Published online May 16, 2023. doi: 10.12998/wjcc.v11.i14.3356
Peer-review started: March 2, 2023
First decision: March 24, 2023
Revised: April 2, 2023
Accepted: April 7, 2023
Article in press: April 7, 2023
Published online: May 16, 2023
Processing time: 74 Days and 18.8 Hours
Bladder metastasis from lung cancer with epidermal growth factor receptor (EGFR) mutation is extremely rare. Here, we report a case of bladder metastasis from lung adenocarcinoma with EGFR mutation.
A 53-year-old female patient was diagnosed with advanced lung adenocarcinoma with EGFR exon 19 deletion. Multiple nodules on the bladder wall were found by regular examination of the pelvic cavity through computed tomography during targeted therapy. Further cystoscopy and histological examination of bladder biopsy tissues confirmed the bladder metastasis from lung adenocarcinoma. In addition, genetic analysis of the bladder metastasis revealed EGFR T790M mutation. The patient achieved a good response to a third-generation EGFR tyrosine kinase inhibitor.
During routine follow-up of lung cancer patients, imaging examination of the pelvic cavity should be performed to avoid missing bladder metastasis. The ultimate diagnosis of bladder metastasis sill depends on the pathological result of biopsy tissues.
Core Tip: Bladder metastasis from lung cancer with epidermal growth factor receptor (EGFR) mutation is extremely rare. We reported a case of bladder metastasis from lung adenocarcinoma with EGFR mutation. During routine follow-up of lung cancer patients, imaging examination of the pelvic cavity should be performed to avoid missing bladder metastasis. The ultimate diagnosis of bladder metastasis sill depends on the pathological result of biopsy tissues as determined by cystoscopy. Bladder metastasis with EGFR mutation seems to respond well to the treatment of EGFR tyrosine kinase inhibitors.
- Citation: Jin CB, Yang L. Bladder metastasis from epidermal growth factor receptor mutant lung cancer: A case report. World J Clin Cases 2023; 11(14): 3356-3361
- URL: https://www.wjgnet.com/2307-8960/full/v11/i14/3356.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i14.3356
Bladder cancer is one of the most common urinary carcinomas, only a small percentage of which are metastases from a distant primary cancer. Previous studies have shown that the primary tumors with bladder metastases could originate from stomach, melanoma, breast and lung[1]. In addition, lung cancer with bladder metastasis is especially rare. Here, we described a case of bladder metastasis from lung adenocarcinoma that was found during targeted therapy by accident. In particular, genetic analysis of the bladder metastasis tissue showed epidermal growth factor receptor (EGFR) exon 19 deletion and exon 20 T790M mutation.
A lung cancer patient returned to the hospital for re-examination with a complaint of significant loss of appetite during targeted therapy.
Significant loss of appetite started one month before the patient’s return to the hospital.
In April 2019, a 53-year-old woman went to the hospital with pain in the left leg and was found to have a pulmonary nodule. Positron Emission Tomography-Computed Tomography showed a solid mass in the upper lobe of the left lung, multiple small nodules in the bilateral lungs and bone destruction in the left ischium and femur. Brain magnetic resonance imaging revealed multiple nodules in the left temporal lobe and cerebellum. The pathological diagnosis based on the left lung mass biopsy sample was adenocarcinoma. Genetic analysis of the biopsy tissue revealed EGFR exon 19 deletion. The first-generation EGFR tyrosine kinase inhibitor icotinib was administered. The patient achieved stable disease, but clinical symptoms did not improve significantly. A chemotherapy regimen (pemetrexed) was administered for two cycles simultaneously during targeted therapy in July 2019. Until January 2022, the patient continued to show significant loss of appetite.
The patient denied any family history of malignant tumors.
Her vital signs were as follows: Body temperature, 36.6℃; blood pressure, 120/80 mmHg; heart rate, 85 beats per min; respiratory rate, 20 breaths per min. Furthermore, there was no positive signs related to the disease.
Levels of serum tumor markers were as follows: Carcinoembryonic antigen, 263 ng/mL; carbohydrate antigen 125, 64.5 U/mL; squamous cell carcinoma antigen, 0.99 ng/mL. No abnormality was found in routine blood and urine analyses.
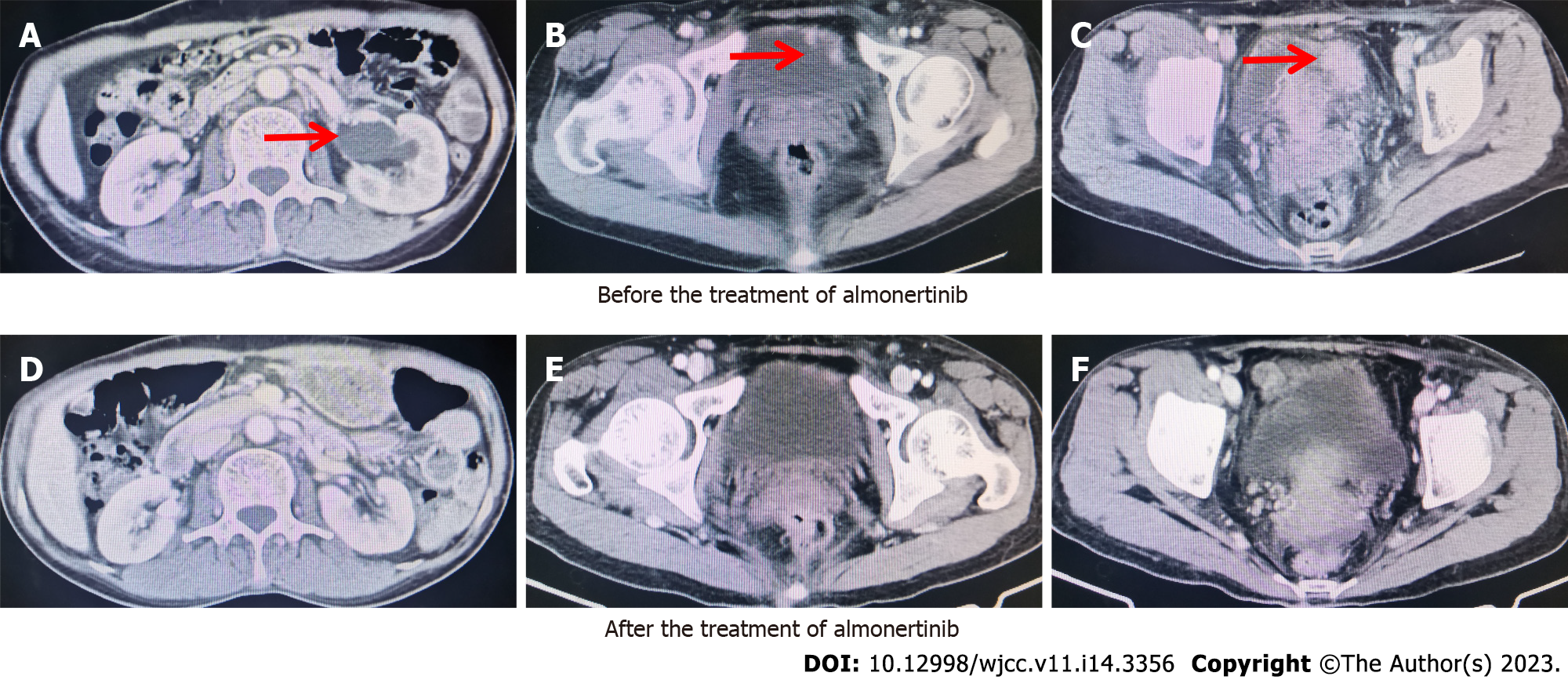
Examination of the chest, abdomen and pelvic cavity through computed tomography revealed multiple nodules on the bladder wall (Figure 1). The lesions of the lung and brain were stable.
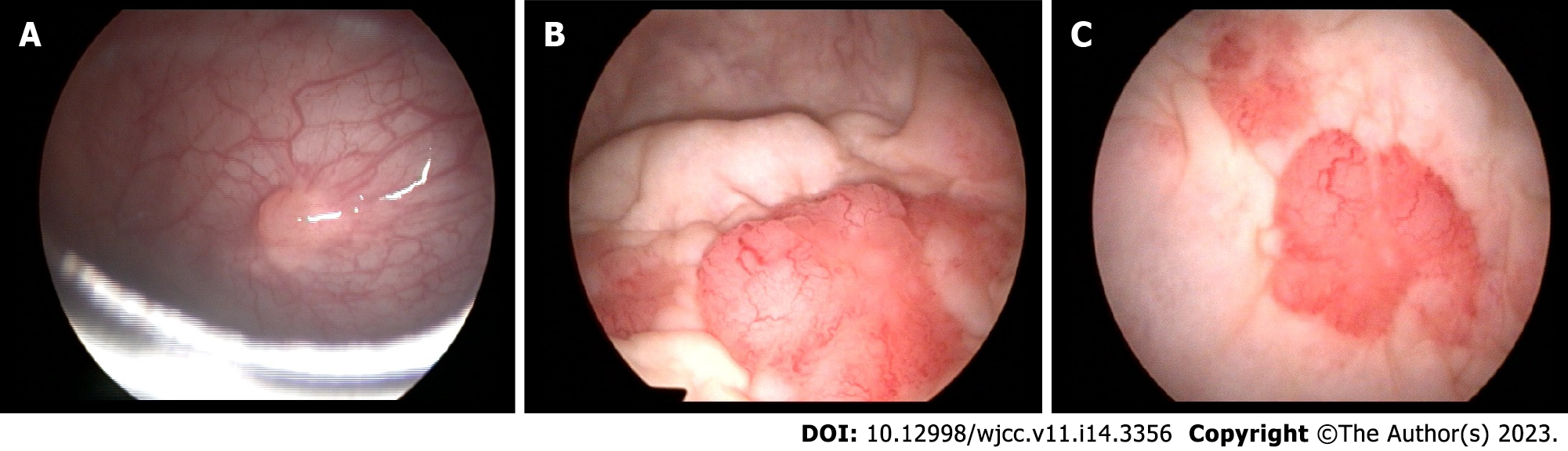
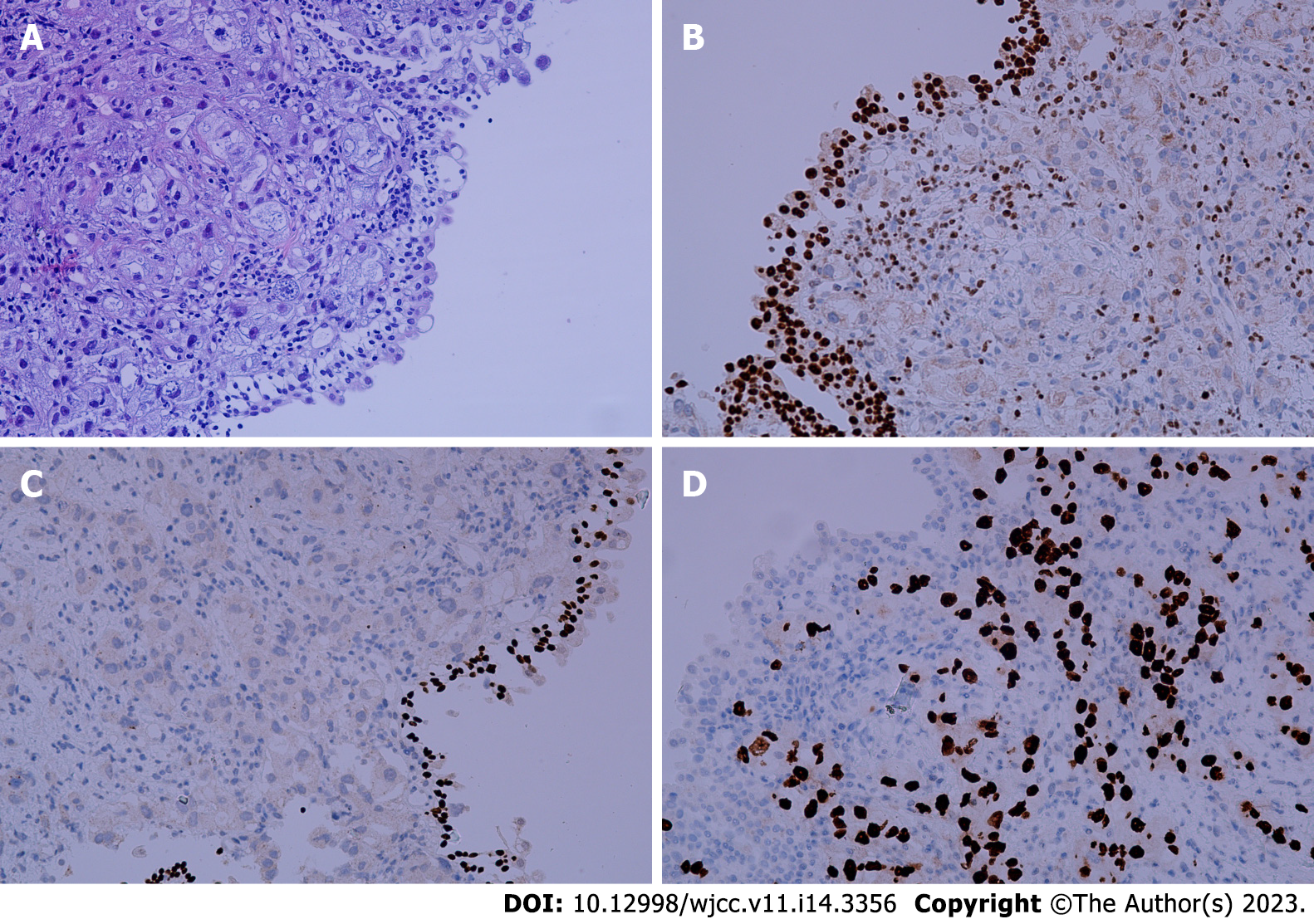
To determine the origin of the nodules on the bladder wall, cystoscopic examination was subsequently performed. The cystoscopy analysis revealed multiple solid lesions on the anterior and bottom walls of the bladder (Figure 2). Bladder lesion biopsy was performed, and histological examination showed that the sample was a bladder metastasis derived from lung adenocarcinoma. Immunohistochemistry analysis showed positive staining for TTF-1 and CK7 and negative staining for P40 and GATA3 (Figure 3). Furthermore, genetic analysis of the mass biopsy showed EGFR exon 19 deletion and exon 20 T790M mutation.
Given the above findings combined with the patient’s medical history, the final diagnosis was bladder metastasis derived from lung adenocarcinoma with EGFR exon 19 deletion and exon 20 T790M mutation.
In February 2022, the patient began to receive targeted therapy with the third-generation EGFR tyrosine kinase inhibitor almonertinib and achieved a partial response.
One year after the treatment with almonertinib, the patient had sustained partial remission. There were no obvious adverse events.
Lung cancer is the most common cancer in males worldwide and the most frequent cause of cancer-related death. The main hematogenous metastatic sites for lung cancer are the bone, brain, liver, and adrenal glands. Metastasis in the bladder, which is an uncommon distant metastatic site, has been reported in only a few cases thus far. According to the timing of occurrence, bladder metastasis can be divided into two types: synchronous and metachronous metastasis. Synchronous bladder metastasis is mostly found during examinations of the primary site. For the metachronous type, the mean time from the diagnosis of lung cancer to the occurrence of bladder metastasis is one year[2]. In our case, bladder metastasis occurred thirty-three months after the initial diagnosis of lung cancer.
For primary bladder cancer, a common clinical manifestation is macroscopic hematuria at diagnosis. Macroscopic hematuria is also a late-stage manifestation of bladder metastasis, as malignant cells must infiltrate the bladder lining. In addition to hematuria, hydronephrosis is another common symptom that can present in combination with hematuria. In addition, other symptoms, such as pelvic pain and dysuria, can also suggest the possibility of bladder metastasis of lung cancers. In our case, the patient had no typical symptoms related to bladder metastasis. However, left hydronephrosis was seen on imaging examination, which disappeared after effective targeted therapy.
During routine follow up of lung cancer patients, the examination of the pelvic cavity through computed tomography or magnetic resonance imaging should be performed to avoid overlooking bladder metastasis. The definite diagnosis is based on pathological examination of the bladder biopsy tissues.
Cystoscopy plays an important role in the diagnosis of bladder tumors. Some studies have indicated that bladder metastasis is likely to be isolated, while primary bladder tumors are frequently found in multiples. In our case, multiple lesions were found on cystoscopy. According to the previous cases, a common location of bladder metastasis is the lateral walls of the bladder[2]. Because of the route of blood circulation, bladder metastases are usually located in the lamina propria or muscularis propria of the bladder wall, while primary bladder tumors often originate from the mucosa. In our case, multiple bladder metastases were found on the anterior and bottom walls of the bladder.
Primary bladder cancer cases mostly include urothelial carcinoma. According to previously reported cases, the most common pathological type of bladder metastasis from lung cancer is adenocarcinoma[2]. Confirmed diagnosis of bladder tumors depends on immunohistochemistry analysis of biopsy tissues. In our case, the immunohistochemistry analysis showed positive staining for TTF-1 and CK7 and negative staining for P40 and GATA3. The marker CK-7 represents epithelial origin and thus cannot distinguish between lung and bladder cells. The marker GATA3 suggests urothelial differentiation and thus helped eliminate the possibility of urothelial origin. The positive TTF-1 staining suggested that the primary lung adenocarcinoma was the origin with high sensitivity and specificity. Therefore, we confirmed the diagnosis of bladder metastasis from lung cancer by combined analysis of these markers.
In previously published case reports, there were only two cases mentioning the gene mutation status of the lung cancer[3,4]. Both lung cancer patients with bladder metastasis had sensitive EGFR mutations and lacked the T790M mutation before and after the treatment with targeted therapy or chemotherapy. However, in our case, the T790M mutation was detected using bladder biopsy tissue after the progression on first-line targeted therapy. Moreover, the bladder metastasis responded well to targeted therapy with third-generation EGFR tyrosine kinase inhibitors. Due to the limited reported cases and available information, no correlation between the clinical characteristics of lung cancer patients and the occurrence of bladder metastasis has been found until now.
Bladder metastasis from lung cancer with EGFR mutation is extremely rare. During routine follow-up of lung cancer patients, imaging examination of the pelvic cavity should be performed to avoid missing bladder metastasis. The ultimate diagnosis of bladder metastasis sill depends on the pathological result of biopsy tissues as determined by cystoscopy. Bladder metastasis with EGFR mutation seems to respond well to the treatment of EGFR tyrosine kinase inhibitors.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Konala VM, United States; Sehrawat A, India S-Editor: Ma YJ L-Editor: A P-Editor: Yuan YY
| 1. | Zaghbib S, Chakroun M, Saadi A, Boussaffa H, Znaidi N, Rammeh S, Ayed H, Chebil M. Isolated bladder metastasis from lung adenocarcinoma: a case report. J Surg Case Rep. 2021;rjab195. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 2. | Sanguedolce F, Loizzi D, Sollitto F, Di Bisceglie M, Lucarelli G, Carrieri G, Bufo P, Cormio L. Bladder Metastases from Lung Cancer: Clinical and Pathological Implications: A Systematic Review. Oncology. 2017;92:125-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Li X, Zhang L, Zeng L, Wang X, Song W, Zhong D. Difficult differential diagnosis of bladder pedicled masses about metastasis from non-small cell lung cancer: A case report. Cancer Biol Ther. 2021;22:106-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Kuga T, Machida K, Ito H, Matsuo M. Bilateral Hydronephrotic Bladder Metastasis from Lung Cancer. Intern Med. 2018;57:1801. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |