Published online Mar 26, 2023. doi: 10.12998/wjcc.v11.i9.2009
Peer-review started: November 12, 2022
First decision: January 30, 2023
Revised: February 1, 2023
Accepted: March 3, 2023
Article in press: March 3, 2023
Published online: March 26, 2023
Processing time: 124 Days and 17 Hours
Cerebral ischemic stroke is attributed to paradoxical cerebral embolism. Pulmonary arteriovenous fistula (PAVF) is a rare potential cause of cerebral ischemic stroke, and cerebral ischemic stroke induced by PAVF in children is rare.
We report a case of right PAVF that presented as a transient ischemic attack (TIA) in a 13-year-old boy. The patient underwent embolization therapy and remained clinically stable for 2 years after treatment.
TIA induced by PAVF in children is rare, lacks typical clinical manifestations, and should not be ignored.
Core Tip: Pulmonary arteriovenous fistula (PAVF) is a rare potential cause of cerebral ischemic stroke. Children with PAVF have atypical clinical presentations, and even present with cerebral ischemic stroke or transient ischemic attack as the only clinical finding. If a PAVF is suspected, we recommend that appropriate examinations should be performed for early detection, and then active treatment and follow-up should be offered.
- Citation: Zheng J, Wu QY, Zeng X, Zhang DF. Transient ischemic attack induced by pulmonary arteriovenous fistula in a child: A case report. World J Clin Cases 2023; 11(9): 2009-2014
- URL: https://www.wjgnet.com/2307-8960/full/v11/i9/2009.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i9.2009
Cases of cerebral ischemic stroke induced by pulmonary arteriovenous fistula (PAVF) are mostly reported in adults, and are largely attributed to paradoxical cerebral embolism (PCE)[1-5]. Due to congenital or acquired arteriovenous communications, PCE can be caused by emboli transferring from a vein to an artery, or transferring from the right heart system to the left heart system. PCE is most commonly induced via a patent foramen ovale (PFO)[6], and PAVF is a rare potential cause. Cerebral ischemic stroke induced by PAVF in children is rare. We report the case of a 13-year-old boy with a transient ischemic attack (TIA) induced via PAVF. We aim to bring attention to this rare cause of PCE with the goal of decreasing the rate of missed diagnosis.
A 13-year-old boy was admitted to our hospital on September 2, 2020 due to intermittent dizziness for 2 d.
The patient presented with intermittent dizziness and bilateral limb weakness for 2 d. During the attack, he fainted and then recovered spontaneously approximately 5 min later. He had no dyspnea, nausea, vomiting, tinnitus, hearing loss, or convulsions.
The patient had a no previous medical history.
The patient had no relevant personal or family history.
Physical examination showed no neurological or cardiorespiratory abnormalities. His vital signs were stable.
The results of laboratory examinations were normal.
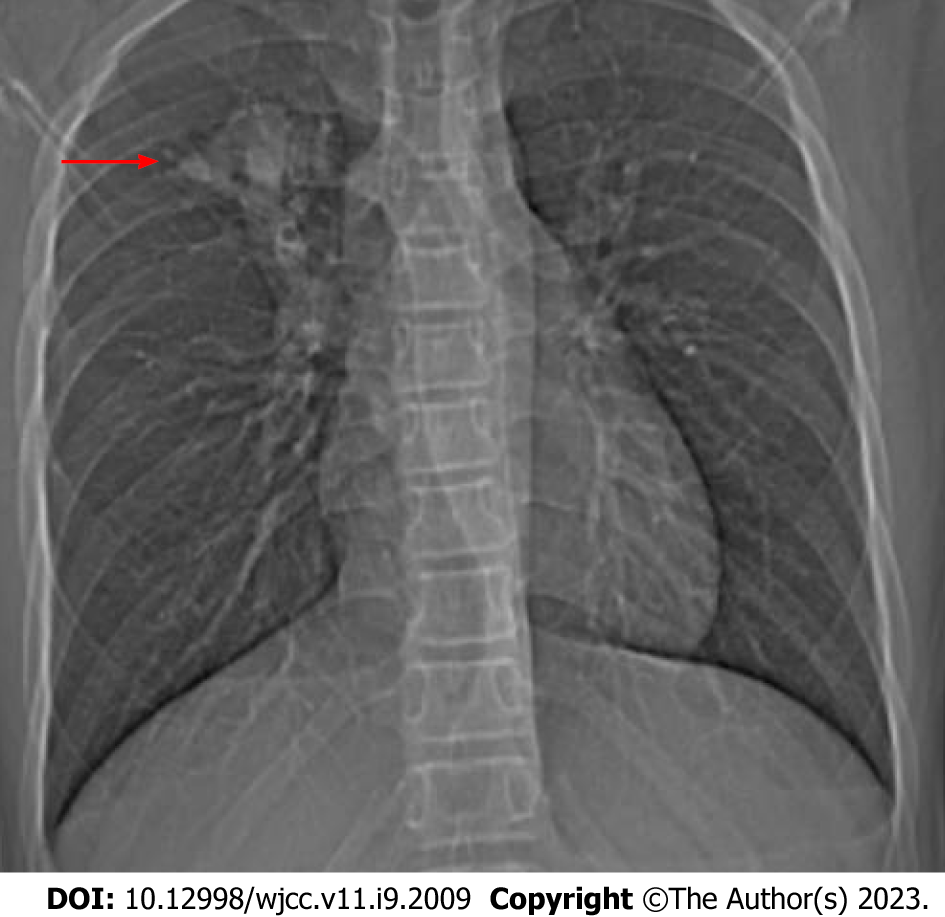
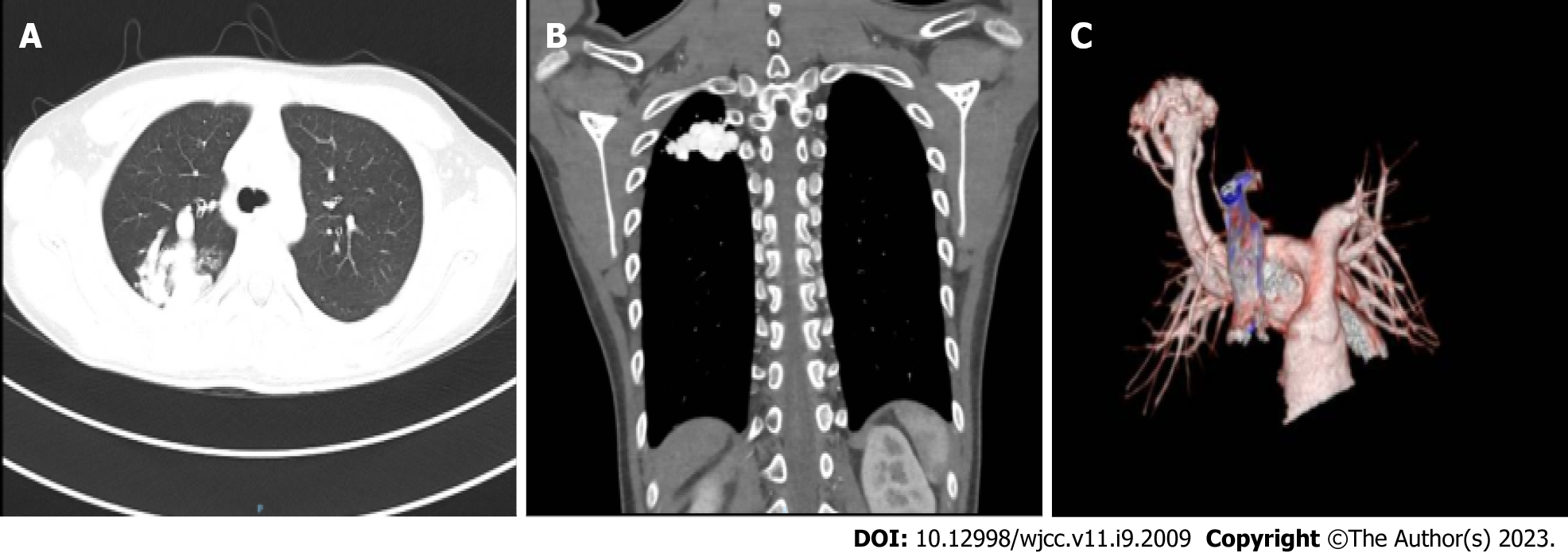
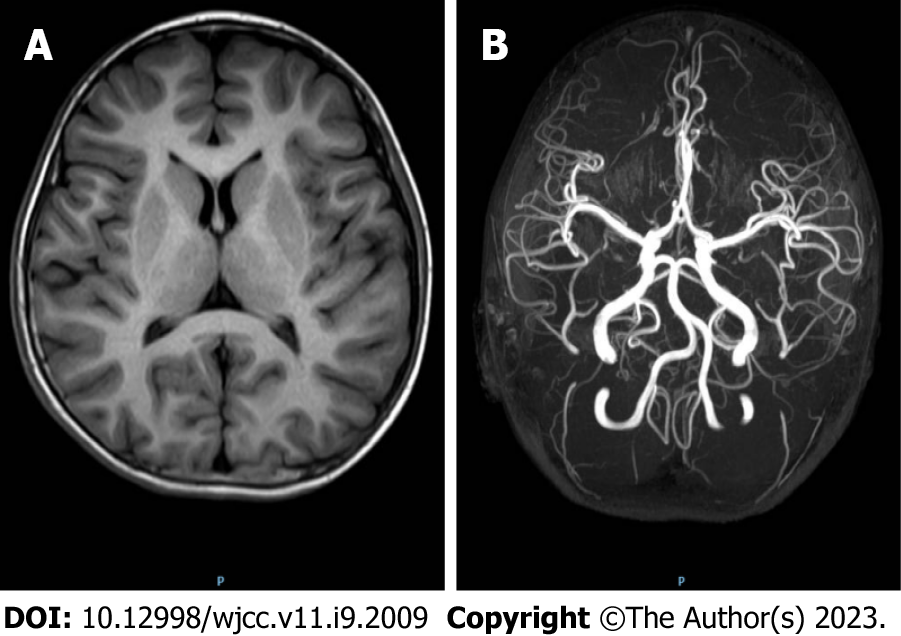
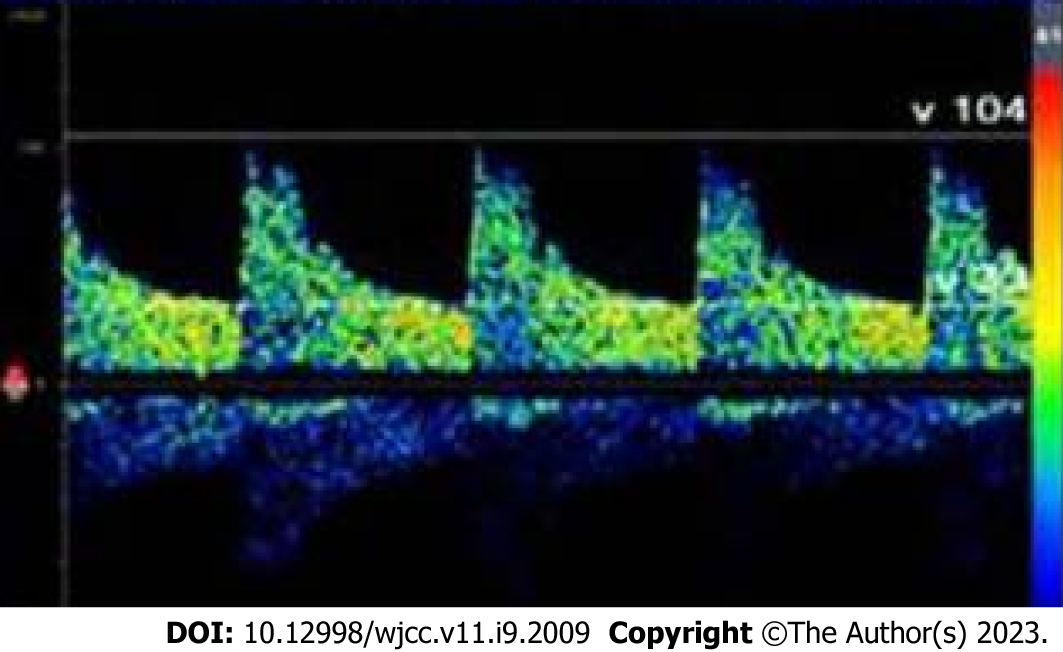
Subsequent chest x-ray showed a mass shadow in the right upper lung (Figure 1). Cardiac color ultrasound showed no obvious abnormalities and no PFO was seen. Cardiovascular computed tomography (CT) angiography (CTA) showed that the right upper pulmonary artery (diameter 7.4 mm) had expanded. Its branching vessels were thickened and twisted into an abnormal vascular nest with direct reflux into the right upper pulmonary posterior vein, and the artery finally merged into the right upper pulmonary vein (Figure 2). Brain magnetic resonance imaging and cerebral artery magnetic resonance angiography showed no obvious abnormalities (Figure 3). Contrast-enhanced transcranial Doppler (c-TCD) ultrasound was remarkable for a large right-to-left shunt (RLS) (Figure 4).
The patient was diagnosed with TIA and PAVF. TIA induced via PAVF was considered.
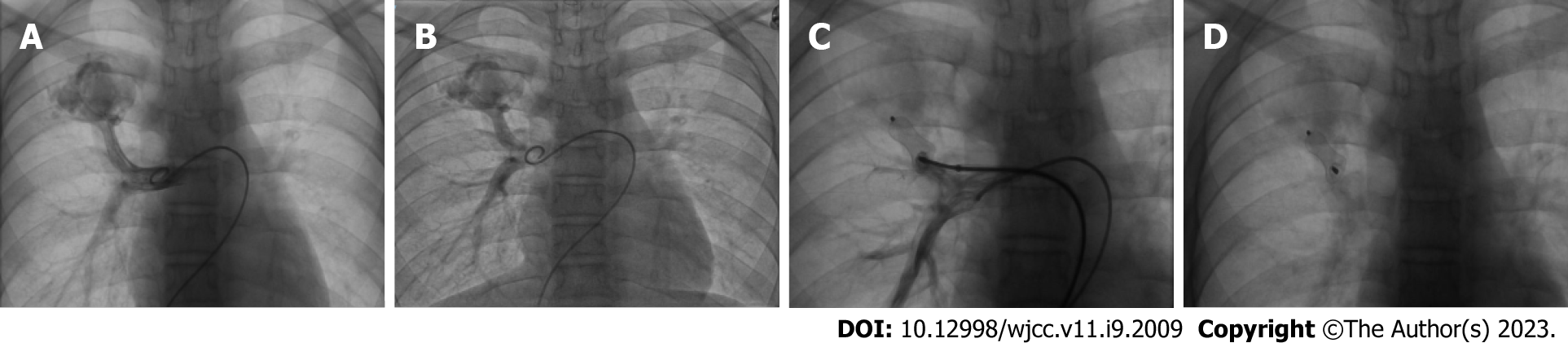
The patient underwent embolization therapy of the PAVF under general anesthesia on the day 3 of hospitalization. Intraoperative angiography showed that the PAVF originated from the right upper pulmonary branch artery (Figure 5A and B), which was no longer detected after embolization with a vascular plug (Figure 5C and D).
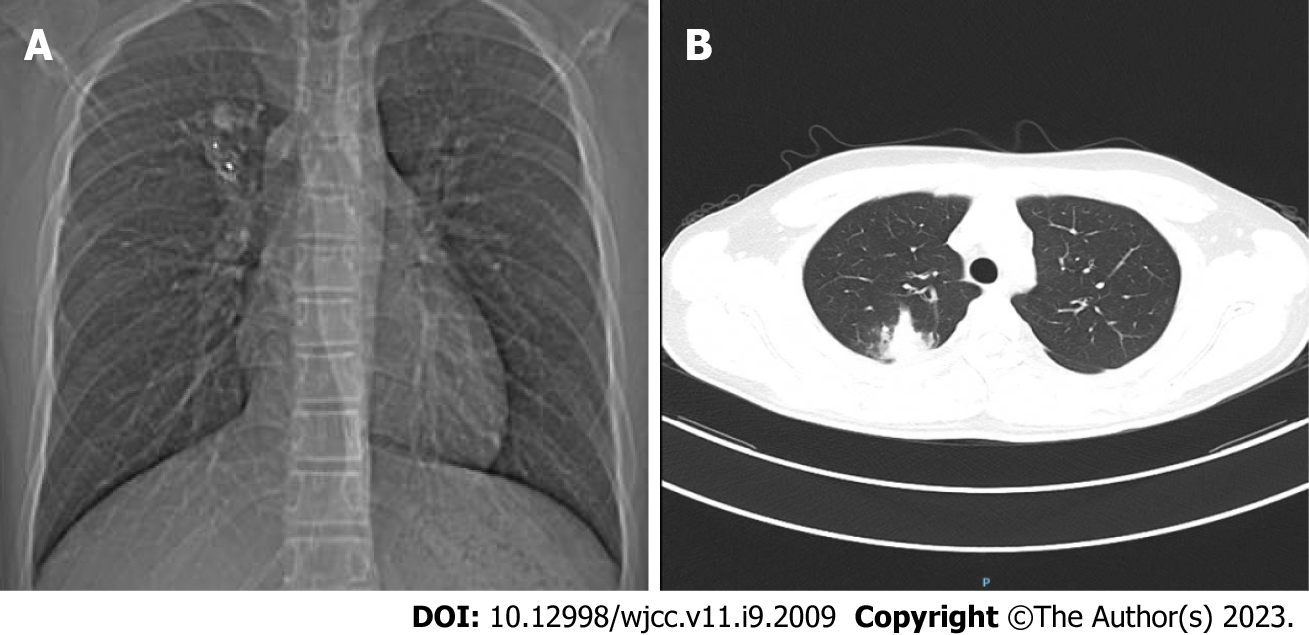
At the 10 mo postoperative follow-up, a chest x-ray showed that the position of the vascular plug was stable (Figure 6A), and a CT scan showed that the PAVF had markedly shrunk (Figure 6B). At the 1 year and 2 years postoperative follow-up points, the patient remained clinically stable without symptoms of dizziness, limb weakness, or fainting.
The presence of a RLS, which can result in paradoxical brain embolism, is an important etiology of ischemic stroke especially in young adults. PFO and PAVF are the most important causes of RLS. TCD ultrasound is currently reported to be a noninvasive and useful method for detecting RLS. The gold standard for detecting RLS is contrast-enhanced transesophageal echocardiography. It is recommended that these examinations be carried out immediately after onset of stroke[7]. A previous report showed that the prevalence of PAVF is 0.026%[8], and TIA is a clinical manifestation of PAVF in up to 20% of cases[1]. At present, it is believed that the risk factors for cerebral ischemic stroke in patients with PAVF are as follows: (1) Feeding artery diameter > 3 mm; and (2) existence of multiple PAV malformations[9]. Whether patients with PAVF present with clinical manifestations depends on the level of the RLS. There are intrapulmonary and extrapulmonary manifestations in patients with PAVF. The intrapulmonary manifestations include dyspnea after activity, dizziness, easy fatigability, and others[10-12]. Physical examination may reveal cyanosis, clubbing of fingers or toes, or continuous chest murmur. Some patients may only present with abnormal arterial blood gas analysis. The extrapulmonary manifestations include migraine, TIA, ischemic stroke, brain abscess, epilepsy, and others[10-12].
Espejo-Herrero et al[1] reported a patient with TIA presenting with a short-term (30 min) right limb paralysis, with subsequent pulmonary arteriography showing a PAVF. Pulmonary digital subtraction angiography (DSA) is the gold standard for the diagnosis of PAVF, which can determine fistula size, feeding artery, draining vein, and other conditions[10]. However, DSA is an invasive examination. As a noninvasive procedure, CTA can not only show the lesions (even mild lesions) and the blood vessels involved in PAVF, but can also accurately judge peripheral and complex PAVF anatomy, which is more helpful in diagnosis[10]. At present, c-TCD is widely used for RLS screening, which can observe the dynamics of emboli entering the intracranial arteries and the changes of cerebral blood flow in real time[13]. In our case, c-TCD ultrasound revealed a large RLS, which was in line with the diagnosis of PAVF.
Most PAVFs will gradually enlarge and rarely shrink spontaneously, which may cause serious complications. The mortality rate in untreated patients with PAVF is as high as 50%, which can be reduced to 3% after treatment. It is currently recommended that active treatment should be pursued in patients with symptomatic or asymptomatic PAVF if the lesion diameter exceeds 3 mm. PAVF treatments mainly include surgery and interventional embolization, both of which can improve the symptoms of hypoxia and prevent the occurrence of central nervous system complications[10,11]. Todo et al[14] reported a patient with recurrent ischemic stroke caused by PAVF with a feeding artery diameter of 1.80 mm, and embolic events were successfully prevented after fistula embolization. Our patient was treated with interventional embolization of PAVF in our hospital. The patient had no recurrent seizure or TIA symptoms for 2 years, further suggesting that recurrent TIA symptoms are indeed associated with PAVF.
Although PAVF is a rare cause of abnormal embolism, it should not be ignored. Most patients with PAVF have atypical clinical presentations, and can even present with cerebral ischemic stroke or TIA as the only clinical finding. Therefore, in patients with cryptogenic stroke, especially children, appropriate examinations should be performed to determine whether a PAVF may be present. If a PAVF is discovered, active treatment and follow-up should be pursued.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Khouzam RN, United States; Suwanto D, Indonesia S-Editor: Fan JR L-Editor: Filipodia P-Editor: Fan JR
| 1. | Espejo-Herrero JJ, Bravo-Rodríguez F, Triviño-Tarradas F, Ysamat-Marfá R, Zurera-Tendero LJ, Canis-López M. [Transient ischemic attack as the presenting symptom of a pulmonary arteriovenous fistula]. Rev Neurol. 2005;40:163-165. [PubMed] |
| 2. | Roshanali F, Mandegar MH, Oraii S. Traumatic pulmonary arteriovenous fistula may be misdiagnosed with residual shunt after patent foramen ovale closure. BMJ Case Rep. 2012;2012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Wozniak L, Mielczarek M, Sabiniewicz R. Paradoxical brain embolism in a young man: is it only a patent foramen ovale? Neurol Neurochir Pol. 2015;49:61-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Tomelleri G, Bovi P, Carletti M, Mazzucco S, Bazzoli E, Casilli F, Onorato E, Moretto G. Paradoxical brain embolism in a young man with isolated pulmonary arteriovenous fistula. Neurol Sci. 2008;29:169-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Cortes M, Mayeda GS, Liu MW. Recurrent minor strokes/TIA with a right to left shunt. BMJ Case Rep. 2018;2018. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Vindiš D, Hutyra M, Šaňák D, Král M, Čecháková E, Littnerová S, Adam T, Přeček J, Hudec Š, Ječmenová M, Táborský M. Patent Foramen Ovale and the Risk of Cerebral Infarcts in Acute Pulmonary Embolism-A Prospective Observational Study. J Stroke Cerebrovasc Dis. 2018;27:357-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Matsuoka H. [Paradoxical brain embolism]. Rinsho Shinkeigaku. 2005;45:849-851. [PubMed] |
| 8. | Ma X, Li LL, Yu D, Jie B, Jiang S. Management of pulmonary arteriovenous malformations involves additional factors aside from the diameter of feeding arteries: a 3-year case-case retrospective analysis. Respir Res. 2022;23:107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 9. | Holzer RJ, Cua CL. Pulmonary Arteriovenous Malformations and Risk of Stroke. Cardiol Clin. 2016;34:241-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Tellapuri S, Park HS, Kalva SP. Pulmonary arteriovenous malformations. Int J Cardiovasc Imaging. 2019;35:1421-1428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 11. | Majumdar S, McWilliams JP. Approach to Pulmonary Arteriovenous Malformations: A Comprehensive Update. J Clin Med. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 12. | Kramdhari H, Valakkada J, Ayyappan A. Diagnosis and endovascular management of pulmonary arteriovenous malformations. Br J Radiol. 2021;94:20200695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Wessler BS, Kent DM, Thaler DE, Ruthazer R, Lutz JS, Serena J. The RoPE Score and Right-to-Left Shunt Severity by Transcranial Doppler in the CODICIA Study. Cerebrovasc Dis. 2015;40:52-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Todo K, Moriwaki H, Higashi M, Kimura K, Naritomi H. A small pulmonary arteriovenous malformation as a cause of recurrent brain embolism. AJNR Am J Neuroradiol. 2004;25:428-430. [PubMed] |