Published online Feb 16, 2023. doi: 10.12998/wjcc.v11.i5.1137
Peer-review started: October 23, 2022
First decision: December 13, 2022
Revised: December 21, 2022
Accepted: January 16, 2023
Article in press: January 16, 2023
Published online: February 16, 2023
Processing time: 113 Days and 11.3 Hours
Thymolipoma is a rare benign tumor arising from the anterior mediastinal thymus and is composed of mature fatty tissue and interspersed nonneoplastic thymic tissue. This tumor accounts for only a small percentage of mediastinal masses, and the majority of them are asymptomatic and found incidentally. To date, fewer than 200 cases have been published in the world literature, of which most excised tumors weighed less than 0.5 kg and the largest weighed 6 kg.
A 23-year-old man presented with a complaint of progressive breathlessness for 6 mo. His forced vital capacity was only 23.6% of the predicted capacity, and his arterial partial pressure of oxygen and carbon dioxide were 51 and 60 mmHg, respectively, without oxygen inhalation. Chest computed tomography revealed a large fat-containing mass in the anterior mediastinum that measured 26 cm × 20 cm × 30 cm in size and occupied most of the thoracic cavity. Percutaneous mass biopsy revealed only thymic tissue without signs of malignancy. A right posterolateral thoracotomy was successfully performed to remove the tumor along with the capsule, and the excised tumor weighed 7.5 kg, which to our knowledge, was the largest surgically removed tumor of thymic origin. Postoperatively, the patient’s shortness of breath was resolved, and the histopathological diagnosis was thymolipoma. No signs of recurrence were observed at the 6-mo follow-up.
Giant thymolipoma causing respiratory failure is rare and dangerous. Despite the high risks, surgical resection is feasible and effective.
Core Tip: Thymolipoma is a rare benign tumor originating from the anterior mediastinal thymus that can occasionally grow to a massive size. Surgical resection is the only feasible and curative treatment modality. Here, we report a very rare case of thymolipoma that caused respiratory insufficiency by compressing most of the lungs. A right posterolateral thoracotomy was successfully performed, and the completely excised tumor weighed 7.5 kg, which made it the largest reported thymus neoplasm to our knowledge.
- Citation: Gong LH, Wang WX, Zhou Y, Yang DS, Zhang BH, Wu J. Surgical resection of a giant thymolipoma causing respiratory failure: A case report. World J Clin Cases 2023; 11(5): 1137-1143
- URL: https://www.wjgnet.com/2307-8960/full/v11/i5/1137.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i5.1137
Thymolipoma is a rare, slow-growing, benign tumor arising from the anterior mediastinal thymus and is composed of mature fatty tissue and interspersed nonneoplastic thymic tissue[1,2]. Since thymolipomas are soft and noninvasive, the majority of them are clinically quiescent. However, when the tumor becomes too large, it can compress the lungs and cause respiratory symptoms[3]. Surgical resection is the only curative treatment for thymolipomas, and depending on the tumor size and site, various surgical approaches have been reported[1,4]. Here, we report a case of thymolipoma in a 23-year-old male. The tumor weighed more than 7 kg, and to our knowledge, it was the largest reported excised tumor of thymic origin, including various benign and malignant thymic neoplasms[5-9]. The mass was too large for en bloc resection by a sternotomy, so a posterolateral incision for piecemeal resection was selected as the surgical technique.
A 23-year-old Chinese man presented to the hospital with complaints of gradually increasing breathlessness for 6 mo.
One day prior to admission, the patient presented to a local hospital with a complaint of gradually increasing breathlessness for 6 mo, especially after activity. The patient had no history of cough, blood in the sputum, chest tightness, pain, fever, night sweats, weight loss, loss of appetite, or other systemic symptoms. A chest computed tomography (CT) scan revealed a large mass in the anterior mediastinum that occupied all of the right thoracic cavity and part of the left thoracic cavity. Liposarcoma or fibrosarcoma was initially suspected. For further diagnosis and treatment, the patient was then admitted to the Thoracic Medicine Department of our hospital through an outpatient route.
The patient denied any previous surgery, trauma, or other previous significant medical history.
The patient denied any remarkable family history of related diseases.
On physical examination, the results were as follows: Height, 175 cm; weight, 70 kg; body temperature, 36.2 °C; heart rate, 76 beats per min; respiratory rate, 25 breaths per min; and blood pressure, 145/85 mmHg. The superficial lymph nodes, including the supraclavicular and neck lymph nodes, were not palpable. The chest wall was symmetrical without any deformities, and the patient’s breathing was regular. No breath sounds were heard over the right lung field, and the percussion sounds over the right chest were dull. The other physical examination results were unremarkable.
The laboratory testing results were as follows: Hemoglobin, 166 g/L; and hematocrit, 51.7%. Twelve tumor markers, including alpha-fetoprotein, carcinoembryonic antigen, neuron specific enolase, cancer antigen (CA)125, CA15-3, CA242, CA19-9, prostate specific antigen, free-prostate specific antigen, ferritin, beta-human chorionic gonadotropin, and human growth hormone, as measured by protein biochip detection in the serum, were normal. The arterial blood gas analysis without oxygen inhalation results were as follows: pH 7.37, oxygen saturation 85%, partial pressure of carbon dioxide 60 mmHg, partial pressure of oxygen 51 mmHg, bicarbonate 34.7 mmol/L, and base excess 6 mmol/L. The pulmonary function test results were as follows: Forced vital capacity 1.2 L (23.6% predicted), forced expiratory volume in 1 s 0.91 L (21.1% predicted), and vital capacity 1.2 L (22.6% predicted). The other findings from the routine laboratory examinations were within the normal range.
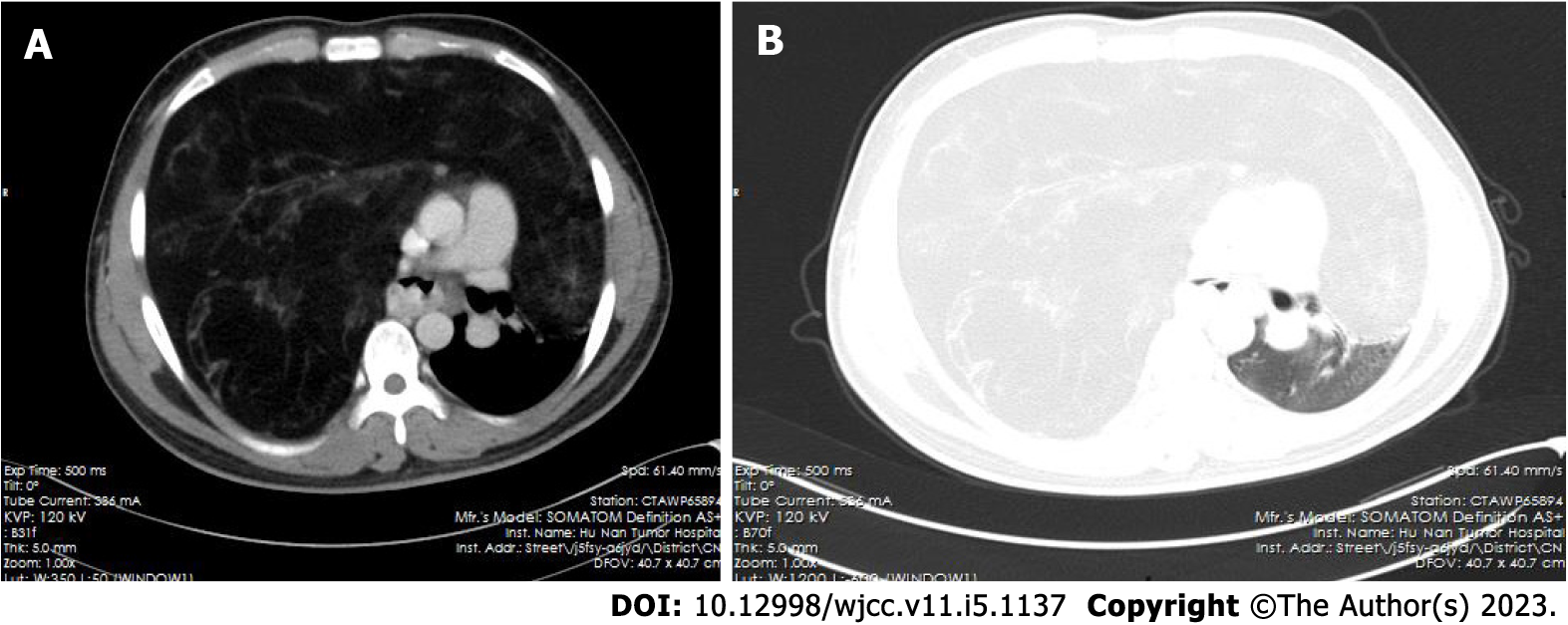
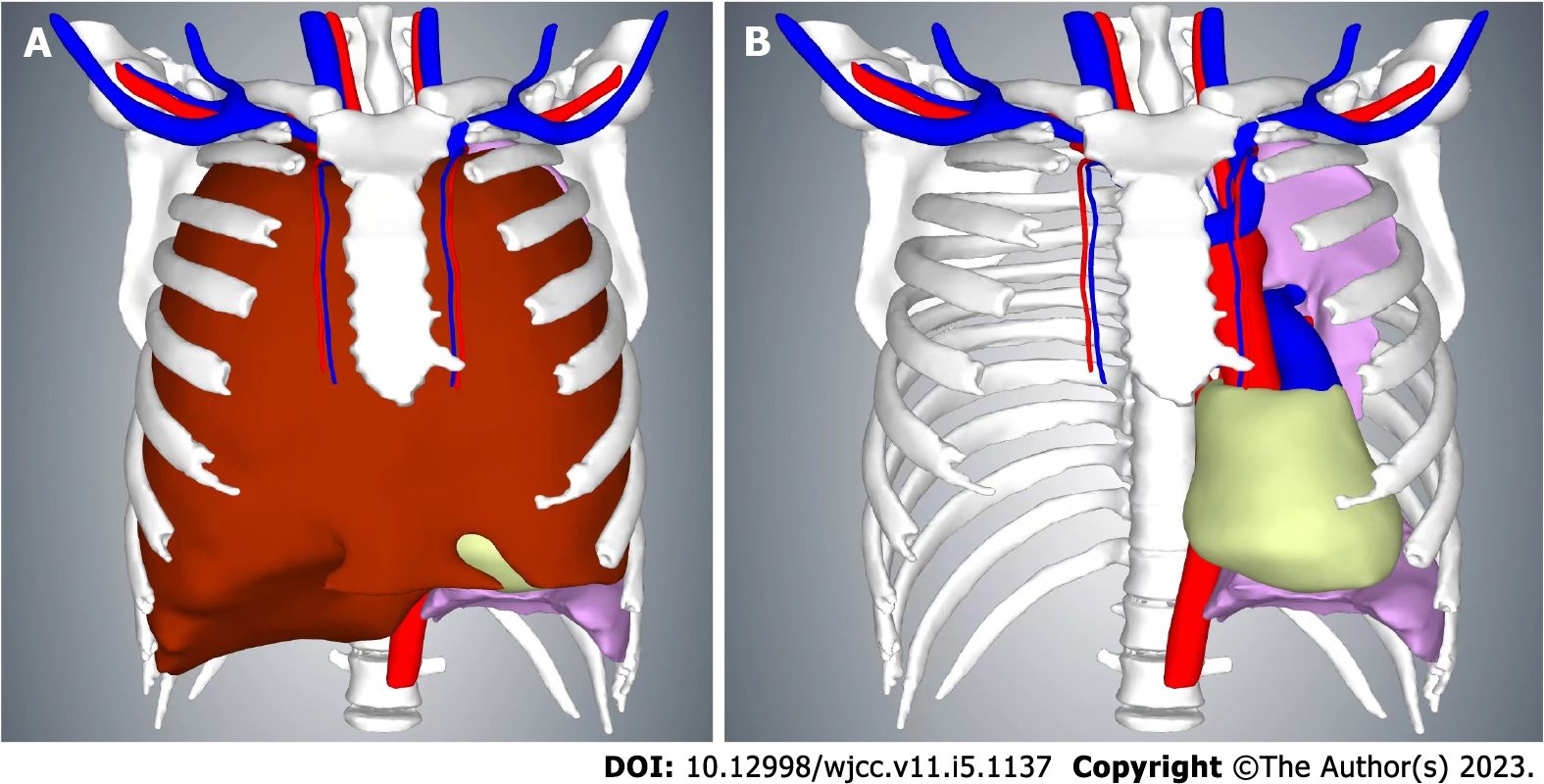
A high-resolution chest contrast-enhanced CT taken in our hospital revealed a large fat-containing mass in the anterior mediastinum, which was approximately 26 cm × 20 cm × 30 cm in size. It occupied almost the entirety of the right thoracic cavity and part of the left thoracic cavity with a clear boundary, and the tumor caused lung collapse and mediastinal shift (Figures 1 and 2). Bronchoscopy showed no tracheal neoplasms, the distal end of the trachea and the carina were compressed and twisted, and the bronchial lumen of the right lung was narrowed to varying degrees by the pressure from an external mass. Magnetic resonance imaging of the head and CT scans of the neck, abdomen, and pelvis showed no obvious abnormalities. The bone scan was also negative.
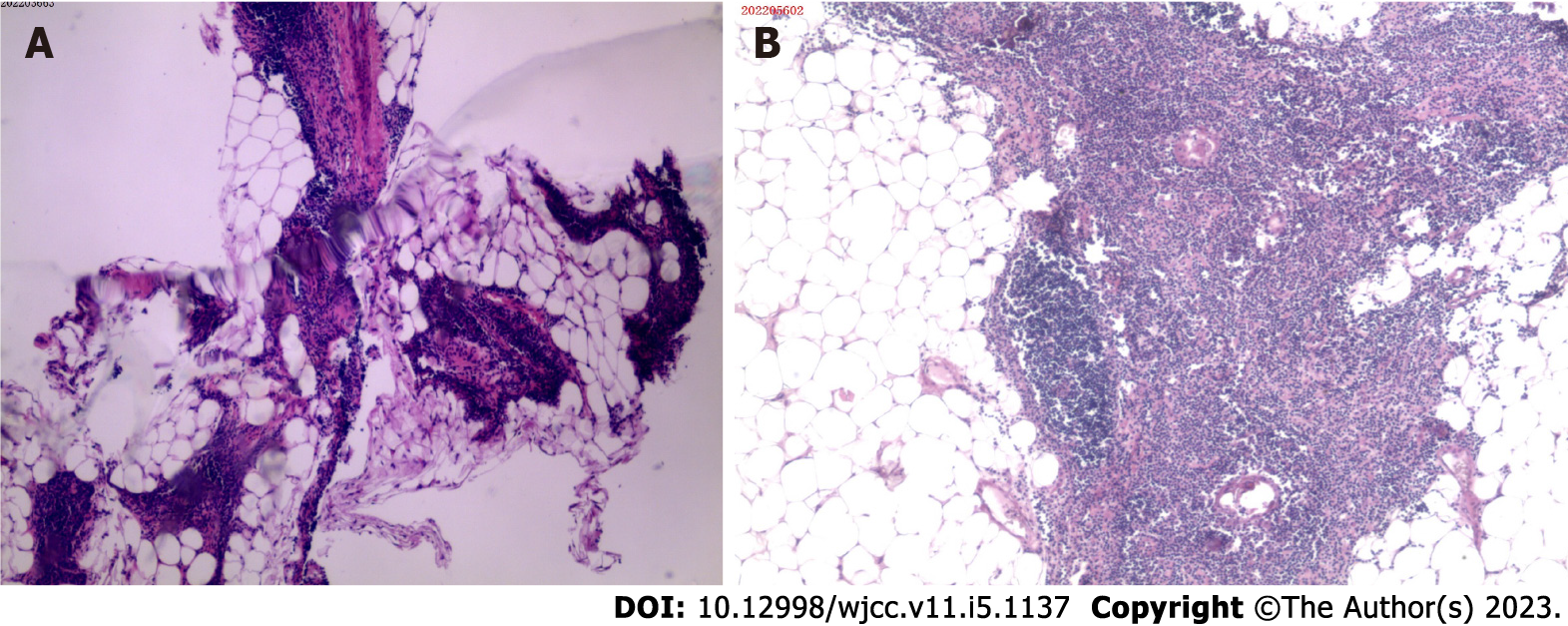
The histopathological results of CT-guided percutaneous thoracic mass biopsy revealed thymic tissue with calcification, and no definite malignancy was found (Figure 3A). Based on the above examination results, the multidisciplinary team concluded that the patient’s anterior mediastinal mass was likely a benign tumor; these types of tumors are not sensitive to radiotherapy and chemotherapy, so surgical resection was recommended. The patient was subsequently transferred to the Department of Thoracic Surgery for surgical treatment.
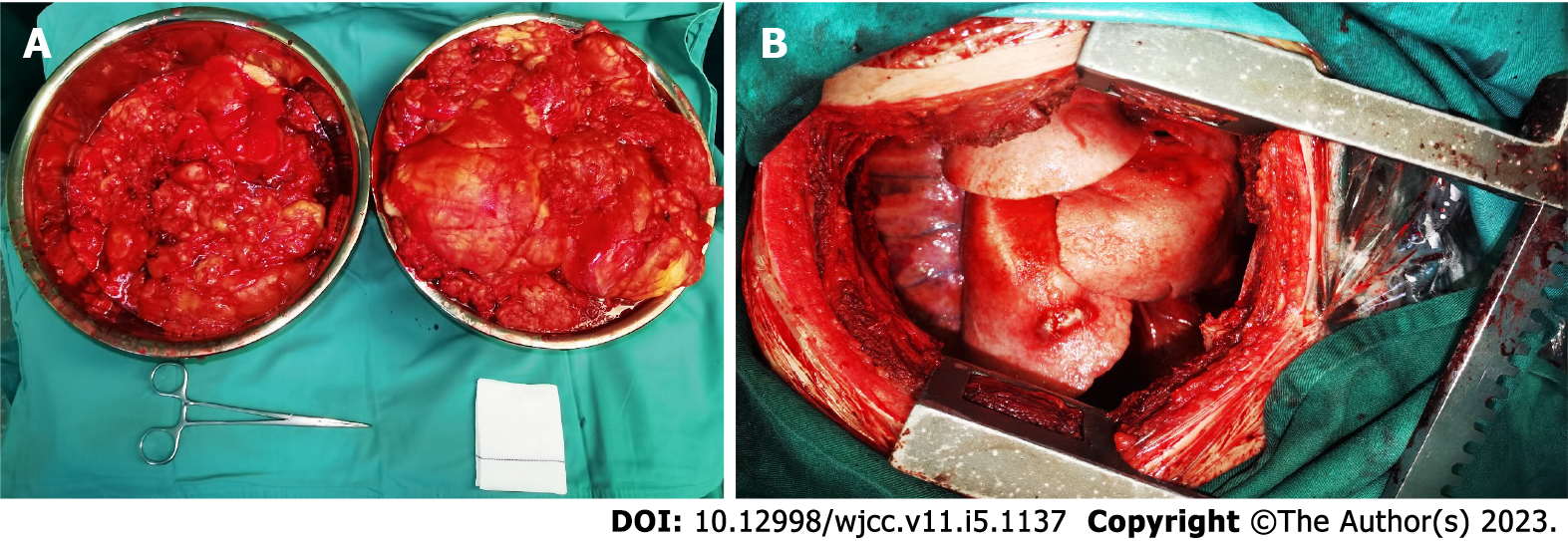
The patient’s anterior mediastinal mass was too large for en bloc resection by a sternotomy. We performed a right posterolateral thoracotomy through the fifth intercostal space and removed part of the fifth rib to enlarge the surgical incision. Subsequent thoracic exploration revealed a large, lobulated, and intact encapsulated lipomatous-like mass originating from the anterior mediastinum, and the mass compressed the heart and lungs. The mass occupied approximately 100% of the right thoracic cavity and 50% of the left thoracic cavity, resulting in a leftward shift of the mediastinum, complete collapse of the right lung, and partial collapse of the left lung. We incised the tumor capsule, removed the portion of the tumor that was in the right thoracic cavity in pieces, and then completely resected the remaining tumor along with the capsule. The excised tumor weighed 7.5 kg (Figure 4). After tumor resection, the right lung was slowly re-expanded without pressurized ventilation to avoid acute pulmonary edema. Two drainage tubes were placed in the right 8th intercostal space. The intraoperative blood loss was approximately 800 mL, and 4 U of concentrated red blood cells and 300 mL of plasma were infused. There were no postoperative complications, the drainage tubes were removed 4 d after surgery, and the patient was discharged 1 d later.
The postoperative histopathological examination revealed that the tumor had an intact capsule and was predominantly composed of mature adipose tissue intermixed with septa of atrophic thymus tissue containing lymphocytes and Hassall’s corpuscles (Figure 3B). The results of immunohistochemical analysis were as follows: TTF-1 (-), EMA (-), Ki67 hot spot (60%), P63 (partial +), CD5 (+), TdT (partial +), CK19 (+), CK5/6 (+), CD20 (+), CD3 (partial +), CD117 (-), CD99 (partial +), CD1a (partial +), CK-P (+), and CK7 (-). Based on the clinical manifestations, as well as laboratory, imaging, and histopathological examinations, the patient’s anterior mediastinal mass was ultimately diagnosed as a thymolipoma.
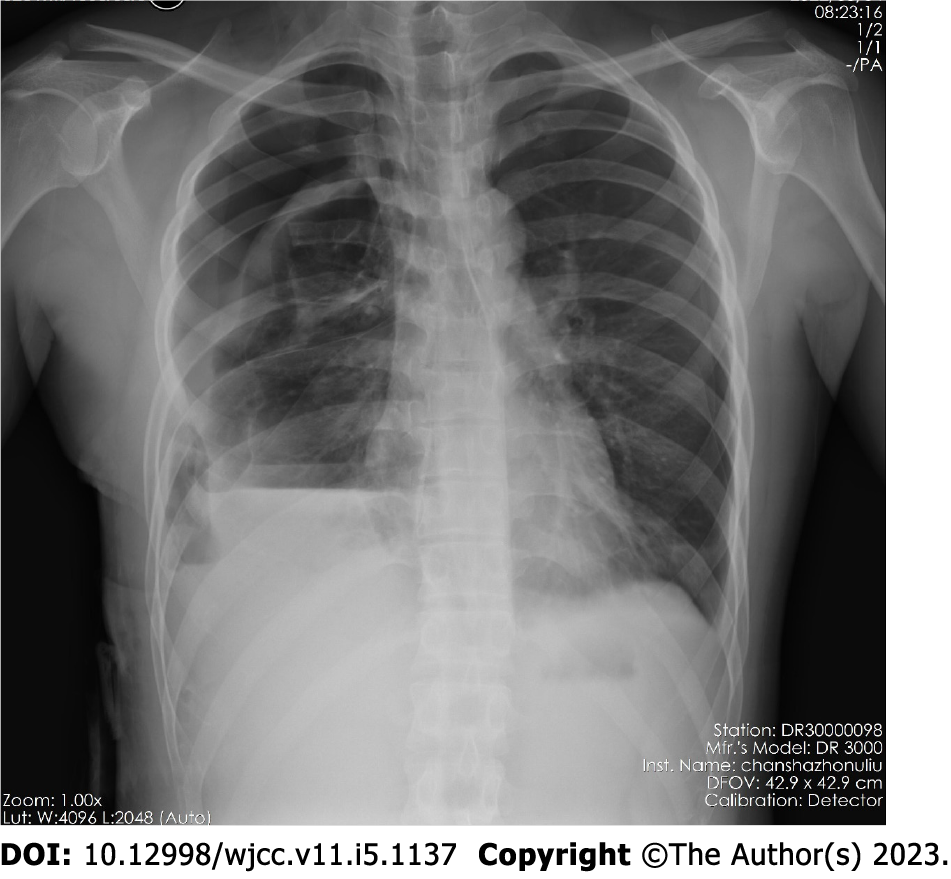
Postoperatively, the patient’s shortness of breath was resolved. Chest X-ray showed that the mediastinum had returned to its normal position, the left lung was almost fully reinflated, and the right lung was relatively small (Figure 5). No signs of recurrence were observed at the 6-mo follow-up.
Thymolipoma, officially named by Hall in 1948, is a rare, slow-growing, benign tumor arising from the anterior mediastinal thymus, and these tumors are composed of mature fatty tissue and interspersed nonneoplastic thymic tissue[1,2]. The pathogenesis remains unclear, and to date, fewer than 200 cases have been published in the literature worldwide[10-14]. These tumors can occur at any age but are more common in young adults. They are lobulated, well encapsulated, and do not recur after complete surgical excision[1,2,15,16].
Since thymolipomas are soft, noninvasive, and located in the anterior mediastinum, more than half of thymolipomas are asymptomatic and diagnosed incidentally by radiological examination[1]. However, when the tumor tissue becomes significantly enlarged, compression of adjacent tissues and organs can occur, and then the patient can develop dyspnea, fatigue, nonproductive cough, chest pain, and even respiratory failure and death[3]. Occasionally, similar to other thymic diseases, a small proportion of patients with thymolipomas may also have certain autoimmune disorders, such as myasthenia gravis, vitamin B12 deficiency, hypogammaglobulinemia, and aplastic anemia. Fortunately, these symptoms may be improved by tumor removal[1,4,17].
In general, patients with giant thymolipomas mainly present with respiratory symptoms. Its characteristic CT feature is a mediastinal fatty dense mass with soft tissue strands that probably correspond to the islets of normal thymic components[18]. However, it is sometimes challenging to diagnose thymolipoma according to the clinical symptoms, signs, or imaging examinations, and biopsy is a definitive diagnostic tool that may be able to differentiate benign thymolipomas from malignant liposarcomas[1].
Surgical resection is the only curative treatment for thymolipomas, and depending on the tumor size and site, various surgical approaches have been reported, including thoracotomy, sternotomy, and video-assisted thoracoscopy[1,4]. The largest resected thymolipoma and thymic liposarcoma previously reported in the literature weighed 6 kg[19] and 5 kg[9], respectively. In our report, the patient’s tumor weighed more than 7 kg, it compressed most of the lungs, and the patient’s preoperative oxygen saturation was less than 90%. Apparently, our patient was a high-anesthetic risk patient, and awake endotracheal intubation was used. In addition, the mass was undoubtedly too large for en bloc resection by sternotomy, so a posterolateral fifth intercostal incision was selected for piecemeal resection.
This article reports a very rare case of thymolipoma that compressed the patient’s lungs, resulting in severely reduced lung function and type 2 respiratory failure. Despite the high risk of anesthesia, the tumor was successfully removed by a posterolateral incision, and the patient’s prognosis was good. The resected tumor weighed 7.5 kg and, to our knowledge, it was the largest surgically removed thymus neoplasm.
We would like to thank our patient for his participation and cooperation in this case report.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bersot CD, Brazil; Fazilat-Panah D, Iran S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Hamouri S, Syaj S, Al-Kraimeen L, Al-Smady M, Alhadidi H, Barakat F. Thymolipoma and its Association with Myasthenia Gravis: a Multi-center Experience. Med Arch. 2021;75:375-381. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 2. | Guimarães MD, Benveniste MF, Bitencourt AG, Andrade VP, Souza LP, Gross JL, Godoy MC. Thymoma originating in a giant thymolipoma: a rare intrathoracic lesion. Ann Thorac Surg. 2013;96:1083-1085. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Yusuf Mohamud MF, Ahmed MA, Ali IH. Extensive mediastinal thymolipoma mimicking pulmonary edema. J Surg Case Rep. 2020;2020:rjaa080. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 4. | Aghajanzadeh M, Asgary MR, Mesbah A, Hemmati H, Delshad MSE, Samidoust P, Hemmati G. Giant thymolipoma of mediastinum and neck - initially misdiagnosed as liposarcoma by core needle biopsy. J Family Med Prim Care. 2018;7:1079-1082. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Aghajanzadeh M, Alavi A, Pourrasouli Z, Aghajanzadeh G, Massahnia S. Giant mediastinal thymolipoma in 35-year-old women. J Cardiovasc Thorac Res. 2011;3:67-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Bian D, Zhou F, Yang W, Zhang K, Chen L, Jiang G, Zhang P, Wu C, Fei K, Zhang L. Thymoma size significantly affects the survival, metastasis and effectiveness of adjuvant therapies: a population based study. Oncotarget. 2018;9:12273-12283. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 7. | Azuma Y, Otsuka H, Makino T, Koezuka S, Anami Y, Sadamoto S, Wakayama M, Tochigi N, Shibuya K, Iyoda A. Giant thymoma successfully resected via median sternotomy and anterolateral thoracotomy: a case report. J Cardiothorac Surg. 2018;13:26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Bolca C, Has A, Bobocea A, Afetelor A, Stoica R, Strambu I, Stoicescu I, Magheran E, Balescu I, Bacalbasa N, Gherghiceanu F, Furtunescu F, Radavoi D, Diaconu C, Paleru C, Cordos I. A Rare Thymic Tumor - Lipofibroadenoma - Always a Postoperative Surprise. In Vivo. 2021;35:3623-3626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Alhames S, Ghabally M. Enbloc resection of the largest thymic liposarcoma: A case report with literature review. Ann Med Surg (Lond). 2020;59:204-206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 10. | Campion T, Maity A, Ali S, Richards P, Adams A. Concurrent thyrolipomatosis and thymolipoma in a patient with myasthenia gravis: a case report and review of the literature. Ann R Coll Surg Engl. 2021;103:e212-e215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 11. | Ogino S, Franks TJ, Deubner H, Koss MN. Thymohemangiolipoma, a rare histologic variant of thymolipoma: a case report and review of the literature. Ann Diagn Pathol. 2000;4:236-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Hayashi A, Takamori S, Tayama K, Mitsuoka M, Ohtsuka S, Aoyama Y, Shirouzu K. Thymolipoma: clinical and pathological features--report of three cases and review of literature. Kurume Med J. 1997;44:141-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Laforga JB, Vierna J. Correspondence re: Moran C, Rosado-De-Christenson M, Suster S: thymolipoma: clinicopathologic review of 33 cases. Mod Pathol 8:741, 1995. Mod Pathol. 1996;9:869. [PubMed] |
| 14. | Sirpal YM, Chadha SK, Banarjee AK. Thymolipoma--a rare mediastinal tumour--report of two cases and review of literature. Indian J Cancer. 1995;32:23-26. [PubMed] |
| 15. | Moran CA, Rosado-de-Christenson M, Suster S. Thymolipoma: clinicopathologic review of 33 cases. Mod Pathol. 1995;8:741-744. [PubMed] |
| 16. | Yamamura M, Aoki K, Takanashi S, Tadokoro M, Furuta S, Takizawa M. [A case report of thymolipoma with high titer of serum anti-acetylcholine receptor antibodies--thymolipoma, a review of 49 reports in Japan]. Nihon Kyobu Geka Gakkai Zasshi. 1994;42:237-242. [PubMed] |
| 17. | Wang H, Li Q, Jiang Q, Yang Y, Liu Y, Gu L, Gong M, Xu G, Chen C. A giant tumor of the mediastinum mixed with thymocytes and adipocytes: a case report. Gland Surg. 2021;10:3163-3166. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Obeso Carillo GA, García Fontán EM, Cañizares Carretero MÁ. Giant thymolipoma: case report of an unusual mediastinal tumor. Arch Bronconeumol. 2014;50:557-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Gamanagatti S, Sharma R, Hatimota P, Guleria R, Arvind S. Giant thymolipoma. AJR Am J Roentgenol. 2005;185:283-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |