Published online Feb 16, 2023. doi: 10.12998/wjcc.v11.i5.1175
Peer-review started: November 12, 2022
First decision: December 26, 2022
Revised: January 7, 2023
Accepted: January 16, 2023
Article in press: January 16, 2023
Published online: February 16, 2023
Processing time: 93 Days and 21.8 Hours
Nocardia pneumonia shares similar imaging and clinical features with pulmonary tuberculosis and lung neoplasms, but the treatment and anti-infective medication are completely different. Here, we report a case of pulmonary nocardiosis caused by Nocardia cyriacigeorgica (N. cyriacigeorgica), which was misdiagnosed as community-acquired pneumonia (CAP) with repeated fever.
A 55-year-old female was diagnosed with community-acquired pneumonia in the local hospital because of repeated fever and chest pain for two months. After the anti-infection treatment failed in the local hospital, the patient came to our hospital for further treatment. Enhanced computed tomography showed multiple patchy, nodular and strip-shaped high-density shadows in both lungs. A routine haematological examination was performed and showed abnormalities in CD19+ B cells and CD4+ T cells. Positive acid-fast bifurcating filaments and branching gram-positive rods were observed in the bronchoalveolar lavage fluid of the patient under an oil microscope, which was identified by matrix-assisted laser desorption ionization-time of flight mass spectrometry as N. cyriacigeorgica. The patient's condition quickly improved after taking 0.96 g compound sulfamethoxazole tablets three times a day.
The antibiotic treatment of Nocardia pneumonia is different from that of common CAP. Attention should be given to the pathogenic examination results of patients with recurrent fever. Nocardia pneumonia is an opportunistic infection. Patients with CD4+ T-cell deficiency should be aware of Nocardia infection.
Core Tip: Patients with CD4+ T-cell deficiency should be aware of Nocardia infection. Nocardia pneumonia shares similar imaging and clinical features with pulmonary tuberculosis and lung neoplasms, but the treatment and anti-infective medication are completely different. Here, we report a case of pulmonary nocardiosis caused by Nocardia cyriacigeorgica (N. cyriacigeorgica), which was misdiagnosed as community-acquired pneumonia with repeated fever. We identified the pathogen by matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF MS). The patient used compound sulfamethoxazole tablets (0.96 g) three times a day. After one week of treatment, the infection index returned to normal, the patient's condition improved significantly, and she was discharged.
- Citation: Hong X, Ji YQ, Chen MY, Gou XY, Ge YM. Nocardia cyriacigeorgica infection in a patient with repeated fever and CD4+ T cell deficiency: A case report. World J Clin Cases 2023; 11(5): 1175-1181
- URL: https://www.wjgnet.com/2307-8960/full/v11/i5/1175.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i5.1175
Repeated fever often means the failure of empirical and conventional anti-infection treatment and that the pathogen has not been completely killed. However, repeated fever of unknown cause has great challenges in clinical diagnosis. Nocardia pneumonia is an opportunistic infection occurring in immunocompromised patients who share similar imaging and clinical features with pulmonary tuberculosis and lung neoplasms, but treatment and anti-infective medication are completely different[1,2]. Nocardia asteroides, Nocardia brasiliensis, Nocardia farcinica and Nocardia otitidiscaviarum are the common pathogens of human disease out of more than 100 defined subtypes of Nocardia to date[3]. Nocardia cyriacigeorgica (N. cyriacigeorgica) is relatively rare in the clinic and has been recognized as an emerging pathogenic bacterium since it was first described in a patient with chronic bronchitis in Germany by Yassin[4,5]. Here, we report a case of pulmonary nocardiosis caused by N. cyriacigeorgica, which was diagnosed as community-acquired pneumonia (CAP) with repeated fever.
A 55-year-old female was admitted to our hospital due to repeated fever and chest pain for two months.
The patient was diagnosed with CAP in the local hospital because of repeated fever and chest pain for two months. She was given anti-infective treatment with cefoperazone sodium/sulbactam sodium, ornidazole sodium chloride, and etimicin sulfate. The situation of the patient did not improve; thus, she went to Zhejiang Provincial People's Hospital for further treatment.
The patient had been cured of tuberculosis six years prior. The patient had no underlying diseases such as hypertension and diabetes, no infectious diseases such as hepatitis and malaria, and no history of surgery or drug addiction. Allergy to penicillins.
The patient was married, employed as a clerk, and had lived somewhere. The patient had no history of living in the epidemic area, no history of travelling, no history of drinking and smoking, no history of exposure to radiation and poison, and no family genetic disease.
The patient's tympanic temperature was 36.9℃, her respiration was 16 breaths/min, her pulse was 67 beats/min, her blood pressure was 109/63 mmHg, her mind was clear, her supraclavicular lymph node was not enlarged, her sternum was not tender, her lungs were auscultated with clear breath sounds, no extensive dry or wet rales were heard, her rhythm was regular, no obvious pathological murmur was heard in the auscultation area of each valve, her liver and spleen were not palpable under the ribs, her abdomen was flat and soft, there was no tenderness or rebound pain, there was no oedemaedema in either leg, and no obvious abnormality was found in the neurological examination.
Abnormal elevations in neutrophils (81.1%), C-reactive protein (CRP) (126.9 mg/L), erythrocyte sedimentation rate (86 mm/h), CD19+ B cells (32%) and plasma fibrinogen (6.5 g/L) and decrease in serum albumin (38.9 g/L), creatine kinase (31 U/L), CD16+CD56+ NK cells (0.7%) and CD4+ T cells (0) were indicated by laboratory examinations (Table 1).
| Laboratory indicators | Measurements | Normal interval |
| Neutrophils | 81.1% | 40%-75% |
| CRP | 126.9 mg/L | < 10 mg/L |
| ESR | 86 mm/h | < 26 mm/h |
| Serum albumin | 38.9 g/L | 40-55 g/L |
| creatine kinase | 31 U/L | 40-200 U/L |
| CD16+CD56+ NK cells | 0.7% | 8%-20% |
| CD19+ B cells | 32% | 7%-23% |
| CD4+ T cells | 0 | 24.5%-41.91% |
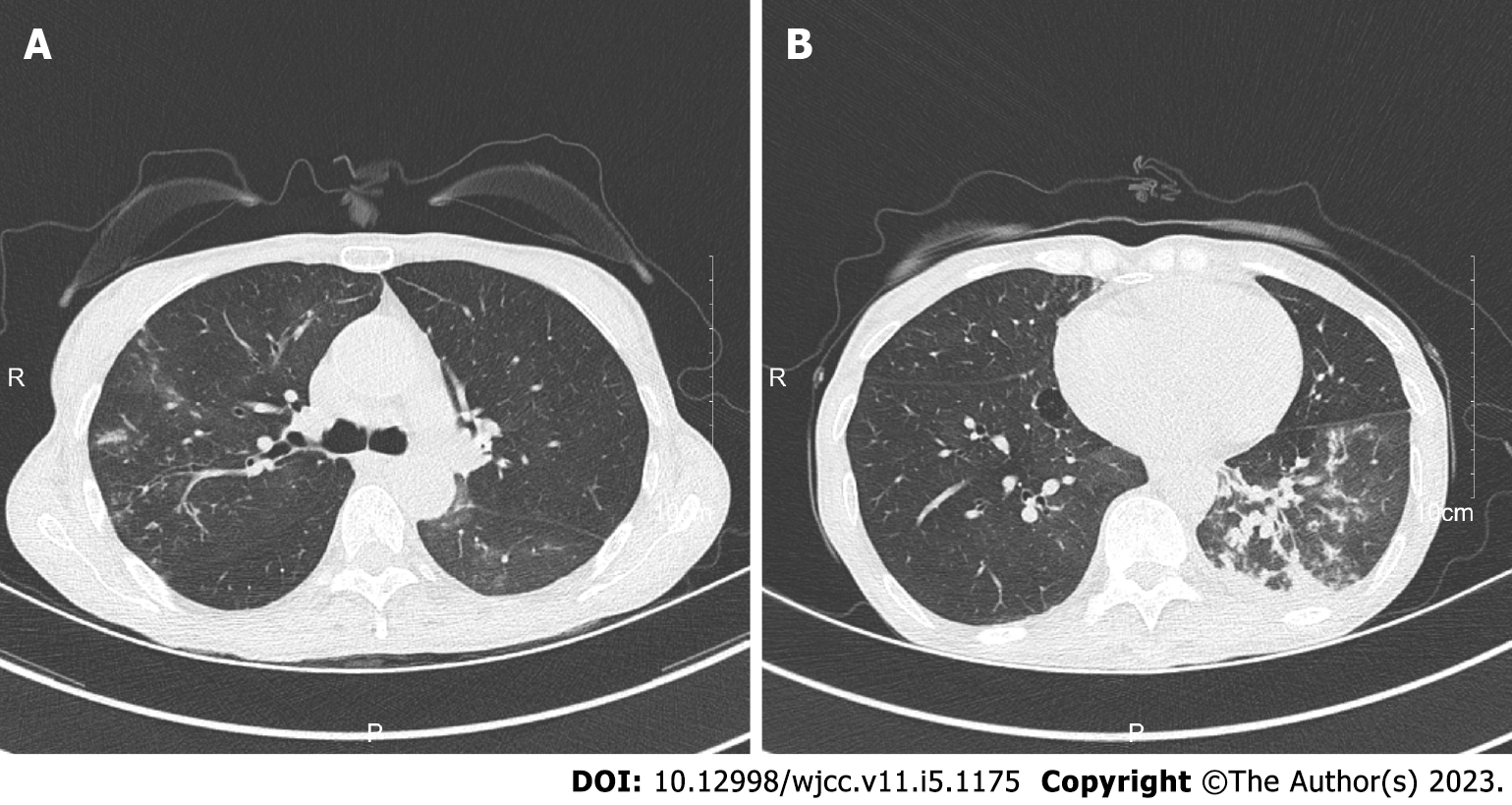
Computerized tomography showed multiple patchy, nodular and strip-shaped high-density shadows in the upper lobe of the right lung and the lower lobe of the left lung, multiple sputum thrombi in the bronchus of the lower lobe of the left lung, and small ground glass density nodules in both lungs (Figure 1).
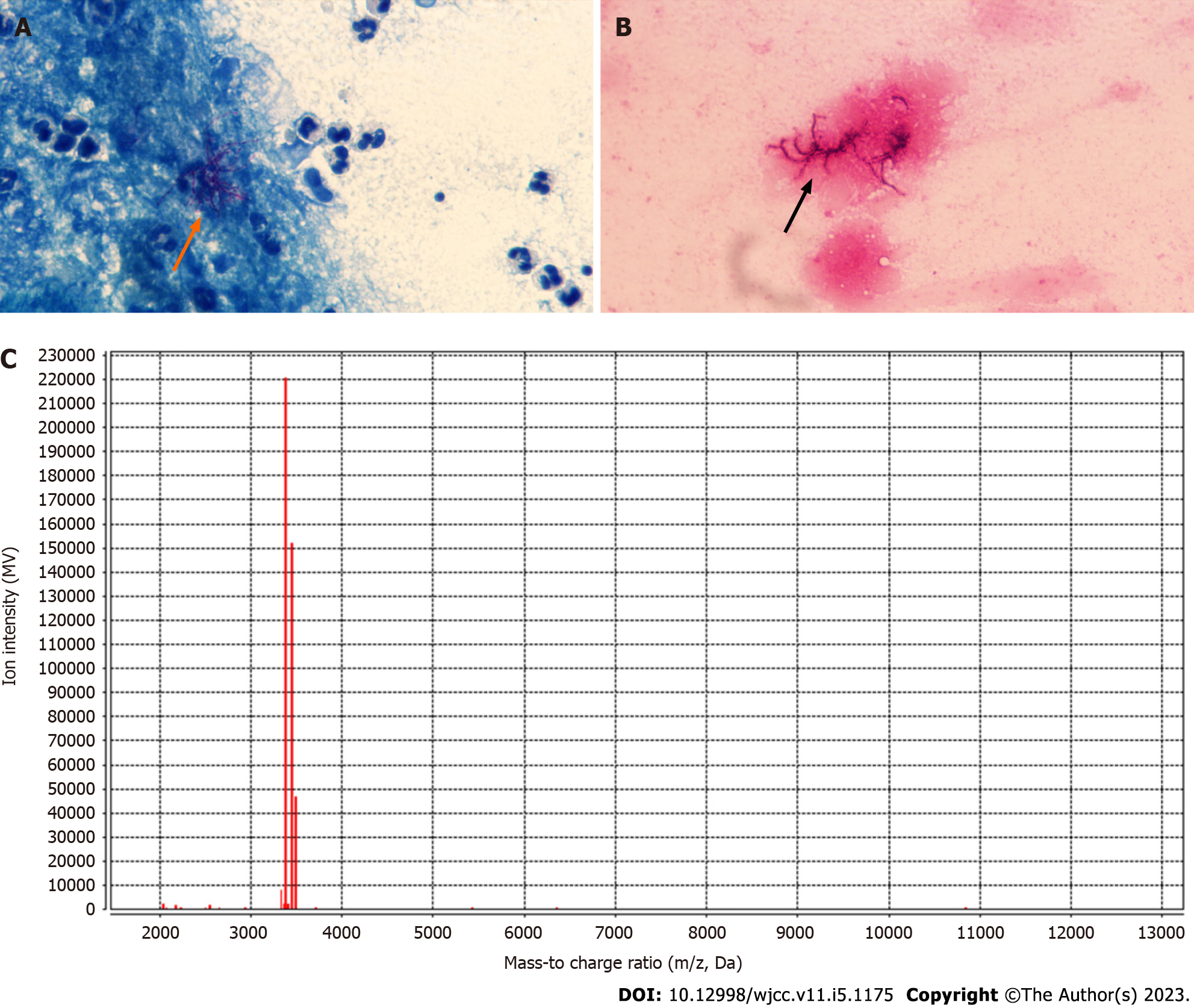
The patient underwent bronchoscopy, and positive acid-fast bifurcating filaments (Figure 2A) and branching gram-positive rods (Figure 2B) were observed in the bronchoalveolar lavage fluid (BALF) of the patient under an oil microscope (both ×1000 magnification). White waxy wrinkled colonies were observed by culture of the bronchoscope brush and BALF of the patient on the blood plate for 3 d, which were identified by matrix-assisted laser desorption ionization-time of fight mass spectrometry (MALDI-TOF MS) (bioMerieux, France) as N. cyriacigeorgica (Figure 2C). The Kirby-Bauer method was performed to determine the maximum zone of inhibition of the isolated N. cyriacigeorgica against amikacin, clarithromycin, imipenem, linezolid, and compound sulfamethoxazole (TMP-SMZ), and an Epsilometer test was performed to determine the minimum inhibitory concentration value of the isolated strain against levofloxacin (Table 2).
| Antibiotics | Method | Result |
| Amikacin | KB | 40 mm |
| Clarithromycin | KB | 35 mm |
| Ciprofloxacin | KB | 10 mm |
| Imipenem | KB | 40 mm |
| Linezolid | KB | 40 mm |
| Levofloxacin | E-test | 32 mm |
| TMP-SMZ | KB | 39 mm |
The patient was diagnosed with pulmonary nocardiosis caused by Nocardia cyriacigeorgica.
Compound sulfamethoxazole tablets (0.96 g) were given orally three times a day.
After one week of treatment, a routine blood examination showed that neutrophils (65.3%) and CRP (0.1 mg/L) had returned to normal; the patient's condition had improved significantly, and she was discharged.
A clear aetiology is particularly important for patients with recurrent fever, but the diagnosis of such patients is often challenging in clinical practice. The lung imaging features of our patient included multiple patchy, nodular and strip-shaped high-density shadows, multiple sputum thrombi and small ground glass density nodules in both lungs. However, manifestations of small or large consolidation shadows, single or multiple nodules, cavities with medium density or above, pulmonary abscess, hilar lymph node enlargement, pleural effusion, empyema, and pleural thickening are also common in fungal infection, pulmonary tuberculosis and other bacterial pneumonia[6-8]. Cough, bloody sputum, chest pain, fever, dyspnoea and empyema are also common in lung cancer patients[9]. It is usually impossible to determine whether there is Nocardia infection by imaging characteristics alone. The specific species of Nocardia can be accurately diagnosed by culture and mass spectrum identification, which are significant for clinical anti-infection treatment. This patient was initially diagnosed with community-acquired pneumonia and received routine antibiotic treatment; however, these antibiotics may not be effective against Nocardia. Sulfonamides are recommended as the first-line drug for patients with nocardiosis. The combination of linezolid will be considered for patients with disseminated nocardiosis or severe cases, while sulfonamides are often not selected as the preferred empirical drug for community-acquired pneumonia because of their side effects[10,11]. The patient obtained an ideal prognosis through compound sulfamethoxazole treatment. For grassroots hospitals, it is necessary to improve the understanding of Nocardia pneumonia. Because cases of Nocardia infection are relatively rare, the clinical laboratories in many grassroots hospitals may have low detection levels due to awareness limitations.
Nocardia widely exists in soil, saprophytes and sewage[12]. It is an obligate aerobic bacterium with positive Gram staining and weak acid-fast staining, which usually leads to opportunistic infection[13,14]. The susceptible population is mainly long-term use of corticosteroids or immunosuppressants, diabetes patients and broad-spectrum antibiotic maintenance patients[15-18]. In this case, the laboratory test of peripheral blood lymphocyte subsets showed that CD16+CD56+ NK cells and CD4+ T cells were significantly reduced compared with normal individuals, while CD19+ B cells were significantly increased, suggesting that the patient may have an immune disease. The CD4+ T cell count can reflect the immune function of patients to some extent. We should pay attention to the analysis of the immune status of patients with Nocardia because even after timely treatment with corresponding antibiotics, such patients will have a high probability of various infections in the future, so regular immunoglobulin treatment to improve immunity and other measures should be considered. However, at present, the prevention of immune infections in patients with recurrent fever in our country is deficient. Laboratory test results showed that the CD4+ T cells in our patient’s peripheral blood were almost completely absent, meaning that the function of helper T cells may have been completely lacking. It has been proven that helper T cells play a key role in the host response to invasion by pathogenic microorganisms and the initiation of anti-infection immunity[19]. For such patients, opportunistic infection is fatal.
An accurate aetiology is the key to treating patients with recurrent fever. Nocardia pneumonia, pulmonary tuberculosis and pulmonary fungal infection cannot be distinguished by pulmonary imaging characteristics alone. Culture and MALDI-TOF MS identification are important techniques for the laboratory diagnosis of pulmonary nocardiosis. Nocardia pneumonia caused by N. cyriacigeorgica infection is relatively rare in clinical practice. Special attention should be given to individuals with abnormal immune function. It is also important to improve the understanding of Nocardia pneumonia in grassroots hospitals.
We thank all members of the microbiology laboratory of Zhejiang Provincial People's Hospital for their help in the collection of clinical data and the fitness coach Hao-Tian Huang for his encouragement.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Microbiology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Cheng J, China; Nakaji K, Japan S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Peng Y, Dong X, Zhu Y, Lv H, Ge Y. A rare case of pulmonary nocardiosis comorbid with Sjogren's syndrome. J Clin Lab Anal. 2021;35:e23902. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Troumani Y, Touhami S, Beral L, David T. Corneal Nocardiosis mistaken for fungal infection. J Fr Ophtalmol. 2015;38:e7-e9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Lin J, Wu XM, Peng MF. Nocardia cyriacigeorgica infection in a patient with pulmonary sequestration: A case report. World J Clin Cases. 2021;9:2367-2372. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Yassin AF, Rainey FA, Steiner U. Nocardia cyriacigeorgici sp. nov. Int J Syst Evol Microbiol. 2001;51:1419-1423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 87] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Schlaberg R, Huard RC, Della-Latta P. Nocardia cyriacigeorgica, an emerging pathogen in the United States. J Clin Microbiol. 2008;46:265-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 87] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 6. | Ha YW, Kim CH, Park Y, Sohn JW, Kim MJ, Yoon YK. Rare case of pulmonary lymphomatoid granulomatosis in conjunction with tuberculosis: A case report. Medicine (Baltimore). 2017;96:e8323. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Liu L, Wu H, Liang J, Wu W, Peng Y, Zhou H, Li X. Rhizomucor pusillus Infection in a Patient with Acute Myeloid Leukaemia After Haematopoietic Stem Cell Transplantation: Clinical Impact of Metagenomics Next-Generation Sequencing. Infect Drug Resist. 2022;15:4285-4290. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (1)] |
| 8. | de Klerk KD, Bau S, Günther G. Diffuse pulmonary small nodular and patchy infiltrates on chest X-ray with hemoptysis: TB or not TB? Pan Afr Med J. 2018;30:121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Sun X, Liu H, Feng R, Peng M, Hou X, Wang P, Wang H, Xu W, Shi J. Biopsy-proven IgG4-related lung disease. BMC Pulm Med. 2016;16:20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Margalit I, Lebeaux D, Tishler O, Goldberg E, Bishara J, Yahav D, Coussement J. How do I manage nocardiosis? Clin Microbiol Infect. 2021;27:550-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 99] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 11. | Root H, Daniels L, Marx A, Bartelt LA, Lachiewicz AM, van Duin D. Sulfonamides without trimethoprim in the treatment of Nocardia infections: A case report and literature review. Transpl Infect Dis. 2021;23:e13452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Lerner PI. Nocardiosis. Clin Infect Dis. 1996;22:891-903; quiz 904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 422] [Cited by in RCA: 419] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 13. | Pan B, Wang FF, He Q. Case report: Nocardia farcinica pneumonia in early-stage post liver transplantation. Front Med (Lausanne). 2022;9:996045. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 14. | Yan H, Li Z, Xia H, Li Q, Bai H. A case report on mixed pulmonary infection of Nocardia nova, Mycobacterium tuberculosis, and Aspergillus fumigatus based on metagenomic next-generation sequencing. Front Public Health. 2022;10:927338. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 15. | Zhang L, Yang Y, Huang S. Disseminated Nocardia farcinica infection in a patient with EGPA receiving hormonotherapy. Lancet Infect Dis. 2021;21:148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Kurosawa S, Sekiya N, Doki N, Yaguchi T, Kishida Y, Nagata A, Yamada Y, Konishi T, Kaito S, Yoshifuji K, Shirane S, Uchida T, Inamoto K, Toya T, Igarashi A, Najima Y, Muto H, Kobayashi T, Kakihana K, Sakamaki H, Ohashi K. The emergence of rare nocardiosis following allogeneic hematopoietic stem cell transplantation in the era of molecular taxonomy. Int J Infect Dis. 2019;89:154-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Muggia VA, Puius YA. Nocardia ignorata Infection in Heart Transplant Patient. Emerg Infect Dis. 2020;26:2788-2789. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Senard O, Blanot S, Jouvion G, Rodriguez-Nava V, Lortholary O, Join-Lambert O, Toubiana J. Fulminant Nocardiosis Due to a Multidrug-Resistant Isolate in a 12-Year-Old Immunocompetent Child. Pediatrics. 2018;141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 19. | Morita R, Schmitt N, Bentebibel SE, Ranganathan R, Bourdery L, Zurawski G, Foucat E, Dullaers M, Oh S, Sabzghabaei N, Lavecchio EM, Punaro M, Pascual V, Banchereau J, Ueno H. Human blood CXCR5(+)CD4(+) T cells are counterparts of T follicular cells and contain specific subsets that differentially support antibody secretion. Immunity. 2011;34:108-121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1342] [Cited by in RCA: 1291] [Article Influence: 92.2] [Reference Citation Analysis (0)] |