Published online Sep 6, 2023. doi: 10.12998/wjcc.v11.i25.5977
Peer-review started: May 23, 2023
First decision: July 17, 2023
Revised: August 1, 2023
Accepted: August 9, 2023
Article in press: August 9, 2023
Published online: September 6, 2023
Processing time: 101 Days and 8.4 Hours
Pyomyositis generally occurs in otherwise healthy young men. Because this condition is unusual among otherwise healthy women in temperate climates, we present the following case.
An otherwise healthy 43-year-old woman presented with bilateral pain in her lower extremities and fever. Magnetic resonance imaging (MRI) findings were indicative of myositis with a possible abscess. We initiated empirical antibiotic therapy with ceftriaxone. However, the swelling and pain in her legs persisted even after 7 d of treatment. Contrast MRI revealed multiple pockets of pus in the vastus lateralis and gluteal muscles. We performed needle aspiration of these abscesses with ultrasound guidance and local anesthesia. Upon culturing, the purulent material was positive for Staphylococcus aureus. We diagnosed her with S. aureus-induced pyomyositis of the vastus lateralis muscle and gluteus region. Based on the antibiotic sensitivity report, ceftriaxone was administered for an additional 7 d. By day 15 post-drainage, the patient was able to start walking. Oral antibiotic therapy was continued for 1 wk following her discharge from hospital, after which her symptoms resolved completely.
Pyomyositis may present with muscle pain, swelling, and fever. Ultrasound-guided percutaneous puncture and drainage may enable timely diagnosis and treatment.
Core Tip: Pyomyositis generally occurs in otherwise healthy young men. We report a case where pyomyositis occurred in an otherwise healthy 43-year-old woman in a temperate climate. This case is unusual because, in temperate regions, pyomyositis usually occurs in immunocompromised patients, such as those with diabetes mellitus. Owing to its rarity in temperate climates and its presentation being characterized by non-specific signs and symptoms, its diagnosis and treatment can be delayed, which can lead to septic shock and death. We hope that our report will help raise awareness and guide the future treatment of patients with pyomyositis.
- Citation: Cui M, Zhang G, Zhang N, Han L, Ma ZQ. Bilateral thigh pyomyositis in an otherwise healthy middle-aged woman: A case report. World J Clin Cases 2023; 11(25): 5977-5981
- URL: https://www.wjgnet.com/2307-8960/full/v11/i25/5977.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i25.5977
Pyomyositis is a bacterial infection of skeletal muscle, usually caused by hematogenous dissemination and often accompanied by abscess formation. Tropical myositis, a suppurative disease, mainly affects children aged 2–5 years and adults aged 20–45 years, whereas pyomyositis in temperate climates mainly affects adult men with coexisting conditions. The reported incidence of pyomyositis in temperate climates has been increasing, owing to the increased use of diagnostic imaging. Pyomyositis generally occurs in otherwise healthy young men, manifesting as muscle swelling, marked tenderness, and indurated muscle swelling that progresses to woody induration of the muscle and overlying tissues[1]. Because this condition is unusual among otherwise healthy women in temperate climates, we present the following case.
A 43-year-old woman, 156 cm in height and 69 kg in weight, who was employed as a cashier in a bakery, was admitted to the department of pain medicine for pain in both of her legs.
The pain had persisted for 3 d, with substantial movement restriction. The patient denied any history of trauma or vaccine injection. She had initially undergone an ultrasound examination of her lower limbs, which had ruled out arteriovenous thrombosis. Despite receiving therapy comprising non-steroidal anti-inflammatory drugs and rest, under the assumption that her pain was caused by muscle strain, the pain and swelling increased and the patient developed a fever and chills.
The patient had no history of diabetes.
The patient did not report having experienced any injury or trauma, and had no recent history of infection, foreign travel, or immunosuppression.
We admitted the patient to investigate the etiology of her fever and pain. Upon physical examination her temperature was 39.1°C, pulse rate was 90 beats/min, and blood pressure was 100/65 mmHg. Her visual analog scale score was 8 cm. No wounds or breaks in the skin were noted on her lower extremities. She had tenderness in both her thighs and left knee joint, as well as in her bilateral gluteus media and small gluteus muscles. Both of the patient’s thighs were swollen and had a sensation of warmth, although no erythema, ecchymosis, or fluctuance were noted in these areas. Respiratory, neurological, and cardiovascular examination results were all normal.
A hematological examination conducted upon the patient’s admission to hospital revealed leukocytosis [white blood cell (WBC) = 19.67 × 109/L] and neutrophilia (neutrophils = 17.92 × 109/L; 91.1%). Her hemoglobin concentration was 83 g/L, C-reactive protein (CRP) concentration was 192 mg/L (normal value: < 7 mg/L), erythrocyte sedimentation rate (ESR) was 96 mm/h (normal value: < 20 mm/h), and her creatine kinase concentration was 306 IU/L (normal value = 24–170 IU/L). Routine urine and stool cultures, liver and kidney function, electrolyte levels, and myocardial enzyme profile were all within the normal range. Tests for autoantibodies associated with rheumatic diseases were negative.
Plain radiographs revealed no bony abnormalities of the knee joint. A lower limb venous ultrasonography excluded phlebothrombosis. A computed tomography (CT) scan of the thorax, abdomen, and pelvis revealed no abnormalities. As we suspected that the patient might have pyomyositis, magnetic resonance imaging (MRI) was performed, which revealed widespread infiltrative edema within the vastus lateralis muscle, indicative of myositis with a possible abscess. We observed no signs or symptoms of knee joint effusion, osteomyelitis, or infiltration.
After obtaining blood cultures, we started the patient on empirical antibiotic therapy with ceftriaxone. She remained febrile during her first 3 d of hospitalization, and after 4 d of antibiotic treatment her temperature decreased to normal levels. Blood cultures taken upon presentation revealed no growth after 3 d. Subsequent laboratory tests revealed improvements in leukocyte (11.31 × 109/L) and neutrophil (9.06 × 109/L) concentrations.
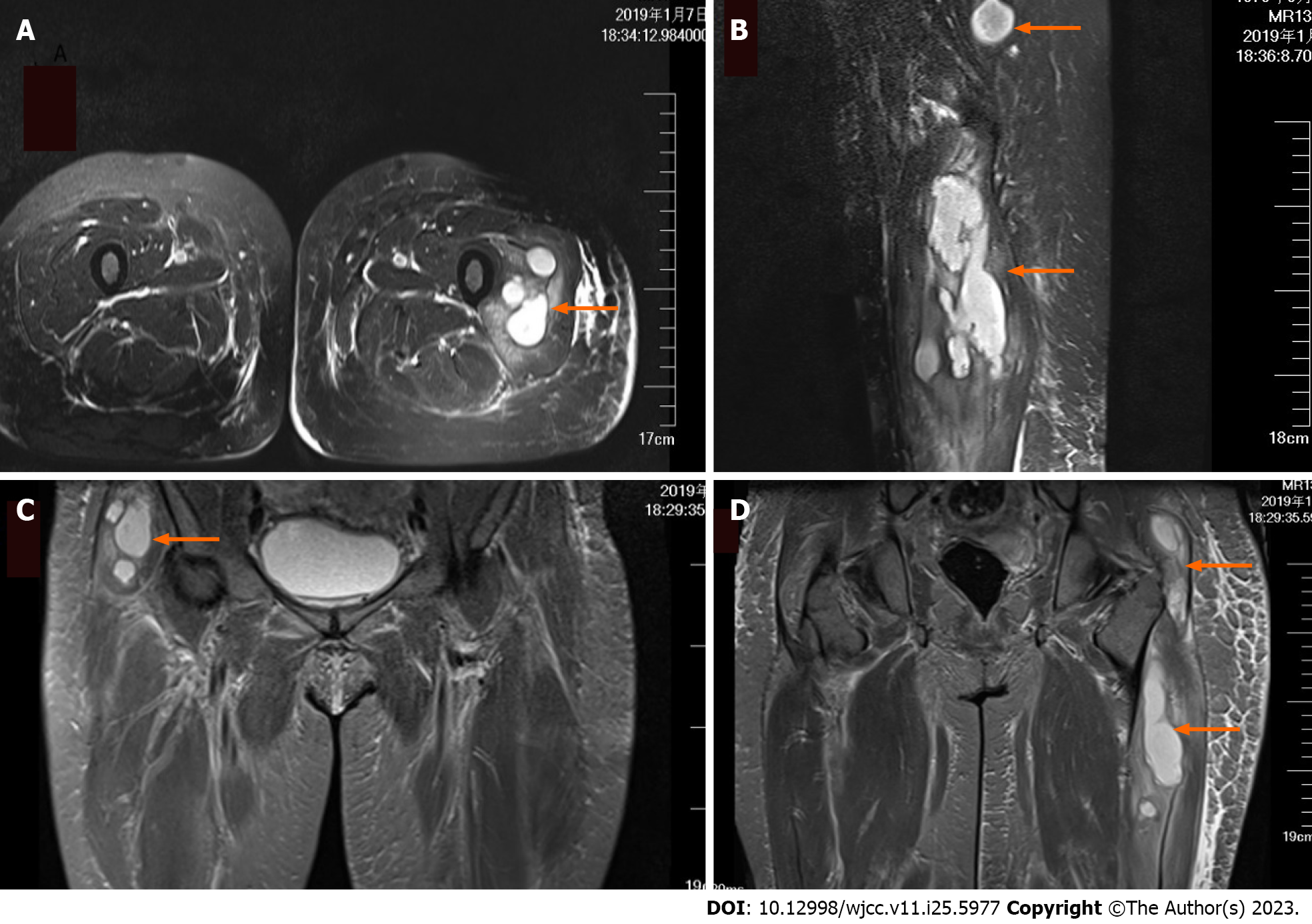
Because we suspected that the patient might have pyomyositis and as 7 d of antibiotic treatment alone did not significantly relieve the swelling or pain in her legs, a repeat MRI of the thighs and hip joint was performed with enhanced contrast. This revealed multiple pockets of pus in the vastus lateralis and gluteal muscles (Figure 1). We performed needle aspiration of these abscesses with ultrasound guidance and local anesthesia, draining about 40 mL (30 mL from the left leg and 10 mL from the right) of purulent material. The purulent content was sent for culturing. The patient’s condition improved after aspiration. Physical examination revealed a reduction in muscle tenderness and localized indurations. A follow-up ultrasound done 3 d after aspiration revealed the accumulation of residual fluid measuring 1.5 cm × 1.2 cm. The patient declined a second round of aspiration. Staphylococcus aureus was observed in the aspiration culture.
In the end, the patient was diagnosed with S. aureus-induced pyomyositis of the vastus lateralis muscle and gluteus region.
Based on the antibiotic sensitivity report, ceftriaxone was administered for an additional 7 d.
By day 15 post drainage, the patient was able to start walking. Laboratory tests revealed a decrease in her WBCs (within the normal range), ESR (59 mm/h), and CRP concentration (6.2 mg/L). Oral antibiotic therapy was continued for 1 wk after the patient was discharged. The total duration of therapy was 3 wk. Subsequent follow-up visits revealed a gradual relief of her symptoms. By her 4-mo follow-up visit, her ESR and CRP concentration had normalized. The patient experienced complete resolution of her symptoms and had no further complaints.
Pyomyositis affects the skeletal muscles, manifesting as high-grade fever with pain in the affected limbs. It is generally considered a tropical infectious disease that affects otherwise healthy children and adults, but it has also been diagnosed with increasing frequency in other parts of the world since the 1970s, with the spread of routine diagnostic imaging tests[2]. The pathogenesis of tropical myositis remains unclear, although it may be related to trauma, parasites, nutritional deficiencies, and viruses.
As this disease is relatively rare in temperate regions and its early presentation is characterized by signs and symptoms that are not very specific, pyomyositis is usually not added to differential diagnoses of muscle pain and swelling until patients fail to respond to treatments of the alternative diagnoses. The case we report here is unusual, as the patient was an otherwise healthy, middle-aged woman with an unremarkable medical history. The muscles involved in pyomyositis are usually deep, so typical inflammatory manifestations may not be visible on the surface. Therefore, pyomyositis should be differentiated from osteomyelitis, malignant tumors, hematoma, septic arthritis, deep vein thrombosis, and thrombotic phlebitis. When pyomyositis is not promptly and properly treated, serious complications such as muscle abscesses, cerebral abscesses, renal failure, septicemia, and death may occur[3,4].
Pyomyositis is characterized by fever, local swelling, and pain. In severe cases, it can lead to shock and death. The large muscle groups of the pelvic girdle and lower extremities are the most common sites of infection. The thigh muscles, particularly the quadriceps (26%), are the most commonly affected muscles, followed by the iliopsoas (14%) and gluteal (10%) muscles[2,5]. The gold standard for the diagnosis of pyomyositis is MRI[6]. In the present case, the patient exhibited swelling and warmth in her thighs, and the final diagnosis was S. aureus-induced pyomyositis, based on the results of an MRI and aspirated fluid cultures. In patients with pyomyositis, blood cultures are usually negative, whereas aspirated fluid cultures are usually positive. In > 85% of cases, S. aureus is the causative organism[3,7].
The principle treatment for suppurative pyomyositis is surgical incision and drainage combined with intravenous antibiotic administration for 2–3 wk. Such drainage can be performed via open surgery, aspiration under ultrasound or CT guidance, or percutaneously. Pyomyositis has been described as having three stages: Invasive, suppurative, and septic, representing a gradual progression from diffuse inflammation to focal abscess formation to a septic state[8]. By the time the disease has progressed for 2–3 wk, suppuration becomes apparent. At that stage, puncture aspiration of the local abscess can be performed. Percutaneous abscess drainage combined with antibiotic therapy is an effective method for the treatment of tropical pyomyositis (also in the suppurative phase). Such drainage can shorten the duration of antibiotic use and hospital stay[9].
The patient in this case was treated with 2 wk of intravenous ceftriaxone, followed by oral antibiotic therapy for 1 wk. As the infection was rather advanced, we performed needle aspiration with ultrasound guidance of the vastus lateralis muscle and gluteus abscess, under local anesthesia. The patient’s condition improved following aspiration. No clear guidelines exist for the duration of such antibiotic treatment, but most experts recommend a combination of intravenous and oral antibiotics for 3-8 wk, regardless of whether the abscess is drained[10]. The duration of therapy for our patient was 3 wk. Surprisingly, pyomyositis rarely requires amputation compared to necrotizing fasciitis and myonecrosis. Even when muscle damage is severe, residual deformities and dysfunction are rarely observed. At the 4-month follow-up visit, our patient exhibited complete resolution of her symptoms and had no further complaints.
A preprint of this report was previously published (Min et al[11], 2022).
The clinical manifestations of pyomyositis, such as muscle pain, swelling, fever, and leukocytosis, can be treated via ultrasound-guided percutaneous puncture and drainage. This can aid its diagnosis, facilitating timely treatment and improving the prognosis. We hope that this report will help guide the future treatment of patients with pyomyositis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Infectious diseases
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Baryshnikova NV, Russia; Ghimire R, Nepal S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Patel SR, Olenginski TP, Perruquet JL, Harrington TM. Pyomyositis: clinical features and predisposing conditions. J Rheumatol. 1997;24:1734-1738. [PubMed] |
| 2. | Hassan FO, Shannak A. Primary pyomyositis of the paraspinal muscles: a case report and literature review. Eur Spine J. 2008;17 Suppl 2:S239-S242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Chauhan S, Jain S, Varma S, Chauhan SS. Tropical pyomyositis (myositis tropicans): current perspective. Postgrad Med J. 2004;80:267-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 148] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 4. | d'Assignies G, Fangio P, De Jonghe B, Lachérade JC, Outin H. [Septic shock due to tropical pyomyositis]. Ann Fr Anesth Reanim. 2003;22:913-914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 5. | Gomez-Reino JJ, Aznar JJ, Pablos JL, Diaz-Gonzalez F, Laffon A. Nontropical pyomyositis in adults. Semin Arthritis Rheum. 1994;23:396-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 70] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Stevens DL, Bisno AL, Chambers HF, Dellinger EP, Goldstein EJ, Gorbach SL, Hirschmann JV, Kaplan SL, Montoya JG, Wade JC; Infectious Diseases Society of America. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014;59:e10-e52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 555] [Cited by in RCA: 962] [Article Influence: 96.2] [Reference Citation Analysis (0)] |
| 7. | Lemonick DM. Non-tropical pyomyositis caused by methicillin-resistant Staphylococcus aureus: an unusual cause of bilateral leg pain. J Emerg Med. 2012;42:e55-e62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Spiegel DA, Meyer JS, Dormans JP, Flynn JM, Drummond DS. Pyomyositis in children and adolescents: report of 12 cases and review of the literature. J Pediatr Orthop. 1999;19:143-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Palacio EP, Rizzi NG, Reinas GS, Júnior MM, Júnior AD, Mizobuchi RR, Yanasse RH, da Silva MV, Branco RB, Galbiatti JA. OPEN DRAINAGE VERSUS PERCUTANEOUS DRAINAGE IN THE TREATMENT OF TROPICAL PYOMYOSITIS. PROSPECTIVE AND RANDOMIZED STUDY. Rev Bras Ortop. 2010;45:260-268. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Wong CH, Choi SH, Wong KY. Piriformis pyomyositis: a report of three cases. J Orthop Surg (Hong Kong). 2008;16:389-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |