Published online Dec 16, 2023. doi: 10.12998/wjcc.v11.i35.8270
Peer-review started: October 26, 2023
First decision: November 20, 2023
Revised: December 1, 2023
Accepted: December 6, 2023
Article in press: December 6, 2023
Published online: December 16, 2023
Processing time: 48 Days and 21.9 Hours
Iron deficiency anemia (IDA) and thalassemia trait (TT) are the most common microcytic and hypochromic anemias. Differentiation between mild TT and early IDA is still a clinical challenge.
To develop and validate a new index for discriminating between IDA and TT.
Blood count data from 126 patients, consisting of 43 TT patients and 83 IDA pa
The new index is the ratio of hemoglobin to mean corpuscular volume. Its sen
This new index has good diagnostic performance in discriminating between mild TT and early IDA. It requires only two results of complete blood count, which can be a very desirable feature in under-resourced scenarios.
Core Tip: The ratio of hemoglobin to mean corpuscular volume was proposed and validated as a new index for discriminating between iron deficiency anemia and thalassemia trait, with a sensitivity and a specificity of 93.5% and 78.4%, respectively. This new index has good diagnostic performance and is useful in under-resourced scenarios.
- Citation: Yao QC, Zhai HL, Wang HC. Ratio of hemoglobin to mean corpuscular volume: A new index for discriminating between iron deficiency anemia and thalassemia trait. World J Clin Cases 2023; 11(35): 8270-8275
- URL: https://www.wjgnet.com/2307-8960/full/v11/i35/8270.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i35.8270
Anemia is still a global health burden with an estimated prevalence of 32.9% in 2010[1]. Iron deficiency anemia (IDA) and thalassemia trait (TT) are the most common microcytic and hypochromic anemias worldwide, primarily affecting people living in underdeveloped countries[2].
Correct diagnosis of IDA and TT is essential for choosing the right treatment method, which is distinctively different between these two anemias. Diagnosing IDA requires measuring the levels of serum ferritin and iron, and total iron binding capacity. β-Thalassemia trait can be diagnosed by a level of hemoglobin subunit alpha 2 (HbA2) higher than 3.5% using hemoglobin electrophoresis. Whereas α-thalassemia trait is indicated by the presence of α-gene mutations using genetic testing. However, these gold standard tests are time-consuming and expensive, which significantly restricts their use and access in scenarios with limited medical resources.
By using red blood cell (RBC) parameters, various mathematical formulas have been constructed as indexes to dis
The present study aimed to propose and validate a novel index to discriminate between IDA and TT using the most common RBC parameters.
This was a retrospective study analyzing the clinical data of the patients diagnosed with IDA or TT during January 2019 through December 2021 at our hospital. The inclusion criteria were: (1) Age ≥ 18 years; and (2) mild TT [mean corpuscular volume (MCV) 55-85 fL, HbA2 levels > 3.5%] or early IDA (Hb > 90 g/L, MCV 55-85 fL, ferritin < 12 ng/mL)[8]. Patients were excluded if they had malignant diseases or active infections. IDA patients with α-TT were also excluded. The study was approved by the Shanghai Tenth People’s Hospital, Tongji University School of Medicine.
Two milliliters of venous blood were drawn from each participant using ethylenediaminetetraacetic acid-containing tubes. Blood cells were counted by using an automated blood cell counter (Sysmex, XS-500i, Japan). Hemoglobin electrophoresis was performed at pH 8.6. levels of HbA2 were measured by the elution method using a cellulose acetate strip. Mutations that cause α-TT were identified using gene sequencing. The serum levels of ferritin were measured using another 5 mL uncoagulated veinous blood using the chemiluminescent immunoassay method.
To develop a new index for discriminating IDA and TT, the clinical data of 126 consecutive patients were reviewed. Linear and nonlinear fisher discriminant curves and receiver operating characteristic (ROC) curves were drawn. Then the formula of the index was determined according to the largest area under the curve. This new index was further validated in another 110 consecutive patients.
The variables between patients with IDA and patients with TT were compared using the Mann-Whitney test due to the non-normal distribution of the data. The degree of agreement between the new index and the gold standards in diagnosing IDA and TT was analyzed using the Kappa coefficient. ROC curves were drawn using a non-parametric method. All statistical analyses were performed using SPSS Statistics 20 software (IBM Corp, Armonk, NY, United States). A P value less than 0.05 was considered statistically significant.
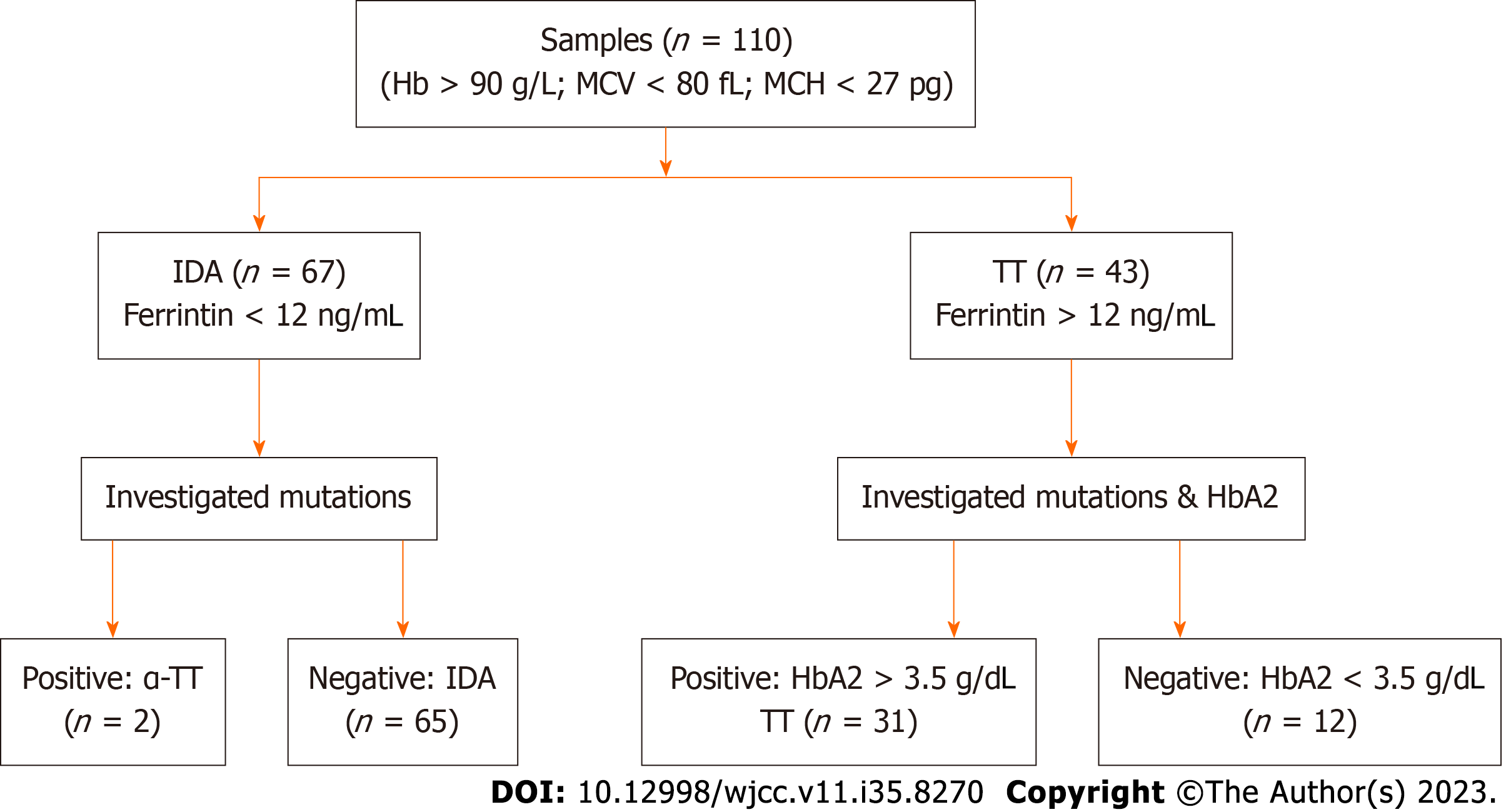
Inclusion and exclusion of the patients for the validation of the new index are shown in Figure 1. The final analysis included 96 patients, consisting of 65 IDA patients and 31 TT patients. The complete blood count results were compared between the IDA patients and the TT patients (Table 1). Compared to the IDA patients, the TT patients had significantly higher levels of RBC, Hb, and hematocrit, and significantly lower levels of MCV and mean corpuscular hemoglobin. No significant difference was noticed in the levels of mean corpuscular hemoglobin concentration, red blood cell distribution width, platelet count, and white blood cells between the TT patients and the IDA patients.
| Variables | Iron deficiency anemia (n = 65) | Thalassemia trait (n = 31) | P value |
| RBC (1012/L) | 4.5 (0.4) | 5.7 (0.6) | < 0.01 |
| Hb (g/L) | 104 (11) | 115 (11) | < 0.01 |
| HCT | 34.2 (3.2) | 37.3 (3.8) | < 0.01 |
| MCV (fl) | 76.2 (4.3) | 65.1 (4.5) | < 0.01 |
| MCH (pg) | 23.4 (1.8) | 20.7 (2.0) | < 0.01 |
| MCHC (g/L) | 305 (11) | 312 (21) | 0.22 |
| RDW (%) | 17.1 (3.8) | 16.6 (1.9) | 0.522 |
| Platelet (109/L) | 298 (72) | 258 (87) | 0.21 |
| WBC (109/L) | 6.03 (2.03) | 7.19 (2.48) | 0.16 |
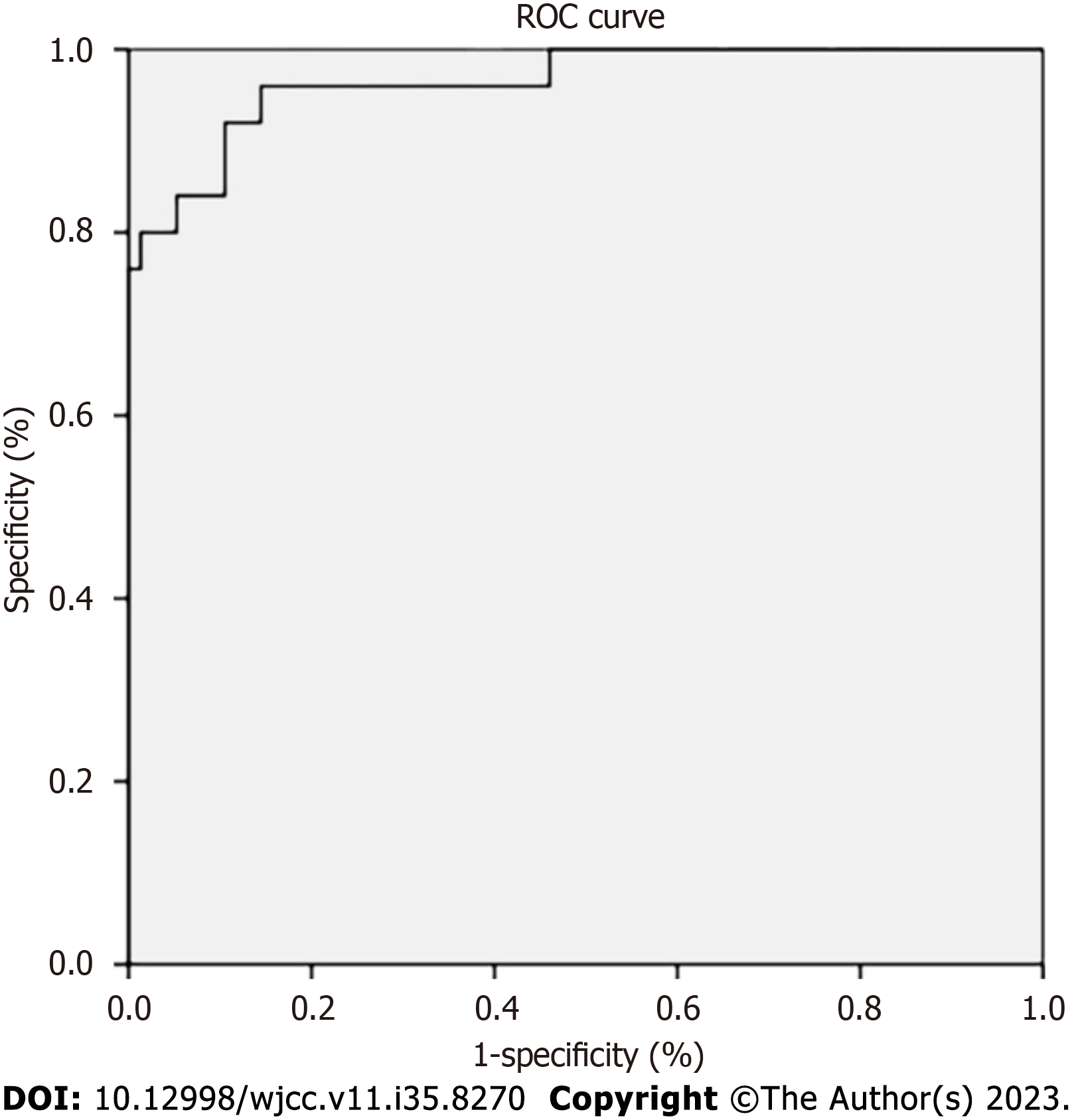
The largest area under the ROC curve for the Hb/MCV indicated that this index had the best performance in discriminating between IDA and TT (Figure 2). Thus, the Hb/MCV ratio was used as the new index formula. The validity of the Hb/MCV index was compared to other gold diagnostic methods, such as molecular techniques for β-TT, HbA2 measurement for α-TT, and ferritin measurement for IDA. As shown by the ROC curve, the cut-off value of the Hb/MCV index is 1.512, with IDA indicated by a value < 1.512 and TT by a value ≥ 1.512.
The new index showed good diagnostic performance in discriminating between IDA and TT against gold standard diagnostic methods, with a sensitivity and a specificity of 93.5% and 78.4%, respectively (Table 2).
| Diagnostic parameters | TT, % (95%CI) | IDA, % (95%CI) |
| Sensitivity | 93.5 (77.2-98.9) | 78.4 (66.2-87.3) |
| Specificity | 78.4 (66.2-87.3) | 93.5 (77.2-98.9) |
| Accuracy | 83.3 (74.5-89.6) | |
| Youden's index | 0.72 | |
| AUC | 0.97 (0.93-1.00) | |
| Kappa coefficient | 0.65 (0.51-0.80) | |
TT is caused by genetic mutations and tends to cluster in small geographical regions[9]. In these areas with a high incidence of TT, clinicians are more likely to order genetic testing for diagnosis. However, in regions with complex genetic backgrounds, such as Shanghai, there is a great need of a simple preliminary diagnostic screening index for discriminating between microcytic and hypochromic anemias.
IDA is caused by exhaustion of iron storage or insufficient raw materials for hemoglobin synthesis. Iron is also an essential component for many critical cellular processes[6,10]. TT is an anemia caused by abnormal hemoglobin synthesis induced by genetic mutations. The clinical manifestations of both these diseases present as microcytic and hypochromic anemia.
The Hb/MCV index has a high sensitivity of 93.5% in diagnosing TT. Misdiagnosis of IDA as TT is associated with unnecessary medical burdens on patients. Therefore, early screening for TT is of great importance. The new index requires only two basic results of complete blood count and is very convenient for outpatient settings. An Hb/MCV ratio less than 1.512 indicates low risk of TT, which warrants observation and monitoring of Hb and iron indicators over time. Conversely, if the clinical manifestations also fit, an Hb/MCV ratio ≥ 1.512 indicates relatively high risk of TT; genetic testing should then be ordered to confirm the diagnosis.
Despite the convenience and good diagnostic performance of the Hb/MCV index, it is only a screening tool for discriminating between IDA and TT and is not intended to replace the gold standard diagnostic tests for these two anemias.
The Hb/MCV index has good diagnostic performance in discriminating between IDA and TT in patients with high hemoglobin concentration (Hb > 90 g/L). This new index requires only two basic results of complete blood count, which can be a desirable feature in areas with insufficient medical resources.
Iron deficiency anemia (IDA) and thalassemia trait (TT) are common causes of microcytic anemia that are challenging to differentiate, especially in resource-limited settings. A simple screening index using basic complete blood count parameters could facilitate diagnosis.
To develop and validate a new index for discriminating between IDA and TT which only requires two routine complete blood count results.
To determine the optimal formula for a new screening index to differentiate between IDA and TT and validate its performance against gold standard tests.
Retrospective analysis of complete blood counts from 126 patients to develop the index formula based on receiver operating characteristic curves. Prospective validation in 61 additional patients using sensitivity, specificity, and other metrics.
The hemoglobin to mean corpuscular volume ratio (Hb/MCV) showed the best discrimination. An index cut-off of 1.512 differentiated IDA from TT with 93.5% sensitivity and 78.4% specificity.
The Hb/MCV index successfully differentiated between IDA and TT. As it only requires hemoglobin and MCV, which is convenient for use in resource-limited settings.
The Hb/MCV index could facilitate screening and early diagnosis of TT in areas without access to genetic testing. Future studies should evaluate it prospectively across diverse populations.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Hematology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gheith OA, Egypt S-Editor: Liu JH L-Editor: A P-Editor: Xu ZH
| 1. | Pasricha SR. Anemia: a comprehensive global estimate. Blood. 2014;123:611-612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Kassebaum NJ, Jasrasaria R, Naghavi M, Wulf SK, Johns N, Lozano R, Regan M, Weatherall D, Chou DP, Eisele TP, Flaxman SR, Pullan RL, Brooker SJ, Murray CJ. A systematic analysis of global anemia burden from 1990 to 2010. Blood. 2014;123:615-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1183] [Cited by in RCA: 1254] [Article Influence: 114.0] [Reference Citation Analysis (0)] |
| 3. | Hoffmann JJML, Urrechaga E. Verification of 20 Mathematical Formulas for Discriminating Between Iron Deficiency Anemia and Thalassemia Trait in Microcytic Anemia. Lab Med. 2020;51:628-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 4. | Urrechaga E, Hoffmann JJML. Critical appraisal of discriminant formulas for distinguishing thalassemia from iron deficiency in patients with microcytic anemia. Clin Chem Lab Med. 2017;55:1582-1591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 5. | Sirdah M, Tarazi I, Al Najjar E, Al Haddad R. Evaluation of the diagnostic reliability of different RBC indices and formulas in the differentiation of the beta-thalassaemia minor from iron deficiency in Palestinian population. Int J Lab Hematol. 2008;30:324-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 66] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 6. | Janel A, Roszyk L, Rapatel C, Mareynat G, Berger MG, Serre-Sapin AF. Proposal of a score combining red blood cell indices for early differentiation of beta-thalassemia minor from iron deficiency anemia. Hematology. 2011;16:123-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Matos JF, Dusse LM, Borges KB, de Castro RL, Coura-Vital W, Carvalho Md. A new index to discriminate between iron deficiency anemia and thalassemia trait. Rev Bras Hematol Hemoter. 2016;38:214-219. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 8. | Cao A, Galanello R. Beta-thalassemia. Genet Med. 2010;12:61-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 447] [Cited by in RCA: 506] [Article Influence: 33.7] [Reference Citation Analysis (0)] |
| 9. | Wu H, Huang Q, Yu Z, Zhong Z. Molecular analysis of alpha- and beta-thalassemia in Meizhou region and comparison of gene mutation spectrum with different regions of southern China. J Clin Lab Anal. 2021;35:e24105. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Shen C, Jiang YM, Shi H, Liu JH, Zhou WJ, Dai QK, Yang H. Evaluation of indices in differentiation between iron deficiency anemia and beta-thalassemia trait for Chinese children. J Pediatr Hematol Oncol. 2010;32:e218-e222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 2.1] [Reference Citation Analysis (0)] |