Published online Jun 6, 2023. doi: 10.12998/wjcc.v11.i16.3915
Peer-review started: March 17, 2023
First decision: March 28, 2023
Revised: April 6, 2023
Accepted: May 6, 2023
Article in press: May 6, 2023
Published online: June 6, 2023
Processing time: 77 Days and 5.8 Hours
Tracheal neoplasms represent less than 0.1% of all malignancies and have no established treatment guidelines. Surgical resection with reconstruction is the primary treatment. This study demonstrates successful treatment of concurrent lung and tracheal tumors using surgical excision and intraoperative photo
A 74-year-old male with a history of smoking and chronic obstructive pulmonary disease was diagnosed with tracheal squamous cell carcinoma and right lower lobe adenocarcinoma. A multidisciplinary team created a treatment plan involving tumor resection and PDT. The tracheal tumor was removed through a tracheal incision and this was followed by intraluminal PDT. The trachea was repaired and a right lower lobectomy was performed. The patient received a second PDT treatment postoperatively and was discharged 10 d after the tracheal surgery, without complications. He then underwent platinum-based chemo
Our case of concurrent tracheal and lung cancers was successfully treated with surgical excision and intraoperative PDT which proved safe and effective in this patient.
Core Tip: This case report presents successful treatment of a rare case of concurrent tracheal and lung cancers in a 74-year-old male patient using surgical excision and intraoperative photodynamic therapy (PDT). This approach proved to be safe and effective, resulting in complete regression of the tracheal tumor. The patient's treatment included a combination of lobectomy, tracheal tumor excision, and intraluminal PDT, demonstrating the potential of this approach in managing such complex cases.
- Citation: Jung HS, Kim HJ, Kim KW. Intraoperative photodynamic therapy for tracheal mass in non-small cell lung cancer: A case report. World J Clin Cases 2023; 11(16): 3915-3920
- URL: https://www.wjgnet.com/2307-8960/full/v11/i16/3915.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i16.3915
Tracheal neoplasms account for fewer than 0.1% of all cancer cases[1]. Most tracheal malignancies are secondary tumors, originating from direct infiltration from nearby structures and, less frequently, from hematogenous or lymphatic spread of remote cancers[2]. Due to the rarity of this type of cancer, no definitive treatment guidelines based on randomized clinical trials exist, leaving treatment selection and sequencing to the discretion of the surgeon.
Surgical resection with reconstruction is the primary treatment for tracheal tumors. Segmental resection and reconstruction of the central airway can be effectively and safely performed in most patients. Although complications following tracheal surgery are rare, they can be devastating. Herein, we report the successful treatment of a case of concurrent lung and tracheal tumors through surgical excision and intraoperative photodynamic therapy (PDT).
A 74-year-old male patient presented to the clinic with complaints of intermittent hemoptysis and wheezing.
The patient started observing blood-tinged sputum 1 mo prior to presentation, and his dyspnea worsened 1 wk prior to presentation.
The patient was a former smoker with a 140 pack-year history and a history of moderate-to-severe chronic obstructive pulmonary disease. Two years prior, he had received a percutaneous coronary intervention for stable angina; the treatment had involved implanting a drug-eluting stent in the left obtuse marginal branch of the left circumflex artery.
The patient had no personal or family history of malignant tumors.
Initial physical exam revealed the following: temperature of 36.5 °C; blood pressure of 110/63 mmHg; heart rate at 73/min; respiratory rate at 22/min; and O2 saturation at 93% on room air. Lung examination revealed a barrel chest and poor air entry with moderate inspiratory and expiratory wheezing. Heart and abdominal examinations were within normal limits.
Arterial blood gas testing on admission revealed a pH of 7.5, pCO2 of 24 mmHg, pO2 of 62 mmHg, and HCO3- of 20.5 mEq/L. No other abnormality was found on routine laboratory testing.
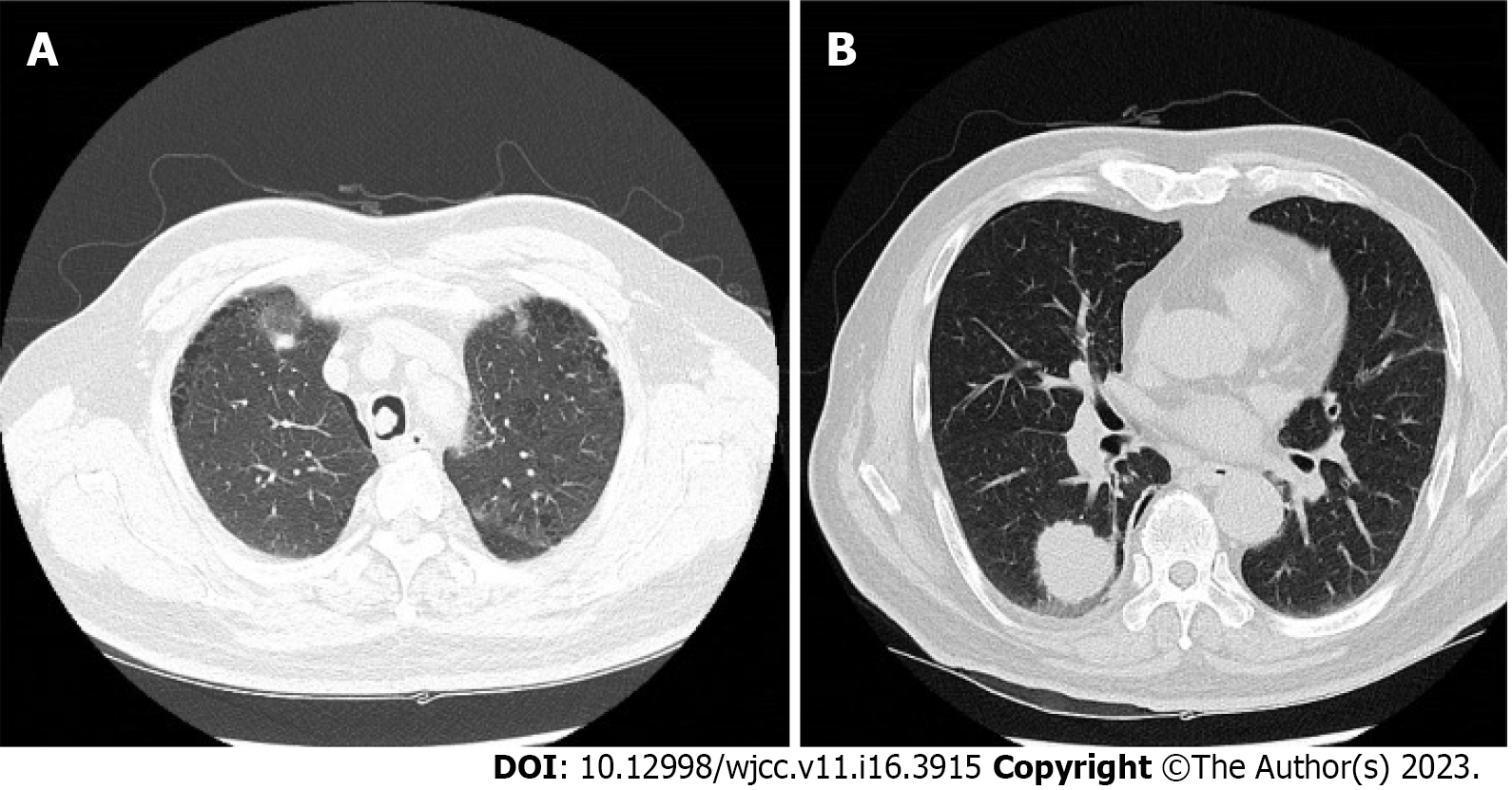
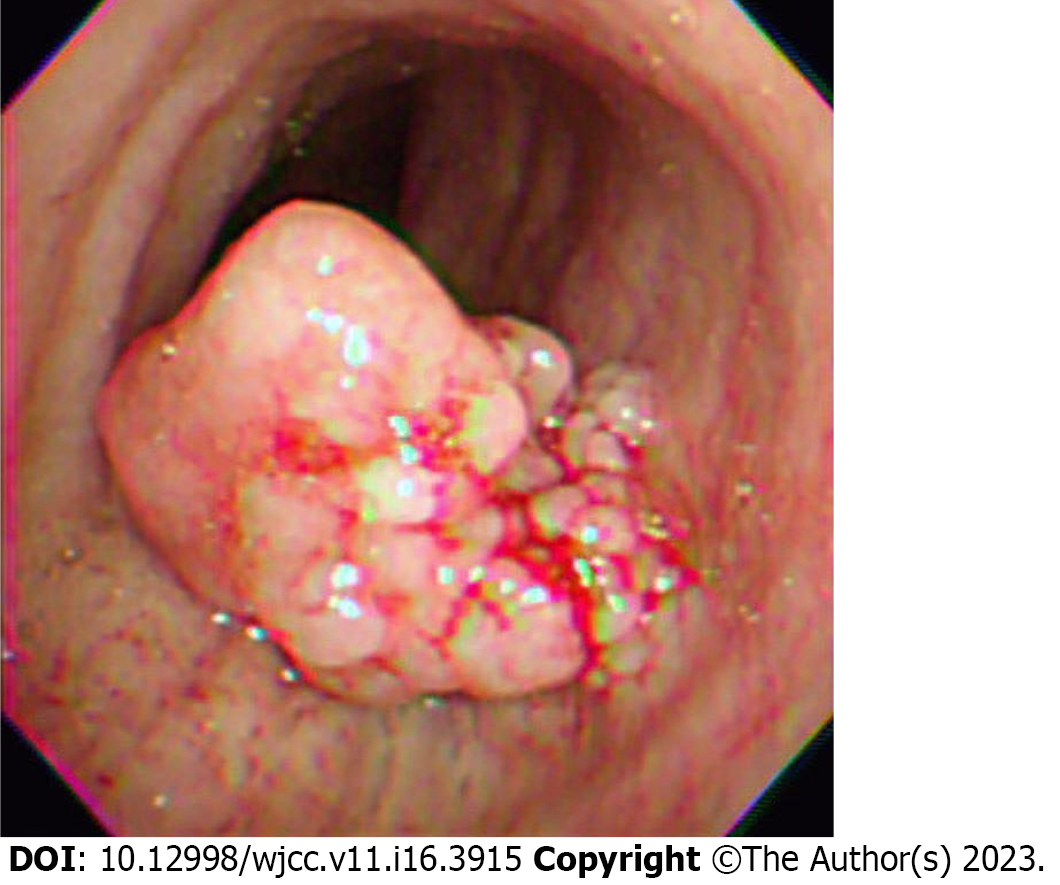
A computed tomography scan of the chest revealed a suspicious polypoid mass in the right mid-tracheal wall and a 3-cm mass in the right lower lobe of the lung (Figure 1). The patient underwent bronchoscopy, which revealed a single tracheal polyp causing up to a 70% tracheal obstruction (Figure 2).
Biopsy samples were taken. The pathology results showed the tracheal lesion to be squamous cell carcinoma and the lung mass to be adenocarcinoma.
A multidisciplinary conference was held to discuss the case. Initially, the plan was to perform a tumor resection of the tracheal lesion through rigid bronchoscopy, but this technique was unavailable at the time of surgery due to problems with the equipment. The next option was to perform a tumor resection through a tracheal incision, followed by PDT. At 48 h before surgery, a 2 mg/kg dose of the photoactive compound Photofrin® (Pinnacle Biologics Inc., Bannockburn, IL, United States) was combined with 40 mL of isotonic saline solution and administered via intravenous injection. To ensure patient safety, selective veno-venous extracorporeal membrane oxygenation (ECMO) was initiated prior to general anesthesia, to guard against introducing it in the possible setting of airway compromise.
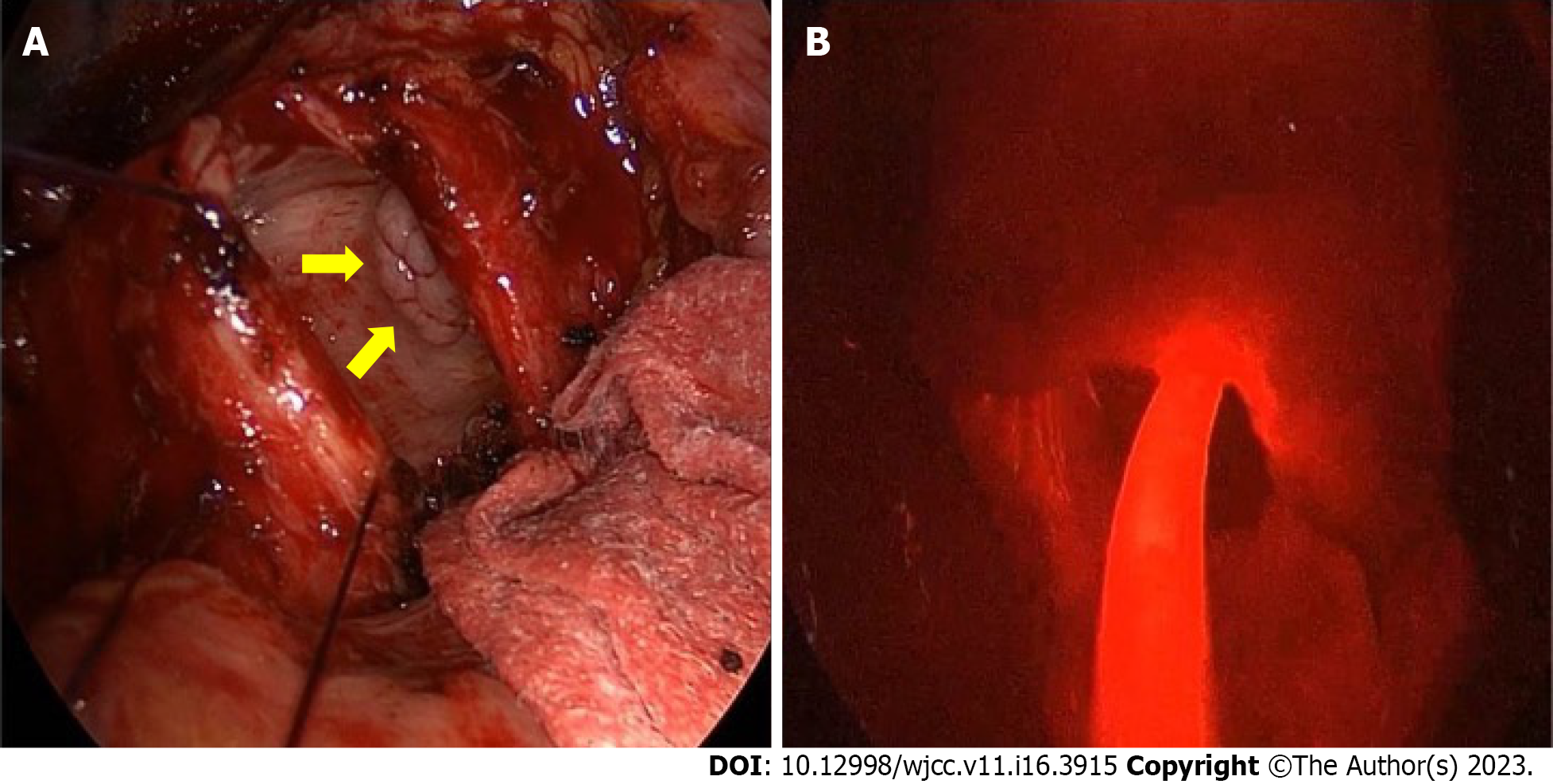
Throughout the surgery, the patient was maintained with 3–4 L/min flow of 100% fraction of inspired oxygen gas at 2–3 L/min, without the need for additional heparin infusions. The tumor was resected at its base using an electrocautery snare, followed by administration of intraluminal PDT (Figure 3). For the PDT, the laser light was irradiated through an optic fiber featuring a 30-mm cylindrical disperser. A 630-nm diode laser (Diomed, Cambridge, United Kingdom) was utilized to emit light into the tracheal lumen (120 J/cm2 at 300 mW for a duration of 400 s). The tracheal margins were reconnected using absorbable continuous sutures. The anastomosis was checked using the underwater method after placement of the endotracheal tube. After reinforcing the trachea, conventional lobectomy of the right lower lobe was performed, and no air leaks were observed at a ventilatory pressure of 25 cmH2O. The patient was ventilated with an endotracheal tube, and a simple sweep gas test, confirmed by pulse oximetry which showed successful performance. ECMO and use of the central venous catheter were discontinued.
After transferring the patient to the intensive care unit, he was maintained on a ventilator. On day 3 after surgery, a second PDT with the same energy as before was administered using flexible bronchoscopy. The patient was discharged 10 d after tracheal surgery with no complications. As there was evidence of lymphovascular invasion in the histopathology of the lung cancer, platinum-based adjuvant chemotherapy was initiated 6 wk after the operation.
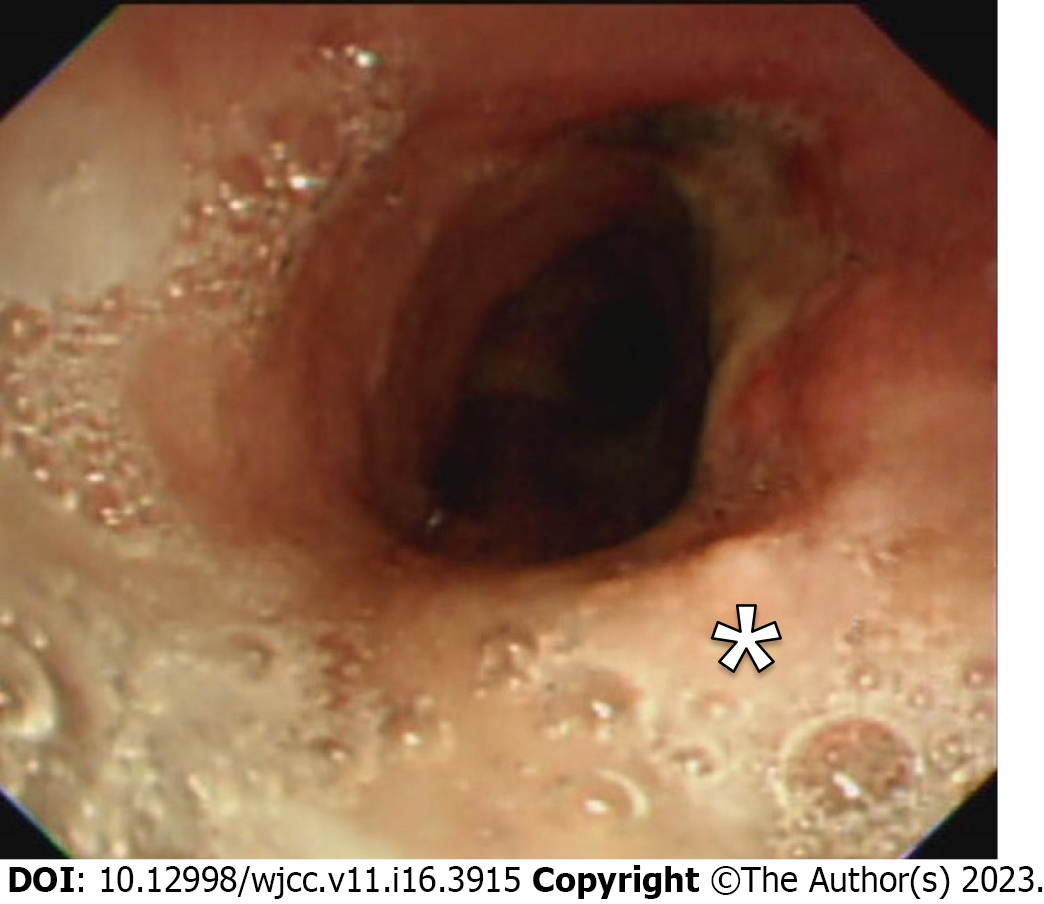
A bronchoscopy conducted 3 mo after the surgery demonstrated tracheal healing, evidenced by re-epithelialization of the healthy mucosal tissue at the site of resection (Figure 4). No recurrence of the tumor was observed during the 15 mo follow-up period.
Tracheal tumors are rare, accounting for less than 1% of all malignancies[1]. Despite their infrequency, they can cause severe airway obstruction in patients. The exact cause of these tumors remains unknown, but risk factors such as smoking, exposure to specific chemicals, and familial history may contribute to their development. The most appropriate treatment plan for a tracheal tumor is dependent on its type and stage, as well as the overall health of the patient. Treatment may include surgical excision, radiation therapy, PDT, chemotherapy, and/or stenting.
PDT has been used as a palliative treatment for malignant airway obstructions in the trachea or bronchi. Based on a recent analysis, patients with early-stage central lung cancer who underwent PDT experienced a full response in 30%-100% of instances, with the total 5-year survival rate being 61%[3]. Ji et al[4] discovered similar outcomes, demonstrating that employment of a second-generation photosensitizer in PDT effectively alleviated airway blockage in advanced non-small cell lung cancer. Overall, PDT has demonstrated efficacy against various types of tumor cells and can be performed on patients who have undergone previous treatments such as surgery, radiation therapy, or chemotherapy. PDT has also been evaluated for its ability to alleviate symptoms and improve survival in patients with advanced, inoperable bronchogenic cancer and endobronchial obstruction[5].
Tracheal resection with end-to-end anastomosis is the preferred treatment for tracheal tumors, as it ensures the restoration of an anatomically normal airway. However, the primary challenge of this procedure lies in the lesion's extent. Not only is it infeasible for lesions of considerable length but it also increases tension at the anastomotic site, potentially causing complications such as separation, granuloma formation, or re-stenosis at the tracheal anastomosis. Anastomotic separation is a particularly severe complication, and can result in dramatic airway loss with potentially fatal outcomes. Complete airway loss is rare but has a high fatality rate, often attributed to excessive tension. While study findings vary, it is widely accepted that complications related to airway separation escalate dramatically when more than 3 to 4 cm of the airway is resected[6,7]. Consequently, our objective in this case was to minimize tension. Our previous research showed that PDT was effective in controlling microscopic residual tumors in the distal trachea, and we expected similar results in this patient[8]. We made an incision in the tracheal wall, removed only the tumor, and applied PDT to the tumor bed. This method allowed us to bypass tracheal segmental resection, which carries the risk of fistulous complications at the anastomotic site.
Herein, we have presented the successful treatment of a patient with concurrent tracheal and lung cancers using a combination of surgical excision and intraoperative PDT. This approach was both safe and effective, and resulted in the complete regression of the protruding tracheal squamous cell carcinoma.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Liu ZW, China; Yu F, China S-Editor: Liu XF L-Editor: Filipodia P-Editor: Zhao S
| 1. | Madariaga ML, Gaissert HA. Secondary tracheal tumors: a systematic review. Ann Cardiothorac Surg. 2018;7:183-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 2. | Junker K. Pathology of tracheal tumors. Thorac Surg Clin. 2014;24:7-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 3. | Moghissi K, Dixon K. Update on the current indications, practice and results of photodynamic therapy (PDT) in early central lung cancer (ECLC). Photodiagnosis Photodyn Ther. 2008;5:10-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 36] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 4. | Ji W, Yoo JW, Bae EK, Lee JH, Choi CM. The effect of Radachlorin® PDT in advanced NSCLC: a pilot study. Photodiagnosis Photodyn Ther. 2013;10:120-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 5. | Wang K, Yu B, Pathak JL. An update in clinical utilization of photodynamic therapy for lung cancer. J Cancer. 2021;12:1154-1160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 60] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 6. | Auchincloss HG, Wright CD. Complications after tracheal resection and reconstruction: prevention and treatment. J Thorac Dis. 2016;8:S160-S167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 45] [Reference Citation Analysis (0)] |
| 7. | Tapias LF, Mathisen DJ. Prevention and management of complications following tracheal resections-lessons learned at the Massachusetts General Hospital. Ann Cardiothorac Surg. 2018;7:237-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 8. | Jung HS, Kim HJ. Definitive surgery and intraoperative photodynamic therapy for locally advanced non-small cell lung cancer: a case report. World J Surg Oncol. 2022;20:265. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |