Published online Dec 26, 2023. doi: 10.12998/wjcc.v11.i36.8595
Peer-review started: November 3, 2023
First decision: November 13, 2023
Revised: November 25, 2023
Accepted: December 7, 2023
Article in press: December 7, 2023
Published online: December 26, 2023
Processing time: 49 Days and 6.1 Hours
Herein, we report the case of a 13-year-old boy with spastic quadriplegia cerebral palsy (CP) at Gross Motor Function Classification System (GMFCS) level II, en
The boy presented with moderate mobility, balance, and overall well-being. He faced challenges with diminished lower limb strength, which affected his daily living and physical fitness capabilities. Our participant was diagnosed with spas
VBT is an innovative, individualized therapy that enhances physical function and QoL in CP, emphasizing its role in ambulatory patients.
Core Tip: This study examined the potential transformative effects of video game-based therapy (VBT) in adolescents diagnosed with cerebral palsy (CP). The 6-wk VBT program demonstrated notable improvements in lower limb strength, motor function, and overall quality of life. VBT is distinguished by its creative and patient-centric approach, which is customized to meet the unique needs of each individual. This study highlights the need to incorporate technology-driven rehabilitation approaches into treatment methods for ambulatory patients with CP. It emphasizes the significant implications of such an approach and sets the stage for future multicenter trials that consider a range of functional levels.
- Citation: Mohd Iqbal HA, Ho WS, Zanudin A, Hisham H, Mohd Nordin NA. Effects of video game-based therapy in an adolescent with cerebral palsy: A case report. World J Clin Cases 2023; 11(36): 8595-8602
- URL: https://www.wjgnet.com/2307-8960/full/v11/i36/8595.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i36.8595
Cerebral palsy (CP) is the most common motor disability among children, with an estimated prevalence of one to nearly four per 1000 live births worldwide, as reported by the Centers for Disease Control and Prevention in 2022. Enhancing the quality of life (QoL) has consistently been a primary objective and robust evaluative criterion in therapeutic interventions for adolescents with CP[1,2]. Considerable research has indicated significant empirical evidence regarding the efficacy of modern physiotherapy approaches currently available for children and adolescents diagnosed with CP. Among the existing approaches, video game-based therapy (VBT) can incorporate all the aforementioned elements in the therapeutic process owing to its distinctive attributes of being centered on video content and recreational activities, while being adaptable based on the user's condition. Furthermore, in addition to the heightened excitement experienced during physical activity, VBT offers instantaneous biofeedback to improve users’ movement patterns and experiences.
The current evidence indicates that VBT is a viable therapeutic option for enhancing arm function, postural control, and ambulation in adolescents with CP[3-6]. However, research on the impact of VBT on the physical functioning of children and adolescents with CP, specifically in terms of walking ability, gross motor skills, strength, and QoL, has been lacking. This inadequacy is particularly apparent in the absence of a comprehensive and reliable tool for assessing outcomes. Therefore, this study was conducted to provide essential empirical support for an alternative therapeutic approach for adolescents diagnosed with CP.
This study aimed to produce essential evidence that can assist healthcare professionals in assessing their patients while providing suggestions for their interventions. The present study examined the potential of VBT in enhancing physical function, including lower-limb strength, gross motor skills, walking capacity, and QoL in adolescents diagnosed with CP. The findings of this study provide essential information for healthcare professionals to evaluate their patients and act as a framework for guiding their interventions with patients. The results could potentially influence the physical health and overall well-being of adolescents diagnosed with CP and their respective families.
This case report is based on a boy who was 13 years and 3 months old he was diagnosed with spastic quadriplegia CP. His mother reported of his sedentary preference and inability to walk for long periods, especially outdoors and on inclined surfaces.
When diagnosed, the patient was classified as having Gross Motor Function Classification System (GMFCS) level II. He could walk without assistive equipment by employing a unique knee-gait pattern, and exhibited skills in traversing curbs, uneven surfaces, and barriers. Additionally, he could independently ascend and descend steps within his two-story home with one hand holding the rail.
The participant was born at full term with no other medical complications. He had mild jaundice, which is a common condition in many newborns. However, eventually, the participant's mother observed gross motor developmental deficits, including milestones, such as rolling, compared to his older siblings. Accordingly, the mother sought the expertise of a pediatrician at the hospital.
In 2009, he was referred to our hospital for various medical assessments. In mid-2010, he was officially diagnosed with spastic quadriplegia CP, which mainly explained his motor development impairments. He began his physiotherapy in 2009, following his mother's concerns about gross motor delay. Physiotherapy was conducted on a bi-monthly basis by a pediatric physiotherapist. Physiotherapy aims to provide motor training and home program strategies to effectively target the specific requirements and challenges of the participants.
Prior to VBT, his mother observed an increase in sedentary behavior and his son’s difficulties in long-distance walking, especially during outdoor activities and on inclined surfaces. These concerns were the primary motivating factors behind the pursuit of novel strategies to enhance his physical capabilities and overall well-being.
The patient had no family history of CP or other remarkable neurological conditions as claimed by the mother.
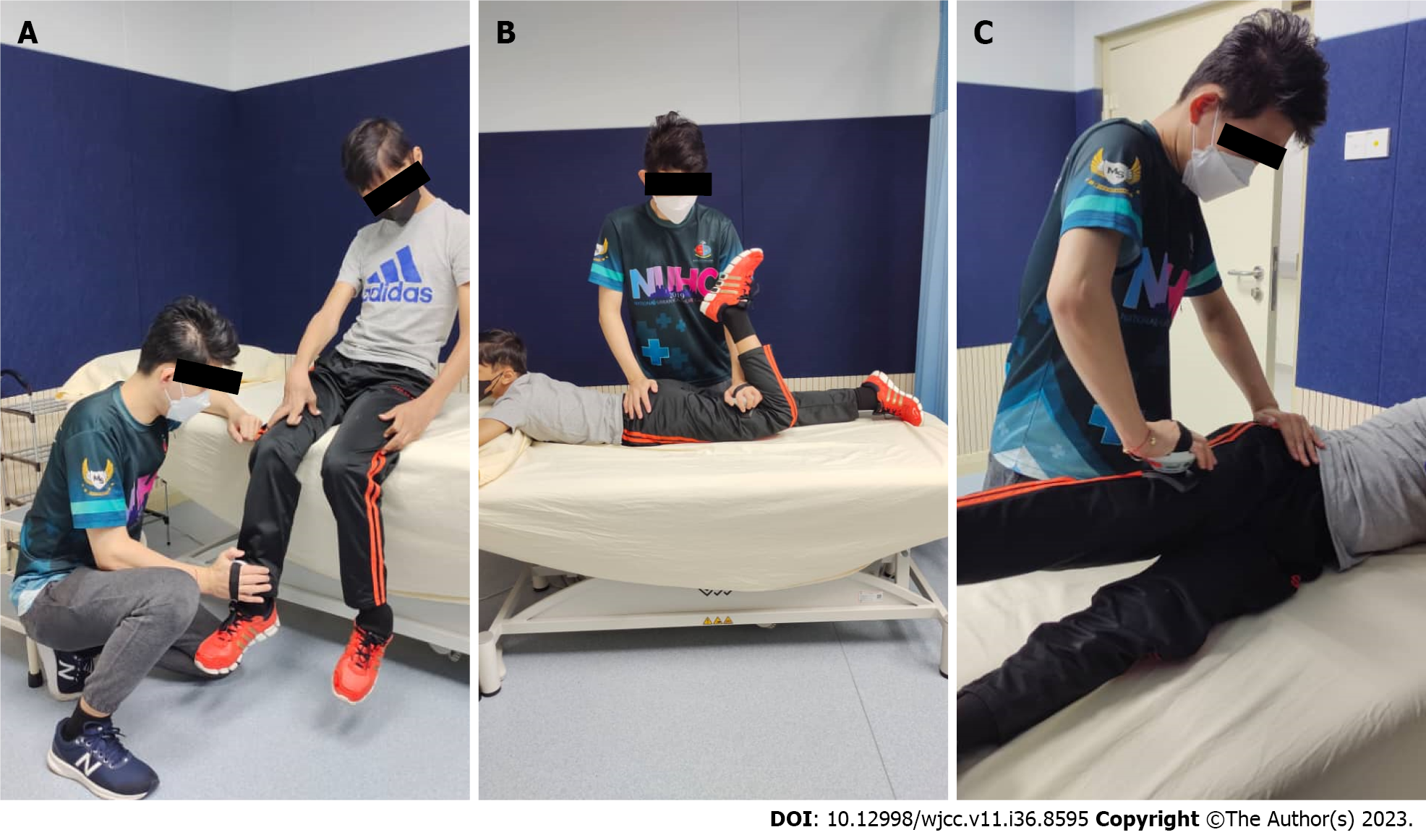
A comprehensive literature review was conducted before selecting assessments for the clinical decision-making process. Muscle strength with respect to body function was assessed using a handheld dynamometer. additionally, general motor ability is evaluated using the Gross Motor Function Measure (GMFM)-88. The 6-min walk test (6 MWT) was used to assess walking capacity, whereas the Pediatric QoL (PedsQL) tool in Malay was used to determine the QoL. Physical examination was performed twice, at baseline and after 4 weeks of VBT.
Muscle strength: Muscle strength was tested using a micro Force Evaluation and Testing 2 (microFET®2) handheld dynamometer (Hogan Health Industries Inc., United States), a small portable device held by the examiner, and placed against the participant’s limit during maximal isometric contraction. According to Goudriaan et al[7], a knee extension interclass correlation (ICC) value of 0.95 for children with CP indicated that the handheld dynamometer was highly reliable.
According to Neumann[8], a pathology that affects the strength, control, or extensibility of hip muscles can signi
Gross motor ability: According to the Center of Childhood Disability Research, the GMFM is a standardized observational instrument designed and validated to measure changes in gross motor function over time in children and adole
Walking capacity: The 6 MWT is a submaximal exercise test that involves walking for 6 min. ICC 0.98 was validated in the CP population by Thompson et al[11]. The 6 MWT was used to determine the participants walking capacity. The test was administered according to the standard protocol, implementing every instruction in accordance with the guidelines of the American Thoracic Society[12].
QoL: To explore the QoL, we chose a PedsQL parent’s proxy questionnaire consisting of a 5-point Likert Scale ranging from 0 to 4, covering four multidimensional functions, namely, physical, emotional, social, and school. Adapting to the local culture, the PedsQL questionnaire was translated into Malay to ease the patient’s career comprehension. The questionnaire has been validated with Cronbach’s α with a range (0.7–0.98) and factor correlation values ranging from 0.1 to 0.57[13].
The laboratory examinations are not applicable.
The imaging examinations is not applicable.
The final diagnosis of the case presented is spastic quadriplegia CP.
The VBT intervention was initiated in the second session after an initial session, in which baseline data assessments were conducted. An interventional session was conducted by a researcher under the guidance of the patient’s pediatric physiotherapist for 6 weeks, consisting of two sessions per week, with each session requiring approximately 1 hour. The principal objective of the program was to enhance engagement in physical activities. Balance, strength, and endurance training exercises were incorporated into the regimen using an X-Box 360 Kinect. The tasks included upper limb movements, marching, side-stepping, weight shifting, single-leg stance (SLS), kicking, squatting, and jumping. All interventions were adapted to be fun and engaging for young adolescents. To make the gaming session more fun and competitive, the researchers also participated in the gaming session during the participants’ resting period to motivate them to perform the tasks at their maximal performance.
Each session started with a warm-up of 10–15 min involving upper limb movements and low-intensity exercises such as side-stepping and marching at a low pace. The session was followed by balance training, such as weight shifting, SLS, and dynamic balance training; strength training involving marching, kicking, squatting, and jumping; and endurance training, a combination of all movements and movement strategies with more significant repetitions. Following this, progress was made according to the participants’ preferences and the researcher's observations. Throughout the in
| Component | Movements | Game |
| Warm up | Upper limb movements side | Dance central: Poker face |
| Stepping | Kinect adventures: Space pop | |
| Marching | Motion explosion: Balance beam | |
| Balance | Single leg stance | Kinect adventures: 20000 leaks |
| Weight shifting | Kinect sports: Target kick | |
| Ice age 4: Slip slider | ||
| Strength | Kicking | Kinect sports: Target kick |
| Jumping | Kinect adventures: River rush | |
| Marching | Kinect sports: Hurdles | |
| Kinect sports: Sprint | ||
| Endurance | Combination of marching, squatting, jumping, and upper limb movements | Ice age 4: Glacier hopper |
| Kinect adventures: Rally ball | ||
| Cool down | Upper limb movements Stepping | Kinect adventures: Space pop Motion explosion: Balance beam |
Clinical observation: The patient exhibited moderate thoracic scoliosis on the right side manifesting as an elevated right shoulder relative to the left shoulder. The participant could walk unaided while maintaining a mild jumping knee gait; however, he encountered challenges when sprinting and walking at high speeds. He could only walk in tandem for five steps and a SLS on the right foot for 2 s and 1 s on the left. He was only able to execute single-leg hopping with his right foot once using a double-hand grasp and was unable to conduct single-leg hopping with his left foot.
Outcome and follow-up
Clinical observation: He could run but still had a mild hopping knee gait. He could maintain the right foot SLS for 5.36 s, whereas he maintained the left foot SLS for 1.36 s. For running, he could now complete a distance of 4.5 min and 5.4 s instead of walking fast.
Description of outcomes: Post-intervention, there were marked increases in strength for his tested lower limb muscles, of which, the left hip extensor had gained the most improvement, from 199.3 N to 541.3 N, followed by the left hip abductor, from 201.1 N to 743.3 N.
The boy’s gross motor function in terms of standing and advanced activities, such as walking, running, and jumping demonstrated no improvement nor deterioration. A decreased of one score in GMFM component D. According to his walking capacity, the distance increased from 368 m to 450 m, yielding an improvement of 82 m.
Assessing the QoL of the boy using the mother’s proxy, the post-intervention PedsQL total scale score rose from 58.7 to 73.9, marking an increase of 17.06%. All the domains in PedsQL which are physical, emotion, social and schooling showed increased scores. The changes in muscle strength, gross motor ability, and QoL after the VBT intervention are shown in Table 2.
| Outcome measure | Pre-intervention | Post-intervention | Change (%) | |
| Muscle strength (N) | Left hip extensor | 199.3 | 541.3 | 34 (> 100) |
| Right hip extensor | 147.2 | 535.4 | 388.2 (> 100) | |
| Left hip abductor | 201.1 | 743.3 | 542.2 (> 100) | |
| Right hip abductor | 212.6 | 752.2 | 539.6 (> 100) | |
| Left knee extensor | 216.2 | 1017.9 | 801. (> 100) | |
| Right knee extensor | 290.1 | 1035.6 | 745.5 (> 100) | |
| GMFM-88 score | Dimension D standing (0-39) | 36 | 35 | 1 (2.7) |
| Dimension E walking, running, jumping (0-72) | 65 | 65 | - | |
| Walking distance (m) | 6 MWT | 368 | 450 | 82 (5.0) |
| Quality of life | PedsQL in physical (0-100) | 71.9 | 81.3 | 9.4 (13.0) |
| PedsQL in emotion (0-100) | 50.0 | 60.0 | 10 (20) | |
| PedsQL in social (0-100) | 35.0 | 65.0 | 30 (85.7) | |
| PedsQL in schooling (0-100) | 70.0 | 85.0 | 15 (21.4) | |
| PedsQL in total (0-100) | 58.7 | 73.9 | 15.2 (25.9) |
Adherence, adverse events, and participant feedback: The participants in this study showed good adherence to the program with 100% attendance. He did not miss any appointments for the program. No adverse events were observed during the intervention period. According to the participant, VBT was fun, and he did not experience fatigue or muscle soreness after every session. The participant’s caregiver also added that her child was more motivated and excited for VBT than the routine physiotherapy appointments.
The VBT intervention enhanced the physical function and QoL of a GMFCS level II adolescents with CP, as indicated by the achievement of positive results on almost all outcome measures. Furthermore, our participants demonstrated high adherence to and a desire to engage in all assigned tasks during the VBT sessions. Participants and their caregivers complied with the entire program and adhered to the schedule for each session. Consistent with findings from prior research[14,15], our participants also reported exceptional joy and amusement compared to routine interventions. Following these sessions, the patient exhibited enhancements in bodily structure, function, and QoL. The participant and his pediatric physiotherapist noted that his posture and balance improved after the intervention[14,15].
Our results are consistent with those of Gercek et al[16], which showed improved lower-extremity muscle strength from VBT. The bilateral hip extensors, hip abductors, and right knee extensors improved post-intervention, potentially because of the exercises performed during VBT training. The participants performed lower limb-intensive exercises during training, including marching, squatting, kicking, and jumping, at a specific velocity corresponding to the tempo of the events. As the required pace increases, stamina, endurance, and reaction time are required. Voluntary active range of motion, weight-bearing movements, and the functionality and velocity of the movements themselves must have contributed to the increase in muscle strength. Our hypothesis was consistent with findings by van Vulpen et al[17], showing an association of improvement in strength with the functionality of the velocity in strength training exercises.
Pre-intervention, the participant was able to perform most of the gross motor activities in GMFM component D (standing); however, he had difficulty in performing the SLS, with the right-foot SLS better than a left-foot SLS (right: 2 s; left: 1 s). After the intervention, SLS time in both feet improved, with right-foot SLS to a greater extent (right: 5.36 s; left: 1.56 s). With respect to component E (walking, running, and jumping), he possesses difficulty in performing tandem walking (5/10 steps), running 4.5 m (fast walking instead), and single leg hopping (right: One hop with two-hand held; left: 0/10 with two-hand held). Post-intervention, the changes were tandem walking (3/10 steps), running 4.5 m (able to run), and single-leg hopping (right: One hop without hand-held; left: 0/10). These changes were consistent with the findings of Gercek et al[16], who showed improvements in motor function post-intervention. These changes are likely due to the nature of virtual reality (VR), which addresses the critical factors of motor training, including intensity, repetition, task orientation, and multisensory environments. According to Brien and Sveistrup[18], enriched environments are known to promote neuronal plasticity changes documented using functional magnetic resonance imaging, and have shown that training in VR offers the potential for long-term learning from adaptive cerebral plasticity consistent with significant functional motor improvements in CP. Despite the minimal changes, we expect to see a more substantial improvement in the participants’ gross motor skills with a longer intervention of a minimum of 8 weeks is being performed, especially in the gait component. According to Ghai S and Ghai I[4], a VBT of less than 4 times per week, 20–30 min, for more than 8 weeks can have a maximum effect on gait. Therefore, a trial utilizing these suggestions could be conducted to harness this impact. In addition, the improvement in muscle strength and gross motor function to different extents was consistent with the findings of Shin et al[19], who showed no correlation between muscle strength and gross motor function in CP.
Upon pre-intervention, the participant completed a distance of 368 m. After the intervention, an increment of 82 m was obtained. This finding is consistent with a previous study[20] showing that VBT intervention can improve walking capacity in adolescents with CP. Throughout our intervention, the VBT involved repetitive practice and movement correction. As pointed out by Chen et al[3] in a similar study utilizing VR, the repetitions used during VR sessions were high, and the child performed up to 150 reaching movements in 3 min without realizing them while playing the video games. Although the repetitions of movement in our study were not recorded, more significant repetitions within a specific time frame are required, which we believe have contributed to the build-up of endurance in the participants, thus resulting in a significant outcome.
QoL improvement as a result of overall improvement in the participants’ physical and social functioning were reported with all aspects acquiring significant increment, and out of all, social functioning improved by the most (85.7%). An increase in score (from 4 to 2) was observed in Components 1 (relationships with other adolescents), 4 (inability to perform activities that other adolescents are capable of), and 5 (catching up with other adolescents’ pace). Two of the three questions were based on the participants’ physical abilities. With improvements in bodily functions shown in the physical functioning domain, which may have contributed to his school functioning domain improvement, the emotional and social aspects of the QoL increased significantly. Although the exact cause-and-effect relationship between these domains is still unknown, our findings indicate that the enhancements in gross motor function, walking ability, and overall physical functions, such as muscle strength, are indeed associated with the improvements observed in the social domain of the PedsQL, which are in line with the findings of Shelly et al[21], who stated that the psychological domain of QoL was significantly associated with the functioning level.
In conclusion, increments in muscle strength, particularly hip extensor, 6 MWT, GMFM-88 domains D and E, and PedsQL scores post-intervention, indicated that VBT could improve physical function and QoL of CP with GMFCS level II. Although the improvements are apparent, the results of this case study should be carefully interpreted as the outcomes of a single-subject case study have limited generalizability to a larger population, with limitations such as the short duration of the VBT program and follow-up assessment once participants finish the program. In the future, to ensure an optimal number of participants, recruitment planning should consider the barriers of participants visiting the clinic for VBT for two sessions per week. In addition, the PedsQL Adolescent Report should be employed to provide additional validation of the QoL outcomes. Subsequent research should focus on the frequency and durations of VBT interventions, with specific emphasis on the duration, number of sessions per week, and localization of VBT programs.
This is the first case report to examine the effect of VBT intervention in an adolescent with spastic quadriplegia and GMFCS level II CP in a local setting. This study demonstrated the clinical applicability of VBT intervention in elevating physical function with improvements in muscle strength, gross motor function, and walking capacity, ultimately improving the QoL of adolescents with CP. Table 3 sums up the advantages and disadvantages of standard care and VBT in adolescents with CP.
| Standard care for cerebral palsy | Video game-based therapy for cerebral palsy | |
| Functional training; Facilitation of normal patterns of movement; Passive range of motion; Stretching exercise; Strengthening exercise; Positioning; Manual technique; Functional electrical stimulation; Splinting; Maintenance training | Refer to Table 1 | |
| Pros | Basic technique and well-known by physiotherapists; Most of the essential equipment available in the physiotherapy department | Active motor training with progressive challenges; Motivational and fun activities; Games were tailored to patients' ability, preference, and functional goals; Bi-weekly training with a structured program and assessments |
| Cons | Patients tend to get bored with repetitive treatment | Physiotherapists need to be trained on how to operate the games; Not all physiotherapy department has the equipment and space for the VBT |
In summary, the aforementioned case study involving a 13-year-old boy diagnosed with spastic quadriplegic CP, underscores the need for timely identification and intervention in the field of pediatric neurological disorders. Despite difficulties in the gross motor development, he has sought and engaged in ongoing physiotherapy since 2009, which highlights the compliance and support of both his family and healthcare professionals in addressing his distinct requirements.
The implementation of VBT as a novel intervention shows the potential for improving participants’ physical functioning and QoL. The preliminary evaluation indicated his competence in walking while emphasizing his difficulties in navigating outdoor environments and ascending inclined slopes. The VBT, in conjunction with his family’s assistance, seeks to mitigate these constraints and enhance holistic welfare.
This case highlights the importance of customized therapies for children diagnosed with CP as well as the potential advantages of rehabilitation methods that include technology. As the intervention progresses, and subsequent assessments are conducted, significant insights will be gained regarding the efficacy of VBT in treating children with spastic quadriplegic CP. These findings serve as valuable resources for informing future treatment approaches for comparable instances.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Malaysia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Batta A, India S-Editor: Lin C L-Editor: A P-Editor: Lin C
| 1. | Zanudin A, Mercer T, Samaan C, Jagadamma K, McKelvie G, van der Linden M. A Community-Based Exercise Program For Ambulant Adolescents And Young Adults With Cerebral Palsy, A Feasibility Study. Eur J Adapt Phys Act. 2021;14:1-15. [DOI] [Full Text] |
| 2. | Zanudin A, Mercer TH, Jagadamma KC, van der Linden ML. Psychometric Properties Of Measures Of Gait Quality And Walking Performance In Young People With Cerebral Palsy: A Systematic Review. Gait Posture. 2017;58:30-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Chen Y, Fanchiang HD, Howard A. Effectiveness of Virtual Reality in Children With Cerebral Palsy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Phys Ther. 2018;98:63-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 125] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 4. | Ghai S, Ghai I. Virtual Reality Enhances Gait in Cerebral Palsy: A Training Dose-Response Meta-Analysis. Front Neurol. 2019;10:236. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 5. | Cho C, Hwang W, Hwang S, Chung Y. Treadmill Training with Virtual Reality Improves Gait, Balance, and Muscle Strength in Children with Cerebral Palsy. Tohoku J Exp Med. 2016;238:213-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 98] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 6. | Yoo JW, Lee DR, Cha YJ, You SH. Augmented effects of EMG biofeedback interfaced with virtual reality on neuromuscular control and movement coordination during reaching in children with cerebral palsy. NeuroRehabilitation. 2017;40:175-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | Goudriaan M, Nieuwenhuys A, Schless SH, Goemans N, Molenaers G, Desloovere K. A new strength assessment to evaluate the association between muscle weakness and gait pathology in children with cerebral palsy. PLoS One. 2018;13:e0191097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 8. | Neumann DA. Kinesiology of the hip: a focus on muscular actions. J Orthop Sports Phys Ther. 2010;40:82-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 387] [Cited by in RCA: 431] [Article Influence: 28.7] [Reference Citation Analysis (0)] |
| 9. | Yazici G, Varol F, Volkan M, Çitaker S. Reliability of make and break tests in assessing intrinsic foot muscle strength using A handheld dynamometer in healthy young adults. Türk Fizyoterapi ve Rehabilitasyon Dergisi. 2020;31:263-269. [DOI] [Full Text] |
| 10. | Te Velde A, Morgan C. Gross motor function measure (GMFM-66 & GMFM-88) User's manual, book review. Pediatric Physical Therapy. 2022;34:88-89. [RCA] [DOI] [Full Text] [Cited by in RCA: 17] [Reference Citation Analysis (0)] |
| 11. | Thompson P, Beath T, Bell J, Jacobson G, Phair T, Salbach NM, Wright FV. Test-retest reliability of the 10-metre fast walk test and 6-minute walk test in ambulatory school-aged children with cerebral palsy. Dev Med Child Neurol. 2008;50:370-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 168] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 12. | American Thoracic Society. . Guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111-117. |
| 13. | Ainuddin HA, Loh SY, Chinna K, Low WY, Roslani AC. Psychometric properties of the self-report Malay version of the Pediatric Quality of Life (PedsQLTM) 4.0 Generic Core Scales among multiethnic Malaysian adolescents. J Child Health Care. 2015;19:229-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Viana RB, de Oliveira VN, Dankel SJ, Loenneke JP, Abe T, da Silva WF, Morais NS, Vancini RL, Andrade MS, de Lira CAB. The effects of exergames on muscle strength: A systematic review and meta-analysis. Scand J Med Sci Sports. 2021;31:1592-1611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 15. | Bryanton C, Bossé J, Brien M, McLean J, McCormick A, Sveistrup H. Feasibility, motivation, and selective motor control: virtual reality compared to conventional home exercise in children with cerebral palsy. Cyberpsychol Behav. 2006;9:123-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 178] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 16. | Gercek N, Tatar Y, Uzun S. Alternative exercise methods for children with cerebral palsy: effects of virtual vs. traditional golf training. Int J Dev Disabil. 2022;68:933-942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 17. | van Vulpen LF, de Groot S, Rameckers E, Becher JG, Dallmeijer AJ. Improved Walking Capacity and Muscle Strength After Functional Power-Training in Young Children With Cerebral Palsy. Neurorehabil Neural Repair. 2017;31:827-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 49] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 18. | Brien M, Sveistrup H. An intensive virtual reality program improves functional balance and mobility of adolescents with cerebral palsy. Pediatr Phys Ther. 2011;23:258-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 81] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 19. | Shin HI, Sung KH, Chung CY, Lee KM, Lee SY, Lee IH, Park MS. Relationships between Isometric Muscle Strength, Gait Parameters, and Gross Motor Function Measure in Patients with Cerebral Palsy. Yonsei Med J. 2016;57:217-224. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Arnoni JLB, Pavão SL, Dos Santos Silva FP, Rocha NACF. Effects of virtual reality in body oscillation and motor performance of children with cerebral palsy: A preliminary randomized controlled clinical trial. Complement Ther Clin Pract. 2019;35:189-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 21. | Shelly A, Davis E, Waters E, Mackinnon A, Reddihough D, Boyd R, Reid S, Graham HK. The relationship between quality of life and functioning for children with cerebral palsy. Dev Med Child Neurol. 2008;50:199-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 81] [Article Influence: 4.8] [Reference Citation Analysis (0)] |