side effects. However, we think that caudal epidural steroid injection is limited in that it cannot deliver injectates selectively to the lesion site. For caudal epidural steroid injection, 20-25 mL of a mixed solution with steroids, anesthetic, and saline is injected through the sacral hiatus into the lumbosacral epidural space[6]. Because the total amount of steroid in mixed solution is only 1-2 mL, it is significantly diluted. Therefore, only a small portion of the injected steroid reaches the target lesion. Third, the follow-up timeline is not flexible. In situations where the patient does not respond to the treatment recommended by clinicians and suffers from intense pain, it would be desirable for patients to seek medical attention earlier to explore alternative treatments.
Each country has its preferred treatment strategies for LBP; these approaches are bound to differ depending on the country’s healthcare system and culture. By considering the strengths and weaknesses of the French treatment algorithm, LBP treatment strategies in other countries or healthcare facilities could be adapted to enhance patient outcomes and satisfaction.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kelleni MT, Egypt S-Editor: Zheng XM L-Editor: A P-Editor: Yu HG
| 1. | Yang J, Li XL, Li QB. Novel approach of ultrasound-guided lateral recess block for a patient with lateral recess stenosis: A case report. World J Clin Cases. 2024;12:1010-1017. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Park KS, Kim S, Seo JY, Cho H, Lee JY, Lee YJ, Lee J, Kim MJ, Choi YE, Yang CS, Han CH, Ha IH. Effectiveness and Safety of Pharmacopuncture Therapy for Chronic Low Back Pain: A Protocol for a Pragmatic Randomized Controlled Trial. J Pain Res. 2022;15:2629-2639. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 3. | Haute Autorité de Santé. Prise en charge du patient présentant une lombalgie commune. 2019. Available from: https://www.has-sante.fr/jcms/c_2961499/fr/prise-en-charge-du-patient-presentant-une-lombalgie-commune. |
| 4. | Lee JH, Chang MC. Some suggestions for pain physicians working in real-world clinical settings. J Yeungnam Med Sci. 2023;40:S123-S124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Chang MC. Conservative Treatments Frequently Used for Chronic Pain Patients in Clinical Practice: A Literature Review. Cureus. 2020;12:e9934. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Kim KM, Kim HS, Choi KH, Ahn WS. Cephalic spreading levels after volumetric caudal epidural injections in chronic low back pain. J Korean Med Sci. 2001;16:193-197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |