Published online May 16, 2023. doi: 10.12998/wjcc.v11.i14.3261
Peer-review started: November 28, 2022
First decision: February 7, 2023
Revised: February 15, 2023
Accepted: April 10, 2023
Article in press: April 10, 2023
Published online: May 16, 2023
Processing time: 169 Days and 1.6 Hours
Primary seminal vesicle adenocarcinoma is a rare malignancy that is difficult to diagnose.
A 54-year-old man with an 18-year history of a seminal vesicle cyst presented with worsening hematospermia that had persisted for one month. Dynamic contrast-enhanced computed tomography and pelvic magnetic resonance imaging indicated a mass with a cystic-solid component. Robot-assisted seminal vesicle tumor resection was performed, and primary seminal vesicle adenocarcinoma was confirmed pathologically. The patient received pelvic radiotherapy for six weeks, and to date, no evidence of recurrence has been found.
Seminal vesicle cysts should be monitored long-term. Seminal vesicle adenocarcinoma presents with non-specific symptoms and can be diagnosed by immunohistochemistry.
Core Tip: Primary seminal vesicle adenocarcinoma with a long history of seminal vesicle cyst has rarely been reported. Primary seminal vesicle adenocarcinoma is a rare malignancy that is difficult to diagnose. Herein, we present a case of pathologically confirmed primary adenocarcinoma of seminal vesicle with a long history of seminal vesicle cyst.
- Citation: Yao Y, Liu S, He YL, Luo L, Zhang GM. Primary seminal vesicle adenocarcinoma with a history of seminal vesicle cyst: A case report and review of literature. World J Clin Cases 2023; 11(14): 3261-3266
- URL: https://www.wjgnet.com/2307-8960/full/v11/i14/3261.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i14.3261
Adenocarcinoma of the seminal vesicle is an extremely rare tumor of the genitourinary system[1]. The early stage of the disease is often asymptomatic and is not easily detected and diagnosed. Seminal vesicle cyst combined with seminal vesicle carcinoma has been reported in a few cases[2-4]. However, adenocarcinoma of the seminal vesicle with a long history of seminal vesicle cysts has not been reported. When symptoms such as hematuria, hematospermia, or localized pain occur, it often means advanced or progressing disease with prostate or lung metastases, leading to a poor prognosis[5]. Notably, metastatic cancer of the seminal vesicles due to metastases from primary prostate, bladder, or rectal cancer invasion is more common; therefore, these conditions should be carefully differentiated[6,7].
Owing to the rarity of seminal vesicle adenocarcinoma, there are no unified guidelines for treatment. Currently, the optimal treatment is radical resection[8]; however, because of the complex anatomy and the small space around the seminal vesicles and the proximity to the rectum, surgical resection is difficult[9]. Robot-assisted surgery, which has the advantages of fine operation and full exposure of the surgical field, is becoming more popular in the field of urology and appears to be more suitable for seminal vesicle tumors than other surgical approaches[10]. Chemotherapy, radiation, and hormonal therapy have been reported for the adjuvant treatment of seminal vesicle adenocarcinoma[2,5]. We report a case of primary seminal vesicle adenocarcinoma with a long history of seminal vesicle cyst resected by Da Vinci robot-assisted surgery.
A 54-year-old man presented to our outpatient clinic with a history of a seminal vesicle cyst found on physical examination 18 years previously.
The patient’s symptoms started 18 years ago with a seminal vesicle cyst found on physical examination. The patient reported occasional hematospermia, hematuria, and perineal discomfort. His symptoms worsened one month prior to presentation.
When first identified, the seminal vesicle cyst was treated by unroofing and decompression; however, the cyst recurred. During regular surveillance, magnetic resonance imaging revealed seminal vesicle cyst.
The patient had no personal or family history.
Digital rectal examination revealed no obvious abnormalities.
The prostate specific antigen concentration was within the normal range at 0.587 ng/mL (normal range: 0-4 ng/mL).
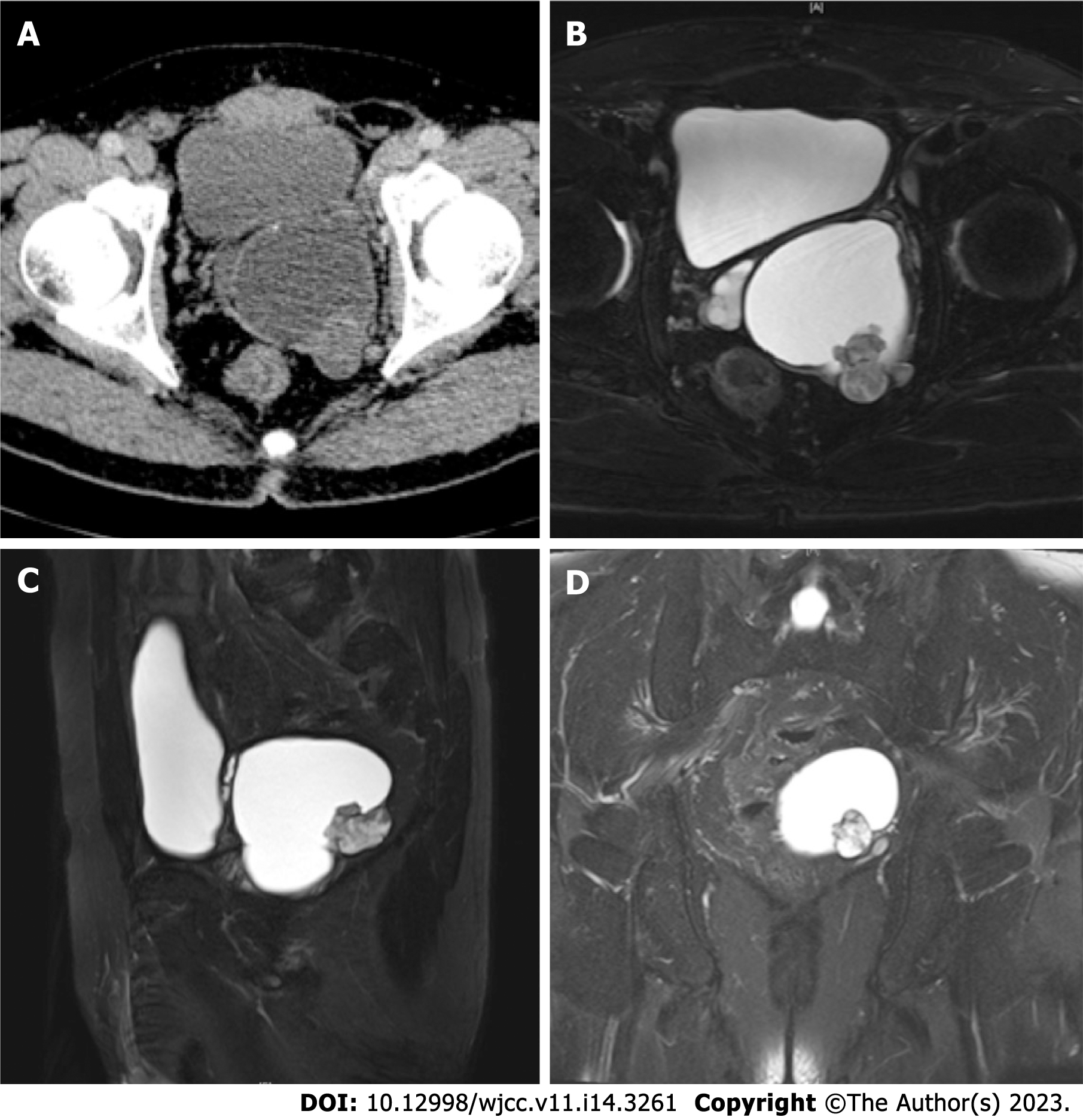
Ultrasonography revealed a 6.9 cm × 5.1 cm × 4.8 cm cystic mass in the left seminal vesicle with a papillary hypoechoic mass in the vesicle wall. Pelvic dynamic contrast-enhanced computed tomography revealed a cystic-solid mass closely related to the seminal vesicles and prostate with an enhancing solid component (Figure 1A). Pelvic magnetic resonance imaging demonstrated a cystic-solid component mass (Figures 1B-D).
The final diagnosis of the present case was primary seminal vesicle adenocarcinoma.
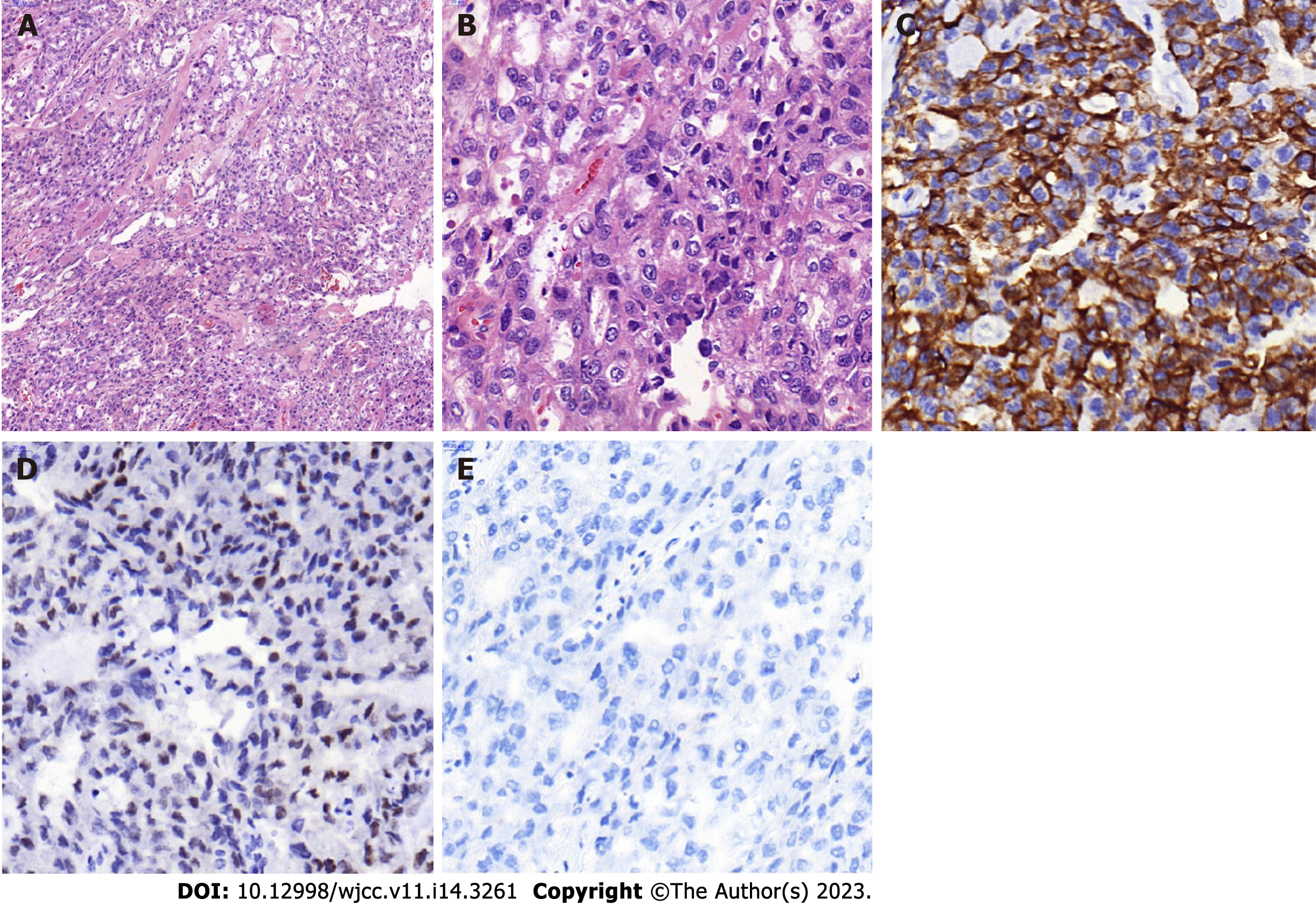
Robot-assisted seminal vesicle tumor resection was performed. A 7 cm light brown cystic mass was seen and was completely removed along with the left seminal vesicle after aspiration of the cystic fluid. A 2 cm × 1.5 cm nodular thickening was seen in the wall of the capsule, and the mass was grayish-white in cross-section. Postoperative pathology revealed that the tumor cells grew in a blister-like, solid, sieve-like, and papillary pattern, with necrosis, and some cells showed a boot-nail-like pattern (Figures 2A and B). The tumor cells invaded beyond the muscle into the extra-muscular tissue and nerves. The tumor did not involve the resection margin. Immunohistochemical staining was positive for cytokeratin (CK)7 (Figure 2C), partially positive for paired-box gene 8 (Figure 2D), and negative for carcinoembryonic antigen, prostate-specific antigen, CK20 (Figure 2E), calretinin, CK5/6, and Wilms’ tumor-1. Considering the tumor morphology and the immunohistochemical results, moderately and poorly differentiated seminal vesicle adenocarcinoma was diagnosed pathologically.
The patient was in stable condition after surgery and was discharged seven days later. Two months after discharge, the patient received radiotherapy at a dose of 66 Gray in 30 fractions for six months. After four months of follow-up, no local recurrence or distant metastasis was found in imaging.
Adenocarcinoma of the seminal vesicle is the most common pathological type of seminal vesicle cancer originating from the lining epithelium of the seminal vesicle. Seminal vesicle adenocarcinoma was first reported in 1925[9]. Thiel and Effert collected and reviewed 52 cases of primary seminal vesicle adenocarcinoma[1]. In the following two decades, few cases were reported. The average age of the patients was 63 years; the youngest was only 19 years old, and the oldest was 90 years old[1].
In our case, the patient had an 18-year history of seminal vesicle cyst, which to our knowledge has not been reported previously. Seminal vesicle cyst is thought to be related to renal dysplasia and is caused by the accumulation of secretions owing to abnormal development of the urogenital tract[4]. Seminal vesicle cysts with renal agenesis have been reported in many cases[2-4,11]. In our case, bilateral kidneys and ureters developed normally. Hematospermia and hematuria are common with seminal vesicle adenocarcinoma[1]. Dysuria is uncommon unless the tumor invades the bladder triangle or is very large[12].
It is difficult to distinguish primary seminal vesicle adenocarcinoma from metastatic seminal vesicle carcinoma. Imaging examination is helpful in making the diagnosis, but the usefulness of this examination is limited. Dalgaard and Giertsen[13] proposed the following diagnostic criteria: Tumor confirmed as carcinoma microscopically and confined to the seminal vesicle; no primary carcinoma in other parts of the body; and preferably, the tumor has a papillary structure similar to that of a non-tumorous seminal vesicle. With developments in imaging technology, targeted core biopsy provides an opportunity for preoperative pathological diagnosis[6,14,15]. However, biopsy of a mass with a cystic component is impractical, and the cyst may be punctured, resulting in leakage of cyst fluid; therefore, biopsy was not performed in this case. With these considerations, it is often difficult to make a diagnosis of seminal vesicle adenocarcinoma preoperatively, and surgical resection is recommended to determine the next step in treatment based on the pathological features.
There are no standardized guidelines for the treatment of seminal vesicle adenocarcinoma, and Bhat et al[2] reported that robot-assisted laparoscopic surgery may be the preferred choice for localized disease. The stable robotic arms and clear magnification, which reveals a fuller field of vision, result in less blood loss, shorter operation times, and shorter hospital stay compared with conventional surgery. The extent of the surgical resection depends on the degree of the tumor invasion to the surrounding tissue[16]. Prostatovesiculectomy with lymph node dissection has been reported in some localized cases because seminal vesicle adenocarcinoma is prone to invade the ejaculatory duct[6,17-19]. In some cases, seminal vesicle resection, only, was performed for localized disease, and no recurrence was observed within five years[2,4]. No recurrence was observed during the follow-up for localized margin-negative disease without adjuvant therapy[4,17,18]. Adjuvant chemotherapy or adjuvant radiotherapy has been reported in some localized margin-negative cases[2,6], but there is insufficient evidence of comparative survival differences with and without adjuvant therapy. In cases of positive margins, adjacent organ infiltration, metastasis, or recurrence, radiotherapy, chemotherapy or anti-androgen therapy has been reported to prolong recurrence-free survival or overall survival[5,9,20-23].
In the past, most seminal vesicle carcinomas were reported to have a poor prognosis, and patients died within two years because most had peripheral infiltration and distant metastasis at the time of diagnosis[1,2,20,24]. Some cases that were detected early and operated early were reported to achieve long-term survival[2,4,17,18].
We report a rare case of seminal vesicle adenocarcinoma with a long history of seminal vesicle cyst. Seminal vesicle cyst has the possibility of malignant transformation. The disease is diagnosed by histopathological and immunohistochemical analysis. We emphasize that seminal vesicle cyst should be followed-up long-term, especially when there are symptoms such as hematospermia and hematuria.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Chaturvedi HTC, India; Koubaa M, Tunisia; Sezer HF, Turkey S-Editor: Wang JJ L-Editor: A P-Editor: Zhang YL
| 1. | Thiel R, Effert P. Primary adenocarcinoma of the seminal vesicles. J Urol. 2002;168:1891-1896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 65] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Bhat A, Banerjee I, Kryvenko ON, Satyanarayana R. Primary seminal vesicle adenocarcinoma: a lethal yet cryptic malignancy with review of literature. BMJ Case Rep. 2019;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Kondo N, Shiono Y, Yoshino Y, Sugaya S, Abe M, Koshitaka Y. [Papillary adenocarcinoma in a seminal vesicle cyst associated with contralateral renal agenesis: a case report]. Hinyokika Kiyo. 2007;53:175-178. [PubMed] |
| 4. | Lee BH, Seo JW, Han YH, Kim YH, Cha SJ. Primary mucinous adenocarcinoma of a seminal vesicle cyst associated with ectopic ureter and ipsilateral renal agenesis: a case report. Korean J Radiol. 2007;8:258-261. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Campobasso D, Fornia S, Ferretti S, Maestroni U, Cortellini P. Primary bilateral seminal vesicle carcinoma: description of a case and literature review. Int J Surg Pathol. 2012;20:633-635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Bhardwaj N, Rastogi P, Attri VS, Bora GS, Gorsi U. Primary seminal vesicle adenocarcinoma: A case report of rare entity and discussion of its differential diagnosis using immunohistochemical approach for the core biopsy specimen. Andrologia. 2020;52:e13512. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Ormsby AH, Haskell R, Jones D, Goldblum JR. Primary seminal vesicle carcinoma: an immunohistochemical analysis of four cases. Mod Pathol. 2000;13:46-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 47] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Navallas M, Vargas HA, Akin O, Pandit-Taskar N, Fine SW, Eastham JA, Hricak H. Primary seminal vesicle adenocarcinoma. Clin Imaging. 2011;35:480-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Yin T, Jiang Y. A 5-year follow-up of primary seminal vesicle adenocarcinoma: A case report. Medicine (Baltimore). 2018;97:e12600. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Poelaert F, Joniau S, Roumeguère T, Ameye F, De Coster G, Dekuyper P, Quackels T, Van Cleynenbreugel B, Van Damme N, Van Eycken E, Mottrie A, Lumen N; Belgian RALP Consortium. Current Management of pT3b Prostate Cancer After Robot-assisted Laparoscopic Prostatectomy. Eur Urol Oncol. 2019;2:110-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Okada Y, Tanaka H, Takeuchi H, Yoshida O. Papillary adenocarcinoma in a seminal vesicle cyst associated with ipsilateral renal agenesis: a case report. J Urol. 1992;148:1543-1545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 38] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Martínez-Peñuela A, Rosario Mercado M, Aldave J, Martínez-Peñuela JM. [Primary adenocarcinoma of the seminal vesicles]. Arch Esp Urol. 2009;62:671-673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Dalgaard JB, Giertsen JC. Primary carcinoma of the seminal vesicle; case and survey. Acta Pathol Microbiol Scand. 1956;39:255-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 58] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Tochigi K, Matsukawa Y, Ishida S, Funahashi Y, Fujita T, Kato M, Gotoh M. A case of primary adenocarcinoma of the seminal vesicle treated by total laparoscopic pelvic exenteration. Aktuelle Urol. 2021;52:50-53. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Angulo JC, Romero I, Cabrera P, González J, Rodríguez-Barbero JM, Núñez-Mora C. [Vesiculectomy with laparoscopic partial prostatectomy in the treatment of primary adenocarcinoma of the seminal vesicle with carcinomatous transformation of the ejaculatory duct]. Actas Urol Esp. 2011;35:304-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Xu X, Bai Y, Shi Z, Gan H. [A case report of primary adenocarcinoma of the seminal vesicle]. Chin J Urol. 2020;41:550-551. [DOI] [Full Text] |
| 17. | Dell'Atti L. Importance of an Early Diagnosis in Primary Adenocarcinoma of the Seminal Vesicle. Rare Tumors. 2016;8:6187. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Möhring C, Bach P, Kosciesza S, Goepel M. [A primary adenocarcinoma of the seminal vesicles. Case report of a rare malignancy]. Urologe A. 2008;47:616-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Smith BA Jr, Webb EA, Price WE. Carcinoma of the seminal vesicle. J Urol. 1967;97:743-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Benson RC Jr, Clark WR, Farrow GM. Carcinoma of the seminal vesicle. J Urol. 1984;132:483-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 84] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 21. | Lal H, Yadav P, Jena R, Jain M. Metastatic primary seminal vesicle adenocarcinoma: management of a rare tumour with multiagent chemotherapy and hormonal therapy. BMJ Case Rep. 2017;2017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Rodriguezkees OS. Clinical improvement following estrogenic therapy in a case of primary adenocarcinoma of the seminal vesicle. J Urol. 1964;91:665-670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 16] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Terrisse S, Camblor ME, Vérine J, Gauthier H, Mongiat-Artus P, Culine S. Primary adenocarcinoma of the seminal vesicle. Rare Tumors. 2017;9:7074. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 24. | Katafigiotis I, Sfoungaristos S, Duvdevani M, Mitsos P, Roumelioti E, Stravodimos K, Anastasiou I, Constantinides CA. Primary adenocarcinoma of the seminal vesicles. A review of the literature. Arch Ital Urol Androl. 2016;88:47-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |