Published online Sep 16, 2023. doi: 10.12998/wjcc.v11.i26.6122
Peer-review started: May 13, 2023
First decision: August 2, 2023
Revised: August 7, 2023
Accepted: August 11, 2023
Article in press: August 11, 2023
Published online: September 16, 2023
Processing time: 118 Days and 4.4 Hours
At present, the incidence rate of ischemic stroke in young people is increasing yearly, and the age of onset is increasingly young. Therefore, primary and secondary prevention of ischemic stroke in young people, especially secondary prevention, is particularly crucial.
We aimed to comprehensively evaluate risk factors for stroke recurrence in first-ever young ischemic stroke (YIS) patients.
The meta-analysis was used to quantitatively analyze the research results on risk factors for stroke recurrence in first-ever YIS patients both domestically and internationally. Stata12.0 software was used for heterogeneity testing, publication bias analysis, sensitivity analysis, and the calculation of combined odds ratios and 95% confidence intervals.
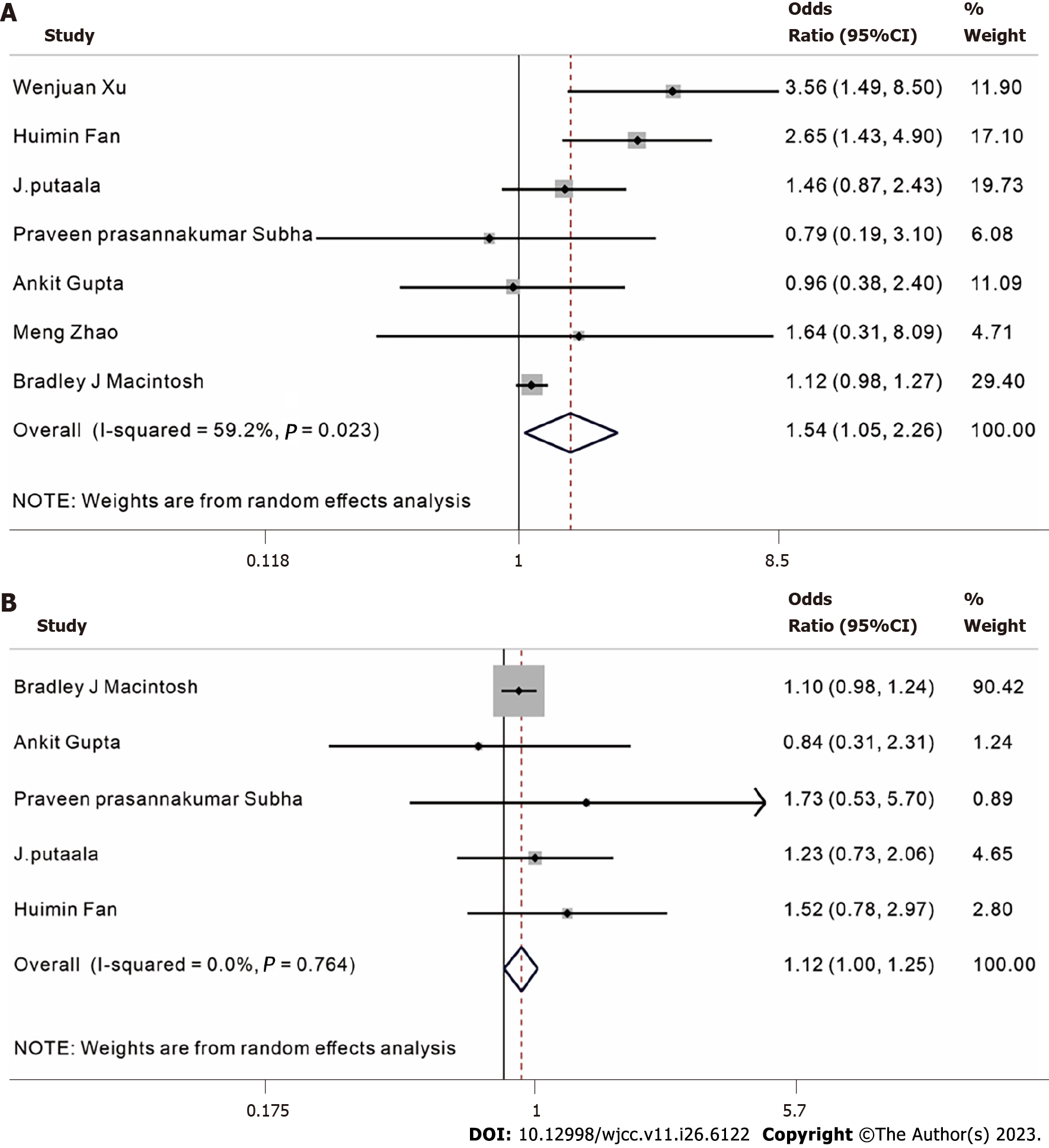
The odds ratio (OR) values of the relationship between hypertension and hyperlipidemia and recurrence of first-ever YIS were 1.54 (1.05-2.26) and 1.12 (1.00-1.25), respectively. The OR values of male sex, type 2 diabetes, smoking, drinking and YIS recurrence were 1.66 (0.98-2.79), 1.01 (0.64-1.59), 1.21 (0.83-1.76), and 1.28 (0.82-2.53), respectively. The relationship between male sex, type 2 diabetes, smoking, drinking and YIS recurrence was ambiguous.
Hypertension and hyperlipidemia are important risk factors for stroke recurrence in first-ever YIS patients, and active intervention should be taken.
Core Tip: This article mainly uses the meta-analysis technology to retrieve stroke risk factors. The meta-analysis is used to quantitatively analyze the research results on risk factors for stroke recurrence in first-ever young ischemic stroke (YIS) patients both domestically and internationally. Finally, we find that hypertension and hyperlipidemia are important risk factors for stroke recurrence in first-ever YIS patients, and active intervention should be taken, in order to realize the precise target intervention of young people with ischemic stroke and reduce the disability rate and mortality rate.
- Citation: Xia Y, Liu H, Zhu R. Risk factors for stroke recurrence in young patients with first-ever ischemic stroke: A meta-analysis. World J Clin Cases 2023; 11(26): 6122-6131
- URL: https://www.wjgnet.com/2307-8960/full/v11/i26/6122.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i26.6122
Worldwide, stroke is the main cause of death and disability and is characterized by high disability rates, high mortality rates, and high recurrence rates[1]. With the rapid development of the economy and society, the incidence rate of ischemic stroke in young people is gradually increasing, and the age of onset is gradually becoming younger. Compared with ischemic stroke in elderly individuals, the etiology of ischemic stroke in young people is more diversified, which leads to certain difficulties in diagnosis.
Research has shown that there are approximately 2 million new youth strokes worldwide each year, with ischemic stroke being the main cause and a high recurrence rate of stroke[2]. However, its treatment methods and effects are still limited. Young people are the backbone of families, society, and even the country. Once they are disabled or even killed, significant damage to society and families occurs. This study used the meta-analysis method in evidence-based medicine to systematically evaluate the research results of risk factors for stroke recurrence in first-ever young ischemic stroke (YIS) patients, explore risk factors for stroke recurrence in first-ever YIS patients, and provide a theoretical basis for formulating preventive measures for YIS patients.
Inclusion criteria were as follows: (1) The study subjects were YIS patients and met the diagnostic criteria for acute ischemic stroke, as well as the age limit for young stroke (18-50 years of age)[3,4]; (2) the research objective was to explore the risk factors for recurrent stroke after the onset of the first stroke; (3) the experimental design was a case control study or a current or retrospective study that was divided into a case group and a control group, and exposure factors were compared between the two groups; (4) the length of time the research had been conducted or the date that the study occurred had been publicly published; (5) there were clear regulations for sample sizes; and (6) the original data provided odds ratio (OR) values and 95% confidence intervals (95%CIs), or the corresponding data formulas could be used to calculate OR values and 95%CIs.
Exclusion criteria were as follows: Lichtenstein's[5] standards and custom standards were used to evaluate the quality of literature and eliminate literature with poor quality, duplicate reports, incomplete data, and incorrect calculations.
Internationally recognized system evaluation retrieval strategies were adopted. The search databases included the China National Knowledge Infrastructure Database (2003-2023), the VIP Database (1989-2023), the Wanfang Database (1981-2023), PubMed, and Web of Science. Published literature on the risk factors for stroke recurrence in first-ever YIS were screened and collected. "Young ischemic stroke", "young cerebral infarction", "young brain infarction" or "young ischemic infarction" and "risk factors" were used as search terms; "risk factors" and "young ischemic stroke" or "ischemic stroke of young adults" were used as search terms; and a combination of subject words and keywords was used to search.
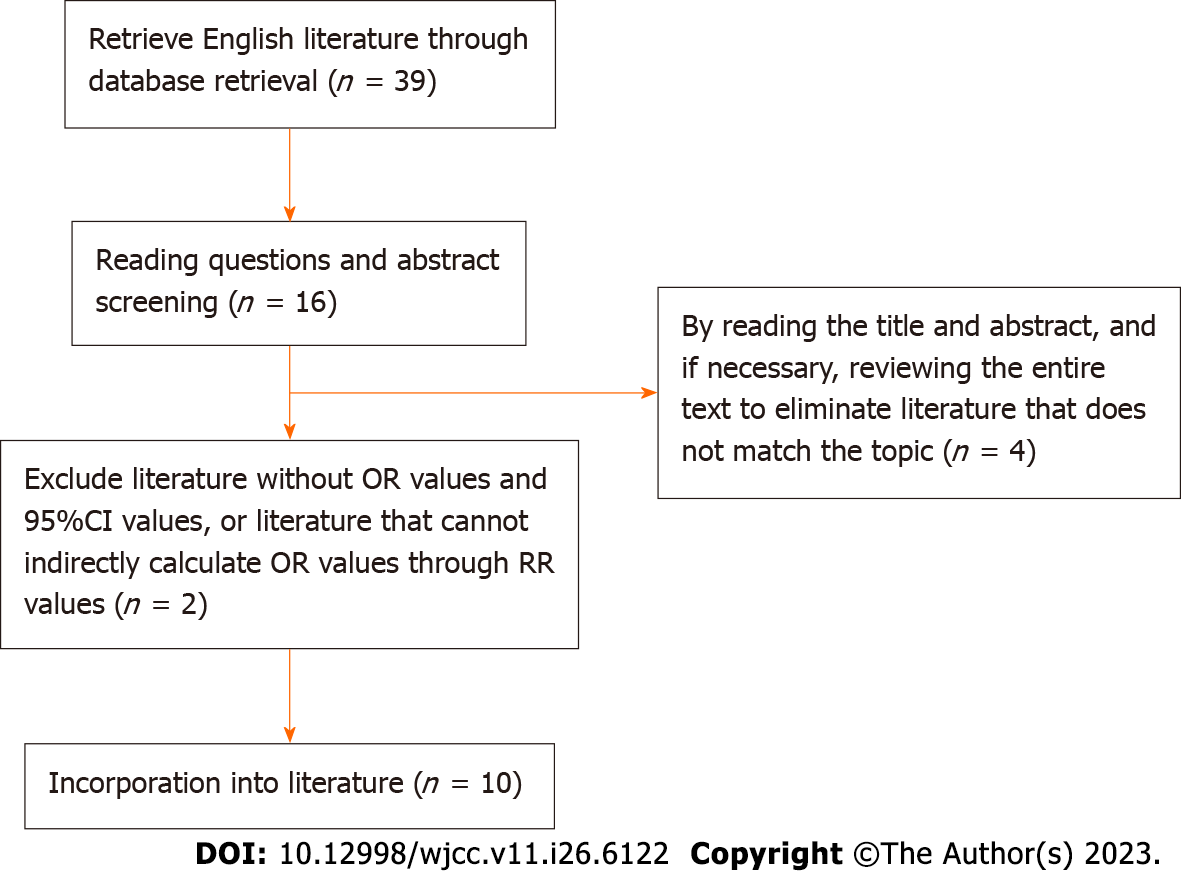
All retrieved literature was checked for duplicates based on the author, year, and title of the literature. One researcher independently selected the literature, extracted the data, and checked each one before another researcher conducted a review. When selecting literature, we first read the title and abstract, and after excluding significantly unrelated literature, we further read the entire text to determine whether it was ultimately included. For literature that met the inclusion criteria, the content of data extraction mainly included author, year, sample size, and journal name.
According to the above retrieval method, a total of 39 English studies were retrieved and screened according to the inclusion and exclusion criteria. Finally, a total of 10 studies were found to be consistent with the research topic of this article. Please refer to the flowchart in Figure 1 for details.
The statistical software Stata 12.0 provided by the International Evidence Based Medicine Collaboration Network was used to conduct heterogeneity testing on the collected data and to calculate the combined OR values and 95%CIs. (1) When heterogeneity test results of P > 0.05 were obtained, a fixed-effects model was used for meta-analysis; when heterogeneity test results of P ≤ 0.05 were obtained, a random-effects model was used; (2) The merged OR value and 95%CI and whether there was statistical significance were determined based on whether the OR value was within the 95%CI; and (3) When the number of included studies was ≥ 6, a funnel plot analysis was used to determine whether there was publication bias.
According to the above retrieval strategy, a total of 39 English studies were retrieved and screened according to the inclusion and exclusion criteria. Finally, a total of 10 studies were included in this study, with a total of 3291 cases and 8270 controls. The basic information of the included literature is detailed in Table 1.
| Number | Ref. | Number of cases | Number of controls | Publication of journals |
| 1 | Yang et al[11], 2016 | 64 | 171 | Neuroscience |
| 2 | Xu et al[12], 2021 | 110 | 139 | BMC Neurology |
| 3 | Fan et al[13], 2018 | 74 | 358 | Medicine |
| 4 | Putaala et al[14], 2009 | 86 | 550 | Neurology |
| 5 | Song et al[15], 2017 | 293 | 64 | International Journal of Neuroscience |
| 6 | Subha et al[16], 2015 | 15 | 85 | Ann Indian Acad Neurol |
| 7 | Gupta et al[17], 2022 | 63 | 63 | Annals of indian Academy |
| 8 | Vibo et al[18], 2021 | 273 | 164 | European Stroke |
| 9 | Zhao et al[19], 2017 | 121 | 575 | World Neurosurgery |
| 10 | MacIntosh et al[6], 2021 | 2192 | 6101 | Journal of the American Heart Association |
Researchers used the NOS to evaluate the quality of the literature. If there were any differences, they could resolve them through consultation or consultation with third parties. NOS includes 4 items for "research object selection" (4 points), 1 item for "inter group comparability" (2 points), and 3 items for "outcome measurement" (3 points), with a maximum score of 9 points. A score of ≥ 6 points was considered high-quality literature, and a score of < 6 points was considered low-quality literature (Table 2).
According to the research contents included in the literature and the number of references for each risk factor, this study selected six risk factors for systematic evaluation: male sex, hypertension, hyperlipidemia, type 2 diabetes, smoking, and drinking.
Heterogeneity test: A heterogeneity test was carried out on the references of various risk factors. The literature on the relationship between hyperlipidemia, type 2 diabetes, drinking and the incidence of YIS had good consistency (P > 0.05); therefore, the fixed-effects model was used. There was heterogeneity (P < 0.05) in the literature on the relationship between male sex, hypertension, smoking, and the onset of YIS; therefore, a random-effects model was used.
Meta-analysis results: The results showed that the combined OR values of hypertension and hyperlipidemia were both greater than 1 and statistically significant. Therefore, it was a risk factor for stroke recurrence in first-ever YIS patients (Figure 2). The combined OR values of male sex, type 2 diabetes, smoking and drinking were 1.66, 1.01, 1.21 and 1.28, respectively, but the 95%CI included "1", so this study cannot consider male sex, type 2 diabetes, smoking and drinking as risk factors for stroke recurrence in patients with first-ever YIS (Table 3).
| Risk factor | Number of merged literature | Case group | Control group | I2, % | P value | Metaanalysis model | Merge OR values | 95%CI |
| Male | 5 | 2678 | 7049 | 80.80 | < 0.001 | Random effect model | 1.66 | (0.98-2.79) |
| Hypertension | 7 | 2661 | 7871 | 59.20 | 0.023 | Random effect model | 1.54 | (1.05-2.26) |
| Hyperlipidemia | 5 | 2430 | 7157 | 0.00 | 0.764 | Fixed effect model | 1.12 | (1.00-1.25) |
| Type 2 diabetes | 6 | 2551 | 7732 | 42.70 | 0.12 | Fixed effect model | 1.01 | (0.64-1.59) |
| Smoking | 5 | 2430 | 7157 | 71.10 | 0.008 | Random effect model | 1.21 | (0.83-1.76) |
| Drinking | 3 | 152 | 506 | 41.10 | 0.183 | Fixed effect model | 1.28 | (0.82-2.53) |
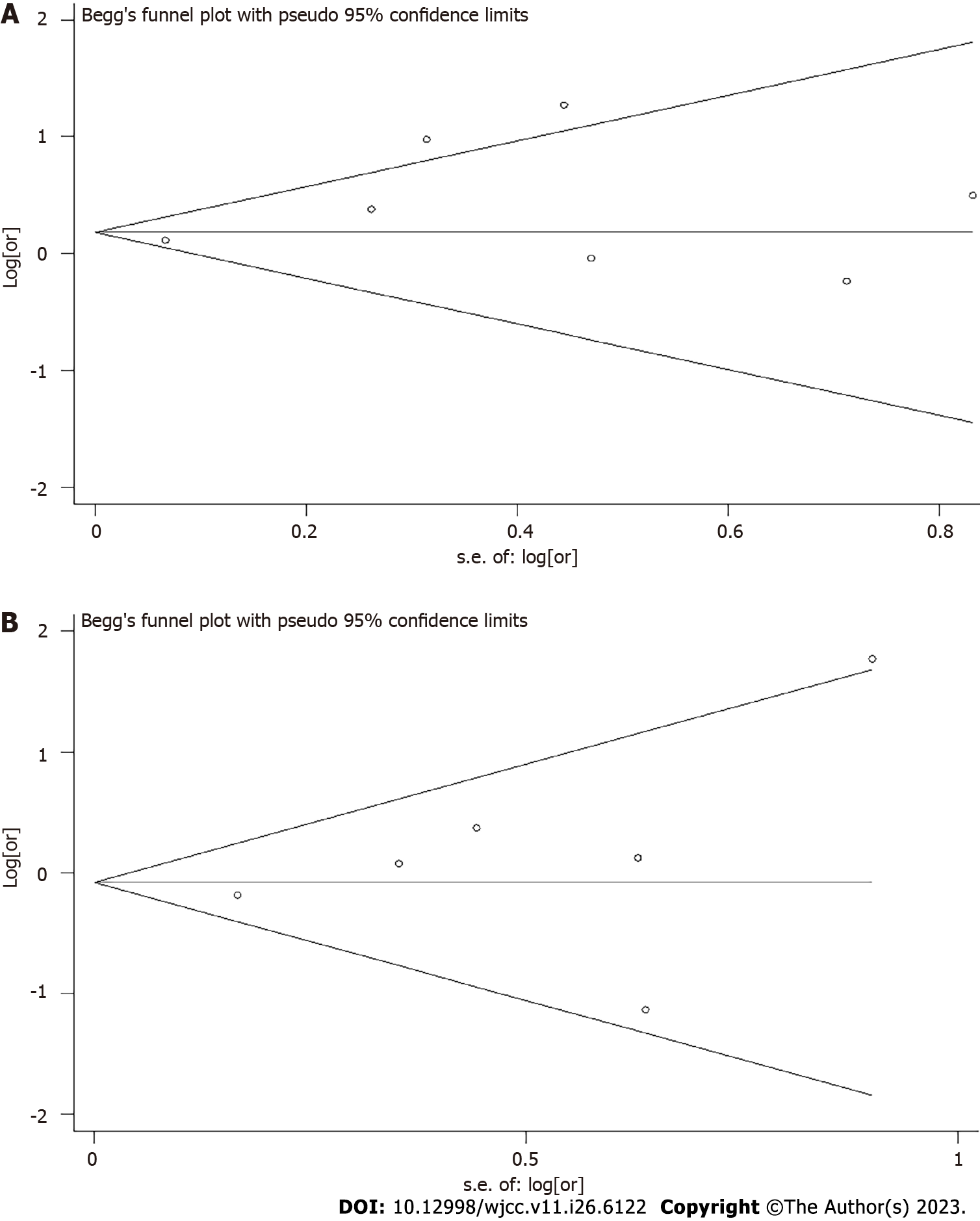
The publication bias analysis of hypertension was conducted using se [log (or)] as the x-axis and log [or] as the y-axis to plot a funnel plot of the relationship between hypertension and first-ever YIS stroke recurrence. The results showed that the funnel plot symmetry of hypertension was poor, indicating the presence of publication bias (Figure 3A).
The published bias analysis of type 2 diabetes used se [log (OR)] of the reference as the abscissa and log [OR] as the ordinate to draw a funnel chart of the relationship between type 2 diabetes and first-ever YIS stroke recurrence. The results showed that the funnel plot symmetry of type 2 diabetes was relatively poor, suggesting that there might be publication bias (Figure 3B).
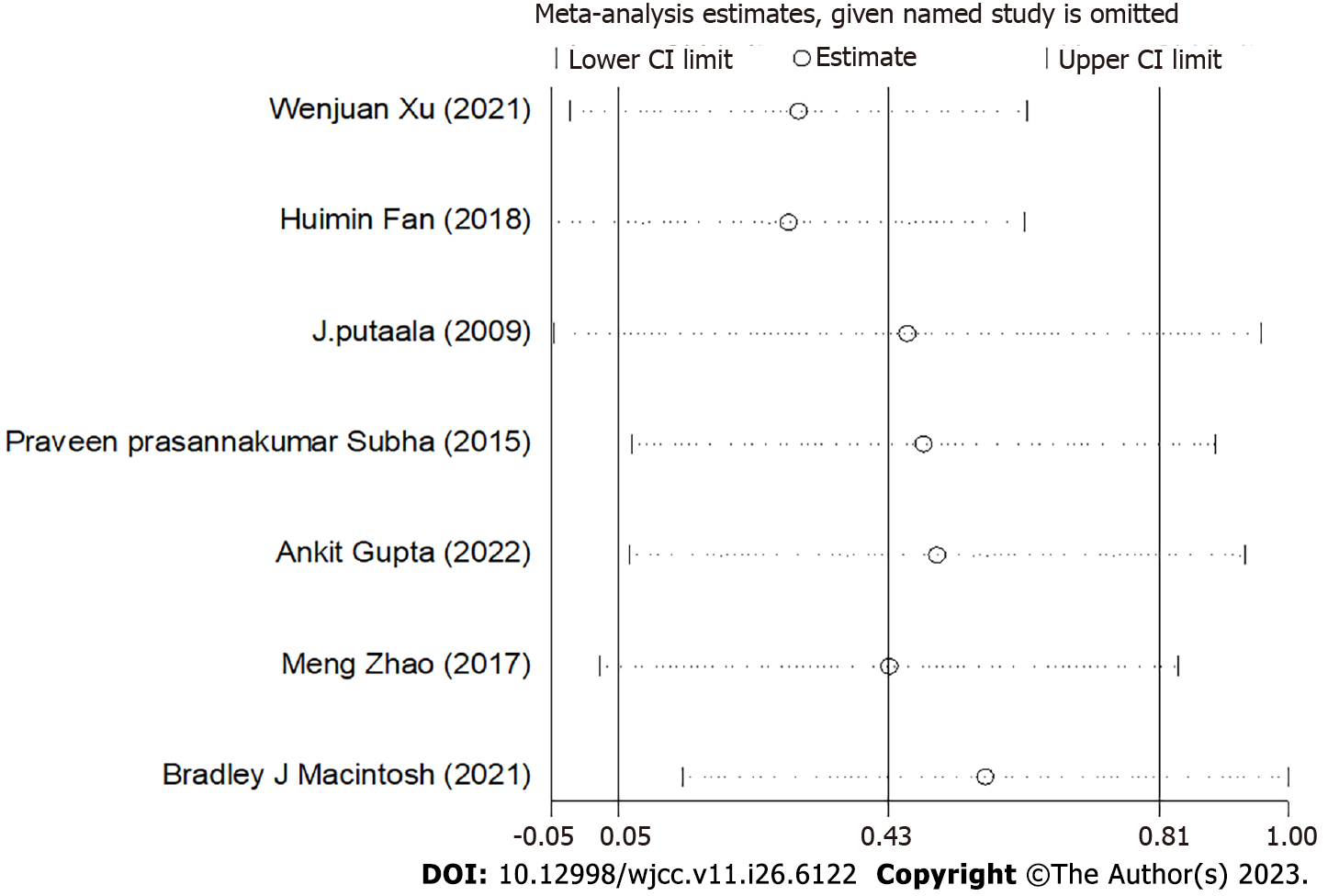
Sensitivity analysis was conducted on hypertension using a one-by-one exclusion method. The sensitivity analysis results suggested excluding any study (except for the research paper published by Bradley Macintosh in 2021), and the combined results of the remaining studies were statistically significant (95%CI value excluding 1), consistent with the original merged results (95%CI value excluding 1), indicating that the research results were relatively stable. The slightly higher heterogeneity of hypertension might be related to the research paper published by MacIntosh et al[6] in 2021, but the overall results were relatively stable and had high credibility (Figure 4).
Ischemic stroke is a disease with a high incidence rate, high recurrence rate and high disability rate, affecting approximately 12 million patients worldwide every year, of which approximately 10% occur in individuals under 50 years old[7,8]. At present, the definition of youth stroke is not yet unified, and different studies have different definitions of its age limit. We defined young ischemic stroke based on the age range used in multiple large-scale studies, which was 18-50 years old[8-10]. Compared with elderly ischemic stroke, there were certain differences in the risk factors and etiology of the first onset and recurrence of YIS, and different studies had similar or conflicting views[11-19]. Therefore, this article adopted the method of meta-analysis to eliminate false information while retaining true information and to eliminate relatively unreliable research conclusions, and we strived to identify high-risk key factors that led to recurrent stroke in YIS patients after their first onset to minimize the disability or even mortality rate of YIS patients as much as possible.
This study showed that the combined OR values of hypertension and hyperlipidemia were both greater than 1, and that result was statistically significant. Therefore, it was a risk factor for stroke recurrence in first-ever YIS patients (Figure 2). The combined OR values of male sex, type 2 diabetes, smoking and drinking were 1.66, 1.01, 1.21 and 1.28, respectively, but the 95%CI included "1", so this study cannot consider male sex, type 2 diabetes, smoking and drinking as risk factors for stroke recurrence in patients with first-ever YIS (Table 3). Research has shown that hypertension changes the cerebrovascular system through the deposition of fibrin in blood vessels and the hypertrophy of smooth muscles, thus causing atherosclerosis and ultimately leading to stenosis or occlusion of blood vessels in the affected area and secondary cerebral ischemia[20]. Many scholars believe that hypertension destroys the integrity of the blood-brain barrier and increases the vascular permeability of the brain, which is the precursor of serious cerebrovascular damage and one of the primary causes of stroke[21-25]. This study found that hypertension was an independent risk factor for stroke recurrence in first-ever YIS patients. Therefore, YIS patients must reduce their blood pressure in a timely manner, but excessive blood pressure reduction should be avoided, as that could lead to hypoperfusion injury. Grade-3 hypertension blood pressure management concepts could be followed (gentle, morning rise, long-term compliance), and more attention should be given to the systolic blood pressure of first-ever YIS patients. Several studies[26-29] showed that platelet activation was closely related to the degree of atherosclerosis. Atherosclerosis is mainly caused by dyslipidemia. Plasma lipids existed in the form of lipoproteins. Plasma endogenous triglycerides were bound to low-density lipoprotein (LDL) and very low density lipoproteins (VLDL) and transported. The increase in endogenous triglycerides in plasma was essentially an increase in LDL and VLDL. Cells absorb more cholesterol from LDL and VLDL particles, leading to an increase in cholesterol and phospholipid content in patients' platelets and enhanced platelet activity. Therefore, it could be considered that the effect of endogenous triglycerides on platelet aggregation function was essentially the effect of elevated LDL and VLDL on platelet aggregation function.
Some scholars have reported that compared with women, men might have more bad habits (such as smoking, excessive drinking, staying up late, heavy physical labor, etc.) due to high social pressure, which may be related to the formation of carotid atherosclerotic plaques, but male sex might not have a fundamental impact or role in the recurrence of ischemic stroke[30,31]. This study also concluded that there was no clear correlation between male sex and recurrent cerebral infarction after the first ischemic stroke in young people. It is well known that chronic hyperglycemia leads to endothelial dysfunction, inflammation and accelerated atherosclerosis processes, resulting in macrovascular complications due to the effects of increased oxidant production, lipoprotein enrichment and the formation of advanced glycation end products. Long-term hyperglycemia could also damage vascular endothelial cells, increase the adhesion of blood-forming components, and lead to circulatory dysfunction leading to ischemia[32-34]. However, this article did not find that type 2 diabetes was a risk factor for the recurrence of ischemic stroke in young people who had ischemic stroke for the first time. According to our speculation, the reason may be that the recurrence of ischemic stroke may mainly depend on the blood sugar control level of type-2 diabetes patients (the blood sugar control level can be monitored by glycosylated hemoglobin and other indicators). If the blood sugar of patients is well controlled, it may not quickly lead to the serious damage to endothelial cells that could cause severe atherosclerotic plaque formation. In addition, this article did not find a fundamental impact of smoking and alcohol consumption on first-ever ischemic stroke in young people, which may be due to bias in the records of previous medical history by relevant scholars (such as whether they quit smoking, specific daily smoking counts and durations, whether they quit drinking, specific daily alcohol consumption and durations, etc.). In the end, when comparing and analyzing the results, due to insufficient data, recording accuracy and incomplete typing, there would be bias in the classification and statistical results. This may also be due to the limited impact of smoking and alcohol consumption on endothelial cell damage, which would not directly lead to the recurrence of ischemic stroke.
In conclusion, among the six risk factors screened above, hypertension and hyperlipidemia were important risk factors for stroke recurrence in patients with first-ever YIS. Although male sex, type 2 diabetes, smoking, and alcohol consumption may damage vascular endothelial cells, their role in the recurrence of ischemic stroke may be limited. Therefore, we must attach great importance to the blood pressure levels of young first-ever ischemic stroke patients, especially the control of ambulatory blood pressure levels. In addition, hyperlipidemia was also a key risk factor for stroke recurrence, and it was necessary to actively monitor blood lipid levels and control them within a reasonable range. Finally, it is hoped that more large-scale, prospective, and high-quality clinical studies will be conducted in the future to observe the relevant risk factors for first-ever ischemic stroke in young people while striving to minimize the disability and even mortality rates of patients, thereby improving the quality of life and health level of young people.
This meta-analysis revealed that hypertension and hyperlipidemia were important risk factors for stroke recurrence in first-ever YIS patients, and active intervention should be taken.
At present, the incidence rate of ischemic stroke in young people is increasing yearly, and the age of onset is increasingly young. Therefore, primary and secondary prevention of ischemic stroke in young people, especially secondary prevention, is particularly crucial.
We aimed to comprehensively evaluate risk factors for stroke recurrence in first-ever young ischemic stroke (YIS) patients.
We aimed to comprehensively evaluate risk factors for stroke recurrence in first-ever young ischemic stroke (YIS) patients.
The meta-analysis was used to quantitatively analyze the research results on risk factors for stroke recurrence in first-ever YIS patients both domestically and internationally. Stata12.0 software was used for heterogeneity testing, publication bias analysis, sensitivity analysis, and the calculation of combined odds ratios and 95% confidence intervals.
The OR values of the relationship between hypertension and hyperlipidemia and recurrence of first-ever YIS were 1.54 (1.05-2.26) and 1.12 (1.00-1.25), respectively. The OR values of male sex, type 2 diabetes, smoking, drinking and YIS recurrence were 1.66 (0.98-2.79), 1.01 (0.64-1.59), 1.21 (0.83-1.76), and 1.28 (0.82-2.53), respectively. The relationship between male sex, type 2 diabetes, smoking, drinking and YIS recurrence was ambiguous.
Hypertension and hyperlipidemia are important risk factors for stroke recurrence in first-ever YIS patients, and active intervention should be taken.
This paper investigates the independent recurrence risk factors of first-ever young ischemic stroke patients and assesses the importance and criticality of traditional risk factors.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Clinical neurology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Ait Addi R, Morocco; Park Y, South Korea S-Editor: Liu JH L-Editor: A P-Editor: Yu HG
| 1. | Kim JT, Lee JS, Kim BJ, Kang J, Lee KJ, Park JM, Kang K, Lee SJ, Kim JG, Cha JK, Kim DH, Park TH, Lee KB, Lee J, Hong KS, Cho YJ, Park HK, Lee BC, Yu KH, Oh MS, Kim DE, Choi JC, Kwon JH, Kim WJ, Shin DI, Yum KS, Sohn SI, Hong JH, Lee SH, Park MS, Choi KH, Ryu WS, Saver JL, Bae HJ. Admission hyperglycemia, stroke subtypes, outcomes in acute ischemic stroke. Diabetes Res Clin Pract. 2023;196:110257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 2. | Campbell BCV, De Silva DA, Macleod MR, Coutts SB, Schwamm LH, Davis SM, Donnan GA. Ischaemic stroke. Nat Rev Dis Primers. 2019;5:70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 510] [Cited by in RCA: 1062] [Article Influence: 177.0] [Reference Citation Analysis (0)] |
| 3. | Wang G, Fang B, Yu X, Li Z. [Interpretation of 2018 guidelines for the early management of patients with acute ischemic stroke]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2018;30:289-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 4. | Putaala J, Metso AJ, Metso TM, Konkola N, Kraemer Y, Haapaniemi E, Kaste M, Tatlisumak T. Analysis of 1008 consecutive patients aged 15 to 49 with first-ever ischemic stroke: the Helsinki young stroke registry. Stroke. 2009;40:1195-1203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 460] [Cited by in RCA: 550] [Article Influence: 34.4] [Reference Citation Analysis (0)] |
| 5. | Lichtenstein MJ, Mulrow CD, Elwood PC. Guidelines for reading case-control studies. J Chronic Dis. 1987;40:893-903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 69] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | MacIntosh BJ, Cohen E, Colby-Milley J, Fang J, Zhou L, Ouk M, Wu CY, Shah BR, Lanctôt K, Herrmann N, Linkewich E, Law M, Black SE, Swartz RH, Kapral MK, Edwards JD, Swardfager W. Diabetes Mellitus Is Associated With Poor In-Hospital and Long-Term Outcomes in Young and Midlife Stroke Survivors. J Am Heart Assoc. 2021;10:e019991. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (1)] |
| 7. | Peng SH, Lai YJ, Lai WJ, Li AH, Yen HH, Huang LW, Tang CW. Impact of smoking on one year functional outcomes after thrombectomy for young stroke patients. J Neurointerv Surg. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Wu YY, Chen PY, Wu CC, Chen HJ, Liang CL, Lee YC, Lin CW, Hung CM, Lin IF, Wang HK. Long-term mortality rates of young stroke in Taiwan: A decade-long epidemiology population-based study. Eur Stroke J. 2022;7:447-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Zhang GB, Huang HW, Guo W. [Prevention and treatment of stroke in Chinese and African young adults]. Zhonghua Yu Fang Yi Xue Za Zhi. 2022;56:1142-1149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 10. | Weller JM, Dorn F, Meissner JN, Stösser S, Beckonert NM, Nordsiek J, Kindler C, Deb-Chatterji M, Petzold GC, Bode FJ; GSR-ET investigators. Endovascular thrombectomy in young patients with stroke. Int J Stroke. 2023;18:453-461. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 11. | Yang J, Shen Z, Wen H, Zhou H, Li C. The effect of vertebral artery hypoplasia in posterior circulation infarction in young patients. Int J Neurosci. 2016;126:1092-1096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Xu W, Zhang X, Chen H, Zhao Z, Zhu M. Prevalence and outcome of young stroke patients with middle cerebral artery stenosis. BMC Neurol. 2021;21:99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Fan H, Hao X, Yang S, Li Y, Qin W, Yang L, Yuan J, Hu W. Study on the incidence and risk factor of silent cerebrovascular disease in young adults with first-ever stroke. Medicine (Baltimore). 2018;97:e13311. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 14. | Putaala J, Kurkinen M, Tarvos V, Salonen O, Kaste M, Tatlisumak T. Silent brain infarcts and leukoaraiosis in young adults with first-ever ischemic stroke. Neurology. 2009;72:1823-1829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 53] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 15. | Song X, Xue S, Zhao J, Wu J. Screening for Fabry's disease in young patients with ischemic stroke in a Chinese population. Int J Neurosci. 2017;127:350-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Subha PP, Pillai Geethakumari SM, Athira M, Nujum ZT. Pattern and risk factors of stroke in the young among stroke patients admitted in medical college hospital, Thiruvananthapuram. Ann Indian Acad Neurol. 2015;18:20-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Gupta A, Saluja A, Saraswathy KN, Imnameren L, Yadav S, Dhamija RK. PON1 (Paraoxonase 1) Q192R Gene Polymorphism in Ischemic Stroke among North Indian Population. Ann Indian Acad Neurol. 2022;25:100-105. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Vibo R, Schneider S, Kõrv L, Mallene S, Torop LA, Kõrv J. Estonian young stroke registry: High burden of risk factors and high prevalence of cardiomebolic and large-artery stroke. Eur Stroke J. 2021;6:262-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | Zhao M, Deng X, Gao F, Zhang D, Wang S, Zhang Y, Wang R, Zhao J. Ischemic Stroke in Young Adults with Moyamoya Disease: Prognostic Factors for Stroke Recurrence and Functional Outcome after Revascularization. World Neurosurg. 2017;103:161-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 20. | Caplan LR. Lacunar infarction and small vessel disease: pathology and pathophysiology. J Stroke. 2015;17:2-6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 118] [Cited by in RCA: 163] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 21. | Li L, Scott CA, Rothwell PM. Association of Younger vs Older Ages With Changes in Incidence of Stroke and Other Vascular Events, 2002-2018. JAMA. 2022;328:563-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 54] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 22. | Huang H, Wu B, Liu L, Tang X, Yi Z, Zeng L, Jing K, Pan C. Variability of blood pressure response to orthostatism and reproducibility of orthostatic hypotension in hospitalized patients with acute ischemic stroke. Blood Press Monit. 2023;28:47-51. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 23. | Oyake K, Tateishi T, Murayama J, Shijima N, Sekizuka T, Otaka Y, Momose K. Blood pressure reduction cut-points for orthostatic hypotension in stroke survivors using a sit-up test: a multicentre cross-sectional study. J Hypertens. 2023;41:83-89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Collette SL, Uyttenboogaart M, Samuels N, van der Schaaf IC, van der Worp HB, Luijckx GJR, Venema AM, Sahinovic MM, Dierckx RAJO, Lingsma HF, Kappen TH, Bokkers RPH; MR CLEAN Registry Investigators. Hypotension during endovascular treatment under general anesthesia for acute ischemic stroke. PLoS One. 2021;16:e0249093. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 25. | Mehta T, McClure LA, White CL, Taylor A, Benavente OR, Lakshminarayan K. Effect of Postural Hypotension on Recurrent Stroke: Secondary Prevention of Small Subcortical Strokes (SPS3) Study. J Stroke Cerebrovasc Dis. 2019;28:2124-2131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 26. | Wang C, Du Z, Ye N, Shi C, Liu S, Geng D, Sun Y. Hyperlipidemia and hypertension have synergistic interaction on ischemic stroke: insights from a general population survey in China. BMC Cardiovasc Disord. 2022;22:47. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 20] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 27. | Myran L, Nguyen TN. Icosapent Ethyl (Vascepa) for Hyperlipidemia/Hypercholesterolemia to Reduce Risk of Heart Attack and Stroke. Am Fam Physician. 2021;103:117-118. [PubMed] |
| 28. | Wang JS, Dai HH, Yan YB, Gong XH, Li X, Li HS, Wang B. Research of stroke combined hyperlipidemia-induced erectile dysfunction in rat model. Aging Male. 2019;22:278-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 29. | Xu Z, Tong S, Pan H, Cheng J. Associations of extreme temperatures with hospitalizations and post-discharge deaths for stroke: What is the role of pre-existing hyperlipidemia? Environ Res. 2021;193:110391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 30. | Ahmed R, Mhina C, Philip K, Patel SD, Aneni E, Osondu C, Lamikanra O, Akano EO, Anikpezie N, Albright KC, Latorre JG, Chaturvedi S, Otite FO. Age- and Sex-Specific Trends in Medical Complications After Acute Ischemic Stroke in the United States. Neurology. 2023;100:e1282-e1295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 20] [Reference Citation Analysis (0)] |
| 31. | Edrissi C, Rathfoot C, Knisely K, Sanders CB, Goodwin R, Nathaniel SI, Nathaniel T. Age Stratification in Acute Ischemic Stroke Patients with Heart Failure. J Clin Med. 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 32. | Getu RA, Aga F, Badada T, Workie SG, Belew MA, MekonnenRN K. Knowledge of stroke risk factors and warning symptoms among adults with type 2 diabetes in Addis Ababa, Ethiopia, 2021: an institution-Based cross-sectional study. BMC Cardiovasc Disord. 2023;23:21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 33. | Bill O, Mazya MV, Michel P, Prazeres Moreira T, Lambrou D, Meyer IA, Hirt L. Intima-Media Thickness and Pulsatility Index of Common Carotid Arteries in Acute Ischaemic Stroke Patients with Diabetes Mellitus. J Clin Med. 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 34. | Liu D, Yang K, Gu H, Li Z, Wang Y. Predictive effect of triglyceride-glucose index on clinical events in patients with acute ischemic stroke and type 2 diabetes mellitus. Cardiovasc Diabetol. 2022;21:280. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 31] [Reference Citation Analysis (0)] |