Published online Mar 6, 2023. doi: 10.12998/wjcc.v11.i7.1521
Peer-review started: October 22, 2022
First decision: November 22, 2022
Revised: December 6, 2022
Accepted: February 16, 2023
Article in press: February 16, 2023
Published online: March 6, 2023
Processing time: 131 Days and 3.3 Hours
Invasive breast carcinoma with osteoclast-like stromal giant cells (OGCs) is an extremely rare morphology of breast carcinomas. To the best of our knowledge, the most recent case report describing this rare pathology was published six years ago. The mechanism controlling the development of this unique histological formation is still unknown. Further, the prognosis of patients with OGC involvement is also controversial.
We report the case of a 48-year-old woman, who presented to the outpatient department with a palpable, growing, painless mass in her left breast for about one year. Sonography and mammography revealed a 26.5 mm × 18.8 mm asymmetric, lobular mass with circumscribed margin and the Breast Imaging Reporting and Data System was category 4C. Sono-guided aspiration biopsy revealed invasive ductal carcinoma. The patient underwent breast conserving surgery and was diagnosed with invasive breast carcinoma with OGCs, grade II, with intermediate grade of ductal carcinoma in situ (ER: 80%, 3+, PR: 80%, 3+, HER-2: negative, Ki 67: 30%). Adjuvant chemotherapy and post-operation radiotherapy were initiated thereafter.
As a rare morphology of breast cancer, breast carcinoma with OGC occurs most often in relatively young women, has less lymph node involvement, and its occurrence is not race-dependent.
Core Tip: We present a case of invasive breast carcinoma with Osteoclast-like stromal giant cells (OGC). Complete radiographic images, clinico-pathologic characteristic features, and immunohistochemical stains were reported. Breast carcinomas with OGCs are believed to be mostly luminal A invasive carcinomas of no particular type, prevalent among young women, and having good outcomes. Moreover, there seems to be no relationship between the incidence of the disease and ethnicity. Although only one third of the patients develop axillary lymph node metastases, a sentinel node procedure is recommended for these cases.
- Citation: Wang YJ, Huang CP, Hong ZJ, Liao GS, Yu JC. Invasive breast carcinoma with osteoclast-like stromal giant cells: A case report. World J Clin Cases 2023; 11(7): 1521-1527
- URL: https://www.wjgnet.com/2307-8960/full/v11/i7/1521.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i7.1521
Osteoclast-like stromal giant cells (OGCs) are rarely observed and are found in organs such as the breast, gall bladder, liver, thyroid, and pancreas[1]. Carcinoma with osteoclastic (or osteoclast-like) giant cells of the breast constitutes only 0.5%–1.2% of breast carcinomas[2]. The unique stromal feature can be found within invasive, ductal, lobular, squamous, or papillary breast carcinomas. The prognosis of OGC-involved breast cancer is controversial. A lower cytological grade is found in mammary carcinomas with OGC, which leads to a good prognosis. However, about one third of cancers with OGC develop axillary node metastases[3]. The therapeutic plan for cancers with OGC is strongly correlated with the expression of histochemical stains such as the estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER-2). Genomic testing analysis is currently the preferred method for classification and early disease detection.
A palpable, growing, and painless mass in the patient’s left breast for approximately one year.
A 48-year-old, unmarried, premenopausal female presented to the outpatient department with a palpable, growing, and painless mass in the left breast for approximately one year. The patient reported no recent body weight loss, poor appetite, or bone pain. She also denied having undergone regular breast ultrasound or mammography. We arranged a series of tests to analyze the mass.
The patient denied the occurrence of any systemic diseases. The patient had no history of malignancy, hypertension, diabetes mellitus, or hypertensive heart disease.
The patient exhibited normal social functioning and self-care. She experienced normal menstruation with menarche at 14 years of age and her previous menstrual period was one week prior to presenting at the clinic. There was no family history of breast cancer or any other malignancy.
Physical examination revealed an unmovable, hard mass in the left breast, approximately 3 cm in diameter, at the 12 o'clock position, and 2 cm away from the nipple. No skin dimpling, nipple discharge, nor any palpable node in the axillary region or neck were observed.
Laboratory studies revealed no specific abnormalities and the tumor markers were within the normal range.
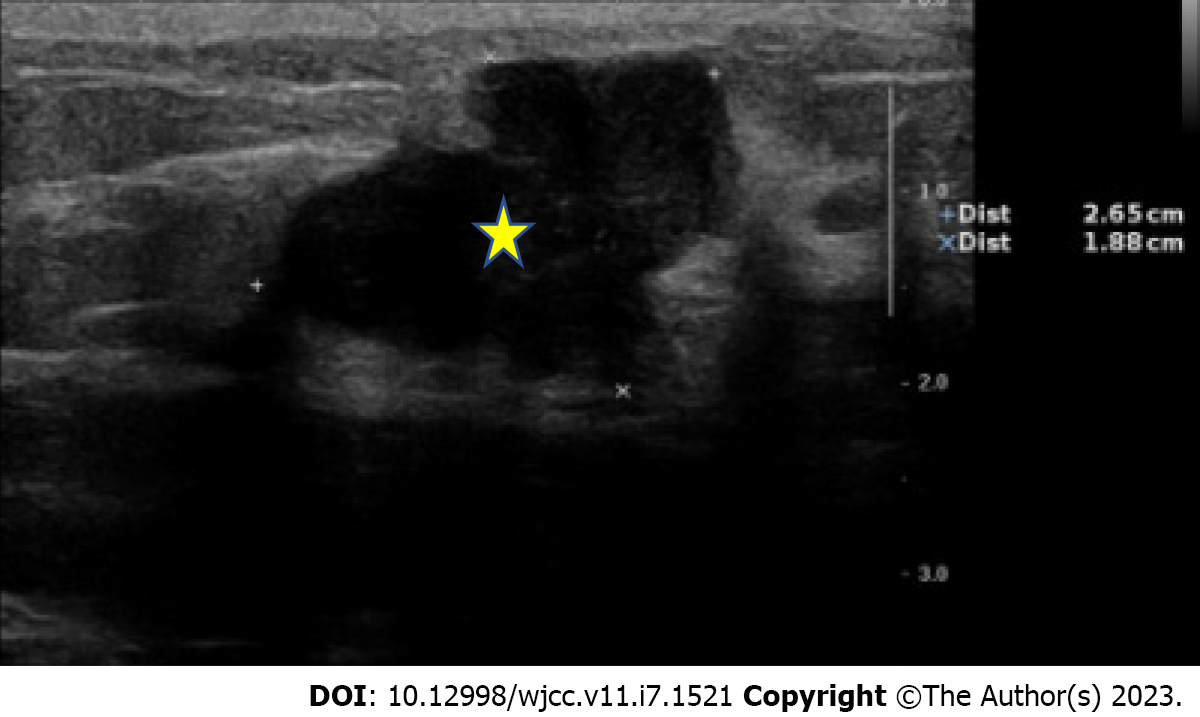
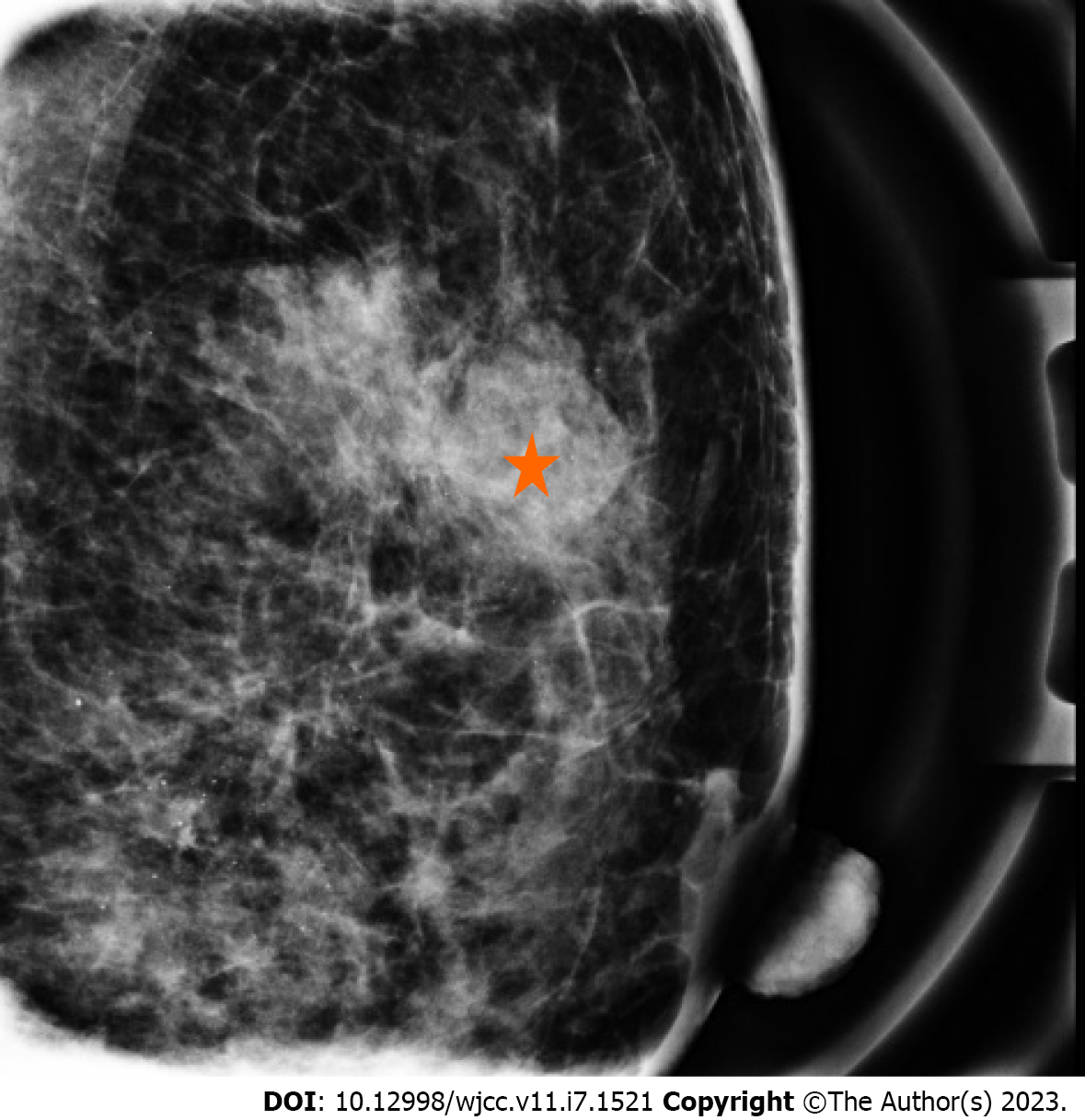
Sonography revealed a 26.5 mm × 18.8 mm asymmetric, lobular mass with a circumscribed margin of BI-RADS category 4C (Figure 1). Mammography revealed a partial, circumscribed lobular mass in the upper outer quadrant of the left breast with amorphous and punctate calcifications (Figure 2). Sonography-guided aspiration biopsy was performed and the pathology revealed an invasive ductal carcinoma of grade I.
Based on the aspiration pathology results, invasive breast carcinoma was diagnosed. Prior to the operation, further imaging using magnetic resonance imaging was performed, which revealed a mass lesion over the left breast without evidence of focal mass or enlarged node in the bilateral axillary regions or the neck.
The patient underwent a partial mastectomy and sentinel node dissection. The pathology report finally revealed invasive breast carcinoma with OGC, grade II and ductal carcinoma in situ of intermediate grade (ER: 80%, 3+, PR: 80%, 3+, HER-2: negative, Ki 67: 30%). There was no evidence of lymph node metastasis. Whole-body positron emission tomography scan and bone scan revealed no distant metastasis. Breast cancer, pT2N0M0 of stage IIA was finally diagnosed.
Adjuvant chemotherapy and post-operation radiotherapy were initiated after the breast conserving surgery.
At the time of writing this manuscript, the patient was under standard treatment without any therapeutic side effects.
The occurrence of OGCs is rare and the actual number of cases may be underestimated owing to the lack of a disease code or missing histological examination[4]. Diagnosis of OGCs can be challenging because they can occur in different types of carcinomas; moreover, they appear similar to foreign-body giant cells associated with fat necrosis[1]. In addition, sonography and mammography findings of tumors with OGCs may sometimes mimic those of benign lesions. Thus, aspiration biopsy or core biopsy is suggested for early detection.
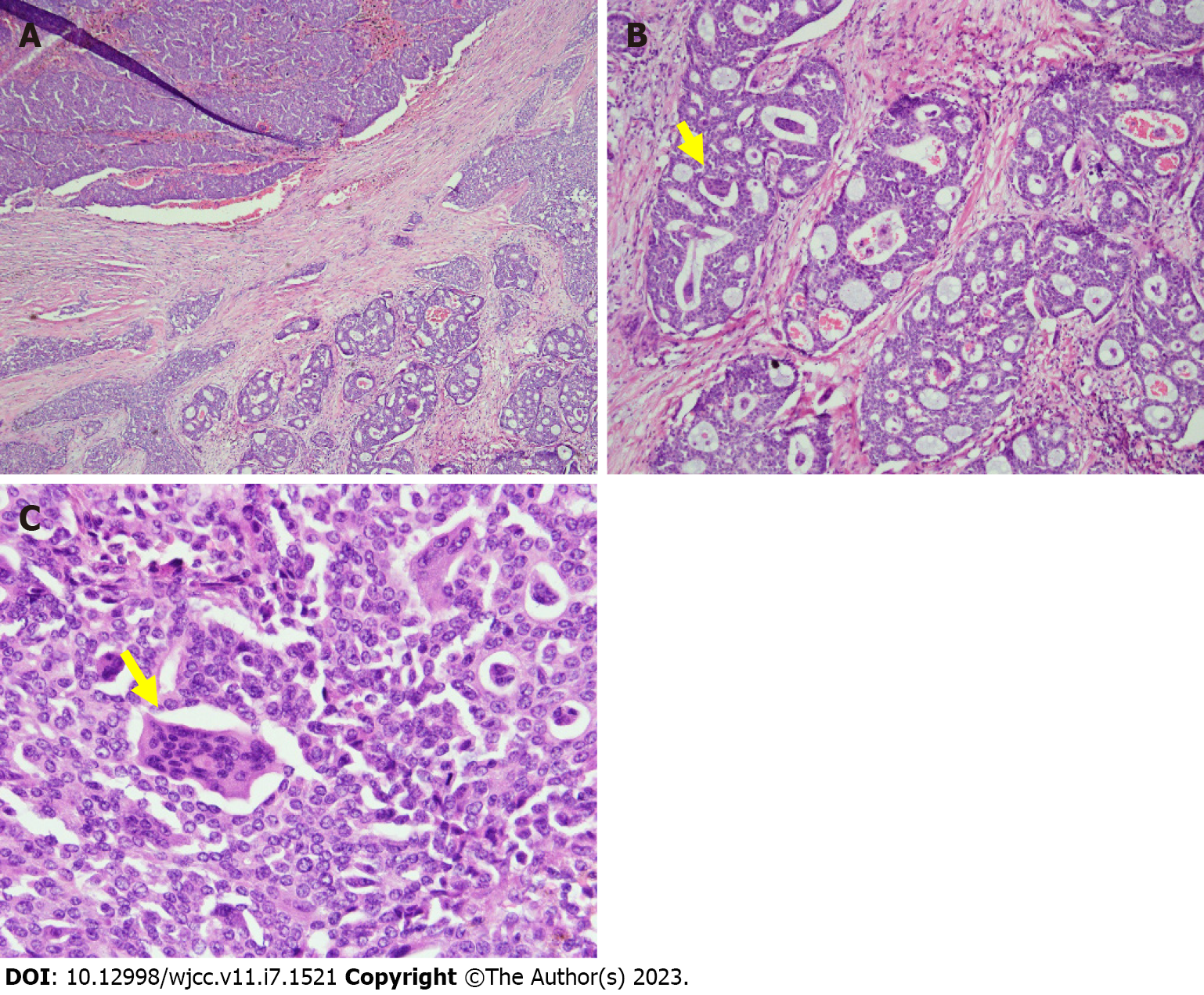
Microscopically, in our case, the infiltrative mammary tumor was composed of ducts, small nests, and cribriform pattern with embedded multinucleated OGCs (Figure 3). The background also showed red blood cell extravasation and hemosiderin deposition. Inflammatory OGCs are associated with an inflamed, fibroblastic, hypervascular stroma composed of extravasated erythrocytes, lymphocytes, and monocytes, as well as mononucleated and binucleated histiocytes, which sometimes contain hemosiderin. There are two hypotheses regarding the formation of OGCs. In the first, the tumor induced hypervascular microenvironment could enhance microphage migration and OGC transformation[5]. The second hypothesis links OGC formation with viral infection, such as the Epstein Barr virus or high-risk human papilloma viruses 16/18, accounting for the oncogenic factor[6,7]. Currently, the first hypothesis is preferred.
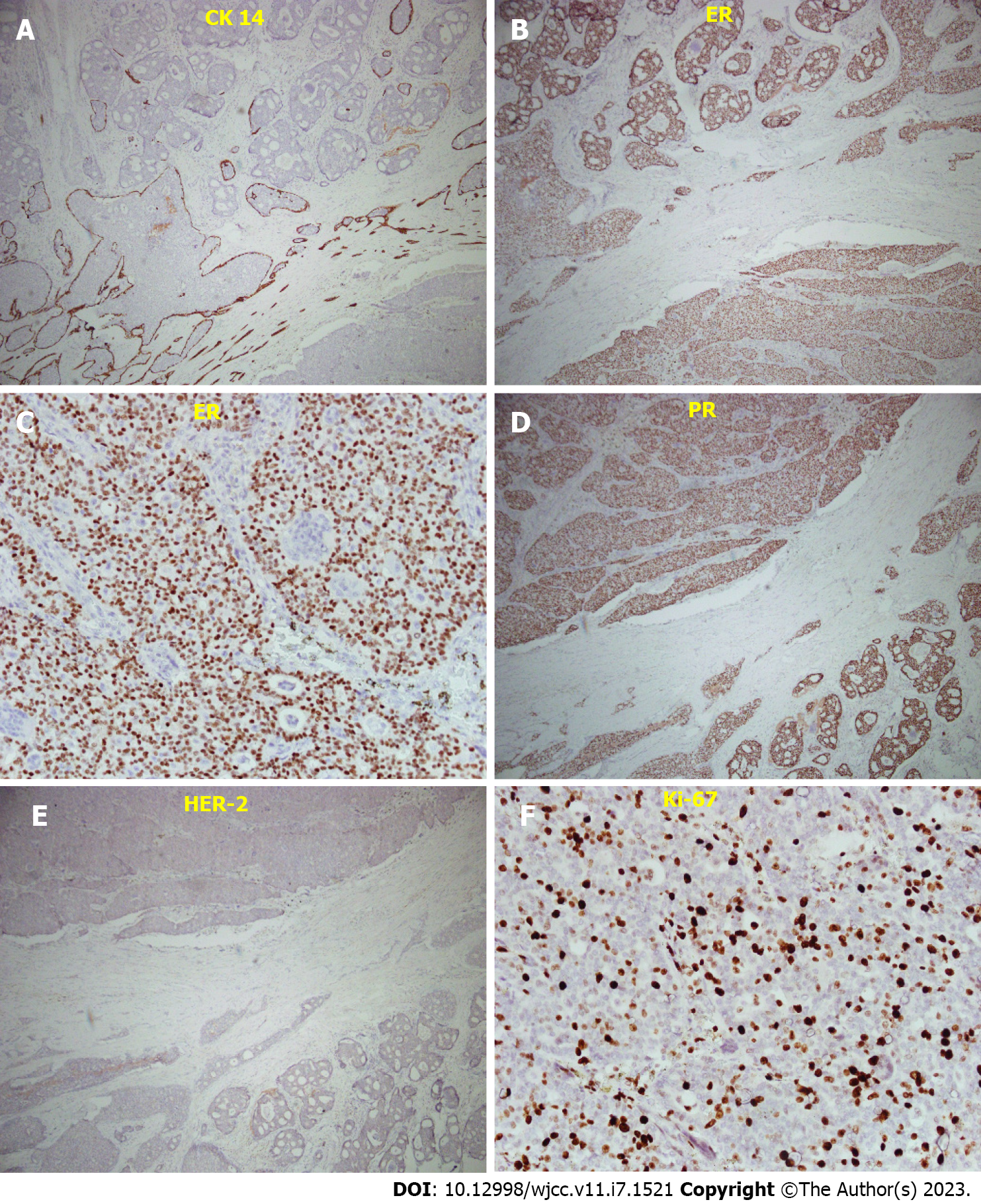
Additionally, immunohistochemical staining revealed ER positivity, PR positivity, HER-2 negativity, and low levels of the proliferation index Ki-67(< 30%), which are attributed to the luminal A subtype. Cytokeratin 14 staining represented ductal carcinoma in situ (Figure 4). Recently, breast carcinomas with OGCs were believed to be mostly luminal A invasive carcinomas of no special type (IC NST), occurring in relatively young women (median age: 46 years old), and resulting in good prognoses[8]. While only one third of breast carcinomas with OGCs develop axillary lymph node metastases, a sentinel node procedure is recommended for these cases.
Breast carcinoma with OGCs was first described by Rosen in 1979[9]. Since then, there are multiple case reports demonstrating this unique morphology of breast cancer. More discussions of its clinical appearance, prognosis, histopathology, and molecular portrait have also been reported. Here, in addition to sharing the first case of invasive breast carcinoma with OGC infiltration in Chinese Taipei, we also aggregated the recent case reports (Table 1). Since Caucasians and Asians share a similar numbers of cases, this morphology is not race-dependent. This disease is found among relatively young women, with a median age of 46 years for the patients described in the recent case reports. There was no lymph node involvement in these case reports underscoring the good prognosis of this disease.
| Ref. | Region/races | Case number | Median age | Tumor size | Lymph node metastasis |
| Zagelbaum et al[10], 2016 | United States/Caucasian | 1 | 64 | 4 cm | None |
| Niu et al[1], 2014 | China/Asian | 1 | 46 | 4 cm | None |
| Albawardi et al[11], 2014 | United Arab Emirates/Mediterranean | 1 | 45 | 3 cm | None |
| Shishido-Hara et al[5], 2010 | Japan/Asian | 2 | 63 | 2 cm | None |
| Cai et al[2], 2005 | United States/Asian | 4 | 44 | 1.1–4 cm | None |
| Our case, 2023 | Chinese Taipei/Asian | 1 | 48 | 3.2 cm | None |
Currently, there are limited cases of invasive breast carcinoma with OGCs. The most recent integrated case report was presented in 2016[10]. Our case demonstrated a standard presentation of invasive breast carcinoma with OGCs. The prognosis was believed to be associated with the type of carcinoma, regardless of the OGC presence. Although there are few cases of lymph node metastasis with this type of breast cancer, a sentinel node procedure is still recommended. As there are few cases of this disease, further research is warranted.
The authors wish to acknowledge the assistance of the people in the Department of Surgery, Tri Service General Hospital, National Defense Medical Center. This report would not have been possible without their efforts in data collection and interprofessional collaboration in treating this patient.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Pathology
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Chen B, China; Shen ZY, China S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
| 1. | Niu Y, Liao X, Li X, Zhao L. Breast carcinoma with osteoclastic giant cells: case report and review of the literature. Int J Clin Exp Pathol. 2014;7:1788-1791. [PubMed] |
| 2. | Cai N, Koizumi J, Vazquez M. Mammary carcinoma with osteoclast-like giant cells: a study of four cases and a review of literature. Diagn Cytopathol. 2005;33:246-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Cai G, Simsir A, Cangiarella J. Invasive mammary carcinoma with osteoclast-like giant cells diagnosed by fine-needle aspiration biopsy: review of the cytologic literature and distinction from other mammary lesions containing giant cells. Diagn Cytopathol. 2004;30:396-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Jacquet SF, Balleyguier C, Garbay JR, Bourgier C, Mathieu MC, Delaloge S, Vielh P. Fine-needle aspiration cytopathology--an accurate diagnostic modality in mammary carcinoma with osteoclast-like giant cells: a study of 8 consecutive cases. Cancer Cytopathol. 2010;118:468-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Shishido-Hara Y, Kurata A, Fujiwara M, Itoh H, Imoto S, Kamma H. Two cases of breast carcinoma with osteoclastic giant cells: are the osteoclastic giant cells pro-tumoural differentiation of macrophages? Diagn Pathol. 2010;5:55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 6. | Athanasou NA, Wells CA, Quinn J, Ferguson DP, Heryet A, McGee JO. The origin and nature of stromal osteoclast-like multinucleated giant cells in breast carcinoma: implications for tumour osteolysis and macrophage biology. Br J Cancer. 1989;59:491-498. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 72] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Yahia ZA, Adam AA, Elgizouli M, Hussein A, Masri MA, Kamal M, Mohamed HS, Alzaki K, Elhassan AM, Hamad K, Ibrahim ME. Epstein Barr virus: a prime candidate of breast cancer aetiology in Sudanese patients. Infect Agent Cancer. 2014;9:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 8. | Cyrta J, Benoist C, Masliah-Planchon J, Vieira AF, Pierron G, Fuhrmann L, Richardot C, Caly M, Leclere R, Mariani O, Da Maia E, Larousserie F, Féron JG, Carton M, Renault V, Bidard FC, Vincent-Salomon A. Breast carcinomas with osteoclast-like giant cells: a comprehensive clinico-pathological and molecular portrait and evidence of RANK-L expression. Mod Pathol. 2022;35:1624-1635. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Rosen PP. Multinucleated mammary stromal giant cells: a benign lesion that simulates invasive carcinoma. Cancer. 1979;44:1305-1308. [PubMed] [DOI] [Full Text] |
| 10. | Zagelbaum NK, Ward MF 2nd, Okby N, Karpoff H. Invasive ductal carcinoma of the breast with osteoclast-like giant cells and clear cell features: a case report of a novel finding and review of the literature. World J Surg Oncol. 2016;14:227. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Albawardi AS, Awwad AA, Almarzooqi SS. Mammary carcinoma with osteoclast-like giant cells: a case report. Int J Clin Exp Pathol. 2014;7:9038-9043. [PubMed] |