Published online Feb 16, 2023. doi: 10.12998/wjcc.v11.i5.1158
Peer-review started: November 8, 2022
First decision: November 23, 2022
Revised: December 6, 2022
Accepted: January 20, 2023
Article in press: January 20, 2023
Published online: February 16, 2023
Processing time: 97 Days and 17.1 Hours
Endoscopic submucosal dissection (ESD) post-procedure stricture is a relatively common long-term complication following ESD treatment. A range of approaches has been implemented for the treatment of post-procedural stricture using endoscopic techniques such as endoscopic dilation, self-expandable metallic stent insertion, local steroid injection in the esophagus, oral steroid administration, radial incision and cutting (RIC). The actual efficacy of these different therapeutic options is highly variable, and uniform international standards for the prevention or treatment of stricture.
In this report, we describe the case of a 51-year-old male diagnosed with early esophageal cancer. To protect against esophageal stricture, the patient was administered oral steroids and underwent self-expandable metallic stent insertion for 45 d. Despite these interventions, stricture was detected at the lower edge of the stent following its removal. The patient remained refractory to multiple rounds of endoscopic bougie dilation treatment, and thus suffered from complex refractory benign esophageal stricture. As such, RIC combined with bougie dilation and steroid injection was employed to treat this patient more effectively, ultimately achieving satisfactory therapeutic efficacy.
Combination of RIC, dilation, and steroid injection can be safely and effectively implemented to treat cases of post-ESD refractory esophageal stricture.
Core Tip: Endoscopic submucosal dissection post-procedure stricture is one of the most common long-term complications of the procedure. At present, there is no uniform international standard on how to effectively prevent and treat stricture after resection of large esophageal lesions. we selected to attempt to treat complex refractory esophageal stricture through a combination of radial incision and cutting, dilation, and steroid injection. Satisfactory results were achieved.
- Citation: Pu WF, Zhang T, Du ZH. Combined treatment of refractory benign stricture after esophageal endoscopic mucosal dissection: A case report. World J Clin Cases 2023; 11(5): 1158-1164
- URL: https://www.wjgnet.com/2307-8960/full/v11/i5/1158.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i5.1158
Advances in the endoscopic submucosal dissection (ESD) procedure have led to its canonization as the primary treatment for individuals diagnosed with superficial esophageal cancer[1,2]. However, ESD treatment can result in esophageal stricture, limiting the ability of patients to swallow while increasing their healthcare costs and lowering their overall quality of life. Independent risk factors known to be associated with the onset of post-ESD esophageal strictures include tumors that bypass the esophageal lamina propria mucosal layer or esophageal mucosal defects that cover over 75% of the esophageal circumference and are at least 30 mm in length[3-5]. For ESD procedures covering over 75% of the esophageal circumference, stricture rates are as high as 83.3%-94.1%[6]. A number of treatments for post-ESD esophageal stricture have been developed, with some levels of varying efficacy. However, no reports have yet described the treatment of a case of refractory stricture via radial incision and cutting (RIC) in combination with dilation and steroid injection.
Recurrent dysphagia.
Examination of the patient revealed esophageal mucosal congestion and erosion 28-35 cm from his incisors. Pathological examination revealed severe squamous cell dysplasia of the esophageal mucosa. To mitigate the risk of esophageal stricture development following the ESD procedure, the patient was administered oral 30 mg prednisone acetate tablets for 3 d after surgery with a gradual reduction over 8 wk. Five days after the procedure, the patient underwent self-expandable metallic stent insertion which remained in place for 45 d. However, following stent removal, gastroscopy showed the presence of stricture at the lower edge of the stent. The patient underwent repeated endoscopic bougie dilation procedures in our hospital without any significant effect. Given this repeated treatment failure, we decided to attempt to treat this patient through a combination of RIC, dilation, and steroid injection.
The patient did not have any history of esophageal cancer or any relevant family or genetic history.
Physical examination revealed no abnormalities.
The levels of squamous cell carcinoma antigen and Elccsys CYFRA21-1 were normal.
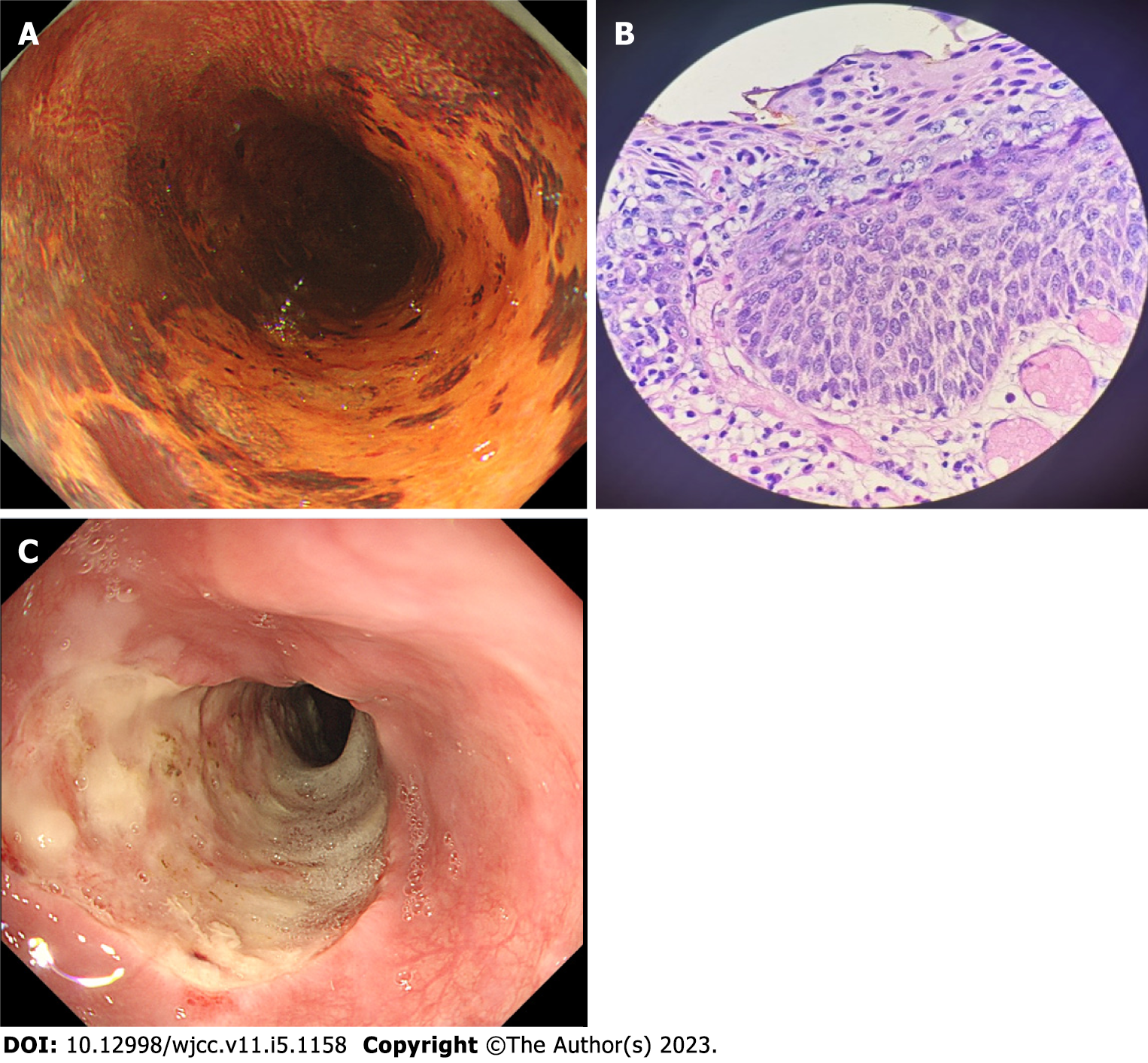
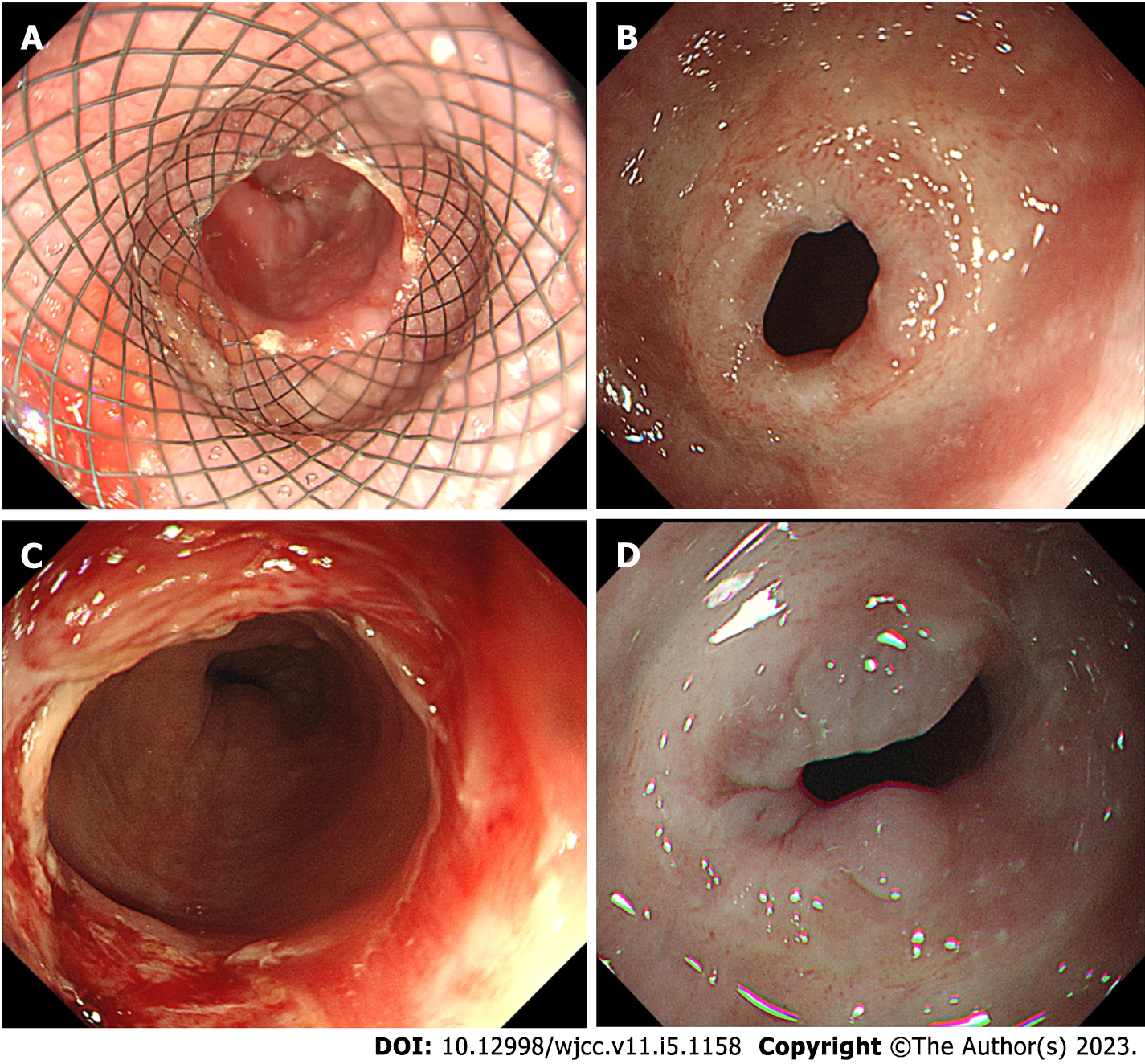
Iodine staining showed that the lesion, located 28-35 cm from the incisors, extended to almost two-thirds of the esophageal circumference with a longitudinal length before treatment of about 7 cm (Figure 1A). Pathological examination revealed severe squamous cell dysplasia of the esophageal mucosa (Figure 1B). The longitudinal length of the mucosal defect after ESD was about 8 cm. After discussion of the methods for preventing postoperative stricture, family members and patients requested stent implantation ESD was conducted and en bloc lesion resection was performed (Figure 1C). Five days after ESD, a silicone-coated esophageal stent system (Micro-Tech [Nanjing] Co., Ltd) was implanted; the stent length was 120 mm with a diameter of 20 mm) (Figure 2A). After removal of the stent, Gastroscope revealed an esophageal stricture 37 cm from the incisors. The site of the stricture was covered by the stent preventing the passage of the gastroscope through the esophagus (Figure 2B). The patient underwent three bougie dilations using an esophagocardiac stricture dilator at intervals of approximately 10 d. Although each time this resulted in a 13 mm expansion (Figure 2C), the procedure was not effective (Figure 2D).
Benign stricture of the esophagus.
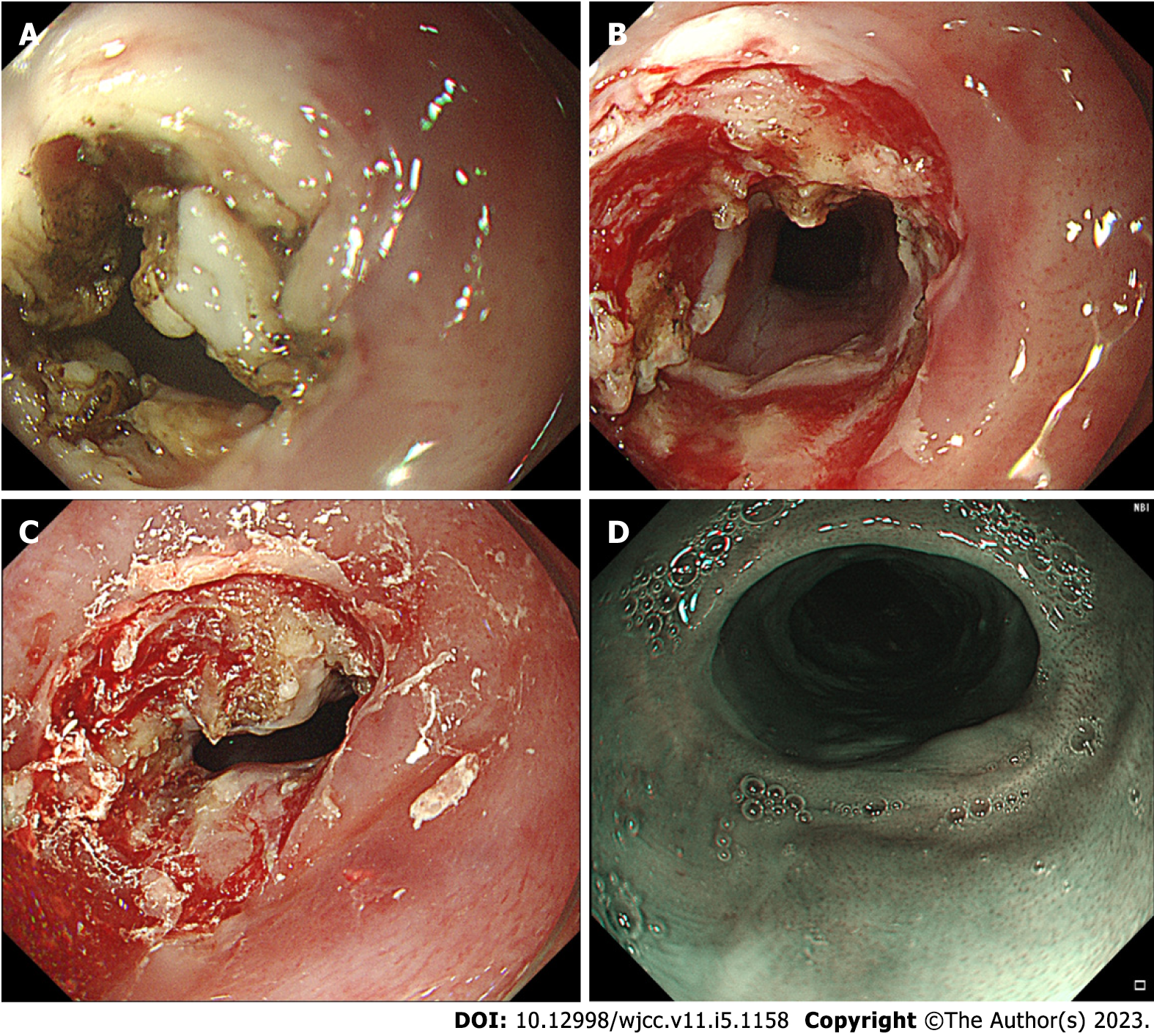
As the patient suffered from severe dysphagia, we ultimately decided after approximately two and a half months to perform an RIC. This was done using an Olympus IT Knife 2, KD-611L, and an ERBE VIO 200 S high-frequency selectrical cutting device. This was done to remove the scar tissue together with expansion treatment to fully open the stricture ring, after which an 80 mg (2 mL) Triamcinolone Acetonide steroid injection was administered at the stricture surface and surrounding mucosa to prevent scar formation (Figure 3A-C).
After this combined treatment procedure, the patient was able to eat normally. At three months post-treatment, white scar formation was observed in the esophagus, but the gastroscope was able to pass without any resistance (Figure 3D). During the one-year follow-up, the patient did not experience any dysphagia or related symptoms.
Endoscopic resection has emerged as an increasingly common treatment for precancerous lesions and early esophageal cancer cases, conferring the same benefits as more invasive surgical treatment[7-9]. However, high esophageal stricture rates in patients who undergo such treatment remain a pressing clinical challenge[10]. In an effort to prevent post-ESD stricture development, Ezoe et al[11] implemented an endoscopic balloon dilatation (EBD) strategy but found that 59% of patients still developed stricture even if they had undergone six rounds of prophylactic EBD. Endoscopic dilatation is a relatively straightforward procedure that can effectively prevent or treat post-ESD esophageal stricture in many cases. However, this procedure does carry some risk of perforation, and repeated treatment is often required. Stent placement can also reduce the incidence of post-ESD esophageal stricture and lower the need for EBD procedures, but can result in adverse events including stent displacement, chest pain, esophageal perforation, and bleeding[9,10,12]. Several recent reports have described RIC as a novel means of treating refractory cases of rectal or esophageal stricture, allowing for the excision of fibrotic tissue in the target site[13-17]. Yano et al[18] successfully employed a radial resection approach to treat esophageal stricture cases in 8 patients, markedly alleviating their postoperative dysphagia[18]. Moreover, Hashimoto et al[19] first employed steroid injection as a strategy aimed at preventing esophageal stricture development following ESD, reporting a decrease in stricture rates from 75% in control patients to 19% in those that underwent multiple local triamcinolone acetonide injections[19]. Hanaoka et al[20] additionally found that a single round of local triamcinolone acetonide injection was associated with a 10% stricture rate[20]. Delayed perforation is the most significant potential safety concern associated with this local injection approach. Combining oral steroids and localized injections can aid in the prevention of refractory stricture, as demonstrated in a study showing a refractory stricture rate of 30.6% in control patients (11/36) but none in the steroid treatment group (P < 0.001)[21]. Steroids are capable of inhibiting the regeneration of fibroblasts within scar tissue regions, facilitating the degradation of collagen while suppressing collagen synthesis and slowing scar growth. Regenerative medicine strategies are also being increasingly studied to prevent and treat post-ESD esophageal stricture cases[22-24].
Combination of RIC, dilation, and steroid injection can be safely and effectively implemented to treat cases of post-ESD refractory esophageal stricture.
We highly appreciate Dr. Xiao-Guang Guo (Department of Pathology, Nanchong Center Hospital) for providing professional guidance in the pathological diagnosis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Chiba H, Japan; Hamaya Y, Japan; Hikichi T, Japan S-Editor: Li L L-Editor: A P-Editor: Li L
| 1. | Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53206] [Cited by in RCA: 55666] [Article Influence: 7952.3] [Reference Citation Analysis (132)] |
| 2. | Alsop BR, Sharma P. Esophageal Cancer. Gastroenterol Clin North Am. 2016;45:399-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 146] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 3. | Isomoto H, Yamaguchi N, Minami H, Nakao K. Management of complications associated with endoscopic submucosal dissection/ endoscopic mucosal resection for esophageal cancer. Dig Endosc. 2013;25 Suppl 1:29-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 97] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 4. | Mizuta H, Nishimori I, Kuratani Y, Higashidani Y, Kohsaki T, Onishi S. Predictive factors for esophageal stenosis after endoscopic submucosal dissection for superficial esophageal cancer. Dis Esophagus. 2009;22:626-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 146] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 5. | Chen M, Dang Y, Ding C, Yang J, Si X, Zhang G. Lesion size and circumferential range identified as independent risk factors for esophageal stricture after endoscopic submucosal dissection. Surg Endosc. 2020;34:4065-4071. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 6. | Zhang Y, Zhang B, Wang Y, Zhang J, Wu Y, Xiao T, Liao Y, Bao Y, Qiu H, Sun S, Guo J. Advances in the Prevention and Treatment of Esophageal Stricture after Endoscopic Submucosal Dissection of Early Esophageal Cancer. J Transl Int Med. 2020;8:135-145. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | Ning B, Abdelfatah MM, Othman MO. Endoscopic submucosal dissection and endoscopic mucosal resection for early stage esophageal cancer. Ann Cardiothorac Surg. 2017;6:88-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 56] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 8. | Huntington JT, Walker JP, Meara MP, Hazey JW, Melvin WS, Perry KA. Endoscopic mucosal resection for staging and treatment of early esophageal carcinoma: a single institution experience. Surg Endosc. 2015;29:2121-2125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Wen J, Lu Z, Yang Y, Liu Q, Yang J, Wang S, Wang X, Du H, Meng J, Wang H, Linghu E. Preventing stricture formation by covered esophageal stent placement after endoscopic submucosal dissection for early esophageal cancer. Dig Dis Sci. 2014;59:658-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 65] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 10. | Chai NL, Feng J, Li LS, Liu SZ, Du C, Zhang Q, Linghu EQ. Effect of polyglycolic acid sheet plus esophageal stent placement in preventing esophageal stricture after endoscopic submucosal dissection in patients with early-stage esophageal cancer: A randomized, controlled trial. World J Gastroenterol. 2018;24:1046-1055. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 27] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 11. | Ezoe Y, Muto M, Horimatsu T, Morita S, Miyamoto S, Mochizuki S, Minashi K, Yano T, Ohtsu A, Chiba T. Efficacy of preventive endoscopic balloon dilation for esophageal stricture after endoscopic resection. J Clin Gastroenterol. 2011;45:222-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 134] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 12. | Yang YG, Liu CF, Hu JH. Polyglycolic acid sheet plus esophageal stent presents with higher efficacy in preventing esophageal stricture post endoscopic submucosal dissection compared with stent placement alone in early-stage esophageal cancer patients. Int J Clin Exp Med. 2019;12:762-770. |
| 13. | Mizusawa T, Kobayashi M, Terai S. Radial incision and cutting for refractory benign esophageal stricture. Dig Endosc. 2019;31:e46-e47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Jia Y, Chen C, Jin P, Yu D, Wang L, Li S, Sheng J. Endoscopic radial incision combined with dexamethasone therapy for stricture of the esophagus caused by Crohn's disease. Endoscopy. 2019;51:E309-E310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Minamino H, Machida H, Tominaga K, Sugimori S, Okazaki H, Tanigawa T, Yamagami H, Watanabe K, Watanabe T, Fujiwara Y, Arakawa T. Endoscopic radial incision and cutting method for refractory esophageal stricture after endoscopic submucosal dissection of superficial esophageal carcinoma. Dig Endosc. 2013;25:200-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Lee TH, Lee SH, Park JY, Lee CK, Chung IK, Kim HS, Park SH, Kim SJ, Hong SJ, Lee MS. Primary incisional therapy with a modified method for patients with benign anastomotic esophageal stricture. Gastrointest Endosc. 2009;69:1029-1033. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 51] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 17. | Muto M, Ezoe Y, Yano T, Aoyama I, Yoda Y, Minashi K, Morita S, Horimatsu T, Miyamoto S, Ohtsu A, Chiba T. Usefulness of endoscopic radial incision and cutting method for refractory esophagogastric anastomotic stricture (with video). Gastrointest Endosc. 2012;75:965-972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 94] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 18. | Yano T, Yoda Y, Satake H, Kojima T, Yagishita A, Oono Y, Ikematsu H, Kaneko K. Radial incision and cutting method for refractory stricture after nonsurgical treatment of esophageal cancer. Endoscopy. 2013;45:316-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 19. | Hashimoto S, Kobayashi M, Takeuchi M, Sato Y, Narisawa R, Aoyagi Y. The efficacy of endoscopic triamcinolone injection for the prevention of esophageal stricture after endoscopic submucosal dissection. Gastrointest Endosc. 2011;74:1389-1393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 227] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 20. | Hanaoka N, Ishihara R, Takeuchi Y, Uedo N, Higashino K, Ohta T, Kanzaki H, Hanafusa M, Nagai K, Matsui F, Iishi H, Tatsuta M, Ito Y. Intralesional steroid injection to prevent stricture after endoscopic submucosal dissection for esophageal cancer: a controlled prospective study. Endoscopy. 2012;44:1007-1011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 195] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 21. | Chu Y, Chen T, Li H, Zhou P, Zhang Y, Chen W, Zhong Y, Yao L, Xu M. Long-term efficacy and safety of intralesional steroid injection plus oral steroid administration in preventing stricture after endoscopic submucosal dissection for esophageal epithelial neoplasms. Surg Endosc. 2019;33:1244-1251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 22. | Saito Y, Tanaka T, Andoh A, Minematsu H, Hata K, Tsujikawa T, Nitta N, Murata K, Fujiyama Y. Novel biodegradable stents for benign esophageal strictures following endoscopic submucosal dissection. Dig Dis Sci. 2008;53:330-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 108] [Article Influence: 6.4] [Reference Citation Analysis (1)] |
| 23. | Ohki T, Yamato M, Ota M, Takagi R, Murakami D, Kondo M, Sasaki R, Namiki H, Okano T, Yamamoto M. Prevention of esophageal stricture after endoscopic submucosal dissection using tissue-engineered cell sheets. Gastroenterology. 2012;143:582-588.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 336] [Cited by in RCA: 354] [Article Influence: 27.2] [Reference Citation Analysis (0)] |
| 24. | Barret M, Pratico CA, Camus M, Beuvon F, Jarraya M, Nicco C, Mangialavori L, Chaussade S, Batteux F, Prat F. Amniotic membrane grafts for the prevention of esophageal stricture after circumferential endoscopic submucosal dissection. PLoS One. 2014;9:e100236. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |