Published online Feb 16, 2023. doi: 10.12998/wjcc.v11.i5.1000
Peer-review started: October 9, 2022
First decision: November 25, 2022
Revised: December 23, 2022
Accepted: January 16, 2023
Article in press: January 16, 2023
Published online: February 16, 2023
Processing time: 127 Days and 23.9 Hours
It has been said that the number of orthopaedic claims has increased in the last few years. Investigation through the most prevalent cause would help to prevent further cases.
To review the cases of medical complaints in orthopedic patients who had been involved in a traumatic accident.
A retrospective multi-center review of trauma orthopaedic-related malpractice lawsuits from 2010 to 2021 was conducted utilizing the regional medicolegal database. Defendant and plaintiff characteristics along with fracture location, allegations, and litigation outcomes were investigated.
A total of 228 claims referred to trauma-related conditions with a mean age of 31.29 ± 12.56 were enrolled. The most common injuries were at hand, thigh, elbow, and forearm, respectively. Likewise, the most common alleged complication was related to malunion or nonunion. In 47% of the cases, the main problem that led to the complaint was the inappropriate or insufficient explanation to the patient, and in 53%, there was a problem in the surgery. Eventually, 76% of the complaints resulted in a defense verdict, and 24% resulted in a plaintiff verdict.
Surgical treatment of hand injuries and surgery in non-educational hospitals received the most complaints. The majority of litigation outcomes were caused by a physician’s failure to fully explain and educate the traumatic orthopedic patients and technological errors.
Core Tip: Given that orthopedics is ranked as the third most dangerous medical specialty by medical indemnity insurers, an investigation into it is necessary. Many of these complaints arose from a failure to adequately inform patients of the dangers and advantages of their treatment. Surgical treatment of hand injuries was the most complaints from patients in our study. The majority of litigation outcomes were caused by a physician’s failure to fully explain and educate the traumatic orthopedic patients and a technological error. The remedies to these issues are knowledge, practical surgical expertise, and behavioral education.
- Citation: Salimi M, Heidari MB, Ravandi Z, Mosalamiaghili S, Mirghaderi P, Jafari Kafiabadi M, Biglari F, Salimi A, Sabaghzadeh Irani A, Khabiri SS. Investigation of litigation in trauma orthopaedic surgery. World J Clin Cases 2023; 11(5): 1000-1008
- URL: https://www.wjgnet.com/2307-8960/full/v11/i5/1000.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i5.1000
Clinical malpractice has enormous financial consequences for healthcare systems around the world, as well as a significant impact on patients and families[1]. Malpractice is described as professional responsibility resulting from insufficient medical care due to a lack of competence, neglect, or deception. Furthermore, medical liability is defined as the duty to rectify or settle the consequences of medical intervention from a penal, civil, or administrative perspective[2].
Trauma and orthopedic surgery have generally been viewed as a highly litigious specialty because of the volume of operations performed and the accompanying concerns if errors or complications happen[3,4]. Orthopedics is ranked as the third most dangerous medical specialty by medical indemnity insurers, after obstetrics and neurosurgery[5].
Surgeons are also susceptible to burnout because of a high number of medical complaints. The risk of a medical error will rise if burnout occurs for whatever reason, leading to increased patient complaints[6]. Therefore, to avoid burnout among surgeons who deal mostly with trauma cases, it is essential to identify the most common causes of medical complaints.
Orthopaedic patients can be divided into two categories: Traumatic and non-traumatic. These patients are treated in different settings and circumstances. Trauma patients may not adjust to their condition; therefore, their expectations of treatment may be out of line with their state. Many of these complaints arose from a failure to adequately inform patients of the dangers and advantages of their treatment, in addition to the fact that the treatment team may have performed medical malpractice[7,8].
Therefore, this study aimed to investigate the cases of medical complaints in orthopedic patients who had been involved in a traumatic accident.
In this retrospective multi canter descriptive-analytical study, all litigations between March 2010 and March 2021 were studied using the medical councils of Kermanshah and Shiraz provinces. During the next step, the trauma orthopaedic claims were included for more detailed reviews.
We formally requested information about the involved orthopedist(s) and patient(s) as well as details about the alleged malpractice event. In terms of the event’s characteristics, the type of hospital where it occurred (public vs private hospitals), the afflicted anatomical location, the clinical outcome of the case (death vs permanent impairment), and the final forensic decision on the claim (confirmed malpractice vs rejected malpractice).
Demographic data including gender, age, occupation, delineation of geographic areas, comorbidities, history of previous psychiatric disease, and cause of injury were collected.
This study was conducted after obtaining permission from the Kermanshah University of Medical Sciences, Kermanshah, Iran. (IR.KUMS.REC.1399.1064). Data about claims are kept anonymous, and investigations are conducted in strict accordance with ethical standards and strictest confidence. Separating the data collector and analyst eliminated any individual bias in collecting and analyzing data. Additionally, the authors state that they have no conflicting interests during this study.
Continuous variables are expressed as means and standard deviations. Categorical variables were provided as percentages, and the chi-square test was used with a statistical cutoff of P < 0.05. Statistical analysis was performed using SPSS software for Windows, version 25.0 (IBM corporation).
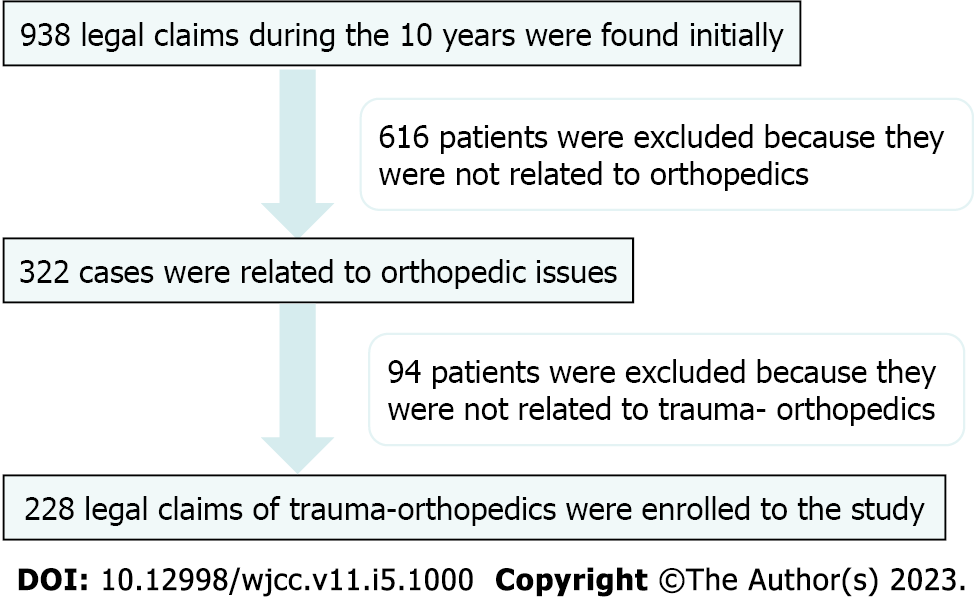
Among the 938 Legal claims during the 10 years mentioned above, 322 were related to orthopedic issues. After reviewing the files one by one, a total of 228 claims referred to trauma-related conditions, fulfilled our inclusion criteria, and were enrolled in the study. Figure 1 demonstrates the pathway of patient selection.
The mean age of the plaintiff was 31.29 years (SD: 12.56, range: 9-70). One hundred and four litigations were during the first half of the study period, while 124 were in the next, and no significant difference was found (P = 0.0879). The average time between the operation and the claim registration was 11.58 (± 15.85) mo, with a median of 6.5 mo. Furthermore, there were an average of 10.42 (± 6.38) mo between the initial litigation and the final forensic decision. Table 1 demonstrates the demographic features of the patients in our study.
| Variable | Frequency total = 228 | aP |
| Gender | < 0.0001 | |
| Male | 162 | |
| Female | 66 | |
| Residence | 0.0879 | |
| Urban | 104 | |
| Rural | 124 | |
| Occupation | 0.1100 | |
| Heavy worker | 54 | |
| Lightworker | 102 | |
| Sedentary | 48 | |
| Unknown | 24 | |
| Comorbidities | < 0.0001 | |
| Yes | 54 | |
| No | 174 | |
| History of psychiatric disease | < 0.0001 | |
| Yes | 12 | |
| No | 216 | |
| Couse of injury | 0.0110 | |
| Vehicle accident | 156 | |
| Falling down | 6 | |
| Occupational injury | 42 | |
| Injury at home | 24 | |
| Hospital of operation | 0.2200 | |
| Government non-educational clinic | 162 | |
| Government educational clinic | 12 | |
| Private clinic | 54 |
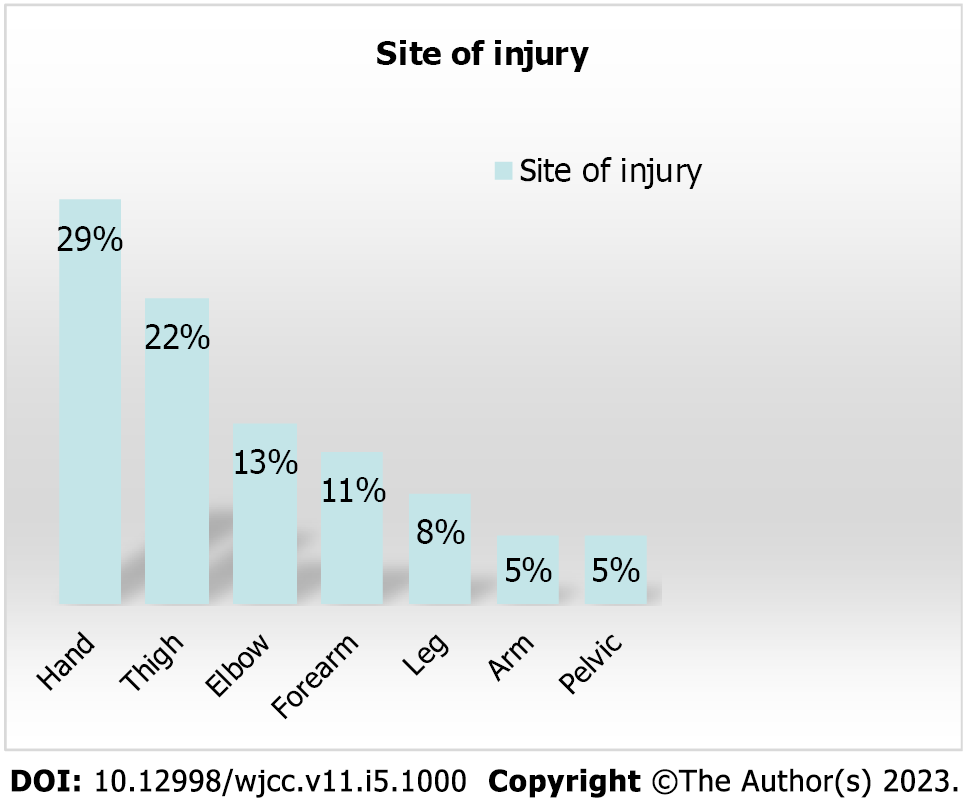
As the Figure 2 demonstrates, the most common injuries were at the hand, thigh, elbow, and forearm, respectively.
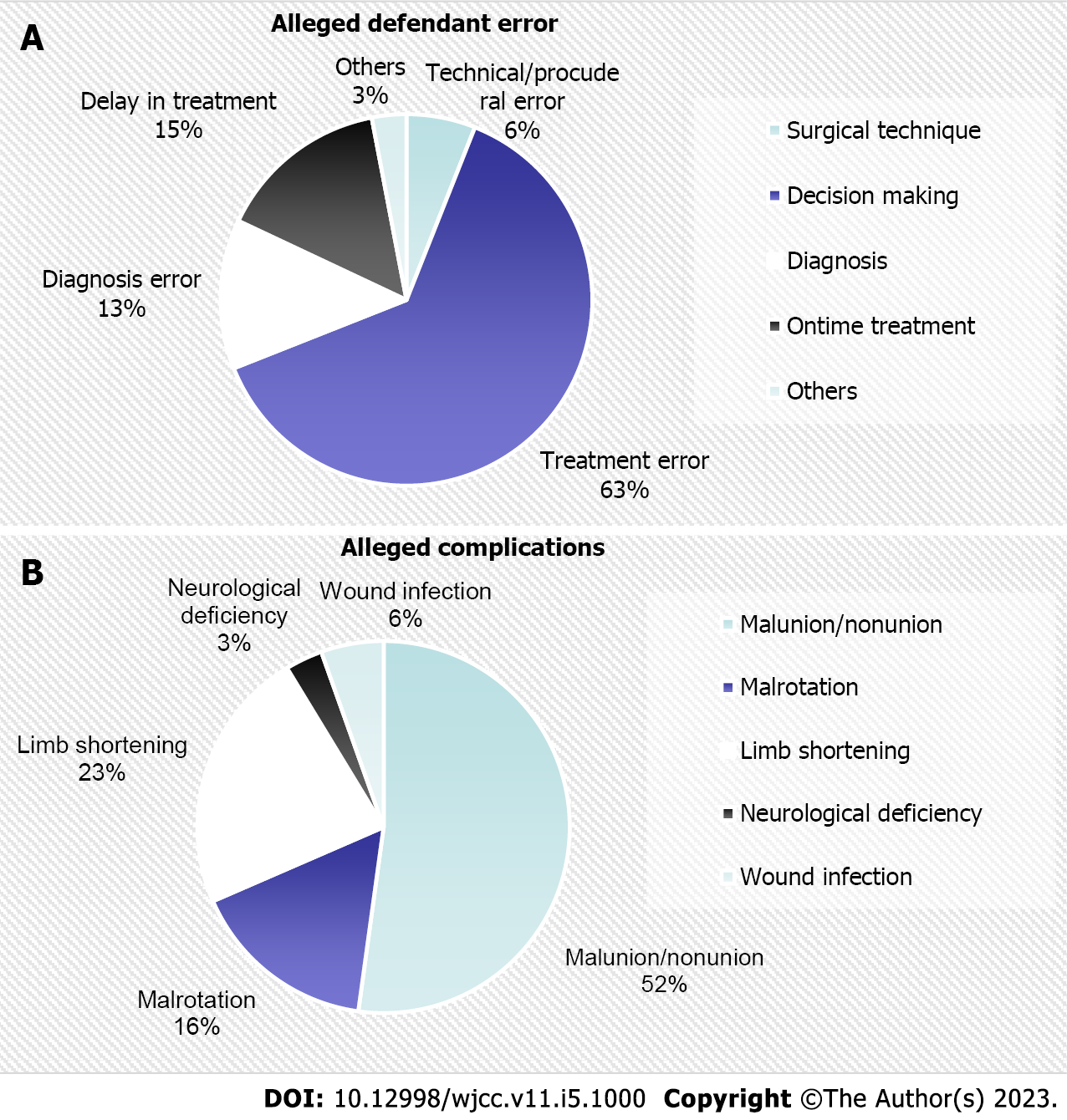
Based on our investigation, most of the alleged defendants’ error is believed to be that the wrong treatment was chosen for patients (Figure 3A). Likewise, the most common alleged complication was malunion or nonunion, and the least was attributed to neurological insufficiencies and surgical site infection, respectively (Figure 3B).
During further investigations, we found that the most common chief complaint was attributed to post-operation complications (58%), prolonged treatment period (18%), malrotation (16%), reoperation need (5%), and persistent pain (3%).
According to the forensic reviews, in 47% of the cases, the main problem that led to the complaint was the inappropriate or insufficient explanation to the patient. In 53%, there was a problem with the surgery (P = 0.2006).
Eventually, 76% of the complaints resulted in a defense verdict, and 24% resulted in a plaintiff verdict (P < 0.0001).
Our results indicate that the primary factor for patients to take action against orthopedic surgeons is the lack of sufficient explanation. Our results also indicated that the most alleged defendants’ errors are a lack of proper decision-making. Based on our analysis, hand injuries[9] were the most common anatomic location of the complaint, with finger malalignment/rotation being the most frequently reported chief complaint. In our study, non-unions, malunions, limb length discrepancies, loss of movement, and residual deformities are the most common cases that are made legal statements against. according to our analysis, patients treated in educational hospitals were less likely to file complaints, even though these hospitals treated more patients, this fact has been highlighted in previous studies as well[10,11].
Fear of litigation causes changes in clinical practice and encourages the abuse of healthcare resources. According to published studies, this can lead to physicians ordering further lab data workup and radiography as a defense strategy against court suits[12,13]. Orthopedic surgeons’ defensive medicine is a significant factor in health care costs with marginal benefit to patients[14]. Understanding the factors that influence litigation outcomes and the factors that generate litigation can help physicians take preventative measures to decrease future litigation risks.
Our assessments show that there has been no significant increase in the number of grievances. The prevalence of litigation claims in Iran is mainly dependent on the region, living conditions, and level of culture of the area in which data is gathered[15]. However, globally speaking, we should proceed with caution in this instance. There is an often-stated trend of increasing litigation cases, however, this trend remains controversial[16,17]. Cichos et al[16] conducted a study on national orthopedic settlement and verdict reports between 1988 and 2013. The results indicated a 215% growth in litigation frequency and also a 280% upturn in the settlement. Erivan et al[17] has also reported a rise in post-arthroplasty complaints between 2006 and 2016 from 0.2% up to 1.2%. on the contrary; a handful of studies indicate decreasing numbers of litigation. A recent study by Gathen et al[18] on an institutional legal database, including all litigations between 2000 and 2017 in a university teaching hospital has shown that significantly fewer litigations per 1000 cases were filed overall in 2009–2017 (65% less; P = 0.003) than in 2000–2008.
Our results indicated that hand complications were the highest, this is closely related to the negative impact it has on the patient’s occupational, social, and mental status. Mouton et al[19] reported a study on eighty claims of hand wounds, filed between 2007 and 2010 that most of the claims, the patient had major cutbacks on occupational and social activities. In a survey by Atrey et al[1], which reviewed 1473 trauma and elective cases of all orthopedic anatomical sites, the most common cause of chief complaint was hip. This gives us more areas to explore the origin of this finding in our study. According to a study by Sasor et al[20], on 430 cases related to hand surgery between 1989 and 2018, the most common reasons for negligence in forensic cases were Failure to diagnose/treat and surgical negligence. Physicians with subspeciality were significantly more likely to win cases which stresses the status of coordinated care in this matter. To avoid being accused of incompetence, surgeons may require a recommendation from other co-workers to validate surgical skills developed across a career. patients may rest easy knowing they are getting the best care possible from surgeons who are aware of their limitations and will refer them to specialists if necessary[21].
Our results indicated the most common problem leading to litigation was inappropriate or insufficient explanations in 47% of the cases. One of the most critical discussions with trauma patients is how to provide knowledge during this brief moment of trauma time to treatment, think about it, and make judgments based on that education. Performing a process that may be done optimally, effectively, and without regular execution of informed consent helps a lot in this case[22], as we discovered that slightly less than half of the complaints were due to a lack of appropriate explanation. Listening, accepting responsibility, apologizing, and doing all we can to make things right with the patient dramatically minimizes the chance of a malpractice lawsuit[23]. Many experts advise against this, and we realize this is contrary to what many people think is the best course of action in today’s society. To some, this may seem counterintuitive, but genuine remorse helps control the patient’s (or family members’) anger, and it also helps build a personal link between them[24]. It has been proven by Atrey et al[1] that improved communication skills, empathy, monitoring, and patient education can significantly reduce the number of litigations. Just like in any other field, educating patients and building trust with them is critical[3].
The most common chief complaint leading to filed complaints was attributed to post-operation complications. The reported rate for complications in trauma surgery is 21.1%, with the incidence of error being 8.7%[25]. Stewart et al[23] has reported no significant difference while dealing with trauma patients compared with other surgical patients and stated the overall actual risk of a malpractice lawsuit to be low. But, when dealing with trauma patients, it is critical to plan ahead of time to avoid therapeutic mistakes, which have been the most common problem. Moreover, achieving the ideal condition and providing the necessary infrastructure[15] is necessary. Hospital infrastructure, surgical equipment, operating rooms, and orthopedic surgeons all play a role in determining the outcome of a patient’s surgery[18]. Training for high-risk cases of patient complaints and ongoing training throughout practice is quite a beneficial matter[26]. Trauma surgeons’ training needs to be more competency-based and behavioral training in dealing with problems and legal issues may fit through the programs; considering that most trauma surgeons are newly graduated, preventing these incidents is essential[18].
Finally, the amount of time it takes for a claim to be registered (6.5 mo) and the compensation made in favor of patients suffering negligence is considerably lower in our study than in developed countries. Understandably, these issues need further investigation to be clarified; the legal system is much involved in this matter. The amount of compensation may seem vague to be announced due to currency issues and inflation in our country[27]. This makes it difficult to analyze the effect of compensation claims in Iran compared to other countries and its effect as a patient safety indicator[28].
This study presents data from litigations occurring in two medical councils of Kermanshah and Shiraz provinces in Iran faced over a period of 11 years. Our study has limitations; one of the first limitations of our study was the possible disparities that could influence our data due to sources’ origin. needless to say, we can use the findings of this study to help develop new policies in this instance. Another limitation due to currency concerns in our country, we cannot compare remuneration in successful claims in other research. Also, due to Freedom of Information Act restrictions, the study did not provide a more detailed clinical picture of individual claims.
Surgical treatment of hand injuries and surgery in non-educational hospitals received the most complaints from patients in our study. Most litigation outcomes were caused by a physician’s failure to fully explain and educate the traumatic orthopedic patients and a technological error.
Trauma orthopedic have been viewed as a highly litigious specialty because of the volume of operations performed and the accompanying concerns if errors or complications happen.
Many complaints n trauma orthopedics arose from a failure to adequately inform patients of the possible adverse effect and advantages of their management. Therefore an investigation in the possible underlying cause of litigation may prevent their recurrence.
To investigate the cases of medical complaints in orthopedic patients who had been involved in traumatic events
A retrospective review of trauma orthopedic malpractice from 2010 to 2021 was conducted utilizing the regional medico-legal database.
A total of 228 claims referred to trauma-related conditions. The most common alleged complication was related to malunion or nonunion. In 47% of the cases, the main problem that led to the complaint was the inappropriate or insufficient explanation to the patient, and in 53%, there was a problem in the surgery.
Most litigation outcomes were caused by a physician’s failure to fully explain and educate the traumatic orthopedic patients and a technological error.
The effect of fully explaining and educating traumatic orthopedic patients about the outcome and prevalence of litigation should be investigated.
The authors wish to express their gratitude to the Clinical Research Development Center of Taleghani and Imam Ali Hospital, University of Medical Sciences, Kermanshah, Iran, and Shohada Tajrish Clinical Research Development Center at Shahid Beheshti University of Medical Sciences in Tehran, Iran, for their support, data collection, cooperation, and assistance throughout the study and manuscript preparation.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Iran
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Abulsoud MI, Egypt; Chrcanovic BR, Sweden S-Editor: Chen YL L-Editor: A P-Editor: Chen YL
| 1. | Atrey A, Gupte CM, Corbett SA. Review of successful litigation against english health trusts in the treatment of adults with orthopaedic pathology: clinical governance lessons learned. J Bone Joint Surg Am. 2010;92:e36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 60] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 2. | Aguirre-Gas HG, Zavala-Villavicencio JA, Hernández-Torres F, Fajardo-Dolci G. Quality of medical care and patient surgical safety: medical error, malpractice and professional liability. Cir Cir. 2010;78:456-462. [PubMed] |
| 3. | Mouton J, Gauthé R, Ould-Slimane M, Bertiaux S, Putman S, Dujardin F. Litigation in orthopedic surgery: What can we do to prevent it? Orthop Traumatol Surg Res. 2018;104:5-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 4. | Fard SB, Mirghaderi SP, Moharrami A, Salimi M, Zarei M. Percutaneous sacroiliac screw fixation in a pediatric with unstable bilateral superior rami and sacral fracture-dislocation; a case report and review of the literature. Trauma Case Rep. 2022;40:100657. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 5. | Coyte PC, Dewees DN, Trebilcock MJ. Medical malpractice--the Canadian experience. N Engl J Med. 1991;324:89-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Travers V. Burnout in orthopedic surgeons. Orthop Traumatol Surg Res. 2020;106:S7-S12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 7. | Ahmed SA, DeFroda SF, Naqvi SJ, Eltorai AEM, Hartnett D, Ruddell JH, Born CT, Daniels AH. Malpractice Litigation Following Traumatic Fracture. J Bone Joint Surg Am. 2019;101:e27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 8. | Salimi M, Dehghani J, Gerami MH. Efficacy of Elastic Intramedullary Nails in Treating Axially Unstable Femur Fracture in Children. Pakistan J of Med Heal Sci. 2021;15:572-6. [DOI] [Full Text] |
| 9. | Majeed H. Litigations in trauma and orthopaedic surgery: analysis and outcomes of medicolegal claims during the last 10 years in the United Kingdom National Health Service. EFORT Open Rev. 2021;6:152-159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 10. | Nimptsch U, Mansky T. Hospital volume and mortality for 25 types of inpatient treatment in German hospitals: observational study using complete national data from 2009 to 2014. BMJ Open. 2017;7:e016184. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 108] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 11. | Adkins ZB, Malik AT, Jain N, Yu E, Kim J, Khan SN. Does Hospital Volume Affect Outcomes in Spine Surgeries? Clin Spine Surg. 2019;32:285-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 12. | Traina F. Medical malpractice: the experience in Italy. Clin Orthop Relat Res. 2009;467:434-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 52] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Kessler D, McClellan M. Malpractice Law and Health Care Reform: Optimal Liability Policy in an Era of Managed Care. J of Pub Econo. 2002;84:175-97. [DOI] [Full Text] |
| 14. | Sethi MK, Obremskey WT, Natividad H, Mir HR, Jahangir AA. Incidence and costs of defensive medicine among orthopedic surgeons in the United States: a national survey study. Am J Orthop (Belle Mead NJ). 2012;41:69-73. [PubMed] |
| 15. | Raeissi P, Taheri Mirghaed M, Sepehrian R, Afshari M, Rajabi MR. Medical malpractice in Iran: A systematic review. Med J Islam Repub Iran. 2019;33:110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 16. | Cichos KH, Ewing MA, Sheppard ED, Fuchs C, McGwin G Jr, McMurtrie JT, Watson SL, Xu S, Fryberger C, Baker DK, Crabtree RM, Murphy AB, Vaughan LO, Perez JL, Sherrod BA, Edmonds BW, Ponce BA. Trends and Risk Factors in Orthopedic Lawsuits: Analysis of a National Legal Database. Orthopedics. 2019;42:e260-e267. [PubMed] |
| 17. | Erivan R, Chaput T, Villatte G, Ollivier M, Descamps S, Boisgard S. Ten-year epidemiological study in an orthopaedic and trauma surgery centre: Are there risks involved in increasing scheduled arthroplasty volume without increasing resources? Orthop Traumatol Surg Res. 2018;104:1283-1289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Gathen M, Jaenisch M, Fuchs F, Weinhold L, Schmid M, Koob S, Wirtz DC, Wimmer MD. Litigations in orthopedics and trauma surgery: reasons, dynamics, and profiles. Arch Orthop Trauma Surg. 2022;142:3659-3665. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 19. | Mouton J, Houdre H, Beccari R, Tarissi N, Autran M, Auquit-Auckbur I. Surgical exploration of hand wounds in the emergency room: Preliminary study of 80 personal injury claims. Orthop Traumatol Surg Res. 2016;102:1009-1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Sasor SE, Chung KC. Litigation in Hand Surgery: A 30-Year Review. Plast Reconstr Surg. 2020;146:430e-438e. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Dutta S, Long WJ, Brown DF, Reisner AT. Automated detection using natural language processing of radiologists recommendations for additional imaging of incidental findings. Ann Emerg Med. 2013;62:162-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 76] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 22. | Bhutta MA, Arshad MS, Hassan S, Henderson JJ. Trends in joint arthroplasty litigation over five years: the British experience. Ann R Coll Surg Engl. 2011;93:460-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 23. | Stewart RM, Johnston J, Geoghegan K, Anthony T, Myers JG, Dent DL, Corneille MG, Danielson DS, Root HD, Pruitt BA Jr, Cohn SM. Trauma surgery malpractice risk: perception versus reality. Ann Surg. 2005;241:969-75; discussion 975. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 32] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 24. | Kraman SS, Hamm G. Risk management: extreme honesty may be the best policy. Ann Intern Med. 1999;131:963-967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 230] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 25. | Bosma E, Veen EJ, Roukema JA. Incidence, nature and impact of error in surgery. Br J Surg. 2011;98:1654-1659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 26. | Mozeika AM, Sachdev D, Asri R, Farber N, Paskhover B. Sociological and Medical Factors Influence Outcomes in Facial Trauma Malpractice. J Oral Maxillofac Surg. 2019;77:1042.e1-1042.e10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 27. | Gidwani S, Zaidi SM, Bircher MD. Medical negligence in orthopaedic surgery: a review of 130 consecutive medical negligence reports. J Bone Joint Surg Br. 2009;91:151-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 28. | Vicente-Guijarro J, Valencia-Martín JL, Fernández-Herreruela C, Sousa P, Mira Solves JJ, Aranaz-Andrés JM; SOBRINA Working Group. Surgical Error Compensation Claims as a Patient Safety Indicator: Causes and Economic Consequences in the Murcia Health System, 2002 to 2018. J Patient Saf. 2022;18:276-286. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |