Published online Feb 16, 2023. doi: 10.12998/wjcc.v11.i5.1217
Peer-review started: December 1, 2022
First decision: December 20, 2022
Revised: December 23, 2022
Accepted: January 16, 2023
Article in press: January 16, 2023
Published online: February 16, 2023
Processing time: 75 Days and 0.8 Hours
Cervical haemorrhage due to spontaneous rupture of a parathyroid adenoma is a rare complication that may cause life-threatening acute airway compromise.
A 64-year-old woman was admitted to the hospital 1 day after the onset of right neck enlargement, local tenderness, head-turning difficulty, pharyngeal pain, and mild dyspnoea. Repeat routine blood testing showed a rapid decrease in the haemoglobin concentration, indicating active bleeding. Enhanced computed tomography images showed neck haemorrhage and a ruptured right parathyroid adenoma. The plan was to perform emergency neck exploration, haemorrhage removal, and right inferior parathyroidectomy under general anaesthesia. The patient was administered 50 mg of intravenous propofol, and the glottis was successfully visualised on video laryngoscopy. However, after the administration of a muscle relaxant, the glottis was no longer visible and the patient had a difficult airway that prevented mask ventilation and endotracheal intubation. Fortunately, an experienced anaesthesiologist successfully intubated the patient under video laryngoscopy after an emergency laryngeal mask placement. Postoperative pathology showed a parathyroid adenoma with marked bleeding and cystic changes. The patient recovered well without complications.
Airway management is very important in patients with cervical haemorrhage. After the administration of muscle relaxants, the loss of oropharyngeal support can cause acute airway obstruction. Therefore, muscle relaxants should be administered with caution. Anaesthesiologists should pay careful attention to airway management and have alternative airway devices and tracheotomy equipment available.
Core Tip: Spontaneous parathyroid haemorrhage is a rare but potentially life-threatening complication. Anaesthesiologists need to take extra care when administering muscle relaxants to avoid increasing the difficulty of endotracheal intubation. Visual intubation tools, alternative airway devices such as laryngeal masks, and even tracheotomy preparations should be readily available.
- Citation: Han YZ, Zhou Y, Peng Y, Zeng J, Zhao YQ, Gao XR, Zeng H, Guo XY, Li ZQ. Difficult airway due to cervical haemorrhage caused by spontaneous rupture of a parathyroid adenoma: A case report. World J Clin Cases 2023; 11(5): 1217-1223
- URL: https://www.wjgnet.com/2307-8960/full/v11/i5/1217.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i5.1217
Spontaneous parathyroid haemorrhage is an exceptionally rare but potentially life-threatening condition due to airway compromise. Haemorrhage may be contained within the parathyroid gland but often presents as extracapsular haemorrhage extending into the neck or mediastinum, manifesting as neck circumference enlargement, neck tenderness, ecchymosis, acute pain, and dyspnoea. Such circumstances may result in a difficult airway[1,2]. We describe a case of spontaneous haemorrhage from a parathyroid adenoma presenting as an acute airway compromise requiring surgical evacuation.
The patient (height 170 cm, weight 75 kg, body mass index 24.5) has no significant fat accumulation in the neck, and denies the history of sleep apnea and any family history of related diseases.
Eight years previously, bilateral thyroid nodules and a right parathyroid nodule had been detected and left untreated. There was a history of neck compression before the onset of the present pharyngeal pain.
She had swelling of the right neck accompanied by tenderness, difficulty in turning the head, pharyngeal pain, and mild dyspnoea 1 d.
A 64-year-old woman with pharyngeal pain of no apparent cause.
Repeat routine blood testing showed that the haemoglobin concentration had decreased from 124 g/L to 108 g/L in 8 h, suggesting active bleeding. Calcium concentration was 2.79 mmol/L (normal level, 2.25-2.75 mmol/L), parathyroid hormone (PTH) had been tested immediately which was 344.50 pg/mL (normal level, 15-65 pg/mL)[3].
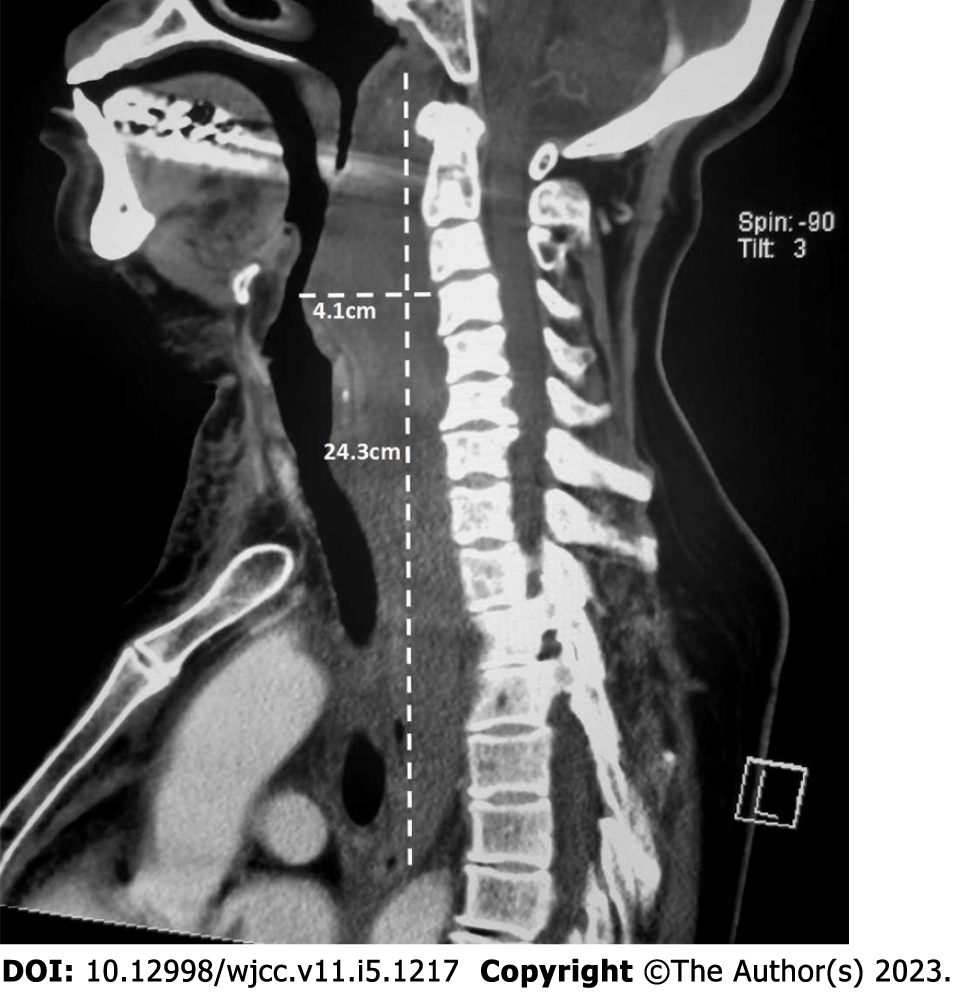
Computed tomography (CT) revealed a soft tissue density lesion in the parapharyngeal space (Figure 1). The nasopharynx, oropharynx, and laryngeal pharynx were compressed and narrowed. The lesion extended from the neck to the mediastinum (Figure 2), involving the posterior pharyngeal wall, middle and upper oesophagus, bilateral carotid sheaths, posterior cervical trachea, thoracic trachea, and posterior thyroid. The thoracic trachea was slightly shifted to the right. The lesion was closely related to a right posterior mass with varying density outside the thyroid.
Auxiliary testing showed a haemoglobin concentration of 124 g/L, leukocyte count of 9.06 × 109/L, and neutrophil ratio of 0.847.
Physical examination revealed mildly congested oral and pharyngeal mucosa, lymphofollicular hyperplasia in the posterior pharyngeal wall, grade 1 sized bilateral tonsils, and a sharp and well-elevated epiglottic margin. The area around the right submandibular gland was swollen, with slightly reddened skin and marked tenderness. It is a pity that we didn't leave the external photograph of the patient's neck and jaw.
Based on the history, clinical manifestations, and auxiliary test results, the patient was diagnosed with rupture and bleeding of a right parathyroid adenoma.
The progressive decrease in the haemoglobin concentration suggested that the bleeding might aggravate the dyspnoea or even lead to asphyxia due to airway compression. Therefore, emergency neck exploration, haemorrhage removal, and right inferior parathyroidectomy were planned.
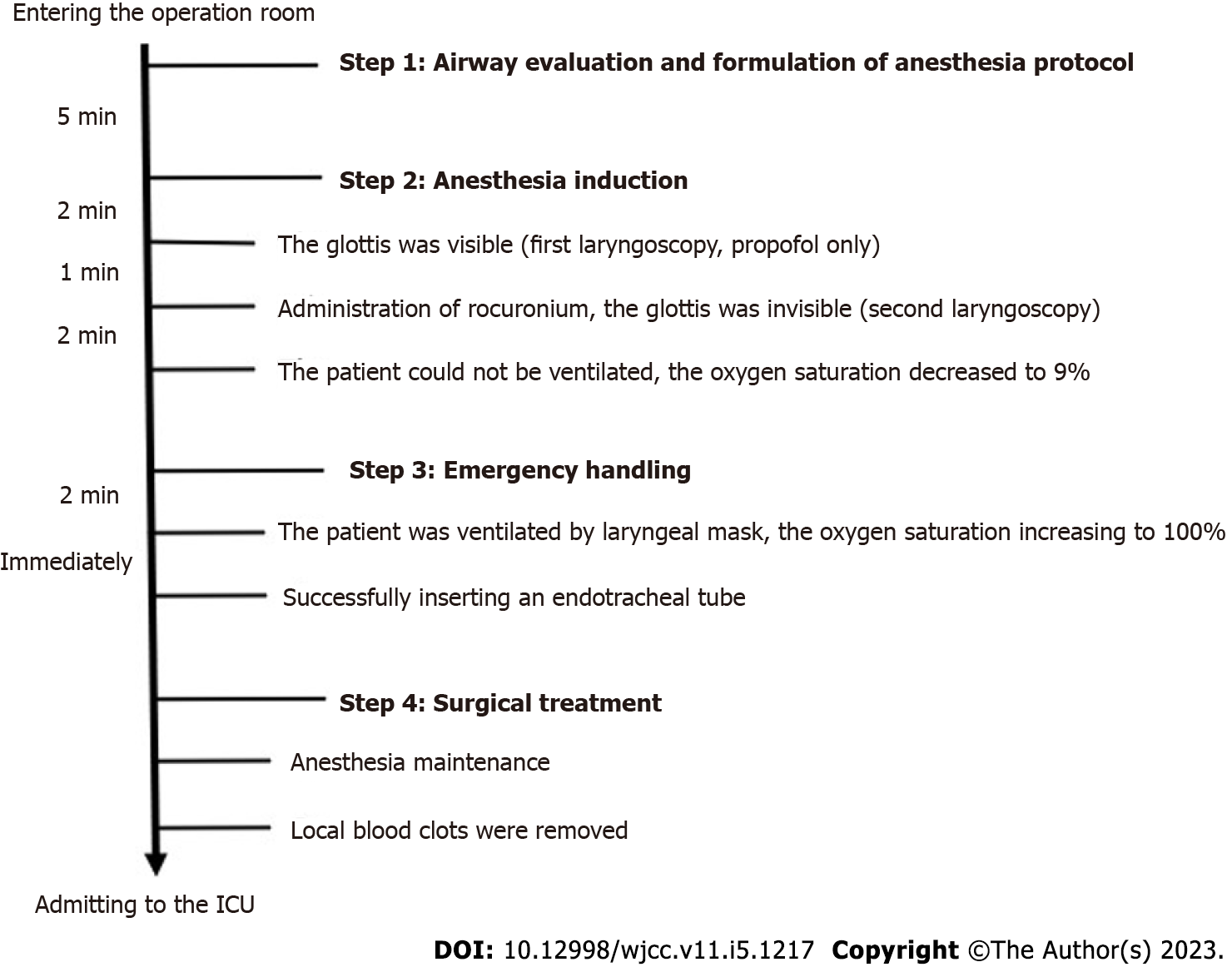
In the operation room, we conducted preoperative airway evaluation: Mouth opening > 3 cm, modified Mallampati grade I, normal dentition, but limited cervical spine movement and CT images showed trachea compression which did not rule out the possibility of difficult airway[4]. Considering that endotracheal intubation guided by fiberoptic bronchoscope in awake state may cause discomfort, cough, and even further aggravate hematoma, we were prepared to give a small dose of propofol. If the glottis can be seen clearly, continuing to administer opioids and muscle relaxants, and directing endotracheal intubation under laryngoscope; If Cormack-Lehane grade is Ⅲ or Ⅳ, we will insert endotracheal tube guided by fiberoptic bronchoscope after the patient regained consciousness. Electrocardiography, pulse oximetry, and non-invasive blood pressure were all continuously monitored during anaesthesia and recorded at fixed intervals of 3 min. After 3 min of preoxygenation, the patient was administered 50 mg of intravenous propofol, and the airway was checked with a video laryngoscope (first laryngoscopy). Although there was cyan-purple-coloured congestion of the posterior pharyngeal wall, the glottis was visible. The patient was then administered 50 mg of propofol and 30 mg of rocuronium intravenously. During the second video laryngoscopy, the visual field was obscured by secretions and blood, and the glottis was not clearly visible. The patient could not be ventilated with a mask, and the oxygen saturation decreased sharply to 9%. Unfortunately, our research center does not have sugammadex to reverse rocuronium after difficult ventilation. A laryngeal mask was applied immediately and the ventilation situation improved, with the oxygen saturation gradually increasing to 100% within 2 min. Fortunately, the experienced anaesthesiologist arriving at the operation room attempted to intubate the patient through the mouth under video laryngoscopy and successfully inserted a #6.5 steel-reinforced endotracheal tube. Anaesthesia was maintained with 1.5%–2% sevoflurane and 100–300 μg/h remifentanil during emergency surgery. A sternal incision (2 cm × 10 cm) was created and the anterior cervical tissue was separated in a layer-by-layer manner. There was a large amount of pooled blood in the trachea and oesophagus. The parathyroid gland at the right lower pole was enlarged, fragile, and had a breach. The right inferior parathyroid gland and right thyroid gland were completely resected, and the left thyroid was partially resected because of a goitre. The right and left thyroid glands hindered the exposure of the right parathyroid gland, the back of the oesophagus, and the trachea. During the operation, the recurrent laryngeal nerve was dissected for protection, and about 200 mL of local blood clots were removed. According to the records, we show the process of the event in chronological order as follows (Figure 3).
After surgery, the patient was admitted to the intensive care unit, extubated on postoperative day 1 (calcium concentration was 2.07 mmol/L, PTH was 26.35 pg/mL), and discharged on postoperative day 9. No postoperative complications occurred. Postoperative pathology showed that the lesion was a parathyroid adenoma with severe bleeding and cystic changes.
Spontaneous haemorrhage of a parathyroid adenoma is a rare condition that was first reported in 1934[5]. Subsequently, there have been over 80 cases of haemorrhage associated with a parathyroid adenoma described in the English literature, and four cases reported in the Chinese literature; the patients in more than half of these cases presented with compressive symptoms due to haemorrhage[1,2]. Spontaneous rupture of a parathyroid adenoma is caused by an imbalance between tumour growth and blood supply[6]. The clinical manifestations of ruptured parathyroid adenoma are mostly atypical, such as neck swelling, pain, ecchymosis, and compression of adjacent anatomical structures in accordance with the location and degree of bleeding . Since no unified diagnostic criteria in clinical practice, Simcic et al[7] had proposed three criteria for the diagnosis of parathyroid tumor rupture and bleeding: acute neck swelling, hypercalcemia, and neck or chest ecchymosis. Compared with imaging examination, not all cases meet the diagnostic criteria, the increase of blood calcium and PTH is more suggestive[1,3,8]. Hypercalcemia may be related to the release of cyst fluid containing high levels of parathyroid hormone caused by acute infarction of parathyroid adenoma, which also explains why the blood calcium and PTH of patients fall to normal levels soon after surgery. Anaesthesia-related problems associated with spontaneous haemorrhage of a parathyroid adenoma include difficult laryngoscopy, airway stenosis due to compression caused by cervical haemorrhage, and even difficult ventilation in extreme cases.
Bleeding in the retropharyngeal and submandibular spaces can cause upper airway obstruction and life-threatening complications[8-11]. Patients with early retropharyngeal haemorrhage may present with a sore throat without dyspnoea and may be misdiagnosed with viral pharyngitis. Twelve to 48 h of bleeding may precede symptoms of respiratory embarrassment[12]. The rapid development of respiratory distress from sublingual, retropharyngeal, and parapharyngeal haemorrhages can be fatal. Bleeding into the retropharyngeal space is serious because of the anatomic characteristics of the pharyngeal muscles. Without muscle support, the pharyngeal airway can be nearly completely blocked. Therefore, muscle relaxants must be used very carefully. In the present case, the glottis was visible during the first video laryngoscopy but was not visible during the second laryngoscopy after rocuronium administration. We speculated that the loss of laryngopharyngeal muscle tone after the administration of rocuronium caused the parapharyngeal haemorrhage to compress the arytenoid cartilages, close the vocal cords, and obstruct the airway. However, no CT images of the laryngopharynx were taken after the rocuronium was administered.
Early cervical exploration was necessary to evacuate the coagulated haematoma and ligate the bleeding vessel. This course of treatment allowed for a shortened duration of hospitalisation. Severe retropharyngeal bleeding was indicated by the bulging of the posterior wall causing an abnormal thickness of the retropharyngeal tissues, which measured greater than 7 mm from the anteroinferior aspect of the second cervical vertebra to the posterior pharyngeal wall[13].
Spontaneous parathyroid haemorrhage is a rare but potentially life-threatening complication. Anaesthesiologists need to take extra care when administering muscle relaxants to avoid increasing the difficulty of endotracheal intubation. Visual intubation tools, alternative airway devices such as laryngeal masks, and even tracheotomy preparations should be readily available.
We sincerely thank all the staff of the Anaesthesiology Department of Peking University Third Hospital for their help in this case report.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Anesthesiology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fu CH, Taiwan; Tsuchiya M, Japan S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Garrahy A, Hogan D, O'Neill JP, Agha A. Acute airway compromise due to parathyroid tumour apoplexy: an exceptionally rare and potentially life-threatening presentation. BMC Endocr Disord. 2017;17:35. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | An L, Ji T, Li L. Diffuse hematoma caused by spontaneous rupture of a parathyroid adenoma: a case report. Braz J Otorhinolaryngol. 2020;86 Suppl 1:48-50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Khan S, Choe CC, Shabaik A, Bouvet M. Parathyroid adenoma presenting with spontaneous cervical and anterior mediastinal hemorrhage: A case report. Medicine (Baltimore). 2019;98:e14347. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Kheterpal S, Han R, Tremper KK, Shanks A, Tait AR, O'Reilly M, Ludwig TA. Incidence and predictors of difficult and impossible mask ventilation. Anesthesiology. 2006;105:885-891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 414] [Cited by in RCA: 379] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 5. | Capps RB. Multiple parathyroid tumors with massive mediastinal and subcutaneous hemorrhage. Am J Med Sci. 1934;188:801-804. [RCA] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 67] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Efremidou EI, Papageorgiou MS, Pavlidou E, Manolas KJ, Liratzopoulos N. Parathyroid apoplexy, the explanation of spontaneous remission of primary hyperparathyroidism: a case report. Cases J. 2009;2:6399. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Simcic KJ, McDermott MT, Crawford GJ, Marx WH, Ownbey JL, Kidd GS. Massive extracapsular hemorrhage from a parathyroid cyst. Arch Surg. 1989;124:1347-1350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 29] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Zhao C, Wang X, Wei H, Ma G. Parathyroid adenoma causing a spontaneous cervical and mediastinal massive hematoma. Int J Clin Exp Med. 2015;8:21826-21829. [PubMed] |
| 9. | Shinomiya H, Otsuki N, Takahara S, Yasui R, Sawada N, Komatsu H, Fujio H, Fujiwara H, Nibu K. Parathyroid adenoma causing spontaneous cervical hematoma: two case reports. BMC Res Notes. 2015;8:726. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Ulrich L, Knee G, Todd C. Spontaneous cervical haemorrhage of a parathyroid adenoma. Endocrinol Diabetes Metab Case Rep. 2015;2015:150034. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | van den Broek JJ, Poelman MM, Wiarda BM, Bonjer HJ, Houdijk AP. Extensive cervicomediastinal hematoma due to spontaneous hemorrhage of a parathyroid adenoma: a case report. J Surg Case Rep. 2015;2015. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Chin KW, Sercarz JA, Wang MB, Andrews R. Spontaneous cervical hemorrhage with near-complete airway obstruction. Head Neck. 1998;20:350-353. [PubMed] [DOI] [Full Text] |
| 13. | Wholey MH, Bruwer AJ, Baker HL Jr. The lateral roentgenogram of the neck; with comments on the atlanto-odontoid-basion relationship. Radiology. 1958;71:350-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 173] [Article Influence: 2.6] [Reference Citation Analysis (0)] |