Published online May 26, 2023. doi: 10.12998/wjcc.v11.i15.3511
Peer-review started: February 7, 2023
First decision: February 28, 2023
Revised: March 6, 2023
Accepted: April 6, 2023
Article in press: April 6, 2023
Published online: May 26, 2023
Processing time: 107 Days and 6.8 Hours
Heart failure (HF) often affects the progress of sepsis patients, although its impact on outcomes is inconsistent and inconclusive.
To conduct a systematic review and meta-analysis of the impact of HF on morta
PubMed, Embase, Web of Science, and the Cochrane Library databases were searched to compare the outcomes of sepsis patients with HF. A random effect model was used to summarize the mortality data, and the odds ratio (OR) and 95% confidence interval (CI) were calculated as effect indicators.
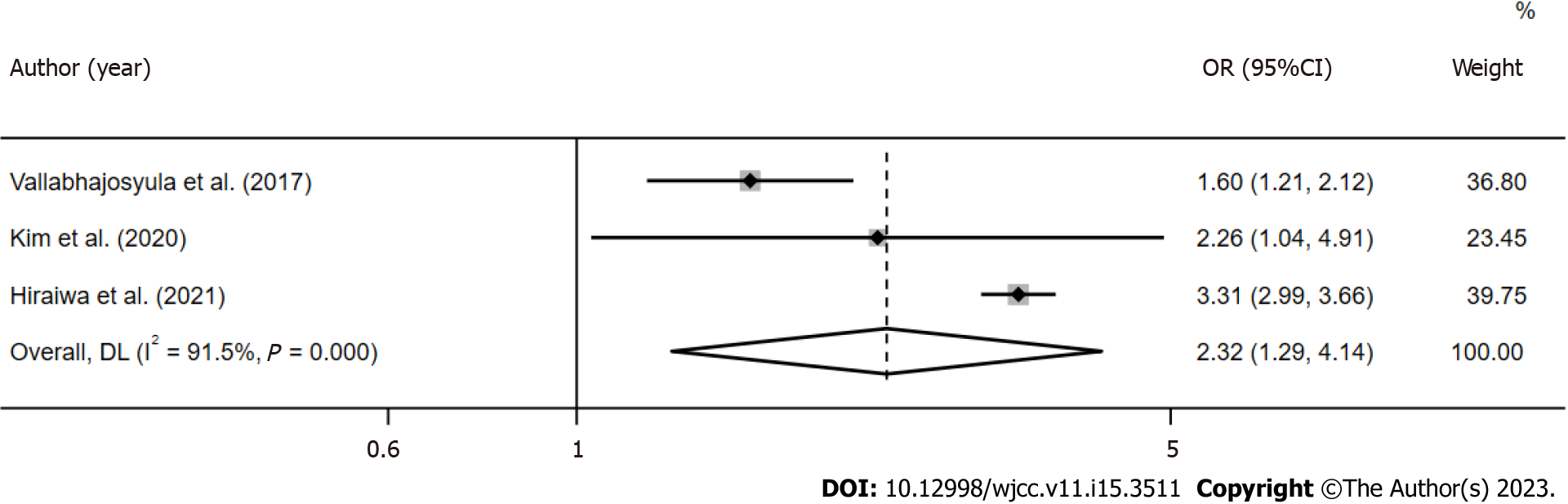
Among 18001 records retrieved in the literature search, 35712 patients from 10 separate studies were included. The results showed that sepsis patients with HF were associated with increased total mortality (OR = 1.80, 95%CI: 1.34-2.43; I2 = 92.1%), with high heterogeneity between studies. Significant subgroup differences according to age, geographical location, and HF patient sample were observed. HF did not increase the 1-year mortality of patients (OR = 1.11, 95%CI: 0.75-1.62; I2 = 93.2%), and the mortality of patients with isolated right ventricular dysfunction (OR=2.32, 95%CI: 1.29-4.14; I2 = 91.5%) increased significantly.
In patients with sepsis, HF is often associated with adverse outcomes and mortality. Our results call for more high-quality research and strategies to improve outcomes for sepsis patients with HF.
Core Tip: Heart failure (HF) treatment and management measures in sepsis patients have been optimized and improved. However, it is still controversial whether HF will worsen the clinical outcomes of sepsis patients. We conducted a meta-analysis to determine if HF tends to increase the risk of death in sepsis patients. Limited by significant publication bias, this issue requires more high-quality research and a focus on strategies to improve outcomes in sepsis patients with HF.
- Citation: Zhu MY, Tang XK, Gao Y, Xu JJ, Gong YQ. Impact of heart failure on outcomes in patients with sepsis: A systematic review and meta-analysis. World J Clin Cases 2023; 11(15): 3511-3521
- URL: https://www.wjgnet.com/2307-8960/full/v11/i15/3511.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i15.3511
Sepsis is defined as life-threatening organ dysfunction caused by maladjustment of the body's response to infection[1]. Sepsis is a major health problem worldwide, and the mortality rate in the intensive care unit (ICU) and hospital can reach 25.8% and 35.3%, respectively[2]. The development of organ dysfunction is the most important clinical event during sepsis as it is directly related to mortality and morbidity[3,4].
Sepsis and heart failure (HF) are common complications in critically ill patients and cause additional complex pathological conditions[5,6]. Studies have shown that sepsis and HF have the highest 30-day readmission rates among medical insurance patients[7]. Sepsis/septic shock causes a quarter of all HF deaths, and HF is likely to be a critical factor in the survival of patients with sepsis[8,9]. It is concerning that the mortality rate in patients with cardiac insufficiency and sepsis is extremely high (can reach 90%)[10]. However, other studies have shown that cardiac dysfunction in sepsis patients does not increase the risk of long-term mortality[11,12]. Furthermore, a meta-analysis determined that the presence of new left ventricular systolic dysfunction associated with sepsis is neither a sensitive nor a specific predictor of mortality[13]. Given these confounding findings, a meta-analysis is warranted to provide a systematic and comprehensive understanding of the impact of HF on sepsis outcomes.
Therefore, the aim of the present study was to determine whether HF increases mortality in patients with sepsis and to summarize and evaluate relevant information on prognosis.
The study protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) with registration No. CRD42022377710. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were adopted in this study[14].
A systematic and comprehensive literature search of PubMed, Embase, Web of Science, and Cochrane Library databases was carried out from inception to November 9, 2022. The search was carried out by combining controlled vocabulary and natural language terms. The main search terms included “sepsis”, “septic shock”, “heart failure”, “cardiac failure”, etc. The complete search strategy can be found in the Supplementary material. The search process was completed independently by two researchers. In addition, the references included in the articles were traced to supplement the relevant literature. According to PRISMA guidelines, systematic and sequential screening of the title and abstract was carried out. After the first screening stage, the full-text eligibility of each selected article was evaluated. Disagreements were settled by collegiate discussion.
The inclusion criteria were: (1) Studies that evaluated patients with HF during sepsis, severe sepsis, and/or septic shock; (2) The control group was composed of patients with sepsis or septic shock without HF; and (3) Studies that reported at least one mortality outcome (i.e., ICU, hospital, 28-day mortality or long-term mortality rates).
The exclusion criteria were: (1) Abstracts, reviews, editorials, letters, case reports, systematic reviews, and meta-analyses; (2) Articles written in languages other than English; (3) Repeated publications; and (4) Insufficient data to estimate odds ratio (OR) and 95% confidence interval (CI) of each related result. Despite minor differences between studies, sepsis was diagnosed following current guidelines and described as organ dysfunction due to infection.
All candidate studies were independently evaluated and extracted by two researchers, and differences were resolved through discussion with a third researcher. The following items were recorded for each study: (1) Basic information included in the study: The name of the main author, the year of publication, background, study design, etc; (2) Baseline characteristics of the subjects and interventions; and (3) Key elements of bias risk assessment. If necessary, the original study author was contacted by email or telephone to obtain information that was not determined but important for this study. Two researchers independently evaluated the bias risk of the included studies and cross-checked the results. The Newcastle Ottawa quality scale (NOS) was used to evaluate the bias risk of observational studies, which included three parts: selection (0-4 points), comparability (0-2 points) and outcome evaluation (0-3 points). High-quality research was defined as having a NOS score of 6 or higher.
All statistical analyses were performed using STATA version 17.0 (Stata Corp, College Station, TX, United States). Mortality data were combined using OR with 95%CI. Using the crude data provided in the candidate articles, we estimated unadjusted OR and 95%CI for prognostic mortality. If statistical results were reported in the article, the adjusted OR was used directly. Heterogeneity of the studies was calculated using Cochran's Q test and the Higgins I-squared statistic, and significant heterogeneity was defined as a Ph < 0.10 or I2 > 50%[15]. If significant heterogeneity was observed, a random effect model was used to summarize the results, otherwise, a fixed effect model was adopted. For significant heterogeneity, the "leave-one-out" method was used for sensitivity analysis, and one study was deleted for each iteration to analyze its influence on aggregate estimation and heterogeneity. Subgroup analysis and meta-regression were performed to examine and explain the heterogeneity of the research results. The Egger[16] and Begg[17] tests were used to assess publication bias, and when significant publication bias was found, the trim-and-fill method[18] was used to further test and adjust for publication bias, and P < 0.05 was considered statistically significant.
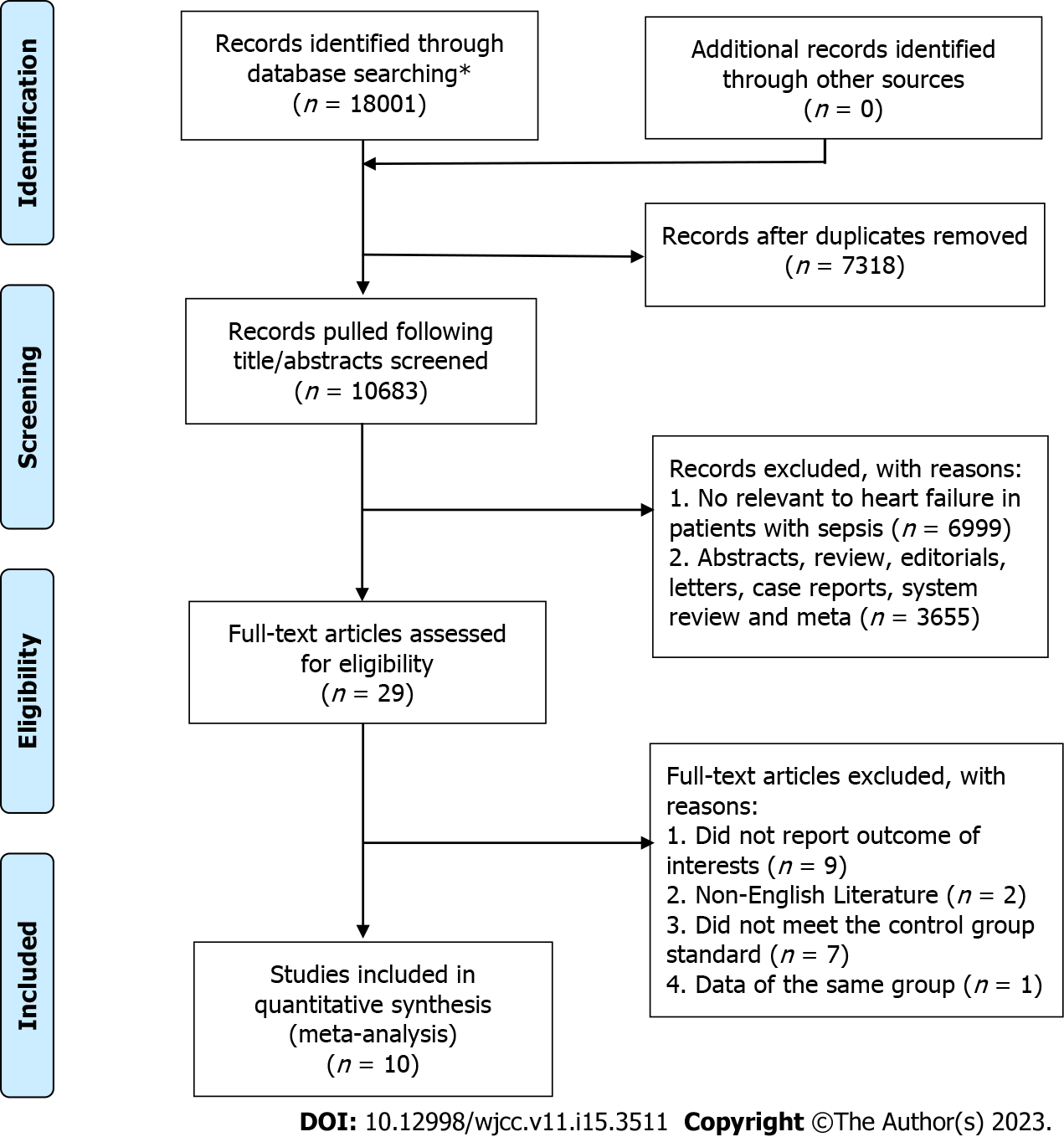
After searching the electronic databases, 18001 publications were retrieved. Following thorough examination according to the inclusion and exclusion criteria, 10 studies (35712 patients in total) published between 2012 and 2021 were finally included in the meta-analysis[4,6,9,11,12,19-23]. A PRISMA flow chart of the study is presented in Figure 1.
The main characteristics of the included studies are reported in Table 1. Of the ten included studies, five studies were conducted in the United States[4,6,11,12,22] and the remaining five studies were from the Republic of China[9], Macedonia[19], France[20], Israel[21] and Japan[23]. Three of the studies were prospective studies[4,19,20] and the other seven were retrospective studies[6,9,11,12,21-23]. Seven studies included intensive care unit (ICU) patients[6,9,12,19-21,23], and two studies were based on relevant databases[21,23]. Three studies included patients admitted to general Medicare hospitals[4,11,22], one of which was based on the healthcare system database[4]. Eight studies reported adjusted OR[4,6,11,12,19,20,22,23], a and two studies reported unadjusted OR[9,21]. In addition, two studies included more than 1000 patients with sepsis[4,11], seven included 100 to 1000 patients with sepsis[9,12,19,21-23], and one included less than 100 patients with sepsis[20]. In these studies, the mortality rate of patients with sepsis ranged from 9.4% to 56.2%, and the average age ranged from 31.5 to 76 years (Table 2). According to the NOS score, all the articles included in the meta-analysis were of high quality.
| Ref. | Year | Setting | Study design | Sepsis severity | Diagnosis of HF | Outcomes | ORs | NOS score (S C O) |
| Grozdanovski et al[19] | 2012 | Single-centre, ICU, Republic of Macedonia | Prospective | Severe sepsis/septic shock | Confirmed by medical record | Hospital mortality | Adjusted | 4 1 2 |
| cui et al[9] | 2014 | Single-centre, ICU, China | Retros-pective | Severe sepsis/septic shock | Confirmed by medical record | Hospital mortality | Unadjusted | 3 1 2 |
| Lemay et al[4] | 2014 | Multicenter, database about medicare hospital, United States | Prospective | Severe sepsis | Confirmed by database of the Department of Veterans’ Affairs Health Care systems | Long-term mortality | Adjusted | 4 2 3 |
| Mourad et al[20] | 2014 | Single-centre, ICU, France | Prospective | Septic shock | Selection with diastolic dysfunction by echocardiography and medical record | Hospital mortality | Adjusted | 4 2 2 |
| Vallabhajosyula et al[12] | 2017 | Single-centre, ICU, United States | Retros-pective | Severe sepsis/septic shock | Selection with ventricular dysfunction by echocardiography and medical record | 1-year mortality | Adjusted | 4 2 3 |
| Abu-Kaf et al[21] | 2018 | Single-centre, ICU databases, Israel | Retros-pective | Severe sepsis | Confirmed by medical record in ISR-SEPSIS | 2-year mortality | Unadjusted | 4 2 2 |
| Arnautovic et al[6] | 2018 | Multicenter, ICU, United States | Retros-pective | Septic shock | Confirmed by medical record | Hospital mortality | Adjusted | 4 2 2 |
| Schuler et al[11] | 2018 | Multicenter, medicare hospital, United States | Retros-pective | Sepsis | Assessment of cardiac failure with SOFA score | long-term mortality | Adjusted | 4 2 3 |
| Kim et al[22] | 2020 | Single-centre, medicare hospital, United States | Retros-pective | Septic shock | Selection with ventricular dysfunction by echocardiography and medical record | 28- day mortality | Adjusted | 4 2 2 |
| Hiraiwa et al[23] | 2021 | Single-centre, ICU database, Japan | Retrospective | Septic shock | Selection with ventricular dysfunction by echocardiography and medical record in MIMIC-III | Hospital mortality | Adjusted | 4 2 3 |
| Ref. | Sample size (M/F) | HF | Disease-related score (median or range) | Sepsis mortality | Age (median or range) | Hospital/ICU LOS (days in median or range) | Mechanical ventilation | Charlson comorbidity index (median or range) |
| Grozdanovski et al[19] | 184 (122/62) | 65 | N/A | 95 (51.6%) | 57.1 (17.9) | 13 (9-20) | N/A | N/A |
| cui et al[9] | 338 (235/103) | 24 | APACHEII: 14.0 (7.4); SOFA: 6.1 (4.1) | 114 (33.7%) | 55.8 (18.7) | 14.3 (9.35) | N/A | 1.2 (1.5) |
| Lemay et al[4] | 2727 (2687/40) | 713 | N/A | 1501 (55.0%) | 76 (6.5) | N/A | 661 (24.2%) | 3.5 (2.6) |
| Mourad et al[20] | 72 (32/40) | 33 | SAPS II: 57 (45.7-69); SOFA: 11 (9-13) | 35 (48.6%) | 58 (49-66) | 8 (4-12.2) | 30 (42%) | N/A |
| Vallabhajosyula et al[12] | 388 (198/190) | 214 | APACHE-III: 83.5 (67.8-106.3); SOFA: 8.7 (6.3-11.7) | 218 (56.2%) | 66.5 (54.6-76.5) | N/A | 213 (54.9%) | 5.33 (3.33-7.67) |
| Abu-Kaf et al[21] | 409 (210/199) | 19 | N/A | 41 (10.02%) | 31.5 (7.4) | 22 (11-43) | N/A | 0.29 (0.64) |
| Arnautovic et al[6] | 109 (48/61) | 89 | APACHEII: 20 (15-26) | 55 (50.5%) | 68 (14) | 8 (4-13) | 73 (67%) | 7 (4-9) |
| Schuler et al[11] | 30163 (14500/4815) | 19315 | N/A | 2847 (9.4%) | 69.8 (17.1) | 3.7 (2.4-6.2) | N/A | N/A |
| Kim et al[22] | 778 (446/332) | 45 | SOFA: 9 (6-11) | 233 (29.9%) | 67 (57-74) | 3.0 (0.0-8.0) | N/A | N/A |
| Hiraiwa et al[23] | 544 (315/229) | 190 | SOFA: 13(11-16) | 235 (43.2%) | 67 (53-78) | 6.7 (2.8-13.3) | 217 (39.9%) | N/A |
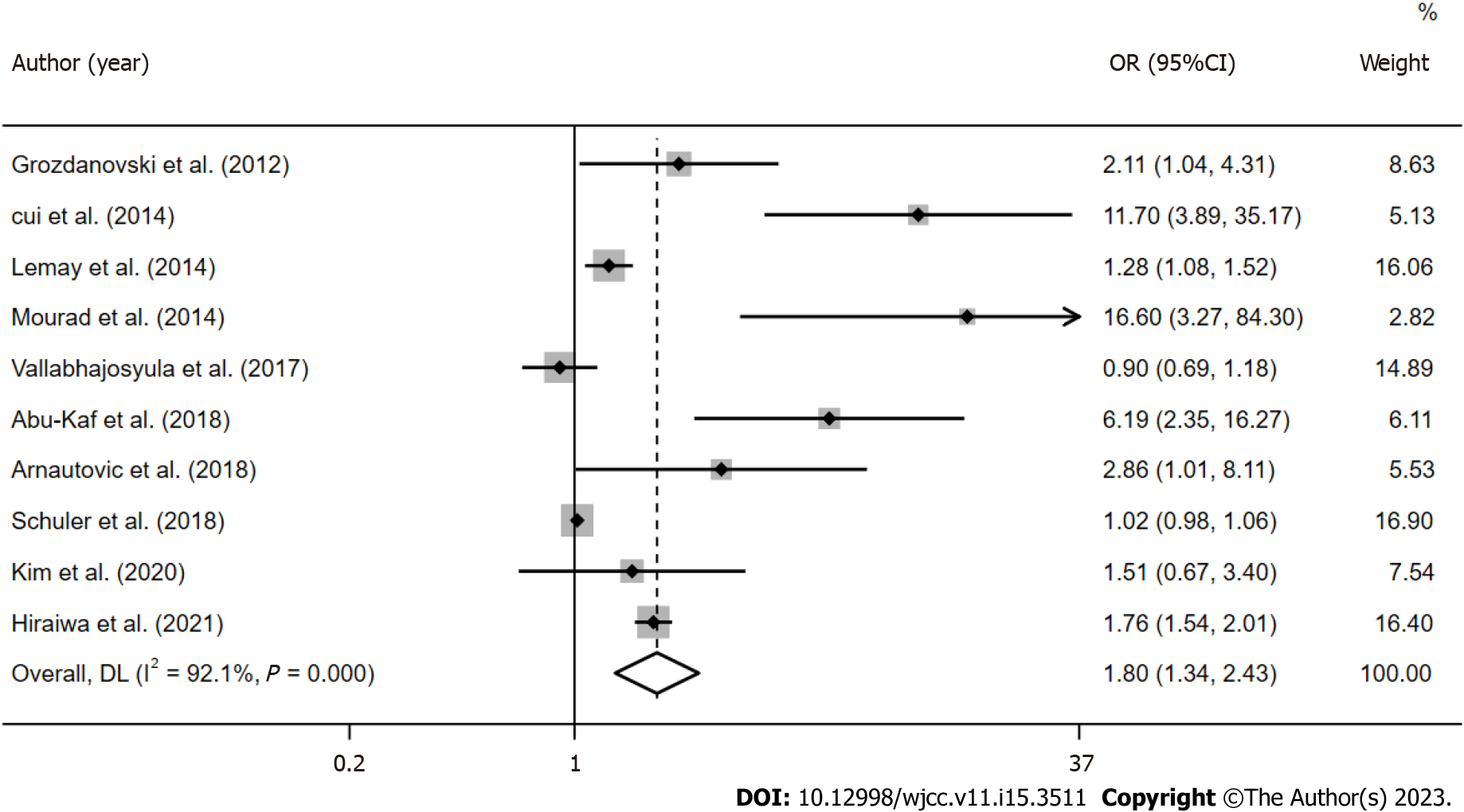
Due to significant heterogeneity (I2 = 92.1%, Ph < 0.001) in the studies included in the meta-analysis, a random-effects model was adopted. The results indicated that sepsis patients with HF were significantly associated with increased mortality, with an OR of 1.80 (95%CI: 1.34-2.43; P < 0.001; Figure 2).
In subgroup analysis, the combined OR of prospective and retrospective studies was 2.53 (95%CI: 0.97-6.61; P > 0.05) and 1.82 (95%CI: 1.24-2.66; P < 0.05), respectively. According to the sample size of patients with HF (≥ 100 patients and < 100 patients), the combined OR was 1.21 (95%CI: 0.90-1.63; P > 0.05) and 4.12 (95%CI: 2.02-8.41; P < 0.001), respectively. According to the grouping analysis of the patients included, the combined OR of patients from the ICU was 2.88 (95%CI: 1.67-4.97; P < 0.001), and that of patients from general hospitals was 1.14 (95%CI: 0.93-1.41; P > 0.05). The combined OR of hospitalization or 28-day mortality was 3.02 (95%CI: 1.67-5.49; P < 0.001), and the combined OR of long-term mortality was 1.18 (95%CI: 0.91-1.54; P > 0.05). In all the studies, the OR in patients with an average age ≥ 65 years and patients under 65 years were 1.29 (95%CI: 0.98-1.71; P < 0.001) and 6.22 (95%CI: 2.39-16.18; P > 0.05), respectively. The combined OR of studies published in the United States was 1.12 (95%CI: 0.93-1.34; P > 0.05), and that of studies published in other countries was 4.45 (95%CI: 1.95-10.12; P < 0.001). Table 3 summarizes further information for each subgroup.
| Analysis | N | Ref. | Random-effect model | Fixed-effect model | Heterogeneity | |||
| OR (95%CI) | P | OR (95%CI) | P | I2 | Ph | |||
| Patient mortality | 10 | [4,6,9,11,12,19-23] | 1.81 (1.34, 2.43) | 0 | 1.08 (1.04, 1.12) | 0 | 0.921 | 0 |
| Subgroup 1: Prospective | 3 | [4,19,20] | 2.53 (0.97, 6.61) | 0.057 | 1.35 (1.15, 1.59) | 0 | 0.819 | 0 |
| Retrospective | 7 | [6,9,11,12,21-23] | 1.82 (1.24, 2.66) | 0.002 | 1.07 (1.03, 1.11) | 0 | 0.937 | 0 |
| Subgroup 2: HF sample size ≥ 100 | 4 | [4,11,12,23] | 1.21 (0.90, 1.63) | 0.216 | 1.07 (1.03, 1.11) | 0 | 0.954 | 0 |
| HF Sample size < 100 | 6 | [6,9,19-22] | 4.12 (2.02, 8.41) | 0 | 3.37 (2.29, 4.95) | 0 | 0.681 | 0.008 |
| Subgroup 3: ICU | 7 | [6,9,12,19-21,23] | 2.88 (1.67, 4.97) | 0 | 1.65 (1.47, 1.86) | 0 | 0.878 | 0 |
| General hospital | 3 | [4,11,22] | 1.14 (0.93, 1.41) | 0.206 | 1.03 (1.04, 1.12) | 0.1 | 0.726 | 0.026 |
| Subgroup 4: Hospital or 28-day mortality | 6 | [6,9,11,19,20,22,23] | 3.02 (1.67, 5.49) | 0 | 1.85 (1.63, 2.10) | 0 | 0.742 | 0.002 |
| long term mortality | 4 | [4,12,21] | 1.18 (0.91, 1.54) | 0.207 | 1.03 (0.99, 1.07) | 0.106 | 0.855 | 0 |
| Subgroup 5: Average age ≥ 65 | 6 | [4,6,11,12,22,23] | 1.29 (0.98, 1.71) | 0.075 | 1.07 (1.04, 1.11) | 0 | 0.928 | 0 |
| Average age < 65 | 4 | [9,19,21] | 6.22 (2.39, 16.18) | 0 | 4.65 (2.86, 7.55) | 0 | 0.703 | 0.018 |
| Subgroup 6: United States | 5 | [4,6,11,12,22,23] | 1.12 (0.93, 1.34) | 0.246 | 1.03 (0.99, 1.07) | 0.112 | 0.665 | 0.018 |
| Other countries | 5 | [9,19-21,23] | 4.45 (1.95, 10.12) | 0 | 1.88 (1.66, 2.14) | 0 | 0.836 | 0 |
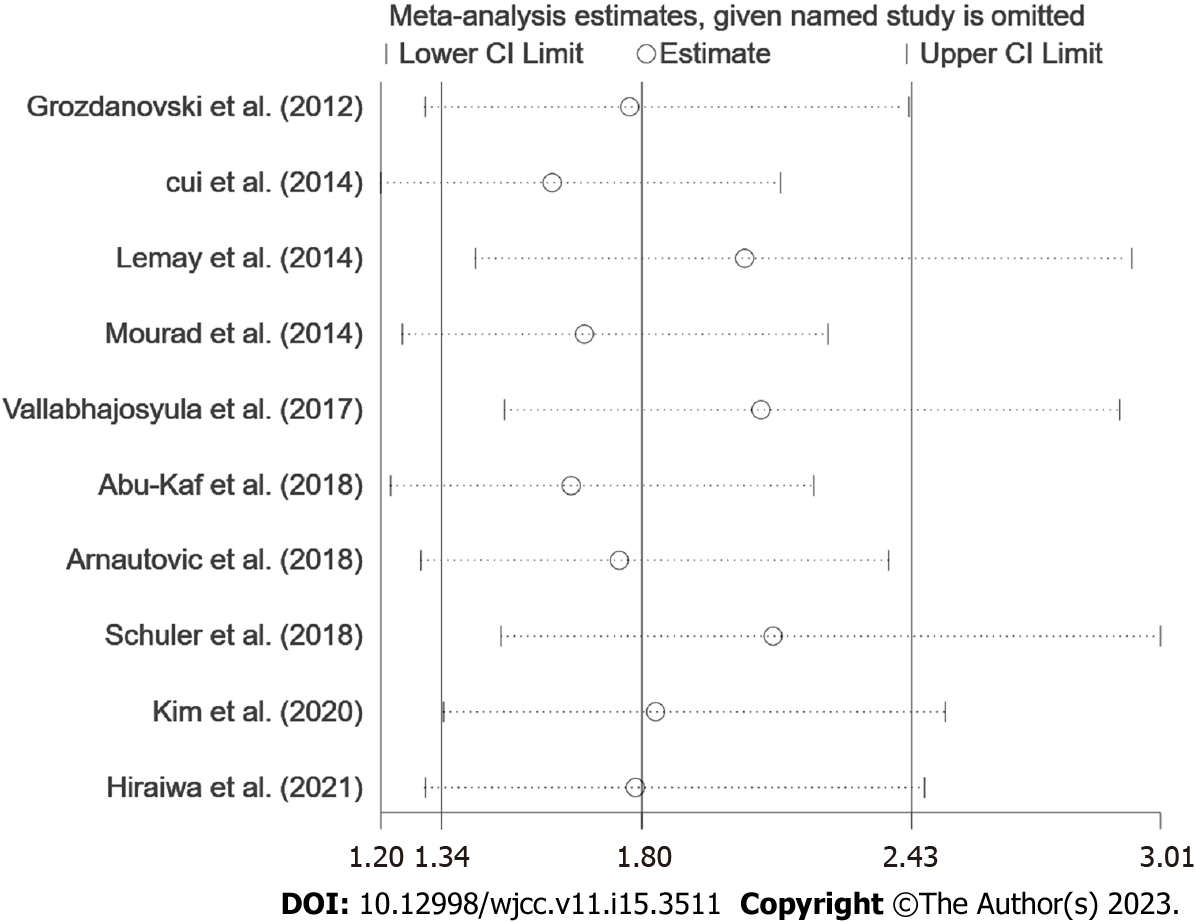
Meta-regression analysis showed that three variables may be related to heterogeneity: the average age of patients (P = 0.008), the country where the research was conducted (P = 0.034), and the number of HF cases (P = 0.021). Sensitivity analysis was used to assess heterogeneity between studies. We sequentially excluded each study to examine the impact of individual studies on estimates of heterogeneity and overall effects (Figure 3). It was found that the study with a large number of cases had a certain impact on the heterogeneity of results[11]. After exclusion of this study[11], the combined OR of mortality in the other studies increased to 2.11 (95%CI: 1.48-3.01; P < 0.001), and heterogeneity decreased (I2 = 85.4%, Ph < 0.001).
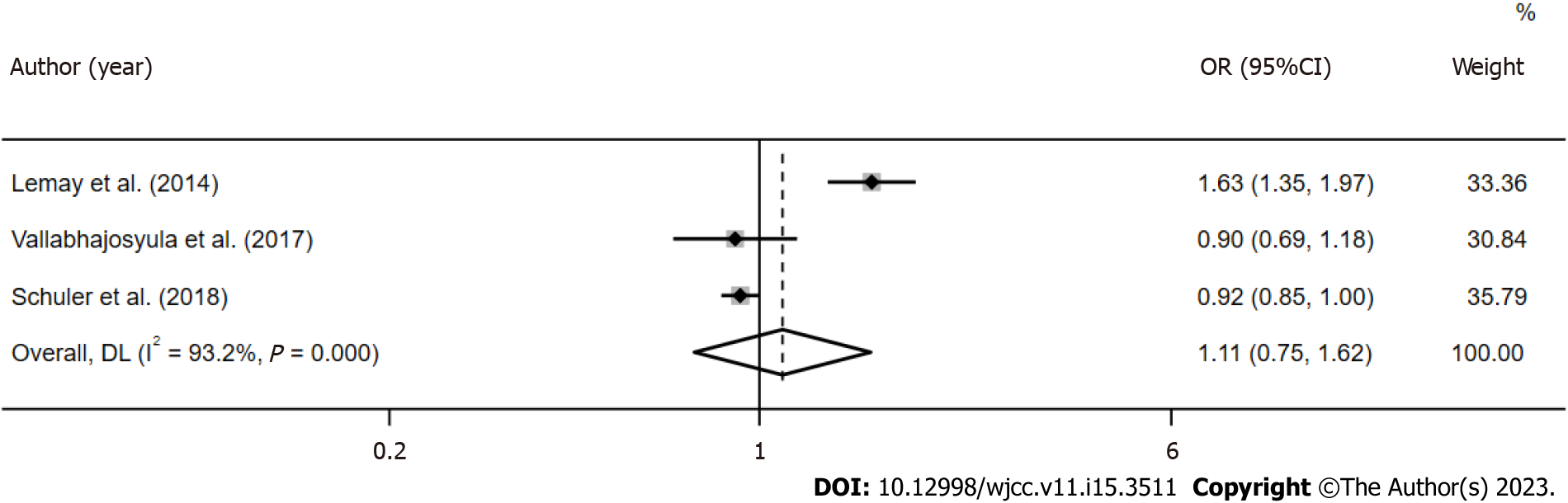
Three studies (33278 patients) reported 1-year mortality data for sepsis patients with HF[4,11,12], and the combined OR was 1.11 (95%CI: 0.75-1.62; P > 0.05; Figure 4). Three studies (1710 patients) reported mortality due to isolated right ventricular (RV) dysfunction with a combined OR of 2.32 (95%CI: 1.29-4.14; P < 0.001; Figure 5)[12,22,23].
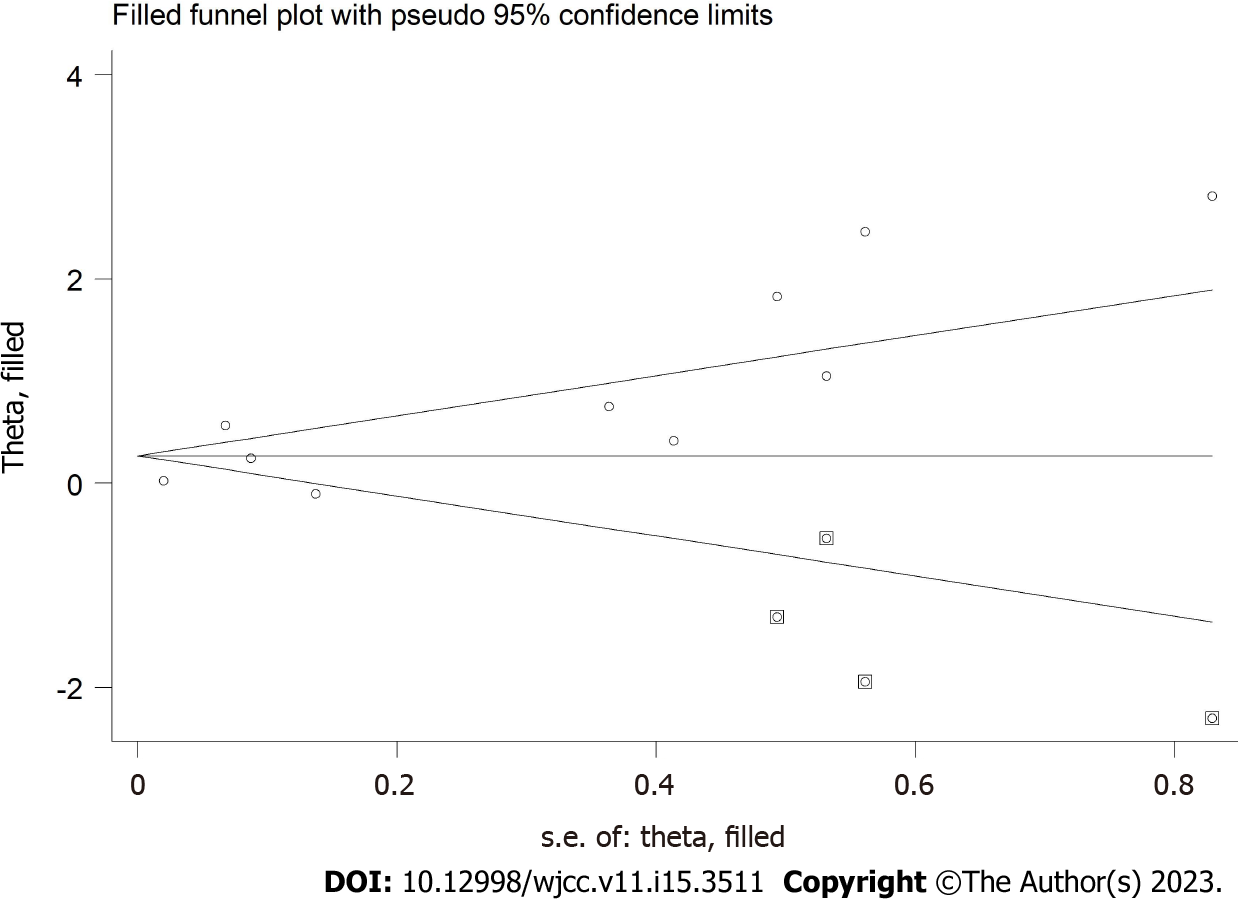
Begg and Egger's tests were conducted to assess publication bias. The mortality of sepsis patients with HF was found to be significantly biased (Begg P = 0.371 and Egger P = 0.017). Therefore, the trim-and-fill method revealed the evidence of four missing studies (Figure 6). If the four potentially missing studies were included, the combined outcome OR of the effect index was 1.306 (95%CI: 0.975-1.749; P > 0.05), this result was not statistically significant and differed from previous results. Therefore, this analysis suggests that our study may have overestimated the effect of HF on mortality in patients with sepsis; thus, it deserves further study.
Sepsis and HF are common complications in critically ill patients, often resulting in additional complex pathological conditions[24]. The results related to sepsis with HF remain inconsistent. Therefore, we conducted a meta-analysis of all relevant studies to better understand the role of HF in the prognosis of sepsis patients. In this systematic review and meta-analysis, 35712 sepsis patients were included. Sepsis mortality risk in patients with HF was significantly increased, indicating that HF may be a risk factor in the clinical process of sepsis.
Our meta-analysis is the first to report pooled estimates of mortality in sepsis patients with HF, which adds to existing evidence on the impact of HF on sepsis outcomes[13]. HF, is an increasingly global epidemic, and has a high incidence rate and mortality[25]. According to the research published by Logeart et al[26] more than a quarter of patients with acute HF are caused by infection. The treatment strategies for sepsis and HF are contradictory, and the treatment plan and severity of the disease may affect the prognosis[27]. Chronic HF has been studied as an independent risk factor for mortality in patients with severe sepsis and septic shock[15]. However, given the current controversy in related studies, we can only draw a cautious conclusion regarding the association between HF and poor outcomes during sepsis.
HF in sepsis can be understood as insufficient cardiac output and oxygen delivery caused by cardiac dysfunction. RV dysfunction can lead to decreased venous return, and left ventricular (LV) diastolic dysfunction may induce impaired LV preload[28]. Septic myocardial dysfunction described in several reviews is increasingly recognized as a major factor in septic shock outcomes[29-31]. The prognosis and therapeutic significance of physiological abnormalities in sepsis-induced myocardial dysfunction remain uncertain[32]. In a study of the impact of ventricular dysfunction on the prognosis of sepsis patients, it was found that RV dysfunction is associated with an increased risk of death[12,22,23]; Isolated RV dysfunction is an independent predictor of 28-day mortality[22], and LV systolic dysfunction is not related to prognosis[23]. In an 8-year study, compared with the control group, the short-term and long-term outcomes of patients with LV dysfunction in severe sepsis/septic shock did not differ and did not increase the risk of long-term adverse HF outcomes[33]. A single center retrospective study showed that clinical outcomes were not different between septic patients with pre-existing LV dysfunction and those without LV dysfunction[34]. LV dilation was associated with lower mortality in a related study[35], but it also depended on the influence of load state, fluid condition or vasoactive drugs. Myocardial insufficiency in sepsis patients and its impact on prognosis still need to be prospectively studied in large sample multicenter trials.
Winters et al[36] conducted a retrospective study and found that the 1-year mortality rate was 7%-43% in patients with sepsis. Septic patients have an ongoing mortality risk beyond short-term end points, and the quality of life in survivors who suffer consistently is impaired. Subgroup analysis showed that HF had an impact on the prognosis of sepsis patients in hospital and on 28-day mortality. Lemay et al[4] found that HF was significantly associated with increased long-term mortality in survivors of severe sepsis. However, when the one-year mortality rate in this meta-analysis was aggregated, HF did not affect the long-term prognosis of sepsis patients. It has been shown that HF is the most common comorbidity in sepsis; moreover, dysfunction of three or more organs is an important independent risk factor for death in patients with severe sepsis and septic shock[37]. Considering the heterogeneity of research results in different backgrounds, the dubious relationship between sepsis and poor prognosis of HF is still unclear, and further reliable prospective cohort studies are needed to finally determine the difference between long-term and short-term prognosis, and determine the intervention strategy to prevent poor outcomes.
This meta-analysis has some limitations. Firstly, our research only included English publications, and only 10 studies met the inclusion criteria. The number of studies and sample size are relatively small. Secondly, we observed marked heterogeneity among the studies and found that the main heterogeneity was due to the age of the study population, different study regions, and the sample size of patients with HF. There may also be other possible sources of heterogeneity, such as the variability of treatment, the severity of complications, and medical conditions. Although it is important to explain these differences in the analysis, we cannot obtain more detailed information due to the inconsistent research methods, reported data types, and the types of HF in the included patients. Thirdly, because not all studies used similar disease severity and disease-related scores, we were unable to adjust these variables. Fourthly, there was obvious publication bias in this study, and our conclusion was reversed through the trim-and-fill method by including missing studies. Thus, our research results lack stability, and further research is needed.
This systematic review and meta-analysis showed that heart failure significantly increased the risk of death in patients with sepsis. However, this conclusion needs to be further verified by more high-quality studies.
Sepsis is one of the main causes of death in the intensive care unit and hospitals. Sepsis patients often have heart failure. However, the impact of heart failure on the mortality of sepsis patients is controversial.
Although the treatment of sepsis has been updated, the effect of heart failure on the outcome of patients with sepsis still requires further study. Understanding whether heart failure, as a comorbidity, will affect the survival of patients with sepsis is significant in order to take appropriate measures to reduce the occurrence of adverse results.
The purpose of our study was to assess whether heart failure increases the mortality of patients with sepsis by collecting existing research evidence.
PubMed, Embase, Web of Science, and Cochrane Library databases from inception to November 9, 2022 were searched to compare the prognosis of sepsis patients with heart failure. The outcome data were summarized in the random effect model using odds ratio (OR) and 95% confidence interval (CI).
Ten studies were included. The results showed that sepsis patients with heart failure were associated with increased total mortality (OR = 1.80, 95%CI: 1.34-2.43; I2 = 92.1%). Heart failure did not increase the 1-year mortality of patients (OR = 1.11, 95%CI: 0.75-1.62; I2 = 93.2%), and the mortality of patients with isolated right ventricular dysfunction (OR = 2.32, 95%CI: 1.29-4.14; I2 = 91.5%) increased significantly.
Contemporary evidence indicates that heart failure significantly increases the risk of death in patients with sepsis, especially right ventricular dysfunction.
Sepsis patients with heart failure should receive highly monitored treatment, and more high-quality related research is needed.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Infectious diseases
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ghimire R, Nepal; Moldovan CA, Romania S-Editor: Ma YJ L-Editor: A P-Editor: Yuan YY
| 1. | Napolitano LM. Sepsis 2018: Definitions and Guideline Changes. Surg Infect (Larchmt). 2018;19:117-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 173] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 2. | Vincent JL, Marshall JC, Namendys-Silva SA, François B, Martin-Loeches I, Lipman J, Reinhart K, Antonelli M, Pickkers P, Njimi H, Jimenez E, Sakr Y; ICON investigators. Assessment of the worldwide burden of critical illness: the intensive care over nations (ICON) audit. Lancet Respir Med. 2014;2:380-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 606] [Cited by in RCA: 841] [Article Influence: 76.5] [Reference Citation Analysis (0)] |
| 3. | Pool R, Gomez H, Kellum JA. Mechanisms of Organ Dysfunction in Sepsis. Crit Care Clin. 2018;34:63-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 173] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 4. | Lemay AC, Anzueto A, Restrepo MI, Mortensen EM. Predictors of long-term mortality after severe sepsis in the elderly. Am J Med Sci. 2014;347:282-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 50] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 5. | Jones TW, Smith SE, Van Tuyl JS, Newsome AS. Sepsis With Preexisting Heart Failure: Management of Confounding Clinical Features. J Intensive Care Med. 2021;36:989-1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (1)] |
| 6. | Arnautovic J, Mazhar A, Souther B, Mikhijan G, Boura J, Huda N. Cardiovascular Factors Associated with Septic Shock Mortality Risks. Spartan Med Res J. 2018;3:6516. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (1)] |
| 7. | Hajj J, Blaine N, Salavaci J, Jacoby D. The "Centrality of Sepsis": A Review on Incidence, Mortality, and Cost of Care. Healthcare (Basel). 2018;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 90] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 8. | Walker AMN, Drozd M, Hall M, Patel PA, Paton M, Lowry J, Gierula J, Byrom R, Kearney L, Sapsford RJ, Witte KK, Kearney MT, Cubbon RM. Prevalence and Predictors of Sepsis Death in Patients With Chronic Heart Failure and Reduced Left Ventricular Ejection Fraction. J Am Heart Assoc. 2018;7:e009684. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 61] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 9. | Cui Y, Wang T, Bao J, Tian Z, Lin Z, Chen D. Comparison of Charlson's weighted index of comorbidities with the chronic health score for the prediction of mortality in septic patients. Chin Med J (Engl). 2014;127:2623-2627. [PubMed] |
| 10. | Arfaras-Melainis A, Polyzogopoulou E, Triposkiadis F, Xanthopoulos A, Ikonomidis I, Mebazaa A, Parissis J. Heart failure and sepsis: practical recommendations for the optimal management. Heart Fail Rev. 2020;25:183-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 57] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 11. | Schuler A, Wulf DA, Lu Y, Iwashyna TJ, Escobar GJ, Shah NH, Liu VX. The Impact of Acute Organ Dysfunction on Long-Term Survival in Sepsis. Crit Care Med. 2018;46:843-849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 110] [Article Influence: 18.3] [Reference Citation Analysis (1)] |
| 12. | Vallabhajosyula S, Kumar M, Pandompatam G, Sakhuja A, Kashyap R, Kashani K, Gajic O, Geske JB, Jentzer JC. Prognostic impact of isolated right ventricular dysfunction in sepsis and septic shock: an 8-year historical cohort study. Ann Intensive Care. 2017;7:94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 90] [Cited by in RCA: 124] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 13. | Sevilla Berrios RA, O'Horo JC, Velagapudi V, Pulido JN. Correlation of left ventricular systolic dysfunction determined by low ejection fraction and 30-day mortality in patients with severe sepsis and septic shock: a systematic review and meta-analysis. J Crit Care. 2014;29:495-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 101] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 14. | Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44932] [Cited by in RCA: 40626] [Article Influence: 10156.5] [Reference Citation Analysis (2)] |
| 15. | Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39087] [Cited by in RCA: 46553] [Article Influence: 2116.0] [Reference Citation Analysis (3)] |
| 16. | Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34245] [Cited by in RCA: 40570] [Article Influence: 1448.9] [Reference Citation Analysis (2)] |
| 17. | Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088-1101. [PubMed] |
| 18. | Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7948] [Cited by in RCA: 9100] [Article Influence: 364.0] [Reference Citation Analysis (0)] |
| 19. | Grozdanovski K, Milenkovic Z, Demiri I, Spasovska K, Cvetanovska M, Kirova-Urosevic V. Early prognosis in patients with community-acquired severe sepsis and septic shock: analysis of 184 consecutive cases. Prilozi. 2012;33:105-116. [PubMed] |
| 20. | Mourad M, Chow-Chine L, Faucher M, Sannini A, Brun JP, de Guibert JM, Fouche L, Lambert J, Blache JL, Mokart D. Early diastolic dysfunction is associated with intensive care unit mortality in cancer patients presenting with septic shock. Br J Anaesth. 2014;112:102-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 21. | Abu-Kaf H, Mizrakli Y, Novack V, Dreiher J. Long-Term Survival of Young Patients Surviving ICU Admission With Severe Sepsis. Crit Care Med. 2018;46:1269-1275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 22. | Kim JS, Kim YJ, Kim M, Ryoo SM, Kim WY. Association between right ventricle dysfunction and poor outcome in patients with septic shock. Heart. 2020;106:1665-1671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 23. | Hiraiwa H, Kasugai D, Ozaki M, Goto Y, Jingushi N, Higashi M, Nishida K, Kondo T, Furusawa K, Morimoto R, Okumura T, Matsuda N, Matsui S, Murohara T. Clinical impact of visually assessed right ventricular dysfunction in patients with septic shock. Sci Rep. 2021;11:18823. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 24. | Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:801-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15803] [Cited by in RCA: 17221] [Article Influence: 1913.4] [Reference Citation Analysis (2)] |
| 25. | Gupta AK, Tomasoni D, Sidhu K, Metra M, Ezekowitz JA. Evidence-Based Management of Acute Heart Failure. Can J Cardiol. 2021;37:621-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 26. | Logeart D, Isnard R, Resche-Rigon M, Seronde MF, de Groote P, Jondeau G, Galinier M, Mulak G, Donal E, Delahaye F, Juilliere Y, Damy T, Jourdain P, Bauer F, Eicher JC, Neuder Y, Trochu JN; Heart Failure of the French Society of Cardiology. Current aspects of the spectrum of acute heart failure syndromes in a real-life setting: the OFICA study. Eur J Heart Fail. 2013;15:465-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 115] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 27. | Zhang B, Guo S, Fu Z, Wu N, Liu Z. Association between fluid balance and mortality for heart failure and sepsis: a propensity score-matching analysis. BMC Anesthesiol. 2022;22:324. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 28. | Vieillard-Baron A, Cecconi M. Understanding cardiac failure in sepsis. Intensive Care Med. 2014;40:1560-1563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 29. | Kakihana Y, Ito T, Nakahara M, Yamaguchi K, Yasuda T. Sepsis-induced myocardial dysfunction: pathophysiology and management. J Intensive Care. 2016;4:22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 205] [Cited by in RCA: 352] [Article Influence: 39.1] [Reference Citation Analysis (0)] |
| 30. | Lv X, Wang H. Pathophysiology of sepsis-induced myocardial dysfunction. Mil Med Res. 2016;3:30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 111] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 31. | Walley KR. Sepsis-induced myocardial dysfunction. Curr Opin Crit Care. 2018;24:292-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 113] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 32. | Hollenberg SM, Singer M. Pathophysiology of sepsis-induced cardiomyopathy. Nat Rev Cardiol. 2021;18:424-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 382] [Article Influence: 95.5] [Reference Citation Analysis (0)] |
| 33. | Vallabhajosyula S, Jentzer JC, Geske JB, Kumar M, Sakhuja A, Singhal A, Poterucha JT, Kashani K, Murphy JG, Gajic O, Kashyap R. New-Onset Heart Failure and Mortality in Hospital Survivors of Sepsis-Related Left Ventricular Dysfunction. Shock. 2018;49:144-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 66] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 34. | Ouellette DR, Shah SZ. Comparison of outcomes from sepsis between patients with and without pre-existing left ventricular dysfunction: a case-control analysis. Crit Care. 2014;18:R79. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 35. | Huang SJ, Nalos M, McLean AS. Is early ventricular dysfunction or dilatation associated with lower mortality rate in adult severe sepsis and septic shock? A meta-analysis. Crit Care. 2013;17:R96. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 102] [Cited by in RCA: 139] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 36. | Winters BD, Eberlein M, Leung J, Needham DM, Pronovost PJ, Sevransky JE. Long-term mortality and quality of life in sepsis: a systematic review. Crit Care Med. 2010;38:1276-1283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 492] [Cited by in RCA: 448] [Article Influence: 29.9] [Reference Citation Analysis (0)] |
| 37. | Grozdanovski K, Milenkovic Z, Demiri I, Spasovska K. Prediction of outcome from community-acquired severe sepsis and septic shock in tertiary-care university hospital in a developing country. Crit Care Res Pract. 2012;2012:182324. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |