Published online Feb 16, 2023. doi: 10.12998/wjcc.v11.i5.1086
Peer-review started: September 18, 2022
First decision: November 11, 2022
Revised: November 15, 2022
Accepted: January 28, 2023
Article in press: January 28, 2023
Published online: February 16, 2023
Processing time: 148 Days and 17.8 Hours
Angioimmunoblastic T-cell lymphoma (AITL) is a subtype of peripheral T-cell lymphoma, with heterogenous clinical manifestations and poor prognosis. Here, we report a case of AITL induced hemophagocytic lymphohistiocytosis (HLH) and disseminated intravascular coagulopathy (DIC).
An 83-year-old man presented with fever and purpura of both lower limbs for one month. Groin lymph node puncture and flow cytometry indicated a diagnosis of AITL. Bone marrow examination and other laboratory related indexes indicated DIC and HLH. The patient rapidly succumbed to gastrointestinal bleeding and septic shock.
This is the first reported case of AITL induced HLH and DIC. AITL is more aggressive in older adults. In addition to male gender, mediastinal lymphadenopathy, anaemia, and sustained high level of neutrophil-to-lymphocyte ratio may indicate a greater risk of death. Early diagnosis, early detection of severe complications, and prompt and effective treatment are vital.
Core Tip: Angioimmunoblastic T-cell lymphoma (AITL) is a subtype of peripheral T-cell lymphoma, with heterogenous clinical manifestations and poor prognosis. Early diagnosis is particularly important. Herein, we report a patient with AITL induced hemophagocytic lymphohistiocytosis (HLH) and disseminated intravascular coagulopathy (DIC). The patient rapidly succumbed to gastrointestinal bleeding and septic shock. The time between onset and death was about one month. To the best of our knowledge, this is the first case of AITL induced HLH and DIC. AITL is more aggressive in older adults. In addition to male gender, mediastinal lymphadenopathy, anaemia, and sustained high level of neutrophil-to-lymphocyte ratio may indicate a greater risk of death. Early diagnosis, early detection of severe complications, and prompt and effective treatment are vital.
- Citation: Jiang M, Wan JH, Tu Y, Shen Y, Kong FC, Zhang ZL. Angioimmunoblastic T-cell lymphoma induced hemophagocytic lymphohistiocytosis and disseminated intravascular coagulopathy: A case report. World J Clin Cases 2023; 11(5): 1086-1093
- URL: https://www.wjgnet.com/2307-8960/full/v11/i5/1086.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i5.1086
Angioimmunoblastic T-cell lymphoma (AITL) is a subtype of peripheral T-cell lymphoma (PTCL), which accounts for 1%-2% of non-Hodgkin’s lymphomas and 15%-20% of PTCLs[1], and presents with heterogenous clinical manifestations and poor prognosis[2]. Early diagnosis is particularly important. Herein, we report a patient with AITL induced hemophagocytic lymphohistiocytosis (HLH) and disseminated intravascular coagulopathy (DIC).
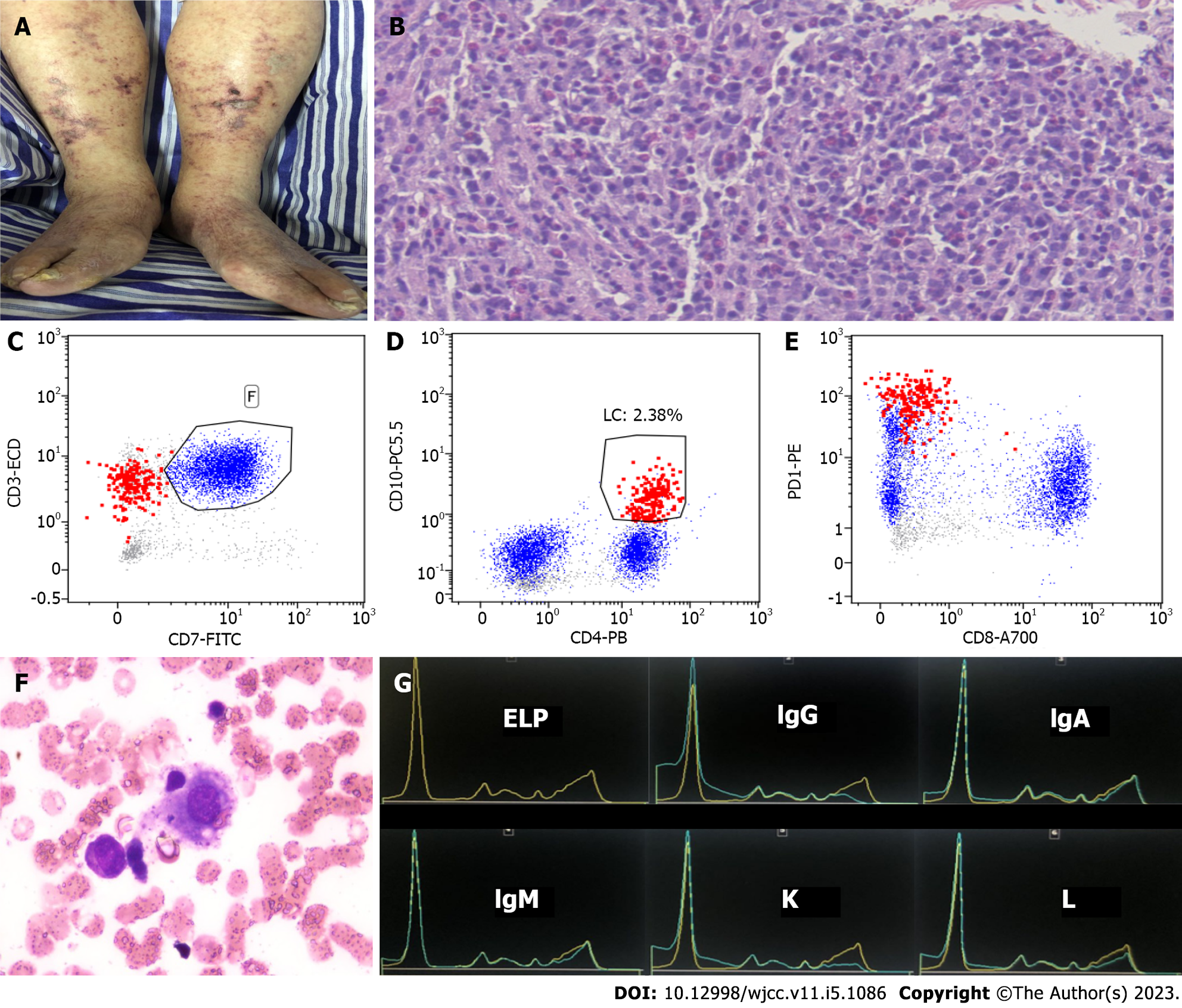
An 83-year-old man presented with fever and purpura of both lower limbs for one month (Figure 1A).
The patient presented with fever and purpura of both lower limbs for one month. He had chills and fever, with the highest body temperature of 40 °C, accompanied by cough and phlegm, no nausea and vomiting, and no abdominal distention, abdominal pain, dizziness, headache, or other discomfort.
The patient was diagnosed with diabetes mellitus for more than one month, had a history of hypertension for more than 30 years, coronary heart disease for 10 years, and renal insufficiency for many years. He denied any history of tuberculosis.
Physical examination showed an appearance of mild anemia, neck, armpit, and groin lymph node enlargement, splenomegaly, and edema and visible purpura of both lower limbs, without other special manifestations.
Groin lymph node puncture showed disappearance of the normal structure of lymph nodes and heterogeneous infiltration of small to medium-sized lymphoma cells, with proliferation of eosinophils (Figure 1B). The lymphoma cells were positive for CD3, CD4, CD10, and PD1, but negative for CD7 and CD8 by flow cytometry (Figure 1C-E). Bone marrow examination showed hemophagocytosis (Figure 1F) without evidence of lymphoma involvement. The hemoglobin concentration and platelet count declined rapidly, with the minimum value of 65 g/L and 53 × 109/L, respectively. A serological examination showed hypertriglyceridemia (triglycerides 3.14 mmol/L), normal value of serum ferritin (299.50 μg/L), elevated levels of soluble interleukin (IL)-2 receptor (16080 U/mL), and hypergammaglobulinaemia. The capillary electrophoresis revealed monoclonal IgG kappa (Figure 1G), without evidence of monoclonal plasma cells in bone marrow and lymph nodes. The coagulation function examination rapidly showed the maximum level of D-dimer (3.85 mg/L), prolonged prothrombin time (52.6 s), prolonged activated partial thromboplastin time (54.1 s), maximum value of International Normalized Ratio (4.57), and hypofibrinogenemia (fibrinogen 1.2 g/L). The dynamic changes of white blood cell (WBC) count, lymphocyte cell count, neutrophil count, and neutrophil-to-lymphocyte ratio (NLR) from nearly onset to death are listed in Table 1.
| Index date | WBC count (× 109/L) | Lymphocyte cell count (× 109/L) | Neutrophil count (× 109/L) | NLR |
| 4-9 | 7.59 | 0.10 | 7.26 | 72.6 |
| 4-14 | 4.78 | 0.48 | 3.98 | 8.29 |
| 4-22 | 5.22 | 0.21 | 4.85 | 23.01 |
| 4-25 | 5.14 | 0.34 | 3.90 | 11.47 |
| 4-27 | 3.83 | 0.33 | 2.89 | 8.76 |
| 4-29 | 5.77 | 0.32 | 4.74 | 14.81 |
| 5-1 | 5.19 | 0.40 | 4.61 | 11.53 |
Positron emission tomography showed splenomegaly, generalized lymphadenopathy, and enhanced activity in the posterior pharyngeal wall, bilateral neck, hilum of the lung and mediastinum, pelvic wall, mesenteric lymph nodes, and groin, suggestive of lymphoma (Figure 2).
The patient was finally diagnosed as having AITL induced HLH and DIC.
The patient’s son chose to refuse treatment.
The patient rapidly succumbed to gastrointestinal bleeding and septic shock. The time between onset and death was about one month.
AITL is aggressive and mainly affects older individuals (median age of 65 years), with a median survival of < 3 years[2,3]. The survival time of our patient was only about one month from onset to death. This was rare and indicated that the disease course was very aggressive.
A few studies reported that AITL was associated with plasma cell proliferation[4-6]. Monoclonal immunoglobulins were detected in this case, without evidence of monoclonal plasma cells. We speculated that AITL related to immunoregulatory disorder stimulated clonal plasma cell proliferation, but it may be undetectable. However, the mechanism involved in the development of the concomitant monoclonal immunoglobulins remains to be clarified. High levels of cytokines, such as IL-6, IL-10, and TNF-α, may serve as possible contributing factors[4,5,7-10]. Whether the concomitant plasma cell proliferation indicated a poor prognosis in AITL deserves further investigation.
There have been few reported cases of AITL associated HLH. One study reported that HLH occurred in a 57-year-old man with AITL during chemotherapy. He subsequently developed multi-organ failure and died after a few days[11]. Another case report described an AITL patient who relapsed with HLH two months after receiving chemotherapy supported by autologous peripheral blood stem cell transplantation (PBSCT). The patient was successfully treated with allogeneic PBSCT with reduced intensity conditioning regimen[12]. Including our case, three cases of AITL induced HLH were confirmed at the time of AITL diagnosis, not during chemotherapy or relapse[13,14]. The clinical features of the three cases are listed in Table 2 (patients 1, 2, and 4. Patient 4 was the present case). HLH is a life-threatening severe complication of AITL. AITL lymphoma cells may produce cytokines and chemokines that cause systemic complications[15]. Epstein-Barr virus (EBV) infected lymphocytes have been reported in up to 97% of AITL cases[16,17]. EBV infection may suggest a possible role for the virus in the etiology. EBV DNA was detectable in these three cases (Table 2). AITL associated HLH had a poor prognosis due to aggressive disease course, especially in the presence of EBV infection, in conjunction with genetic abnormalities and immune dysfunction[16]. Patients 1 and 2 were successfully treated with etoposide together with CHOP regimen and allogeneic HSCT with RIC, respectively. However, our patient (patient 4) had AITL associated HLH with concomitant DIC, and rapidly succumbed to gastrointestinal bleeding and septic shock. There was only one AITL induced DIC case reported previously[18]. The clinical features of the case are listed in Table 2 (patient 3). DIC was mostly caused by sepsis, shock, solid cancer, and hematological malignancies[19,20]. When associated with hematological malignancy, DIC was most frequently accompanied by newly diagnosed acute promyelocytic leukemia (APL) (approximately 70%)[21], followed by non-APL acute myeloid leukemia (17%) and non-Hodgkin’s lymphoma (11%)[22,23]. Coagulopathy with hypofibrinogenemia could also occur with HLH. We could not exclude that DIC was part of the HLH process in our patient. The disease course was very aggressive when accompanied by DIC. Patient 3 succumbed to DIC and fatal gastrointestinal bleeding. Both of patient 3 and patient 4 had a very poor prognosis.
| Patient 1 | Patient 2 | Patient 3 | Patient 4 (the present case) | |
| Sex/age (yr) at the time of diagnosis | 53/male | 62/female | 72/female | 83/male |
| Laboratory findings in peripheral blood | ||||
| % atypical lymphocytes in the blood of all lymphocytes | 9% | NA | NA | NA |
| Hypereosinophilia (%) | NA | NA | Yes (17%) | Yes (9%) |
| Autoantibodies | Antinuclear antibodies and anti-double-stranded DNA antibodies were negative | NA | NA | Anti-TIF-1γ antibodies and anti-Jo-1 antibodies were positive |
| Hypergammaglobulinaemia | Yes (polyclonal) | NA | Yes (polyclonal) | Yes (monoclonal) |
| EBV DNA copies (IU/mL) | 8.42 × 104 | NA, but positive in lymph node biopsy | NA | 131 |
| Immunophenotype/immunohistochemical staining | CD2+, CD3+, CD5+, CD7+, CD10+; CD20dim, PAX5dim, and telomerase Bdim (biopsies of the left cervical lymph node) | CD3+, CD4+, CD8,CD30, CD56 andCD20were negative (cervical lymph node biopsy) | CD4+, CD5+, CD10+ (lymph node) | CD3+, CD4+, CD10+, PD1+, CD7 and CD8 were negative- (lymph node) |
| Clinical manifestation | ||||
| Generalized lymphadenopathy | Yes | Yes | Yes | Yes |
| Bone marrow involvement | Hemophagocytosis and abnormal lymphocytes | Hemophagocytosis, but withoutevidence of lymphoma involvement | No lymphoma infiltration and no evidence of hemophagocytosis, bone marrow infiltration two weeks later | Hemophagocytosis, but without evidence of lymphoma involvement |
| Hepatomegaly | Yes | Yes | Yes | No |
| Splenomegaly | Yes | Yes | Yes | Yes |
| Skin rash/purpura | Yes | NA | NA | Yes |
| Pleural effusion | NA | NA | NA | Yes |
| Severe complication | ||||
| HLH | Yes | Yes | No | Yes |
| DIC | No | No | Yes | Yes |
| Therapy | Etoposide together with CHOP regimen | CHOP, mesna, ifosfamide, mitoxantrone, etoposide; allogeneic HSCT with RIC | Steroids | Anti-infection and other symptomatic treatment |
| Outcome | Successfully treated | Successfully treated | Succumbed to DIC and fatal gastrointestinal bleeding | Succumbed to gastrointestinal bleeding and septic shock |
The risk of death increased and treatment effectiveness decreased with age. Patient 4 was the oldest, followed by patient 3. To the best of our knowledge, our patient was the first case with AITL induced HLH and DIC. Survival was significantly related to age, male gender, mediastinal lymphadenopathy, and anaemia[2,24] which were adverse prognostic factors in our patient. Notably, NLR in AITL was a significant, independent prognostic factor for overall survival (OS), and NLR ≥ 2.2 indicated shorter OS[25]. Table 1 shows that the level of WBC count in our patient was almost within the normal range, whereas lymphocyte count was consistently at a low level and NLR was significantly high from nearly onset to death. We speculated that the patient suffered from severe immunosuppression, and the risk of death was greater when NLR was irreversibly sustained high. Consequently, HLH and DIC were induced, which resulted in rapid and fatal septic shock and gastrointestinal bleeding.
AITL is more aggressive in older adults. In addition to male gender, mediastinal lymphadenopathy, anaemia, and sustained high level of NLR may indicate a greater risk of death. Early diagnosis, early detection of severe complications, and prompt and effective treatment are vital.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Hematology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): E, E
P-Reviewer: Chaturvedi HTC, India; Goldman M, Belgium; Yikilmaz AS, Turkey S-Editor: Chen YL L-Editor: Wang TQ P-Editor: Chen YL
| 1. | Rüdiger T, Weisenburger DD, Anderson JR, Armitage JO, Diebold J, MacLennan KA, Nathwani BN, Ullrich F, Müller-Hermelink HK; Non-Hodgkin's Lymphoma Classification Project. Peripheral T-cell lymphoma (excluding anaplastic large-cell lymphoma): results from the Non-Hodgkin's Lymphoma Classification Project. Ann Oncol. 2002;13:140-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 332] [Cited by in RCA: 305] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 2. | Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R, Advani R, Ghielmini M, Salles GA, Zelenetz AD, Jaffe ES. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127:2375-2390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4245] [Cited by in RCA: 5395] [Article Influence: 599.4] [Reference Citation Analysis (0)] |
| 3. | Federico M, Rudiger T, Bellei M, Nathwani BN, Luminari S, Coiffier B, Harris NL, Jaffe ES, Pileri SA, Savage KJ, Weisenburger DD, Armitage JO, Mounier N, Vose JM. Clinicopathologic characteristics of angioimmunoblastic T-cell lymphoma: analysis of the international peripheral T-cell lymphoma project. J Clin Oncol. 2013;31:240-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 259] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 4. | Balagué O, Martínez A, Colomo L, Roselló E, Garcia A, Martínez-Bernal M, Palacín A, Fu K, Weisenburger D, Colomer D, Burke JS, Warnke RA, Campo E. Epstein-Barr virus negative clonal plasma cell proliferations and lymphomas in peripheral T-cell lymphomas: a phenomenon with distinctive clinicopathologic features. Am J Surg Pathol. 2007;31:1310-1322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 68] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 5. | Huppmann AR, Roullet MR, Raffeld M, Jaffe ES. Angioimmunoblastic T-cell lymphoma partially obscured by an Epstein-Barr virus-negative clonal plasma cell proliferation. J Clin Oncol. 2013;31:e28-e30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Zettl A, Lee SS, Rüdiger T, Starostik P, Marino M, Kirchner T, Ott M, Müller-Hermelink HK, Ott G. Epstein-Barr virus-associated B-cell lymphoproliferative disorders in angloimmunoblastic T-cell lymphoma and peripheral T-cell lymphoma, unspecified. Am J Clin Pathol. 2002;117:368-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 152] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 7. | Sakai H, Tanaka H, Katsurada T, Yoshida Y, Okamoto E, Ohno H. Angioimmunoblastic T-cell lymphoma initially presenting with replacement of bone marrow and peripheral plasmacytosis. Intern Med. 2007;46:419-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Yamane A, Awaya N, Shimizu T, Ikeda Y, Okamoto S. Angioimmunoblastic T-cell lymphoma with polyclonal proliferation of plasma cells in peripheral blood and marrow. Acta Haematol. 2007;117:74-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Ahsanuddin AN, Brynes RK, Li S. Peripheral blood polyclonal plasmacytosis mimicking plasma cell leukemia in patients with angioimmunoblastic T-cell lymphoma: report of 3 cases and review of the literature. Int J Clin Exp Pathol. 2011;4:416-420. [PubMed] |
| 10. | Nagoshi H, Kuroda J, Kobayashi T, Maegawa S, Chinen Y, Kiyota M, Nakayama R, Mizutani S, Shimura Y, Yamamoto-Sugitani M, Matsumoto Y, Horiike S, Taniwaki M. Clinical manifestation of angioimmunoblastic T-cell lymphoma with exuberant plasmacytosis. Int J Hematol. 2013;98:366-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Vella JE, El-Daly H. Hemophagocytic lymphohistiocytosis in a patient with angioimmunoblastic lymphoma: a case report and review of the literature. Int J Surg Pathol. 2012;20:606-609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Matsumura Y, Kuroda J, Shimura Y, Kiyota M, Yamamoto-Sugitani M, Kobayashi T, Matsumoto Y, Horiike S, Taniwaki M. Cyclosporine A and reduced-intensity conditioning allogeneic stem cell transplantation for relapsed angioimmunoblastic T cell lymphoma with hemophagocytic syndrome. Intern Med. 2012;51:2785-2787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Zhang L, Tong C, Tan Y, Peng S, He Y, Wang T. Hemophagocytic lymphohistiocytosis presenting with annular erythema multiforme-like eruptions in a patient with angioimmunoblastic T cell lymphoma: A case report. Exp Ther Med. 2018;16:2060-2065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Yu JT, Hwang WL, Wang RC, Teng CL. Reduced intensity conditioning allogeneic hematopoietic stem cell transplant could be beneficial to angioimmunoblastic T-cell lymphoma patients with hemophagocytic lymphohistiocytosis. Ann Hematol. 2012;91:805-807. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Iannitto E, Ferreri AJ, Minardi V, Tripodo C, Kreipe HH. Angioimmunoblastic T-cell lymphoma. Crit Rev Oncol Hematol. 2008;68:264-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 44] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 16. | Anagnostopoulos I, Hummel M, Finn T, Tiemann M, Korbjuhn P, Dimmler C, Gatter K, Dallenbach F, Parwaresch MR, Stein H. Heterogeneous Epstein-Barr virus infection patterns in peripheral T-cell lymphoma of angioimmunoblastic lymphadenopathy type. Blood. 1992;80:1804-1812. [PubMed] |
| 17. | Weiss LM, Jaffe ES, Liu XF, Chen YY, Shibata D, Medeiros LJ. Detection and localization of Epstein-Barr viral genomes in angioimmunoblastic lymphadenopathy and angioimmunoblastic lymphadenopathy-like lymphoma. Blood. 1992;79:1789-1795. [PubMed] |
| 18. | Pircher A, Verdorfer I, Brunner A, Hopfinger G, Steurer M. Paraneoplastic phenomena and diagnostic challenges in angioimmunoblastic T-cell lymphoma (AITL): report of two cases and review of the literature. In Vivo. 2014;28:327-332. [PubMed] |
| 19. | Okajima K, Sakamoto Y, Uchiba M. Heterogeneity in the incidence and clinical manifestations of disseminated intravascular coagulation: a study of 204 cases. Am J Hematol. 2000;65:215-222. [PubMed] [DOI] [Full Text] |
| 20. | Singh B, Hanson AC, Alhurani R, Wang S, Herasevich V, Cartin-Ceba R, Kor DJ, Gangat N, Li G. Trends in the incidence and outcomes of disseminated intravascular coagulation in critically ill patients (2004-2010): a population-based study. Chest. 2013;143:1235-1242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 21. | Ikezoe T. Pathogenesis of disseminated intravascular coagulation in patients with acute promyelocytic leukemia, and its treatment using recombinant human soluble thrombomodulin. Int J Hematol. 2014;100:27-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 22. | Uchiumi H, Matsushima T, Yamane A, Doki N, Irisawa H, Saitoh T, Sakura T, Jimbo T, Handa H, Tsukamoto N, Karasawa M, Miyawaki S, Murakami H, Nojima Y. Prevalence and clinical characteristics of acute myeloid leukemia associated with disseminated intravascular coagulation. Int J Hematol. 2007;86:137-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 56] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 23. | Chi S, Ikezoe T. Disseminated intravascular coagulation in non-Hodgkin lymphoma. Int J Hematol. 2015;102:413-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Siegert W, Agthe A, Griesser H, Schwerdtfeger R, Brittinger G, Engelhard M, Kuse R, Tiemann M, Lennert K, Huhn D. Treatment of angioimmunoblastic lymphadenopathy (AILD)-type T-cell lymphoma using prednisone with or without the COPBLAM/IMVP-16 regimen. A multicenter study. Kiel Lymphoma Study Group. Ann Intern Med. 1992;117:364-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 80] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 25. | Hong H, Fang X, Huang H, Wang Z, Lin T, Yao H. The derived neutrophil-to-lymphocyte ratio is an independent prognostic factor in patients with angioimmunoblastic T-cell lymphoma. Br J Haematol. 2020;189:908-912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |