Published online Aug 26, 2023. doi: 10.12998/wjcc.v11.i24.5660
Peer-review started: June 13, 2023
First decision: July 7, 2023
Revised: July 13, 2023
Accepted: July 25, 2023
Article in press: July 25, 2023
Published online: August 26, 2023
Processing time: 72 Days and 21.3 Hours
Ileostomies are commonly performed after colon and rectal surgeries. Lapa
To compare the outcomes of laparoscopy-assisted and conventional ileostomies.
Data from 48 consecutive patients who underwent ileostomy at our institution between May 2021 and May 2022 were retrospectively analyzed. The groups comprised 26 and 22 patients who underwent laparoscopic ileostomy (laparoscopic group) and conventional ileostomy (conventional group), respectively, performed by a single surgeon. Patient demographics, operative characteristics, postoperative outcomes, and 30-d morbidities and mortality rates were analyzed.
The two groups had comparable mean ages, sex distributions, American Society of Anesthesiologists scores, and body mass indices. However, the laparoscopic group showed similar operative time, better visualization for adhesion lysis, and lower visual analog scale scores than the conventional group.
Laparoscopy-assisted ileostomy is a safe and efficient method that produces lower visual analog scale scores, better intraoperative visualization for effective adhesion lysis, and similar operative time compared with conventional ileostomy.
Core Tip: Laparoscopy-assisted ileostomy is a novel, safe, and efficient method for managing bowel obstruction in patients with colorectal cancer. Compared with conventional ileostomy, this method results in lower visual analog scale scores and better intraoperative visualization for effective adhesion lysis without extending the operative time.
- Citation: Wang YJ, Lin KH, Kang JC, Hu JM, Chen CY, Pu TW. Benefits of laparoscopy-assisted ileostomy in colorectal cancer patients with bowel obstruction. World J Clin Cases 2023; 11(24): 5660-5665
- URL: https://www.wjgnet.com/2307-8960/full/v11/i24/5660.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i24.5660
Colorectal surgery usually involves colonic resection and anastomosis and that anastomotic leaks can occur. Leaks can lead to fatal abdominal sepsis, loss of pelvic anastomoses, and the requirement of a permanent ostomy. Ileostomies can reduce the need for urgent reoperation in cases of anastomotic leak. Proximal diversion of the gastrointestinal tract is advocated in traditional colorectal surgical practice to avoid high-risk pelvic anastomoses[1], especially in high-risk patients, including those with short colorectal anastomoses (< 10 cm from the anal verge), coloanal anastomoses, technically difficult resections, and malnutrition. Men appear to benefit more from fecal diversion than women[2].
In patients undergoing colorectal surgery, fecal diversion could be beneficial, but complications can occur when an abdominal stoma is constructed. The complications following stoma placement includes minor complications that can be treated locally and major complications that require reoperation and prolonged hospitalization. The open surgical approach is conventionally used for ileostomy. Generally, a site away from the bony prominences and the areas for incision is selected. An area of healthy skin with a diameter of at least 2 inches is ideal, which is usually about two-thirds of the distance from the anterior superior iliac spine to the umbilicus[3]. The muscle is split to pass the stoma through the rectus abdominis.
For many other surgical procedures, the laparoscopic approach has been proven to lead to good outcomes[4]. We introduce a new method for laparoscopy-assisted ileostomy. The improved visualization enables easier identification and repair of coexistent parastomal hernias and adhesion lysis[5]. This study aimed to compare the operative and postoperative outcomes of laparoscopic and conventional ileostomies.
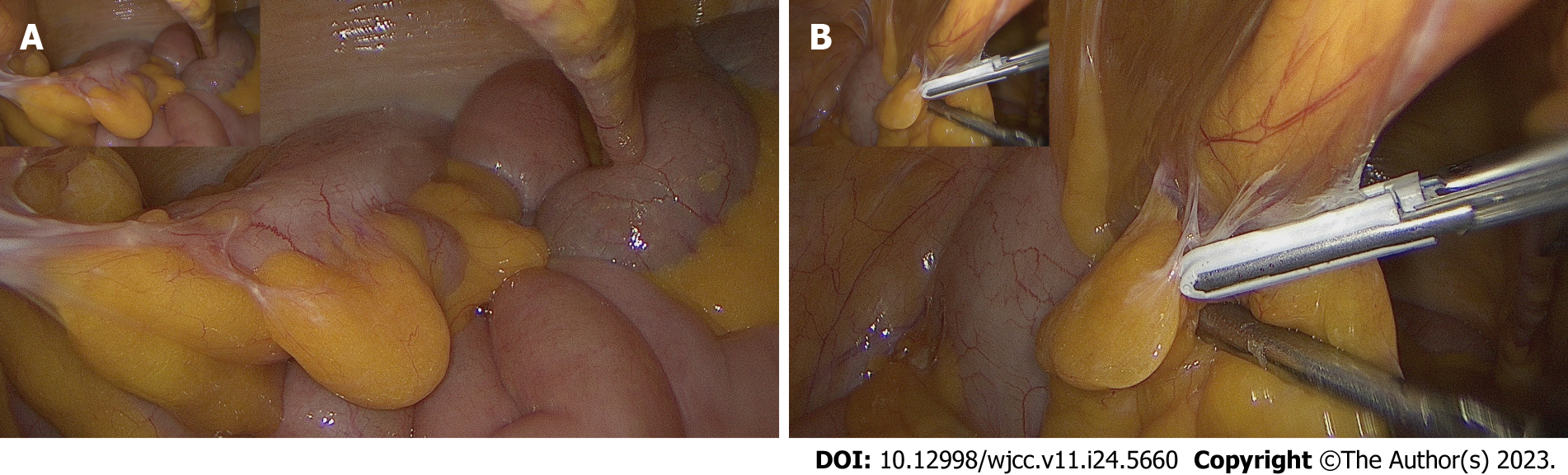
We retrospectively reviewed the data of patients diagnosed with colorectal cancer-related bowel obstruction who underwent ileostomy at our institution between May 2021 and May 2022. Laparoscopic and conventional open ileostomies were performed in 26 and 22 cases, respectively. Laparoscopic ileostomy was performed as follows. Three standard incisions were made, and gas was pumped into the abdomen to obtain pneumoperitoneum. Adhesion lysis was performed subsequently. Specifically, the appropriate loop of the small intestine was grabbed with laparoscopic forceps, pulled out through a cut in the abdomen, and stitched to the skin to form a stoma (Figure 1). The conventional open surgical approach usually involves a 5-6 cm surgical incision on the right side of the abdomen through which the intestine is pulled out to reach the ileum and stitched to the skin to form a stoma.
The following preoperative parameters were analyzed: Age, sex, American Society of Anesthesiologists (ASA) score, and body mass index (BMI). Comorbidities included diabetes mellitus, hypertension, chronic kidney disease, hypothyroidism, cardiac disease, and smoking. Operative parameters included operative time, estimated intraoperative blood loss, whether adhesion lysis was performed, duration of adhesion lysis, largest incision length, and intraoperative complications, such as bleeding, bowel injury, and bladder injury. Postoperative evaluations included visual analog scale (VAS) score, duration of hospital stay, and postoperative complications, such as a leak, ileus, wound infection, and stoma reversal time. Quantitative data are presented as means with standard deviations. The data of the two groups were compared using an independent samples t-test for continuous variables and a cross-table Pearson v2 test for categorical variables. Statistical significance was set at P < 0.05. GraphPad Prism (GraphPad Software, Inc., CA, United States) was used for the analyses.
Patient demographics were similar between the two groups; no significant differences were observed in mean age, sex, BMI, or ASA class (Table 1). Moreover, neither group showed significant differences in the prevalence of diabetes mellitus, hypertension, chronic kidney disease, hypothyroidism, heart disease, or smoking.
| Characteristics | Conventional group (n = 22) | Laparoscopic group (n = 26) | P value |
| Age, yr | 63.5 ± 8.4 | 61.4 ± 7.4 | 0.339 |
| Sex | |||
| Male | 12 (54.5) | 16 (61.5) | 0.624 |
| Female | 10 (45.4) | 10 (38.4) | 0.643 |
| Body mass index, kg/m2 [median (IQR)] | 20.2 ± 3.2 | 20.8 ± 2.8 | 0.47 |
| Mean ASA Class | 2.3 ± 4.9 | 2.3 ± 4.8 | 0.902 |
| Comorbidities | 19 (86.4) | 23 (88.5) | 0.827 |
| DM | 11 (50) | 14 (53.8) | 0.790 |
| Hypertension | 15 (68.2) | 17 (65.4) | 0.838 |
| CKD | 5 (22.7) | 7 (26.9) | 0.738 |
| Hypothyroidism | 0 (0) | 2 (7.7) | 0.184 |
| Cardiac disease | 2 (9.1) | 2 (7.7) | 0.861 |
| Smoking | 2 (9.1) | 4 (15.4) | 0.511 |
| Drinking | 8 (36.4) | 12 (46.2) | 0.493 |
The operative characteristics of the patients are listed in Table 2. There was no significant difference in the mean duration of ileostomy between the groups. Both ileostomy approaches required approximately 50 min for completion (usually less than 1 h). In addition, no significant difference was observed in the estimated intraoperative blood loss. The locations of the adhesions varied between the abdominal wall and bowel loops. All intra-abdominal adhesions visualized during stoma creation were removed in both groups. Significantly more patients in the laparoscopy group than in the open surgery group underwent adhesion lysis. Although adhesion lysis took longer in the laparoscopic group, there was no significant difference in the total operative time between the two groups.
| Operative characteristics | Conventional group (n = 22) | Laparoscopic group (n = 26) | P value |
| Operative time (min, SD) | 50.1 ± 20.4 | 61.5 ± 19.5 | 0.054 |
| Estimated blood loss (mL, SD) | 27.3 ± 14.9 | 30.0 ± 18.1 | 0.576 |
| Adhesion lysis performed | 9 (40.9) | 11 (42.3) | 0.922 |
| Adhesion lysis duration (min, SD) | 11.0 ± 4.3 | 22.2±5.6 | < 0.001 |
| The largest incision length | 5.5 ± 0.7 | 4.1 ± 0.8 | < 0.001 |
| Intraoperative | 3 | 3 | 0.490 |
| complication | |||
| Bleeding | 0 | 1 (3.8) | |
| Bowel injury | 1 (4.5) | 2 (7.7) | |
| Bladder injury | 2 (9) | 0 | |
| Vessel injury | 0 | 0 | |
| Others | 0 | 0 |
The postoperative outcomes of the laparoscopic approach were comparable with those of the conventional approach (Table 3). Lower VAS scores were found in the laparoscopic group. However, there were no significant differences in the mean length of hospital stay and postoperative complications, such as the development of urinary tract infections, pneumonia, or wound infection. There was also no significant difference in the time required for stoma reversal after ileostomy.
| Postoperative outcomes | Conventional group (n = 22) | Laparoscopic group (n = 26) | P value |
| Visual Analogue Scale score | 3.61 ± 0.9 | 3.0 ± 0.9 | 0.046 |
| Length of stay (d, mean ± SD) | 13.3 ± 13.4 | 9.3 ± 4.6 | 0.21 |
| Complications | 3 (13.6) | 1 (3.8) | 0.42 |
| UTI | 0 | 0 | |
| Pneumonia | 1 (4.5) | 0 | |
| Wound infection | 2 (9) | 1 (3.8) | |
| Leakage | 0 | 0 | |
| Ileus (over 5 d) | 0 | 0 | |
| Bleeding | 0 | 0 | |
| Incision hernia | 0 | 0 | |
| Reversal time (wk) | 10.7 ± 4.4 | 9.2 ± 4.1 | 0.226 |
Diverting ileostomy is an important component of the surgical management of lower gastrointestinal malignancies. Using an ileostomy to protect a newly constructed intestinal anastomosis is widely accepted[6,7]. Although laparoscopy is popular and is associated with several advantages, information regarding the outcomes of laparoscopic ileostomy compared with those of conventional ileostomy is lacking.
We introduced a new laparoscopic approach for ileostomy. To our knowledge, this is the first study to discuss and compare these two ileostomy methods in patients with colorectal cancer. The two groups in this retrospective study shared similar clinical characteristics, including age, sex, BMI, mean ASA score, and comorbidities. There were no significant differences in operative time and intraoperative blood loss. Moreover, adhesion lysis was more efficient and accurate in the laparoscopic group than in the conventional group. Postoperative VAS scores were lower in the laparoscopic group.
Whether ileostomy or colostomy is the optimal method for diverting feces remains controversial. Güenaga et al[8] reported that clinical factors, including mortality, wound infection, parastomal hernia, reoperation, anastomotic leak, incisional hernia, and bowel obstruction, were not significantly different between ileostomies and colostomies. Despite this, colostomy patients had significantly higher rates of stoma prolapse than ileostomates[9]. However, no significant differences were observed in the overall complications related to stoma formation and closure between the ileostomy and colostomy groups. Therefore, updated and cumulative meta-analyses and previous studies have not established one method over the other regarding the overall complications associated with stoma formation and closure. Patients diagnosed with colorectal cancer-related bowel obstruction were not included in our retrospective study, and dilatation over the cecum was observed. Loop ileostomy is the preferred fecal diversion method because it has a lower risk of prolapse than colostomy and yields comparable results.
Adhesion lysis was significantly more common in the laparoscopic group than in the conventional group. The enhanced visualization of the adhesions through the creation of pneumoperitoneum may have produced the higher lysis rate in the laparoscopic group. The average time spent on adhesion lysis was longer in the laparoscopic group than in the conventional group, but the degree of adhesion in both groups was difficult to quantify. It is easier for an experienced surgeon than an inexperienced surgeon to distinguish the peritoneum and grab the ileum for stoma formation, leading to fewer bowel-related complications. Placing the working laparoscopic ports did not extend the operative time judging by the overall operative time. Laparoscopic adhesion lysis was beneficial in several studies, which is an additional advantage of this technique[5,10,11]. Further, a drainage tube can be placed if ascites are present during peritoneal exploration.
There are some limitations in our study. First, some biases were inevitable because of the retrospective and single-hospital study design. Second, the sample was small because only one year of retrospective analysis was performed. Therefore, further large-scale prospective studies are needed to verify our results.
Laparoscopy-assisted ileostomy is safe and effective for fecal diversion in patients with colorectal cancer-related bowel obstruction. Compared with traditional ileostomy, the laparoscopic approach provides a better operative view via pneumoperitoneum creation, allowing effective adhesion lysis. Additionally, laparoscopy-assisted ileostomy produces better postoperative VAS scores than open ileostomy and does not extend the operative time or cause significant intraoperative blood loss.
Fecal diversion should be performed in patients with colorectal cancer-related bowel obstruction. The open surgical approach is the more commonly selected approach; however, laparoscopic assistance may be beneficial for this operation.
To compare surgical time and outcomes between laparoscopy-assisted and conventional ileostomy in patients with colorectal cancer-related acute bowel obstruction.
To demonstrate that laparoscopic ileostomy may be a good method for treating bowel obstruction in patients with colorectal cancer.
We investigated and compared patients with colorectal cancer-related bowel obstruction who underwent conventional or laparoscopy-assisted ileostomy at our institution between May 2021 and May 2022.
The mean operative time was similar between the conventional and laparoscopic groups. The laparoscopic group had better intraoperative visualization for appropriate adhesion lysis and lower visual analog scale scores than the conventional group.
Laparoscopy-assisted ileostomy is an efficient method with lower visual analog scale scores, better intraoperative visualization, and similar operative time compared with conventional ileostomy.
Further studies are required to determine the better approach for different conditions of bowel obstruction.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Gupta R, India; Jeong KY, South Korea S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Marusch F, Koch A, Schmidt U, Geibetaler S, Dralle H, Saeger HD, Wolff S, Nestler G, Pross M, Gastinger I, Lippert H. Value of a protective stoma in low anterior resections for rectal cancer. Dis Colon Rectum. 2002;45:1164-1171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 158] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 2. | Hanna MH, Vinci A, Pigazzi A. Diverting ileostomy in colorectal surgery: when is it necessary? Langenbecks Arch Surg. 2015;400:145-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 103] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 3. | Macdonald A, Chung D, Fell S, Pickford I. An assessment of surgeons' abilites to site colostomies accurately. Surgeon. 2003;1:347-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Royds J, O'Riordan JM, Mansour E, Eguare E, Neary P. Randomized clinical trial of the benefit of laparoscopy with closure of loop ileostomy. Br J Surg. 2013;100:1295-1301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Russek K, George JM, Zafar N, Cuevas-Estandia P, Franklin M. Laparoscopic loop ileostomy reversal: reducing morbidity while improving functional outcomes. JSLS. 2011;15:475-479. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Nurkin S, Kakarla VR, Ruiz DE, Cance WG, Tiszenkel HI. The role of faecal diversion in low rectal cancer: a review of 1791 patients having rectal resection with anastomosis for cancer, with and without a proximal stoma. Colorectal Dis. 2013;15:e309-e316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Karahasanoglu T, Hamzaoglu I, Baca B, Aytac E, Erenler I, Erdamar S. Evaluation of diverting ileostomy in laparoscopic low anterior resection for rectal cancer. Asian J Surg. 2011;34:63-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Güenaga KF, Lustosa SA, Saad SS, Saconato H, Matos D. Ileostomy or colostomy for temporary decompression of colorectal anastomosis. Cochrane Database Syst Rev. 2007;2007:CD004647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 82] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 9. | Gavriilidis P, Azoulay D, Taflampas P. Loop transverse colostomy vs loop ileostomy for defunctioning of colorectal anastomosis: a systematic review, updated conventional meta-analysis, and cumulative meta-analysis. Surg Today. 2019;49:108-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 10. | Szomstein S, Lo Menzo E, Simpfendorfer C, Zundel N, Rosenthal RJ. Laparoscopic lysis of adhesions. World J Surg. 2006;30:535-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 127] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 11. | Reissman P, Spira RM. Laparoscopy for adhesions. Semin Laparosc Surg. 2003;10:185-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |