Published online Feb 16, 2023. doi: 10.12998/wjcc.v11.i5.1106
Peer-review started: October 14, 2022
First decision: November 30, 2022
Revised: December 11, 2022
Accepted: January 16, 2023
Article in press: January 16, 2023
Published online: February 16, 2023
Processing time: 123 Days and 3 Hours
Patient satisfaction with facial appearance at the end of orthodontic camouflage treatment is very important, especially for skeletal malocclusion. This case report highlights the importance of the treatment plan for a patient initially treated with four-premolar-extraction camouflage, despite indications for orthognathic surgery.
A 23-year-old male sought treatment complaining about his unsatisfactory facial appearance. His maxillary first premolars and mandibular second premolars had been extracted, and a fixed appliance had been used to retract his anterior teeth for two years without improvement. He had a convex profile, a gummy smile, lip incompetence, inadequate maxillary incisor inclination, and almost a class I molar relationship. Cephalometric analysis showed severe skeletal class II malocclusion (A point-nasion-B point = 11.5°) with a retrognathic mandible (sella-nasion-B point = 75.9°), a protruded maxilla (sella-nasion-A point = 87.4°), and vertical maxillary excess (upper incisor to palatal plane = 33.2 mm). The excessive lingual inclination of the maxillary incisors (upper incisor to nasion-A point line = -5.5°) was due to previous treatment attempts to compensate for the skeletal class II malocclusion. The patient was successfully retreated with decompensating orthodontic treatment combined with orthognathic surgery. The maxillary incisors were repositioned and proclined in the alveolar bone, the overjet was increased, and a space was created for orthognathic surgery, including maxillary impaction, anterior maxillary back-setting, and bilateral sagittal split ramus osteotomy to correct his skeletal anteroposterior discrepancy. Gingival display was reduced, and lip competence was restored. In addition, the results remained stable after 2 years. The patient was satisfied with his new profile as well as with the functional malocclusion at the end of treatment.
This case report provides orthodontists a good example of how to treat an adult with severe skeletal class II malocclusion with vertical maxillary excess after an unsatisfactory orthodontic camouflage treatment. Orthodontic and orthognathic treatment can significantly correct a patient’s facial appearance.
Core Tip: This case report describes a skeletal class II patient who had experienced two-year camouflaged orthodontic treatment but was still unsatisfied with his facial aesthetics. A combined surgical/orthodontic treatment was then carried out. The maxillary incisors were re-positioned and proclined in the alveolar bone, the overjet was increased, and a space was created for orthognathic surgery, including maxillary impaction, anterior maxillary back-setting, and bilateral sagittal split ramus osteotomy to correct his skeletal anteroposterior discrepancy. Orthognathic surgery should be considered the first option when a patient’s chief complaint is about his facial aesthetics and there is severe skeletal deformity. When choosing orthodontic camouflage, orthodontists must be cautious that unfavorable soft tissue changes might occur. After an unsatisfactory orthodontic camouflage treatment, orthodontic and orthognathic treatment can still be used in severe adult skeletal class II malocclusion.
- Citation: Zhou YW, Wang YY, He ZF, Lu MX, Li GF, Li H. Orthodontic-surgical treatment for severe skeletal class II malocclusion with vertical maxillary excess and four premolars extraction: A case report. World J Clin Cases 2023; 11(5): 1106-1114
- URL: https://www.wjgnet.com/2307-8960/full/v11/i5/1106.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i5.1106
Severe skeletal class II malocclusion is characterized by maxillary protrusion, mandibular retrusion, or both. Skeletal class II malocclusion accompanied by vertical discrepancies such as maxillary excess and gummy smiles poses the biggest challenge to orthodontists, but skeletal class II deformations can be treated in several ways. In adult patients, when the condition has a skeletal origin, combined orthognathic-orthodontic treatment is often the best approach[1]. However, for many of these patients, surgery is not a viable option because of medical or financial concerns[2]. Therefore, camouflage therapy can sometimes be an alternative method of treatment[3-6].
Orthodontic treatment with vertical control may decrease the malocclusion and improve facial appearance[7,8], even in adult patients[8-11]. However, the limits between orthognathic surgery and orthodontic camouflage treatment on skeletal class II malocclusion has not been very clear until now. Patients with large A point-nasion-B point (ANB) values present a challenging situation when treated exclusively with orthodontic extraction camouflage for maxillary first premolars and/or mandibular second molars. This approach can aggravate excessively convex profiles and upper lip incompetence and raise the risk of periodontal problems[12]. Thus, the correct boundary between orthognathic surgery and orthodontic camouflage treatment on skeletal class II malocclusion should first be established for accurate treatment planning.
Here, we report a case with severe skeletal class II malocclusion treated with orthodontic camouflage treatment by four premolar extractions. The camouflage treatment led to a negative effect on the patient’s facial appearance. Because of this, the patient then underwent an orthodontic-orthognathic treatment plan to correct his malocclusion and achieve a balanced facial profile.
A 23-year-old male came to the Department of Orthodontics at the clinic of Nanjing Stomatological Hospital. His chief complaint was his facial appearance, especially his upper lip incompetence and the increased convexity of his profile.
He presented a history of a previous two-year orthodontic treatment at another clinic where an attempt was made to retract protruded maxillary anterior teeth but without any improvement. Teeth 14, 24, 35, and 45 had been extracted.
The patient denied any family history of his present illness.
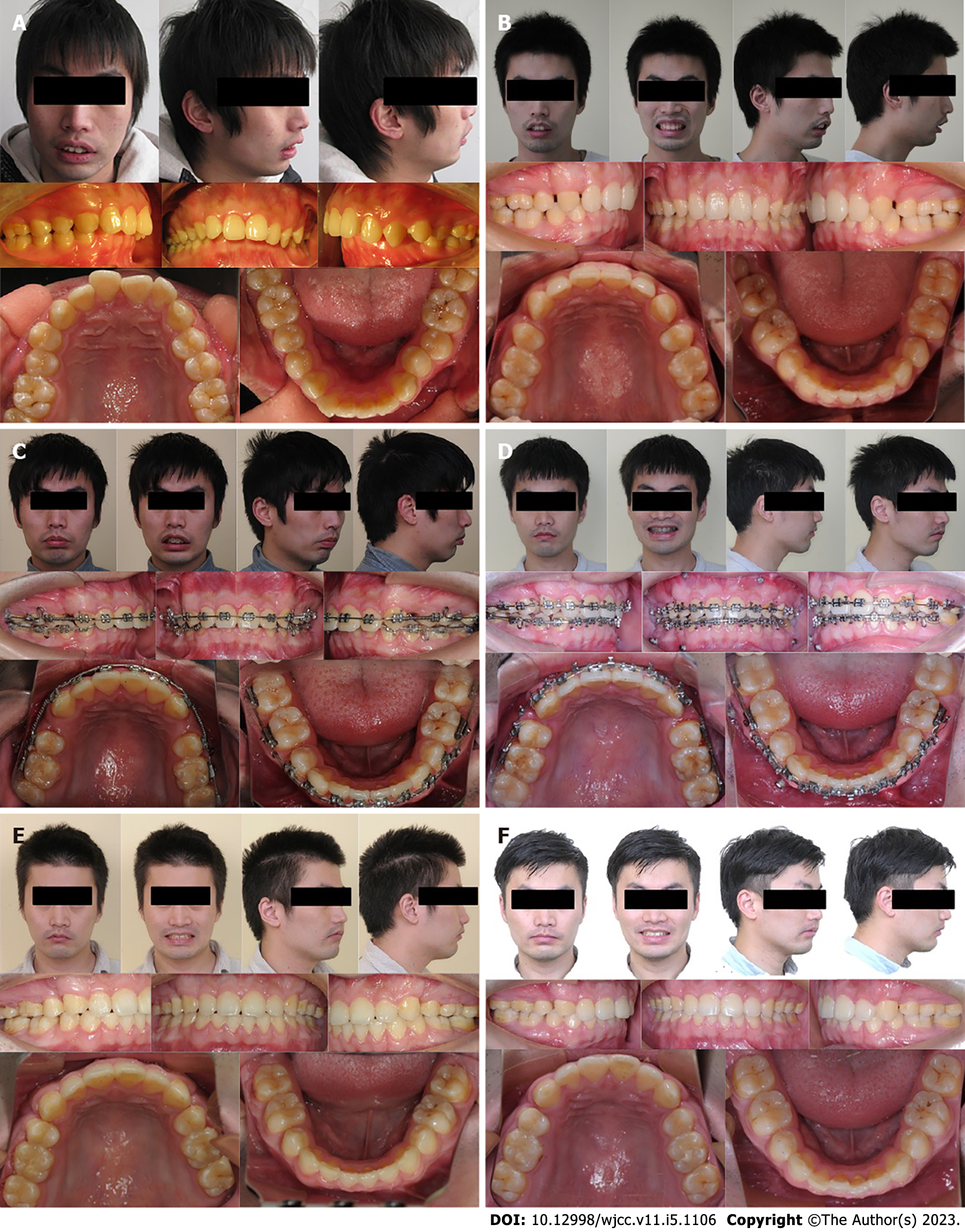
Copies of the initial extra-oral and intra-oral photographs were requested from the original clinic, and new treatment records were collected after the unsuccessful initial treatment. The patient’s photographs before any orthodontic intervention (Figure 1A) showed a typical class II molar and canine relationship and a skeletal class II relationship, with a deep overbite (III°) as well as a deep overjet (6 mm). Mild crowding was found in both the maxillary and mandibular arches. Extra-oral pictures showed upper lip incompetence and a convex profile.
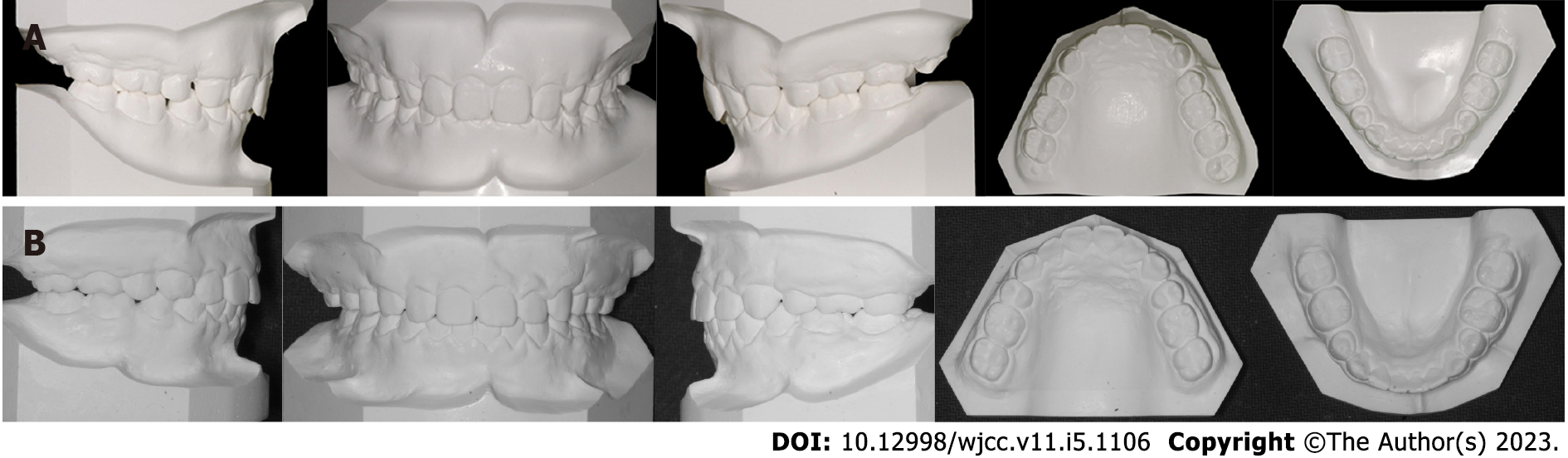
After the initial orthodontic camouflage treatment, extra oral examination revealed a severe convex profile, a deep labiomental fold, excessive gingival display, and an everted upper lip with incompetence (Figure 2B). Intraoral examination revealed that the patient had had teeth 14, 24, 35, 45 extracted, an almost class I occlusion after the camouflage treatment, an unclosed 3 mm space in his maxillary arch, and an unclosed 2 mm space in his mandibular arch. An overjet of 3 mm and an overbite of 4 mm were observed with no transverse discrepancies (Figures 1B and 2A).
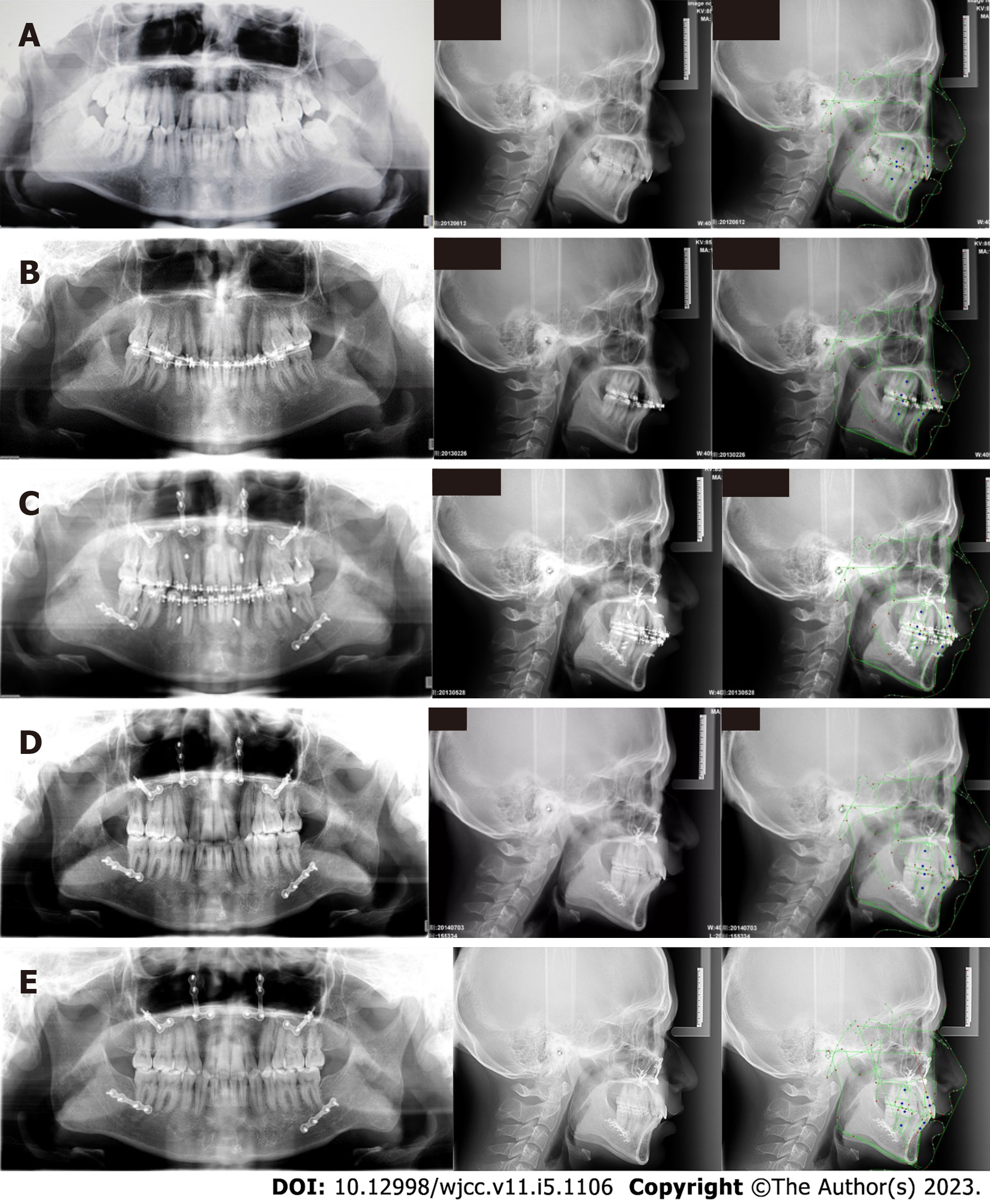
Lateral cephalometric analysis revealed a skeletal class II jaw relation (Figure 3A and Table 1), an increased ANB angle (ANB = 11.5°), a retrognathic mandible [sella-nasion-B point (SNB) = 75.9°], a protruded maxilla [sella-nasion-A point (SNA) = 87.4°], a vertical maxillary excess [upper incisor to palatal plane (U1-PP) = 33.2 mm], and excessive lingual inclination of the maxillary incisors [upper incisor to nasion-A point line (U1-NA) = -5.5°, U1-NA = -6.1 mm). The inclination of the mandibular incisors was normal, and the mandibular plane angle was below average [sella-nasion-mandibular plane (SN-MP) = 31.8°]. A panoramic radiograph showed the extraction of four premolars, the presence of all the third molars, and no pathological findings for the temporomandibular joints (Figure 3A).
| Measurements | Normal | Pre-treatment | Post-treatment | Difference |
| SNA° | 83.77 ± 2.85 | 87.4 | 84.8 | 2.6 |
| SNB° | 79.78 ± 2.98 | 75.9 | 78.1 | -2.2 |
| ANB° | 3.79 ± 1.88 | 11.5 | 6.7 | 4.8 |
| SN-MP° | 34.85 ± 4.09 | 31.8 | 29.1 | 2.7 |
| S-Go/N-Me | 67.02 ± 3.97 | 90.3 | 89.3 | 1 |
| ANS-Me/N-Me | 53.05 ± 1.83 | 66.3 | 67.3 | -1 |
| U1-L1° | 120.62 ± 9.12 | 143.3 | 122.9 | 20.4 |
| U1-NA (mm) | 4.44 ± 2.36 | -6.1 | 1.3 | -7.4 |
| U1-NAº | 23.69 ± 5.74 | -5.5 | 15.7 | -21.2 |
| L1-NB (mm) | 6.84 ± 2.65 | 8.3 | 7.5 | 0.8 |
| L1-NBº | 31.90 ± 6.09 | 30.7 | 34.7 | -4 |
| UL-EP (mm) | 2.16 ± 2.01 | 1.6 | -1.6 | 3.2 |
| LL-EP (mm) | 3.17 ± 2.73 | 4.3 | 0.6 | 3.7 |
| Z angle | 71.22 ± 4.76 | 52.5 | 64.3 | -11.8 |
The patient was diagnosed with skeletal class II mandibular retrognathism with mild maxilla protrusion, vertical maxillary excess, a dental class I malocclusion with teeth 14, 24, 35, and 45 missing, and excess space in both dental arches.
The main treatment objectives were (1) improve the patient’s facial aesthetics by orthognathic surgery; (2) to decompensate the retroclination of the maxillary incisors and create space for orthognathic surgery; and (3) to correct his dental problems by establishing a class I molar relationship with a normal overbite and overjet.
Considering the previous orthodontic camouflage treatment and the patient’s desire to improve his facial aesthetics, orthognathic surgery was recommended. Anterior maxillary osteotomy and maxillary impaction were planned to correct the maxilla protrusion and vertical access, and bilateral sagittal split ramus osteotomy (BSSRO) was planned for moving the mandible forward. Before surgery, orthodontic treatment was needed to open the maxillary extraction space, increase the overjet, and create the necessary space for orthognathic surgery. The opened extraction space was closed by moving the maxillary posterior segment forward. Additionally, chinplasty was recommended to this patient as an alternative to orthosurgical therapy, but he refused this plan because his major concern was his facial appearance.
Pre-surgical orthodontic treatment: The patient’s four third molars were extracted prior to orthodontic treatment. Preadjusted fixed appliances (0.022 × 0.028-inch MBT prescription, 3 M Unitek, Monrovia, CA) were bonded, and the orthodontic treatment was initiated by aligning the maxillary and mandibular teeth using 0.016’ preformed Ni-Ti arch wires. Maxillary and mandibular arch forms were coordinated with each other by sequentially increasing the rigidity of the arch wires. The maxillary anterior teeth were move forward by a Ni-Ti coil spring to increase the space in the maxillary arch, and the maxillary canines and second premolars were positioned to be upright with roots parallel to each other to facilitate the surgical cuts. The torque of the maxillary incisors was corrected at this time as well.
The space in the lower arch was closed (Figures 1C and 3B). Prior to surgery, both the maxillary and mandibular dentition were stabilized on 0.019” × 0.025” stainless steel wire to allow efficient tip and torque expression and to provide adequate rigidity. At the end of pre-surgical phase, the patient had a class I molar relationship and a class II canine relationship, accompanied by an overjet of 8 mm and an overbite of 6 mm. The space between the maxillary canines and second premolars was 6 mm on each side. The maxillary incisors’ gingival exposure was 2 mm at rest and 8 mm upon smiling (Figure 1C).
Surgical treatment: The maxilla was impacted for 3 mm and retracted for 3 mm with Lefort I and anterior maxillary segment osteotomy, then the posterior segment was moved forward to close the extraction space in the maxillary arch. The mandible was then moved forward 5 mm by BSSRO. Rigid internal fixations were carried out to stabilize the osteotomy sites, and the patient was followed up closely. Orthodontic treatment was restarted 12 wk after surgery (Figures 1D and 3C).
Post-surgical orthodontic treatment: The residual spaces in the maxillary arch were closed by mesial movement of the posterior teeth to attain a class I molar relationship. Ten months of treatment were needed to completely close the 2 mm residual space, and final settling was performed to achieve a good intercuspal relation. The entire treatment period was 24 mo. After using the fixed appliances, a pair of clear retainers was prescribed for constant use. The patient was followed for two years after surgery.
The patient presented an improved and more balanced facial appearance at the end of treatment (Figure 1E), with a reduction in his profile convexity and maxillary incisor gingival exposure (Figure 2B and 3D). Both dental arches were well aligned, and their midlines coincided. A normal overjet and overbite with class I molar relationships were also achieved. A post-treatment panoramic radiograph indicated that all of the roots were parallel and that there was no obvious root resorption.
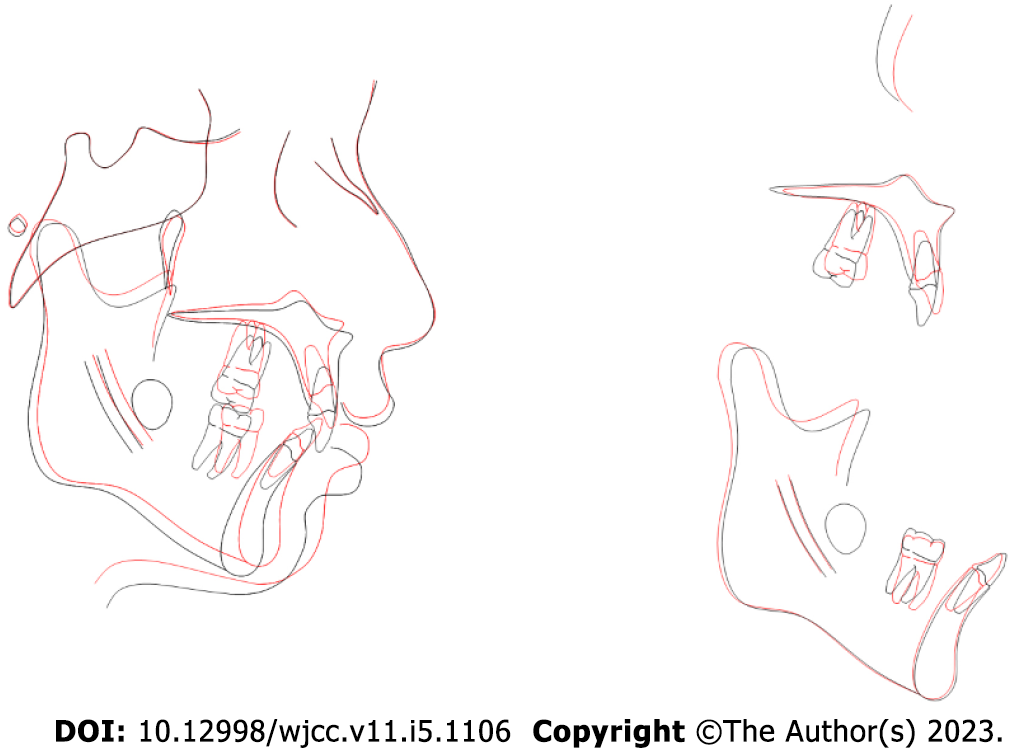
The pre- and post-treatment cephalometric values showed skeletal and dental improvements (Table 1, Figure 4), including decreased ANB angle (ANB = 6.7°), a forward mandible (SNB = 78.1°), and a retracted maxilla (SNA = 84.8°). The vertical maxillary excess was corrected as well (U1-PP = 29.9 mm). The inclination of the maxillary incisors was close to normal (U1-NA = 15.7°, U1-NA = 1.3 mm), and the corrected inclination of the mandibular incisors was almost maintained from the immediate surgical outcome. The mandibular plane angle was decreased by counterclockwise mandible rotation (SN-MP = 29.1°). The post-treatment and 2-year follow-up records indicated a balanced facial appearance and good stability, and the results remained stable except for an approximately 0.5 mm space relapse in the maxillary arch (Figures 1F and 3E).
Achievement of balanced facial aesthetics is one of the primary goals with orthodontic treatment. For nongrowing adult patients with severe skeletal class II malocclusions, orthodontists should keep in mind that the orthosurgical treatment should be the preferred option[13], and we highly recommend that a patient choose orthodontic camouflage treatment in cases of skeletal deformities that present with an acceptable facial appearance.
Facial aesthetics are a big problem when considering treatment results. Orthodontic camouflage treatment just uses tooth movement to compensate for poor aesthetics but does not correct the underlying skeletal problem[14]. In contrast, orthognathic surgery can reposition the jaw and correct maxillary and mandibular discrepancies, improving not only the malocclusion and skeletal relationship of the jaws but also masticatory function and jaw movement[15]. Therefore, orthognathic surgery should be considered the first option when a patient’s chief complaint is about his facial aesthetics. This combined orthodontic and orthognathic treatment can not only improve a patient’s facial appearance but can also improve his confidence and quality of life[16].
Orthodontists must be cautious that unfavorable soft tissue changes might result from orthodontic camouflage alone. Severe mandibular deficiency, vertical maxillary excess, and upper lip incompetence are important factors to contraindicate orthodontic camouflage treatment. In addition, an undesirable increase in the nasolabial angle is common when performing camouflage orthodontics with maxillary premolar extractions[17]. The decision for camouflage treatment or surgery must be made before any treatment begins because presurgical orthodontics to prepare the patient for surgery require an extraction plan that runs counter to that of camouflage. Thus, practitioners must understand how far it is possible to go with orthodontic extraction treatment alone[18,19].
Orthodontic camouflage treatment that extracts maxillary first premolars and mandibular second premolars may exacerbate a patient’s poor facial appearance. The retraction of the maxillary incisors can extrude the maxillary incisors and make the upper lip incompetence more severe[20]. However, the retraction of the maxillary incisors causes the clockwise rotation of the mandible, causing mandibular deficiency to appear look even more pronounced. In this case, facial aesthetics become worse after orthodontic camouflage treatment.
To solve this problem, orthodontic treatment and orthognathic surgery are the best choice such a case. For the orthodontic treatment of the patient in this case study, decompensation of the maxillary incisors was very important. We needed to reopen the maxillary extraction space and create enough room to let the mandible move forward. Recovering the torque of the anterior maxillary was also important in this present case and allowed the surgeon to evaluate the amount of maxillary impaction.
For this patient’s orthognathic surgery, impacting the maxilla surgically allowed the mandible to rotate upward and forward. It has been well documented that the Lefort I down fracture technique with superior repositioning has excellent stability[21]. Furthermore, the forward movement of the mandible contributed to this patient’s successful treatment and improved profile. Maintaining a class I molar relationship was achieved by forward movement of the posterior maxillary segment that was made possible by closing the maxillary premolar extraction spaces.
After two years of follow-up, the patient’s physiological adaptation and morphological change were almost complete, and the results were stable. The patient showed a smile with a pleasant aesthetic and amount of occlusion, and the stability of the treatments indicate that combined orthodontic and orthognathic treatment was the correct choice. However, for the segmental osteotomy in the maxillary arch, the slight relapse of extraction space also indicated that the soft tissue scar may be inhibiting tooth movement.
This case study provides orthodontist with a good example of how to treat an adult with severe skeletal class II malocclusion with vertical maxillary excess after unsatisfactory orthodontic camouflage treatment. Orthodontic and orthognathic treatment can significantly improve a patient’s facial appearance and achieve stable results years after surgery.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Dentistry, oral surgery and medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Dominguez C AI, Colombia; Chisthi MM, India S-Editor: Zhang H L-Editor: A P-Editor: Zhang H
| 1. | Proffit WR, Phillips C, Tulloch JF, Medland PH. Surgical versus orthodontic correction of skeletal Class II malocclusion in adolescents: effects and indications. Adult Orthodon Orthognath Surg. 1992;7:209-220. [PubMed] |
| 2. | Shu R, Huang L, Bai D. Adult Class II Division 1 patient with severe gummy smile treated with temporary anchorage devices. Am J Orthod Dentofacial Orthop. 2011;140:97-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Mihalik CA, Proffit WR, Phillips C. Long-term follow-up of Class II adults treated with orthodontic camouflage: a comparison with orthognathic surgery outcomes. Am J Orthod Dentofacial Orthop. 2003;123:266-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 81] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 4. | Nishimura M, Sannohe M, Nagasaka H, Igarashi K, Sugawara J. Nonextraction treatment with temporary skeletal anchorage devices to correct a Class II Division 2 malocclusion with excessive gingival display. Am J Orthod Dentofacial Orthop. 2014;145:85-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Kaku M, Kojima S, Sumi H, Koseki H, Abedini S, Motokawa M, Fujita T, Ohtani J, Kawata T, Tanne K. Gummy smile and facial profile correction using miniscrew anchorage. Angle Orthod. 2012;82:170-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Lai EH, Yao CC, Chang JZ, Chen I, Chen YJ. Three-dimensional dental model analysis of treatment outcomes for protrusive maxillary dentition: comparison of headgear, miniscrew, and miniplate skeletal anchorage. Am J Orthod Dentofacial Orthop. 2008;134:636-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 66] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 7. | Redlich M, Mazor Z, Brezniak N. Severe high Angle Class II Division 1 malocclusion with vertical maxillary excess and gummy smile: a case report. Am J Orthod Dentofacial Orthop. 1999;116:317-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Kim SJ, Kim JW, Choi TH, Lee KJ. Combined use of miniscrews and continuous arch for intrusive root movement of incisors in Class II division 2 with gummy smile. Angle Orthod. 2014;84:910-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Paik CH, Park HS, Ahn HW. Treatment of vertical maxillary excess without open bite in a skeletal Class II hyperdivergent patient. Angle Orthod. 2017;87:625-633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Wang XD, Zhang JN, Liu DW, Lei FF, Zhou YH. Nonsurgical correction of a severe anterior deep overbite accompanied by a gummy smile and posterior scissor bite using a miniscrew-assisted straight-wire technique in an adult high-angle case. Korean J Orthod. 2016;46:253-265. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Wang XD, Zhang JN, Liu DW, Lei FF, Liu WT, Song Y, Zhou YH. Nonsurgical correction using miniscrew-assisted vertical control of a severe high angle with mandibular retrusion and gummy smile in an adult. Am J Orthod Dentofacial Orthop. 2017;151:978-988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Alencar DS, Cunha Almeida RC, Maues Casagrande CP, Prado R, Hermolin A, de Assis Ribeiro Carvalho F. Orthodontic-surgical treatment for a patient with Class II malocclusion and inadequate maxillary incisor inclination. Am J Orthod Dentofacial Orthop. 2020;157:690-703. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | Lu Y, Zhang W, Zhao B, Liu Y. Vertical Control of a Severe Hyperdivergent Skeletal Class II Malocclusion with Steep Posterior Occlusal Plane in a Camouflage Case. Medicina (Kaunas). 2022;58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 14. | Raposo R, Peleteiro B, Paço M, Pinho T. Orthodontic camouflage versus orthodontic-orthognathic surgical treatment in class II malocclusion: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2018;47:445-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 55] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 15. | Yamamoto T, Kaku M, Ono S, Takechi M, Tanimoto K. Correction of Severe Skeletal Class II High Angle with Mandibular Retrusion and Gummy Smile by Double-Jaw Surgery. Bull Tokyo Dent Coll. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Vaida LL, Negruțiu BM, Zetu IN, Moca AE, Bran S. Substantial Improvements in Facial Morphology through Surgical-Orthodontic Treatment: A Case Report and Literature Review. Medicina (Kaunas). 2022;58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 17. | Kinzinger G, Frye L, Diedrich P. Class II treatment in adults: comparing camouflage orthodontics, dentofacial orthopedics and orthognathic surgery--a cephalometric study to evaluate various therapeutic effects. J Orofac Orthop. 2009;70:63-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 50] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 18. | Burk SM, Charipova K, Orra S, Harbour PW, Mishu MD, Baker SB. A surgeon's perspective on the uncorrected skeletal deformity. Part II: The role of esthetic surgery for orthognathic camouflage. Am J Orthod Dentofacial Orthop. 2022;161:878-885. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 19. | Guo Y, Han X, Xu H, Ai D, Zeng H, Bai D. Morphological characteristics influencing the orthodontic extraction strategies for Angle's class II division 1 malocclusions. Prog Orthod. 2014;15:44. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 20. | Janson G, Mendes LM, Junqueira CH, Garib DG. Soft-tissue changes in Class II malocclusion patients treated with extractions: a systematic review. Eur J Orthod. 2016;38:631-637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 21. | Tabrizi R, Sarrafzadeh A, Shafiei S, Moslemi H, Dastgir R. Does maxillomandibular fixation affect skeletal stability following mandibular advancement? Maxillofac Plast Reconstr Surg. 2022;44:19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |