Published online Feb 16, 2023. doi: 10.12998/wjcc.v11.i5.1094
Peer-review started: November 1, 2022
First decision: November 11, 2022
Revised: November 17, 2022
Accepted: January 16, 2023
Article in press: January 16, 2023
Published online: February 16, 2023
Processing time: 105 Days and 2.1 Hours
Myxofibrosarcoma (MFS) is a fibroblast-derived sarcoma that mainly occurs in subcutaneous tissue. MFS rarely occurs in the gastrointestinal tract, especially in the esophagus.
A 79-year-old male patient was admitted to our hospital for dysphagia for a week. Computed tomography and electronic gastroscopy showed that a giant mass was located 30 cm from the incisor and extended to the cardia. There was incomplete esophageal stenosis. Endoscopic pathology showed spindle cell lesions, which were considered inflammatory myofibroblast like hyperplasia. Considering the strong demands of the patient and his family, and the fact that most inflammatory myofibroblast tumors are benign, we decided to perform endoscopic submucosal dissection (ESD) even if the tumor size was giant (9.0 cm × 3.0 cm). Postoperative pathological examination resulted in a final diagnosis of MFS. MFS rarely occurs in the gastrointestinal tract, especially in the esophagus. Surgical resection and local adjuvant radiotherapy are the first choices to improve the prognosis. This case report firstly described the ESD for esophageal giant MFS. It suggests that ESD may be an alternative treatment for primary esophageal MFS.
This case report for the first time describe the successful treatment of a giant esophageal MFS by ESD, suggesting that ESD may be an alternative treatment for primary esophageal MFS, especially in elderly high-risk patients with obvious dysphagia symptoms.
Core Tip: For the first time, we report a giant esophageal myxofibrosarcoma (MFS) measuring about 9.0 cm × 3.0 cm. We managed to remove the MFS completely through endoscopic submucosal dissection (ESD) without severe complications. This case suggests that ESD may be an alternative treatment for esophageal MFS, especially in aged high-risk patients with obvious dysphagia symptoms.
- Citation: Wang XS, Zhao CG, Wang HM, Wang XY. Giant myxofibrosarcoma of the esophagus treated by endoscopic submucosal dissection: A case report. World J Clin Cases 2023; 11(5): 1094-1098
- URL: https://www.wjgnet.com/2307-8960/full/v11/i5/1094.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i5.1094
Myxofibrosarcoma (MFS) is a fibroblast-derived sarcoma that mainly occurs in the subcutaneous tissue[1,2]. Most cases of MFS occur in the extremities, and only about 20% of cases occur in the trunk, retroperitoneum, heart, etc[3-5]. MFS rarely occurs in the gastrointestinal tract, especially in the esophagus. Surgical resection and local adjuvant radiotherapy are the first choice to improve the prognosis. In this paper, we report a patient with a giant MFS whose family chose endoscopic submucosal dissection (ESD) as a treatment strategy since they considered it was relatively safe and could maintain the anatomical integrity of the esophagus. The challenges for endoscopists were that the MFS with a size of about 9.0 cm × 3.0 cm was too large to be completely removed, and that there would be a high risk of gastrointestinal perforation and bleeding. Fortunately we managed to remove the MFS completely through ESD without severe complications. And the patient recovered well. This case suggests that ESD may be an alternative treatment for primary MFS in the esophagus.
A 79-year-old male patient was admitted to our hospital for dysphagia for a week.
The patient had dysphagia in the last week and had, which was more obvious when eating solid food. He did not have nausea, vomiting, or hoarseness.
The patient had no remarkable medical history.
The patient had no remarkable personal and family history.
No abnormality was found in the physical examination.
Laboratory examinations showed no abnormalities.
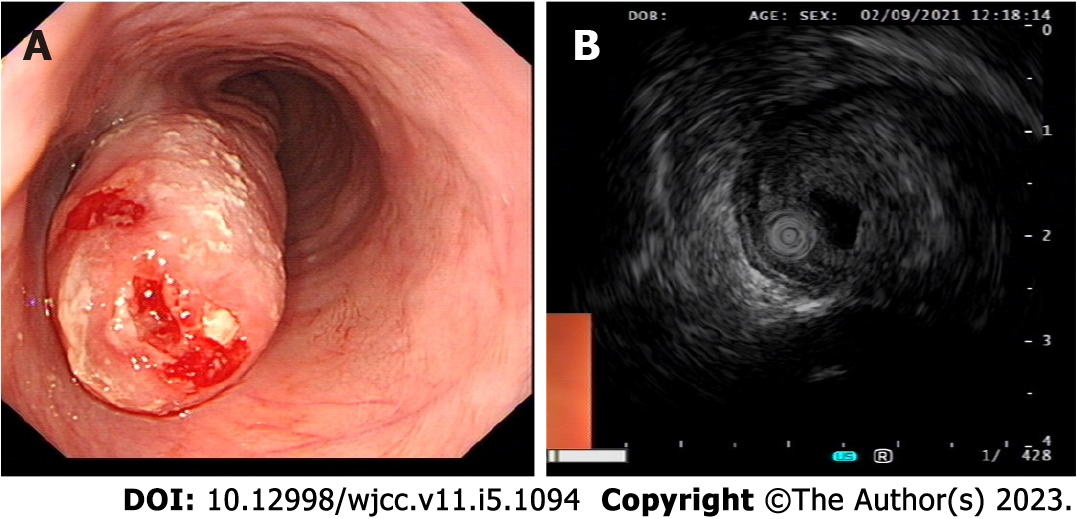
Computed tomography (CT) showed thickening of the lower esophageal wall and stenosis of the lumen. Gastroscopy revealed a giant mass located 30 cm from the incisor and extended to the cardia. There was incomplete esophageal stenosis. Macroscopically, the tumor looked like a serpentine, with a size of about 9.0 cm × 3.0 cm (Figure 1A). Endoscopic ultrasound revealed that the tumor originated from the submucosa, had mixed echo changes, and exhibited some inner cystoid structures (Figure 1B). Endoscopic pathology showed spindle cell lesions, which were considered inflammatory myofibroblast like hyperplasia.
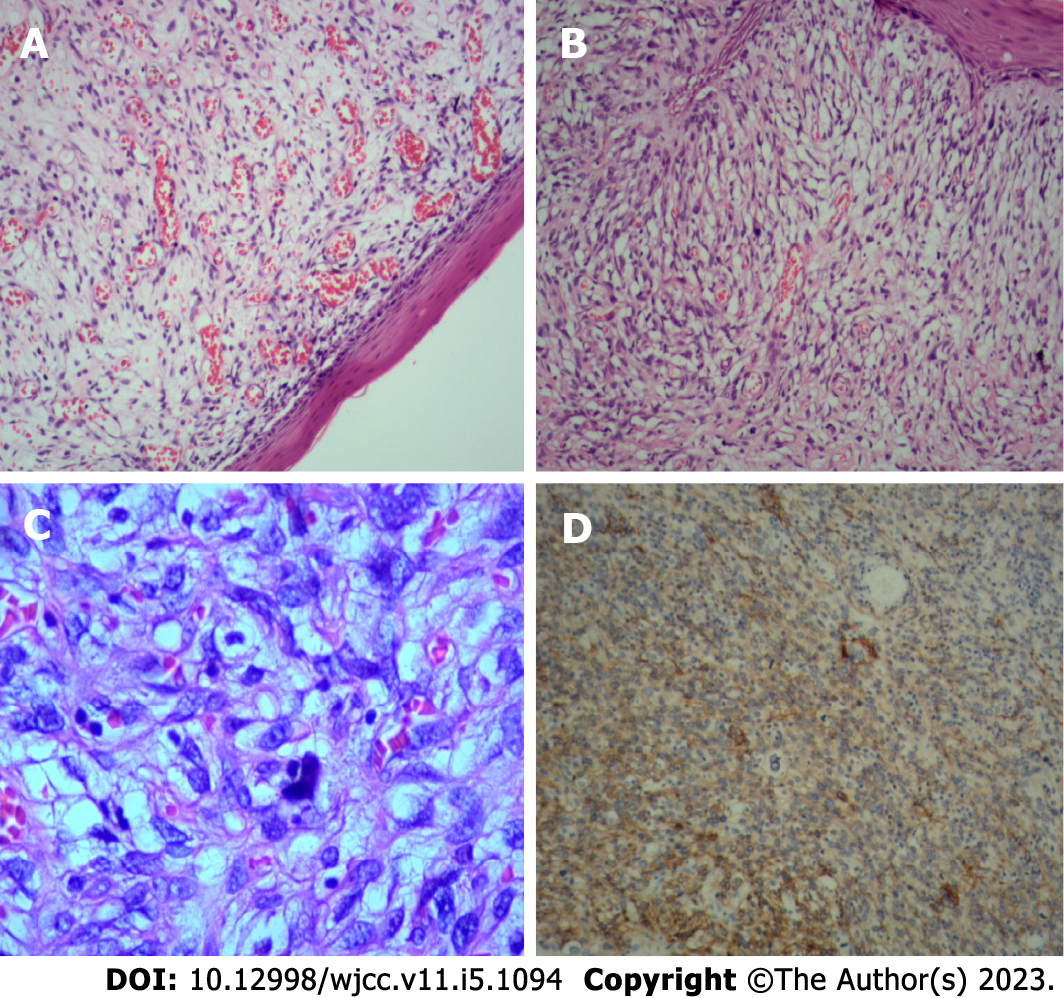
Immunohistochemical staining showed KI67 (55%+), P53 (3+, Mutant), Vimentin (3+), P40 (-), CK5/6 (-), SMA (-), Desmin (-), HMB45 (-), CD34 (-), CD117 (-), DOG-1 (-), CKpan (-), and EBER (-) (Figure 2).
The final diagnosis was MFS.
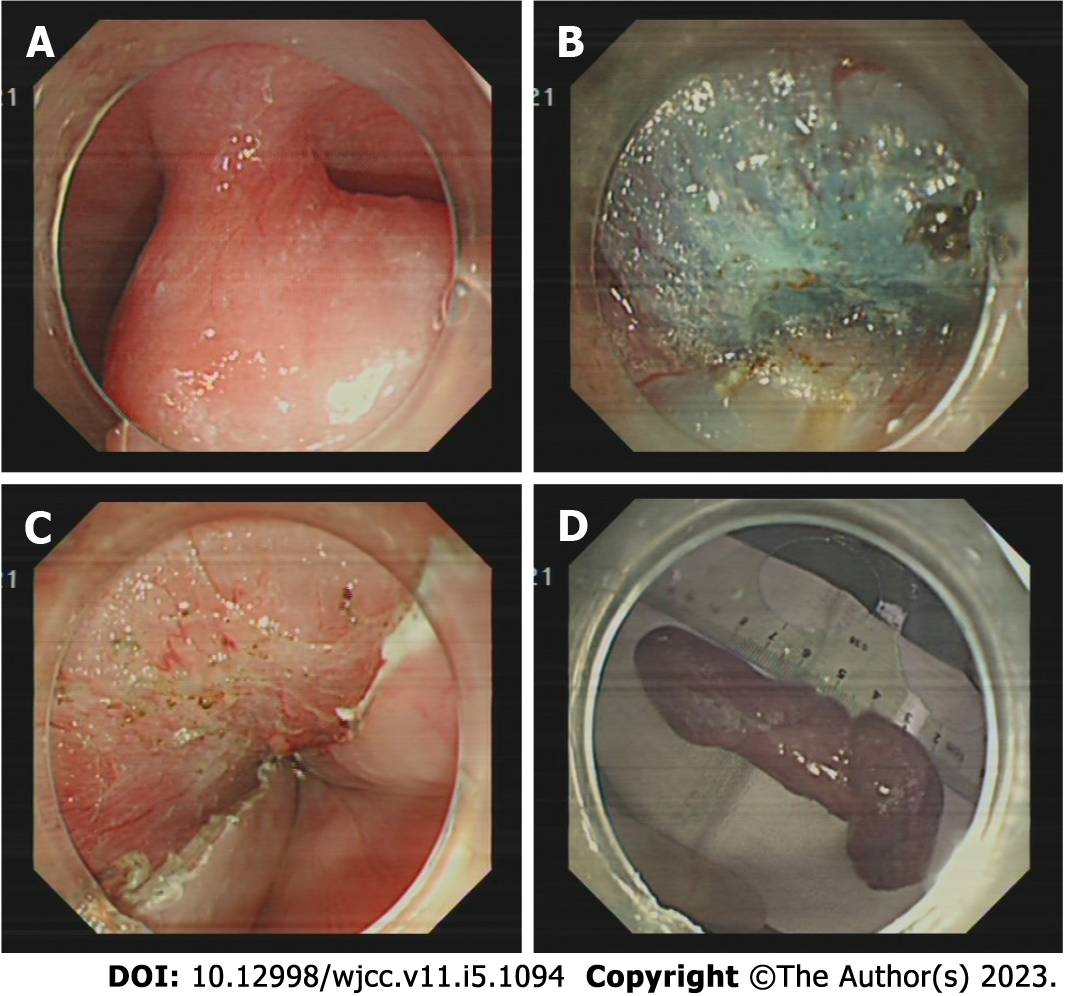
The operation was performed under general anesthesia with transparent cap assisted endoscopic therapy. After injecting the cerium mixture (composed of indigo, adrenaline, sodium hyaluronate, and normal saline) under the mucosa on the oral side, we made an incision using a fixed insulated tip (IT) knife (Olympus, Japan). Then we used the IT knife and double knife (Olympus, Japan) to gradually resect the tumor en bloc without serious complications (Figure 3).
The patient recovered well and was discharged from the hospital a week later without dysphagia.
MFS is a fibroblast-derived sarcoma that mainly occurs in the subcutaneous tissue[1,2]. MFS often occurs in elderly patients, with the extremities and girdles being the most frequently affected sites[6]. Although some studies report a higher incidence in men, the current evidence suggest no obvious gender preference[4,7]. MFS is a malignant fibroblastic neoplasm characterized by a high risk of local recurrence[8]. Surgical resection and local adjuvant radiotherapy are the first choice to improve the prognosis. As a soft tissue tumor mainly occurring in subcutaneous tissue, MFS rarely occurs in the gastrointestinal tract, especially in the esophagus. The diagnosis of this entity is challenging due to its rare and nonspecific clinical manifestations. MFS presents as a heterogeneous soft tissue mass on CT. Magnetic resonance imaging (MRI) is another choice for diagnosis. Typically, T1-weighted MRI shows a low to intermediate signal, and T2-weighted MRI shows that the solid and myxoid components have high signal intensity, and the signal intensity of the myxoid component is higher than that of the fluid[9]. Surgical excision and histologic tests are considered the gold standard for MFS diagnosis, particularly if the tumor is present in a rare location. Thoracoscopic surgery may be the first choice to remove this unusual tumor. However, compared with endoscopic surgery, open surgery is invasive and expensive, and often leads to additional complications, especially in elderly patients. ESD is relatively safe and can keep the integrity of esophageal anatomy. And some scholars have used ESD to treat giant esophageal masses[10,11]. However, ESD may not be able to completely remove the huge tumor. In addition, the risk of esophageal perforation and bleeding is high. If the above situations occur, surgery is still required to remove the tumor. In the present case, considering the obvious symptoms of dysphagia, the advanced age of the patient, and the strong demand of the patient and his family, we decided to perform ESD even if the tumor size was big (9.0 cm × 3.0 cm). Fortunately, the tumor was en bloc removed by ESD without severe complications. Combined with immunohistochemistry results, the tumor was diagnosed as MFS. This is the first case of MFS occurring in the esophagus and being resected by ESD. With the increasing incidence of gastrointestinal tumors, we believe that this case report will help promote the ESD as an alternative treatment for esophageal MFS.
Resection of esophageal MFS by ESD has not been reported before. This case report suggests that ESD may be an alternative treatment for esophageal MFS, especially in elderly high-risk patients with obvious dysphagia symptoms.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Atanasova EG, Bulgaria; Beji H, Tunisia; Vyshka G, Albania S-Editor: Wang JJ L-Editor: Wang TQ P-Editor: Wang JJ
| 1. | Hambleton C, Noureldine S, Gill F, Moroz K, Kandil E. Myxofibrosarcoma with metastasis to the lungs, pleura, and mediastinum: a case report and review of literature. Int J Clin Exp Med. 2012;5:92-95. [PubMed] |
| 2. | Nakahara S, Uemura H, Kurita T, Suzuki M, Fujii T, Tomita Y, Yoshino K. A case of myxofibrosarcoma of the maxilla with difficulty in preoperative diagnosis. Int J Clin Oncol. 2012;17:390-394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Antbring R, Parker SG, Lordan JT, Windsor AC. High-grade myxofibrosarcoma of the abdominal wall. BMJ Case Rep. 2017;2017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Gopalratnam K, Rodriguez JA, Woodson KA, Folman R. A Case of Myxofibrosarcoma in an Unusual Thoracic Location. Case Rep Oncol. 2016;9:39-44. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Lazaros GA, Matsakas EP, Madas JS, Toli DI, Nikas DJ, Kershaw MA, Alpert MA. Primary myxofibrosarcoma of the left atrium: case report and review of the literature. Angiology. 2008;59:632-635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Willems SM, Debiec-Rychter M, Szuhai K, Hogendoorn PC, Sciot R. Local recurrence of myxofibrosarcoma is associated with increase in tumour grade and cytogenetic aberrations, suggesting a multistep tumour progression model. Mod Pathol. 2006;19:407-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 105] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 7. | Rongioletti F. Myxofibrosarcoma: rare malignant skin tumors. New York: Springer, 2014. |
| 8. | Gambarotti M. Myxofibrosarcoma: atlas of musculoskeletal tumors and Tumorlike lesions. New York: Springer International Publishing, 2014. |
| 9. | Inoue M, Yamaguchi M, Kohada Y, Jeongho M, Hatanaka N, Seo S, Misumi T, Shimizu W, Irei T, Suzuki T, Onoe T, Sudo T, Shimizu Y, Hinoi T, Tashiro H. [A Case of Myxofibrosarcoma of the Retroperitoneum]. Gan To Kagaku Ryoho. 2016;43:2109-2111. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 10. | Zhu XS, Dai YC, Chen ZX. Giant Solitary Fibrous Tumor of Esophagus Resected by Endoscopic Submucosal Dissection. Ann Thorac Surg. 2015;100:2340-2343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Zhang SL, Du X, Tang XY, Liu D. Submucosal tunneling endoscopic resection for an unusually sized esophageal submucosal tumor protruding into the mediastinum. Rev Esp Enferm Dig. 2019;111:710-711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |