Published online Mar 6, 2023. doi: 10.12998/wjcc.v11.i7.1593
Peer-review started: November 17, 2022
First decision: January 3, 2023
Revised: January 15, 2023
Accepted: February 13, 2023
Article in press: February 13, 2023
Published online: March 6, 2023
Processing time: 105 Days and 9.7 Hours
Titanium mesh cranioplasty is often performed after decompressive craniectomy. Spontaneous fracture of the titanium prosthesis is an extremely rare postoperative complication. Here, we report a 10-year-old boy who presented with a spon
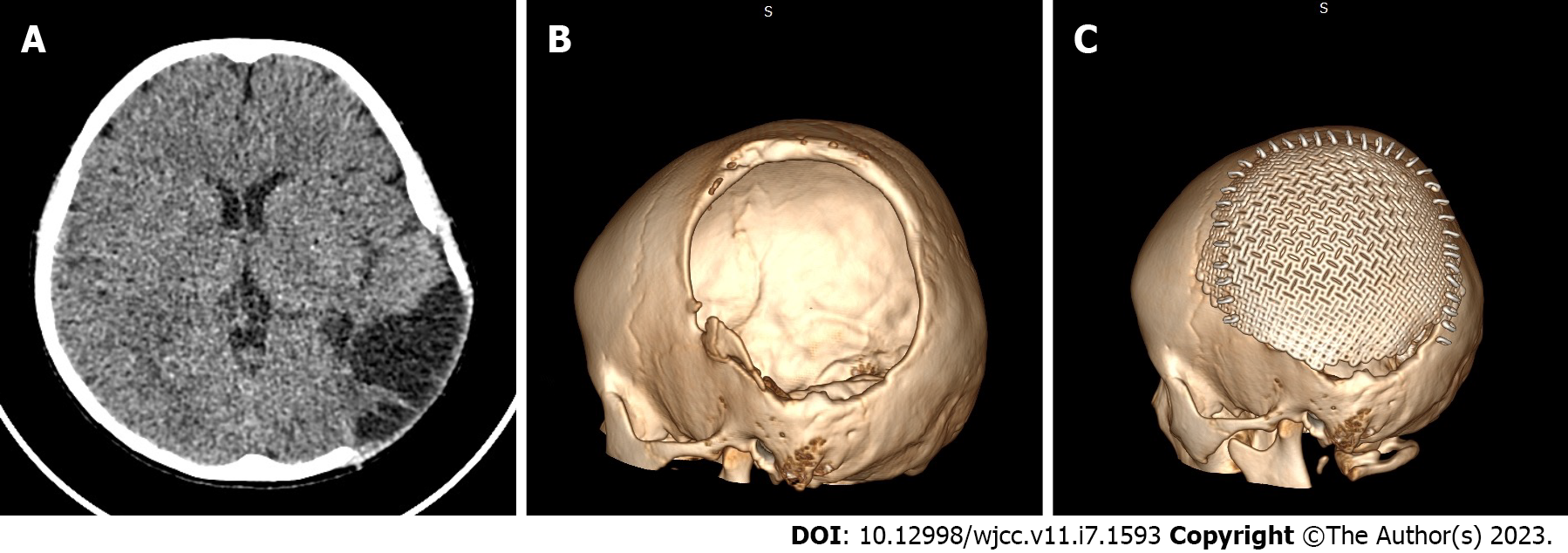
A 10-year-old boy presented with a 1-wk history of a tender bulge over the left temporo-parieto-occipital scalp. He had undergone a temporo-parieto-occipital titanium mesh cranioplasty 26 mo previously. He denied antecedent head trauma. Computerized tomography disclosed a perpendicular fissure in the titanium mesh, suggesting a diagnosis of spontaneous titanium mesh fracture. He underwent a second temporo-parieto-occipital cranioplasty and made an uneventful recovery. Three-dimensional modeling and finite element analyses were used to explore potential risk factors of titanium mesh fracture.
We report a case of spontaneous fracture of a titanium mesh cranioplasty implant. The current case and literature review indicate that titanium mesh implants should be well-anchored to the base of bony defects to prevent fatigue-induced fractures.
Core Tip: Titanium mesh cranioplasty is often indicated after decompressive craniectomy. We present a rare case of a spontaneous fracture of a titanium mesh cranioplasty implant in a 10-year-old boy. By conducting a literature review and finite element analysis, we learned that titanium mesh prosthetic implants should be well-anchored to the base of bony defects to prevent fatigue-induced fractures.
- Citation: Zhang R, Gao Z, Zhu YJ, Wang XF, Wang G, He JP. Spontaneous fracture of a titanium mesh cranioplasty implant in a child: A case report. World J Clin Cases 2023; 11(7): 1593-1599
- URL: https://www.wjgnet.com/2307-8960/full/v11/i7/1593.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i7.1593
Titanium mesh is considered safe for implantation during cranioplasties in both adults and children[1-5], and is among the most commonly used biocompatible materials for calvarial fixation and reconstruction. Although titanium mesh cranioplasty is usually a straightforward surgical procedure, complication rates may reach 34%[6-10]. However, spontaneous fractures of titanium mesh cranioplasty implants are extremely rare. To our knowledge, only one case has been reported previously[11]. Here, we report a spontaneous fracture of titanium mesh without antecedent head trauma in a 10-year-old boy, and provide a literature review to investigate underlying mechanisms and risk factors.
A 10-year-old boy was admitted to our department with complaint of a tender bulge of the left temporo-parieto-occipital scalp of 1 wk duration.
The patient had undergone a temporo-parieto-occipital cranioplasty 26 mo previously. The patient denied antecedent trauma or intensive force to the head.
Three years previously, the patient fell from a height of 3 meters and sustained a closed head injury. He was brought immediately to an emergency department, where he was diagnosed with a left temporo-parieto-occipital laceration, skull fracture, epidural hematoma, and cerebral contusion. He underwent an emergent craniotomy to evacuate the epidural hematoma, followed by a large decompressive craniectomy of the temporo-parieto-occipital skull flap. He made marked clinical improvement and was readmitted to our department 12 mo later for cranioplasty. Computerized tomography (CT) showed a 10 cm × 8 cm bone defect of the left temporo-parieto-occipital skull with a local encephalocele (Figure 1A and B).
The patient denied any significant personal or family medical histories.
Physical examination disclosed a prominent 4 cm × 5 cm tender malformation of the temporo-parieto-occipital scalp.
Results of routine blood and urine analyses were within normal limits.
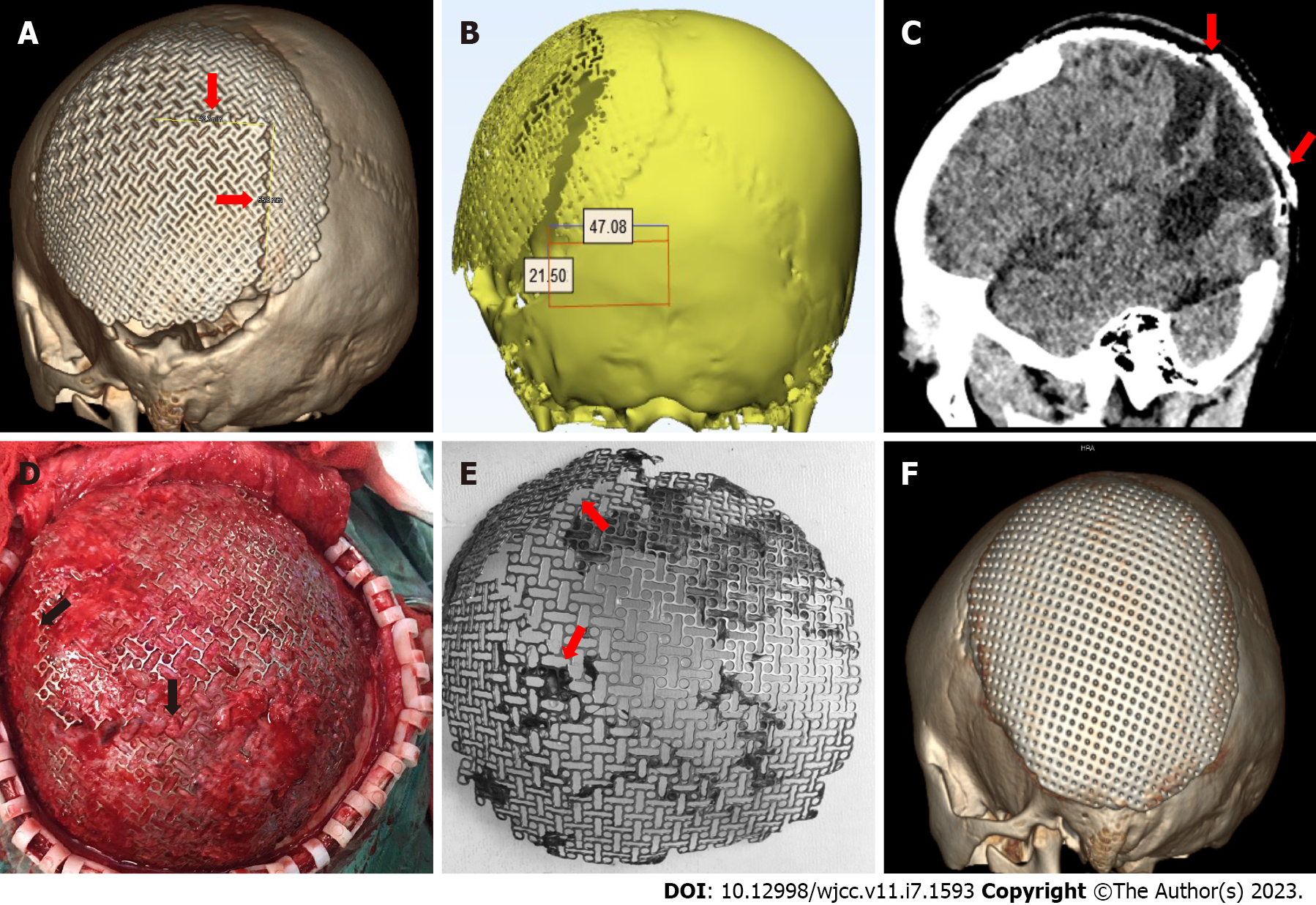
Three-dimensional (3-D) CT reconstruction displayed a clear edge of a titanium mesh fracture, which appeared as a reverse “L”-shaped fissure (Figure 2A-C) that originated from a point 2.21 cm superior to the external occipital protuberance and 4.51 cm left of the midline and extended 5.5 cm superiorly to the parietal bone and then turned anteriorly at a perpendicular angle (Figure 2A and B).
The patient’s history, physical findings, laboratory examinations, and CT images were diagnostic of spontaneous fracture of the titanium mesh.
A temporo-parieto-occipital cranioplasty was performed using a 0.8 mm titanium mesh. Temporal-occipital muscles were stripped from the dura, and the prosthesis was anchored to the base of the bony defect with titanium screws (Figure 2D and F). The temporal-occipital muscles were then fixed to the prosthesis with nylon suture.
The patient was discharged in stable and asymptomatic condition on the 4th postoperative day.
Fractures of orthopedic titanium implants are not rare, especially among devices positioned in the spine and long bones, which are often subjected to weight loading[12-15]. Predisposing factors include: (1) Defective prosthetic material[16]; (2) Poor prosthetic design[17]; (3) Inadequate fixation[18]; (4) Deficient surgical technique[19]; (5) Skull growth; and (6) Biomechanical overload[11]. The titanium mesh used for our patient’s first cranioplasty was patient-matched through computer-assisted design and manufacturing, and its quality was assured. Moreover, the patient did not suffer head trauma and the prosthesis was not subjected to weight loading. Therefore, the risks of defective material, poor design, and weight overloading were eliminated. Regarding fixation and surgical technique, the first titanium mesh was implanted by experienced neurosurgeons using a matched titanium screw fixator system. Thus, these two factors were also excluded, leaving the possibilities of pediatric growing fracture and biomechanical overload.
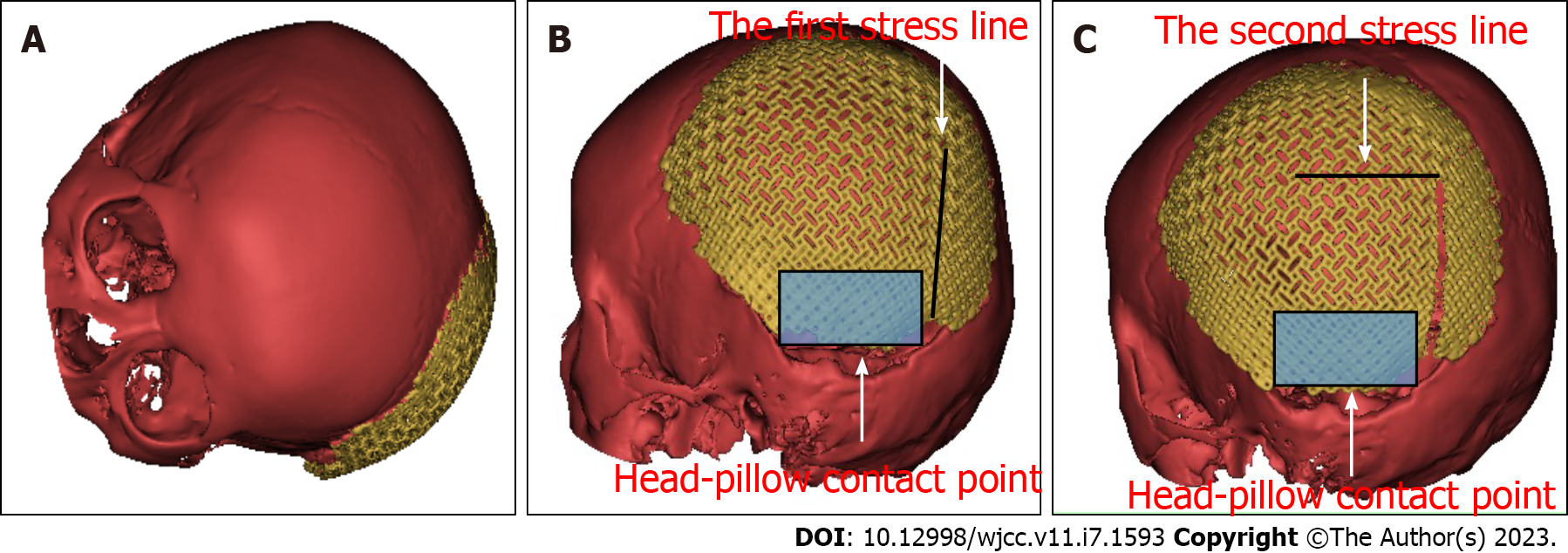
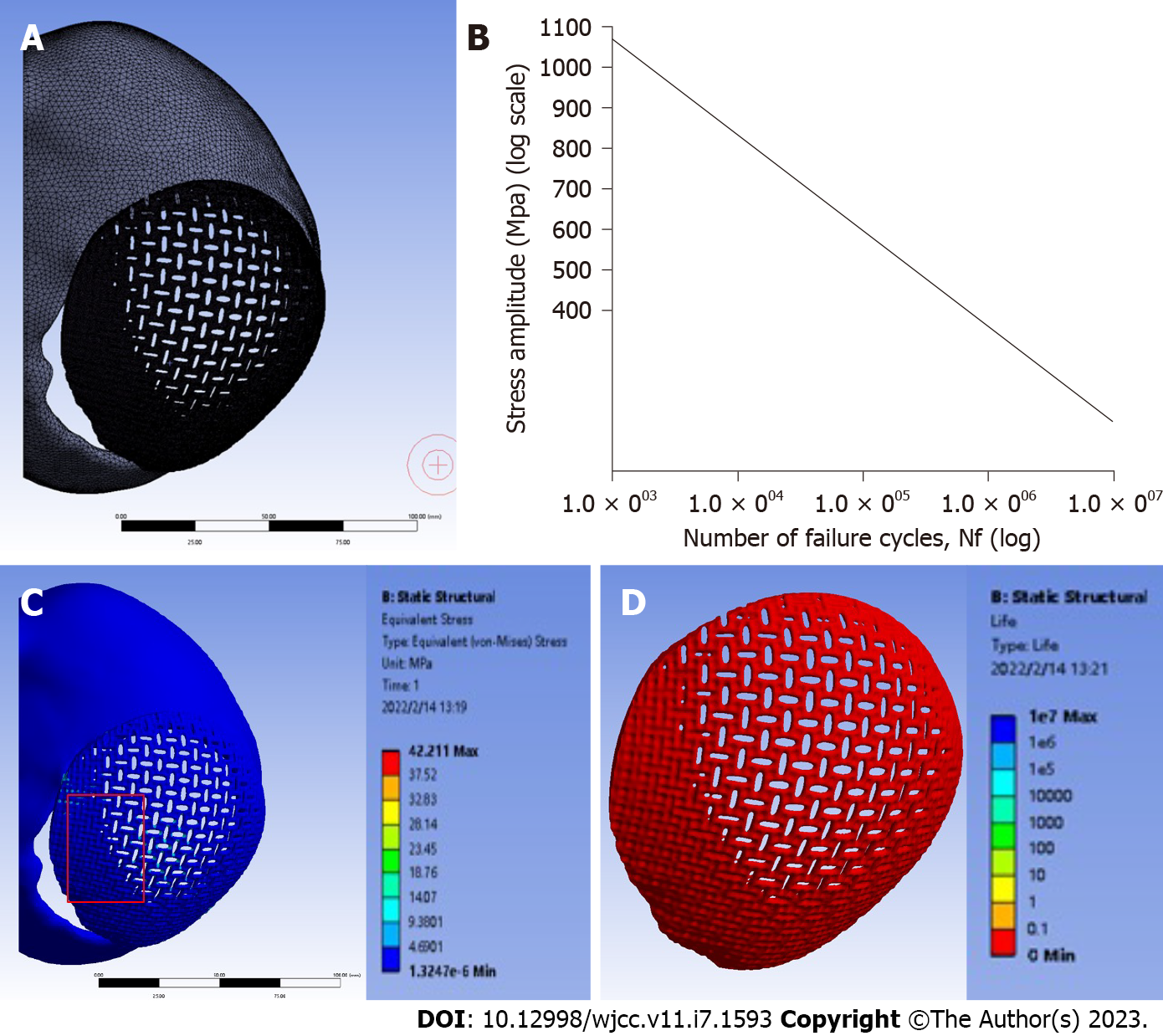
Growing skull fracture, a rare complication of pediatric head trauma, develops after linear fractures with underlying dural tears, and may cause brain herniation[20]. Our patient’s dura was intact during the second reconstructive procedure. Hence, this possibility was also excluded. Therefore, the only remaining possibility was biomechanical overload. Jiang et al[11] reported a similar case in which head-pillow contact during sleep subjected the prosthesis to biomechanical overload. To explore whether head-pillow contact contributed to our patient’s titanium mesh fracture, we performed a simple experiment using a skull model. We created a similar bony defect using a 3-D printed skull model and a plastic mesh to simulate the prosthesis (Figure 3). We fixed the plastic mesh to the model skull and rotated the model on a horizontal plate to simulate head rotation on a pillow (Figure 3A). Because the mesh was not anchored to the base of the bony defect, a remarkable stress line, originating from a point which was 2 cm superior to the protuberantia occipitalis externa and 4 cm left of the midline appeared as soon as the base of the mesh touched the plate (Figure 3B). The shearing force generated along the stress line may lead to fatigue, which could cause a linear fracture. However, this could not explain the reverse "L" rather than a linear configuration of our patient’s fracture. We hypothesized that the stress line might change after dilaceration of a linear fracture. We incised the model mesh along the stress line and again rotated the model on a horizontal plate. This resulted in the emergence of a new perpendicular stress line on the mesh (Figure 3C). To further confirm our hypothesis, we invited Minggong Simulation Technology Co., Ltd to evaluate deformation and stress distributions using finite element analysis. We created a head-pillow contact scenario using a skull-implant assembly model and set the loading force at 50 N (gravitational force of the patient’s head). As seen in Figure 4, finite element analysis showed a maximum stress of 42 MPa under a 50 N load on the head-pillow contact surface, which indicated that the skull-implant structure could bear the weight of the head under normal circumstances (Figure 4C). However, fatigue behavior analysis revealed that the titanium mesh might not tolerate cyclical loading (Figure 4D), implying that our patient’s spontaneous titanium mesh fracture may have resulted from fatigue failure. Therefore, we selected a thickened titanium mesh and anchored it to the base of the bony defect during the second cranioplasty. Follow-up showed excellent results.
We report a case of spontaneous fracture of a titanium mesh cranioplasty implant. The current case and literature review indicate that titanium mesh prosthetics should be well-anchored to the base of bony defects to prevent fatigue-induced fractures.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Alkhatib AJ, Jordan; Hakimi T, Afghanistan; Kung WM, Taiwan S-Editor: Zhang H L-Editor: Filipodia P-Editor: Zhang H
| 1. | Binhammer A, Jakubowski J, Antonyshyn O, Binhammer P. Comparative Cost-Effectiveness of Cranioplasty Implants. Plast Surg (Oakv). 2020;28:29-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 2. | Hitoshi Y, Yamashiro S, Yoshida A, Mukasa A. Cranial Reconstruction with Titanium Mesh for Open Depressed Skull Fracture in Children: Reports of Two Cases with Long-term Observation. Kurume Med J. 2020;66:77-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Sheng HS, Shen F, Zhang N, Lin FC, Li DD, Cai M, Jiang GQ, Lin J. Titanium mesh cranioplasty in pediatric patients after decompressive craniectomy: Appropriate timing for pre-schoolers and early school age children. J Craniomaxillofac Surg. 2019;47:1096-1103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Ma IT, Symon MR, Bristol RE, Beals SP, Joganic EF, Adelson PD, Shafron DH, Singh DJ. Outcomes of Titanium Mesh Cranioplasty in Pediatric Patients. J Craniofac Surg. 2018;29:99-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 5. | Goldstein JA, Paliga JT, Bartlett SP. Cranioplasty: indications and advances. Curr Opin Otolaryngol Head Neck Surg. 2013;21:400-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 82] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 6. | Maqbool T, Binhammer A, Binhammer P, Antonyshyn OM. Risk Factors for Titanium Mesh Implant Exposure Following Cranioplasty. J Craniofac Surg. 2018;29:1181-1186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 7. | Mukherjee S, Thakur B, Haq I, Hettige S, Martin AJ. Complications of titanium cranioplasty--a retrospective analysis of 174 patients. Acta Neurochir (Wien). 2014;156:989-98; discussion 998. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 86] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 8. | Williams LR, Fan KF, Bentley RP. Custom-made titanium cranioplasty: early and late complications of 151 cranioplasties and review of the literature. Int J Oral Maxillofac Surg. 2015;44:599-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 72] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 9. | Yeap MC, Tu PH, Liu ZH, Hsieh PC, Liu YT, Lee CY, Lai HY, Chen CT, Huang YC, Wei KC, Wu CT, Chen CC. Long-Term Complications of Cranioplasty Using Stored Autologous Bone Graft, Three-Dimensional Polymethyl Methacrylate, or Titanium Mesh After Decompressive Craniectomy: A Single-Center Experience After 596 Procedures. World Neurosurg. 2019;128:e841-e850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 54] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 10. | Yoshioka N, Tominaga S. Titanium Mesh Implant Exposure Due To Pressure Gradient Fluctuation. World Neurosurg. 2018;119:e734-e739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | Jiang Y, Wang YK, Yu MK. Spontaneous fracture of cranioplastic titanium implants without head trauma in an adult: A case report. Int J Surg Case Rep. 2016;24:50-53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Kaplan T, Gulbahar G, Gundogdu AG, Han S. An unexpected complication of titanium rib clips. Ann Thorac Surg. 2014;98:2206-2209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Klezl Z, Bagley CA, Bookland MJ, Wolinsky JP, Rezek Z, Gokaslan ZL. Harms titanium mesh cage fracture. Eur Spine J. 2007;16 Suppl 3:306-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Park SW, Kim H, In Y. Fracture of titanium nitride-coated femoral component after total knee arthroplasty. Knee. 2014;21:871-874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Yukata K, Doi K, Hattori Y, Sakamoto S. Early breakage of a titanium volar locking plate for fixation of a distal radius fracture: case report. J Hand Surg Am. 2009;34:907-909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Yeganeh A, Otoukesh B, Kaghazian P, Yeganeh N, Boddohi B, Moghtadaei M. Evaluation of the Etiologies of Implant Fracture in Patients With Fractures of the Implants of Lower Limbs' Long Bones. Med Arch. 2015;69:405-408. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Osman RB, Ma S, Duncan W, De Silva RK, Siddiqi A, Swain MV. Fractured zirconia implants and related implant designs: scanning electron microscopy analysis. Clin Oral Implants Res. 2013;24:592-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 18. | Shinohara K, Takigawa T, Tanaka M, Sugimoto Y, Arataki S, Yamane K, Watanabe N, Ozaki T, Sarai T. Implant Failure of Titanium Versus Cobalt-Chromium Growing Rods in Early-onset Scoliosis. Spine (Phila Pa 1976). 2016;41:502-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 19. | Nematian H, Clarke A, Hedayat E, Vahdati Z, Milan N, Mehrpour SR, Nabian MH, Mazda K. Complications of single growing rod constructs in the treatment of severe early-onset scoliosis: a lesson relearned. Spine Deform. 2022;10:1481-1490. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 20. | Bir SC, Kalakoti P, Notarianni C, Nanda A. John Howship (1781-1841) and growing skull fracture: historical perspective. J Neurosurg Pediatr. 2015;16:472-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |