Published online May 16, 2023. doi: 10.12998/wjcc.v11.i14.3238
Peer-review started: March 2, 2023
First decision: March 14, 2023
Revised: March 25, 2023
Accepted: April 7, 2023
Article in press: April 7, 2023
Published online: May 16, 2023
Processing time: 75 Days and 1.2 Hours
Long-term treatment of attention deficit/hyperactivity disorder (ADHD) is associated with adverse events, such as nausea and vomiting, dizziness, and sleep disturbances, and poor maintenance of late ADHD medication compromises treatment outcomes and prolongs the recovery of patients' social functioning.
To evaluate the effect of non-pharmacological treatment on the full recovery of social functioning in patients with ADHD.
A total of 90 patients diagnosed with ADHD between May 2019 and August 2020 were included in the study and randomly assigned to either the pharmacological group (methylphenidate hydrochloride and tomoxetine hydrochloride) or the non-pharmacological group (parental training, behavior modification, sensory integration therapy, and sand tray therapy), with 45 cases in each group. Outcome measures included treatment compliance, Swanson, Nolan, and Pelham, Version IV (SNAP-IV) scores, Conners Parent Symptom Questionnaire (PSQ) scores, and Weiss Functional Impairment Rating Scale (WFIRS) scores.
The non-pharmacological interventions resulted in significantly higher comp
Non-pharmacological interventions, in contrast to the potential risks of adverse events after long-term medication, improve patient treatment compliance, alleviate patients' behavioral symptoms of attention, impulsivity, and hyperactivity, and improve their cognitive ability, thereby improving family relationships and patient self-evaluation.
Core Tip: This study evaluated the effect of non-pharmacological treatments on the full recovery of social functioning in patients with attention deficit hyperactivity disorder (ADHD). A total of 90 patients with ADHD were included in this study. The non-pharmacological intervention resulted in significantly higher patient compliance than the pharmacological treatment group. Patients in the non-pharmacological intervention group also had significantly higher Weiss Functional Impairment Rating Scale scores on family, daily living skills and self-concept than those receiving medication. Thus, non-pharmacological interventions had a positive impact on the overall recovery of social functioning in ADHD patients compared to long-term pharmacological treatment.
- Citation: Lv YB, Cheng W, Wang MH, Wang XM, Hu YL, Lv LQ. Effect of non-pharmacological treatment on the full recovery of social functioning in patients with attention deficit hyperactivity disorder. World J Clin Cases 2023; 11(14): 3238-3247
- URL: https://www.wjgnet.com/2307-8960/full/v11/i14/3238.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i14.3238
Attention deficit hyperactivity disorder (ADHD) is the most common chronic neurodevelopmental disorder in childhood and adolescence[1,2], characterized by age-inappropriate distractibility, reduced attention span, overactivity, and emotional impulsivity regardless of the setting, and associated cognitive impairment, and learning difficulties. The age of onset of ADHD is uncertain, with a prevalence of 6–14 years and a peak of 8-10 years, with a significant gender difference of[3-8]: 1 between males and females. The prevalence of the disease also varies widely, ranging from 1.3% to 13.4%, with a mean prevalence of 3%. According to reports on ADHD, approximately 70% of children with ADHD develop symptoms into adolescence and are at significantly greater risk for disruptive behaviors and emotions than during childhood. The global prevalence of ADHD has been growing in the past decades[1]. Clinical studies reveal that symptoms continue in 70% of ADHD children throughout adolescence and 30% into adults, creating disturbances in family connections[9]. ADHD is a chronic condition with lifelong consequences, often associated with poor academic performance[10], emotional instability[3], and behavioral problems[4].
Studies have shown that long-term treatment of ADHD is associated with adverse events[5], such as nausea, vomiting, dizziness, and sleep disturbances, and poor maintenance of late ADHD medication compromises treatment outcomes and prolongs the recovery of patients' social functioning[11]. The American Academy of Child and Adolescent Psychiatry advises pharmaceutical therapies for ADHD above behavioral treatment alone[6], although the American Academy of Pediatrics favors behavioral interventions, particularly for preschool-aged children[7,12]. However, controversy persists regarding the optimal intervention paradigm for ADHD.
Currently, the treatment of ADHD is mainly pharmacological. Long-term drug use is prone to insomnia, loss of appetite, headache, abdominal pain, or risk of drug dependence. Moreover, pharmacological treatment has a negligible effect on children's deficits in social functioning caused by environmental and psychological factors. In addition to pharmacological treatment, non-pharmacological treatments such as biofeedback therapy, family therapy, and combined medical-educational interventions also constitute an important part of disease management, with more targeted correction of children's behavioral disorders, more lasting and stable improvement of social functions, and higher safety compared with pharmacological treatment. In traditional Chinese medicine (TCM), the disease mainly involves the kidney and the liver, and according to clinical observation, comorbidities from the two organs represent most of the evidence. Kidney deficiency is more prominent among the symptoms of ADHD. TCM focuses on the combination of disease and evidence and coordinates the functions of the internal organs, resulting in significant therapeutic effects.
Thus, exploring the therapeutic effects of non-pharmacological interventions is of great value and long-term significance for patients with ADHD and their families. Therefore, this study investigated the effect of non-pharmacological treatment on the full recovery of social functioning in patients with ADHD.
Children diagnosed with ADHD between May 2019 and August 2020 were assessed for eligibility. After excluding eight cases with discontinued treatment due to adverse events, two cases that revoked their consent, and two cases whose parents refused follow-up visits, 90 ADHD patients (73 males and 17 females, aged 6–18 years) were included in the study. The included patients were randomly assigned to receive either methylphenidate hydrochloride and tomoxetine hydrochloride (pharmacological group) or parental training, behavior modification, sensory integration therapy, and sand tray therapy (non-pharmacological group), with 45 cases in each group.
The randomization was conducted using an online web-based randomization tool (freely available at http://www.randomizer.org/). For concealment of allocation, the randomization procedure and assignment were managed by an independent research assistant who was not involved in the screening or evaluation of the participants.
The original sample size calculation estimated that 45 patients would be needed in each group to detect a 3-point difference between groups using a 2-sided significance test with a power of 0.8 and an alpha error level of 0.05.
The normality of the sample was determined with the Shapiro–Wilk test. Exploratory analyses of descriptive statistical data were performed using the Tukey test. Inferential statistical analysis of quantitative mean data (PES/WES, ISQ, and B.L) was performed using the non-parametric Wilcoxon-Mann–Whitney U-test.
All included patients, or their guardians, provided written informed consent. The study was approved by the ethics committee of our hospital.
All patients met the diagnostic criteria established in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition, regardless of sex. Patients with mental retardation, character disorder, mood disorder, tic disorder, childhood autism, and schizophrenia were excluded.
Hyperactivity and impulsivity: Hyperactivity and impulsivity mostly manifest in early childhood and become obvious in elementary school. The children are hyperactive, talk much in class, and often fight with their classmates.
Inattention: Children have difficulty concentrating when learning and easily respond to external stimuli.
Learning difficulties: Children with normal intelligence have learning difficulties due to the above-mentioned symptoms, and some develop cognitive impairment and general analysis disorder. The onset of the disease is mostly observed before the age of seven and lasts for more than six months.
Dissonant personality or behavioral disorders: Children are more capricious, stubborn, impulsive, lack self-control, and uncomfortable with social interaction. A small number of cases still have personality and behavioral defects in adulthood.
The pharmacological group received methylphenidate hydrochloride extended-release tablets and tomoxetine hydrochloride tablets.
The non-pharmacological group received parent training, behavior modification, sensory integration therapy, and sand tray therapy. Parent training involved four sessions, including disease awareness, pros and cons of drugs, parent-child relationship, and methods to improve attention span. Behavior modification involved two major courses covering the positive reinforcement method of behavior modification, temporary isolation method, fading method, demonstration method, cognitive behavior therapy, and applied behavior analysis.
In addition, sensory integration therapy involved 45–60 min of training per session over 3–6 mo. The training process included warm-up, vestibular sensory, proprioception, balance, hand-eye coordination, sedation, and fine motor. Warm-up included simple children's songs, finger rhymes, action songs, and story reading. Vestibular sensor entailed rotating, moving, scooting, and crossing obstacles. Their proprioception was stimulated using "heavy work" activities, such as holding, lifting, pushing, and pulling heavy objects. Balance involved crossing the balance beam, walking along the hula hoop, one-legged games, and balance board. Furthermore, hand-eye coordination included throwing balloons and sandbags, hitting target objects, and throwing objects to partners. Sedation included relaxation activities, simple children's songs, finger rhymes, and storytelling. Finally, fine motor included making snacks, scrapbooking activities, art activities, and coloring.
Sand tray therapy involved 10–12 sessions with a unified sand tray therapist, with each session lasting about 40–60 min. The process includes instructional language, familiarization with the environment, feeling the sand, creating a sand tray, playing with the sand tray, dialogue and communication, dismantling the work, and discussion and analysis with parents. All programs were scheduled after school or during weekends for the children. All patients were followed up once a month for the first six months of drug administration and every 2–3 mo thereafter.
The two groups received Tiaoshen Yizhi Decoction consisting of 20 g of Paeoniae Radix Alba, 20 g of Rehmanniae Radix Praeparata, 6 g of Acori Tatarinowii Rhizoma, 20 g of Angelicae Sinensis Radix, 10 g of Lycii Fructus, 15 g of Ostreae Concha, 10 g of Testudinis Carapax et Plastrum, 15 g of Os Draconis, 6 g of Polygalae Radix, 15 g of Margarita, 10 g of Uncariae Ramulus cum Uncis, and 6 g of liquorice root, grounded into powder and one dose was administered daily. The powder was dissolved in 60 mL of boiling water, and half a dose was administered in the morning and in the evening.
The compliance scale designed by our hospital was used to assess the patient's treatment compliance before the parental intervention. Compliance was rated by the parents using a 3-point scale: full compliance, partial compliance, and non-compliance.
In addition, the Swanson, Nolan, and Pelham, Version IV (SNAP-IV) was used for rating, which contains nine inattention problems and nine hyperactivity/impulsivity problems, each with a 4-point scale indicating different levels of severity.
The Conners Parent Symptom Questionnaire (PSQ) was used. The questionnaire has 48 items and includes six factors: character problems, learning problems, psychosomatic problems, impulsivity-hyperactivity, anxiety, and hyperactivity index. The higher the factor score, the more severe the problem.
Finally, the Weiss Functional Impairment Rating Scale (WFIRS) was used to assess patients' social functioning. The scale contains 50 items rated by parents on six domains of family, learning/school, life skills, self-concept, social activities, and adventure activities, each on a scale of 0–4, respectively. The lower the score, the better the social functioning
If the parameter beta is either a difference of means, a log odds ratio, or a log hazard ratio, then it is reasonable to assume that the beta is unbiased and normally distributed. GraphPad Prism 8 was used for image processing, and SPSS 26.0 software was used to organize the data and for statistical analysis. Measurement data were expressed as mean ± SD and analyzed using the t-test. Count data were expressed as a rate (%) and compared using the χ2 test. P < 0.05 indicated that differences were statistically significant.
There were 35 males and 10 females in the pharmacological group, aged 6–18 (9.03 ± 1.78) years, with a duration of disease of 11–35 (23.89 ± 1.77) months and Wechsler IQ scores ≥ 85 (90.23 ± 2.91). In total, 39 cases attended school in urban areas, while 6 cases were schooled in non-urban areas. By contrast, there were 38 males and 7 females in the pharmacological group, aged 6–18 (9.23 ± 1.65) years, with a duration of illness of 11-37 (23.48 ± 2.13) months and Wechsler IQ scores ≥ 85 (90.37 ± 2.75). A total of 36 cases attended school in urban areas and 9 cases in non-urban areas. The characteristics of patients in the two groups were comparable (P > 0.05) (Table 1).
| Characteristics | Pharmaceutical group (n = 45) | Non-pharmaceutical group (n = 45) | t value | P value |
| Sex, n (%) | 0.653 | 0.419 | ||
| Male | 35 (77.78) | 38 (84.45) | ||
| Female | 10 (22.22) | 7 (15.55) | ||
| Age (yr, mean) | 6-18 (9.03 ± 1.78) | 6-18 (9.23 ± 1.65) | 0.553 | 0.582 |
| Duration of disease (mo, mean) | 11-35 (23.89 ± 1.77) | 11-37 (23.48 ± 2.13) | 0.993 | 0.323 |
| Wechsler intelligence score (score, mean) | ≥ 85 (90.23 ± 2.91) | ≥ 85 (90.37 ± 2.75) | 0.235 | 0.815 |
| School, n (%) | 0.720 | 0.396 | ||
| Urban | 39 (86.67) | 36 (80.00) | ||
| Non-urban | 6 (13.33) | 9 (20.00) |
Before treatment, there was no significant difference in compliance between the two groups (P > 0.05). After treatment, 43 (95.56%) of the 45 patients in the non-pharmacological group were compliant. The number of partially compliant patients in the non-pharmacological group increased to 22 (48.89%), while the number of non-compliant patients decreased to 2 (4.44%), indicating that non-pharmacological treatment can improve patients' treatment compliance compared with pharmacological intervention, and the difference was statistically significant (P < 0.05) (Table 2).
| Treatment compliance | Pharmaceutical group (n = 45) | Non-pharmaceutical group (n = 45) | χ2 | P value |
| Before treatment | 0.179 | 0.673 | ||
| Complete compliance | 1 (2.22) | 2 (4.44) | ||
| Partial compliance | 21 (46.67) | 18 (40.00) | ||
| Non-compliance | 23 (51.11) | 25 (55.55) | ||
| Compliance | 22 (48.89) | 20 (44.44) | ||
| After treatment | ||||
| Complete compliance | 12 (26.67) | 21 (46.67) | 15.195 | < 0.001 |
| Partial compliance | 20 (44.44) | 22 (48.89) | ||
| Non-compliance | 13 (28.89) | 2 (4.44) | ||
| Compliance | 32 (71.11) | 43 (95.56) |
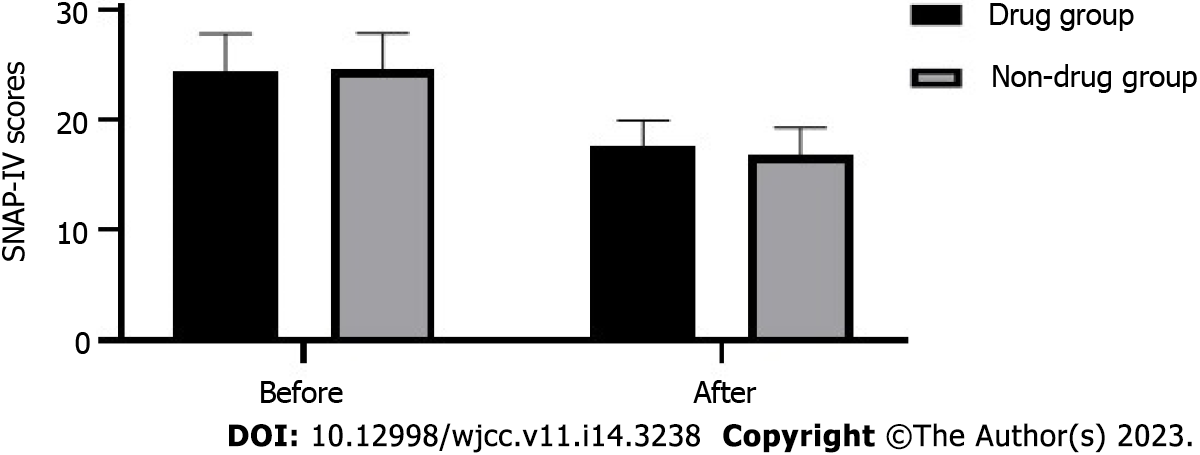
There was no statistically significant difference in SNAP-IV scores between the two groups of patients before treatment (P > 0.05). SNAP-IV scores were significantly reduced in both groups after treatment; the reduction was greater in the non-pharmacological intervention group (16.85 ± 2.48) than in the pharmacological group (17.69 ± 2.28). However, the differences in SNAP-IV scores between the two groups before and after treatment were not statistically significant (P > 0.05) (Figure 1).
After treatment, patients in the pharmacological group had character problems scores of 0.65 ± 0.11, learning problems scores of 0.88 ± 0.25, psychosomatic problems scores of 3.35 ± 1.05, impulsivity-hyperactivity scores of 1.02 ± 0.51, anxiety scores of 1.98 ± 1.21, and hyperactivity index scores of 0.85 ± 0.36. Patients in the non-pharmacological group had character problems scores of (0.61 ± 0.08), learning problems 0.81 ± 0.11, psychosomatic problems scores of 3.21 ± 0.77, impulsivity-hyperactivity scores of 0.87 ± 0.12, anxiety scores of 1.87 ± 0.89, and hyperactivity scores of 0.79 ± 0.35. There were no significant differences in Conners' PSQ scores between the two groups (P > 0. 05) (Table 3).
| Pharmaceutical group (n = 45) | Non-pharmaceutical group (n = 45) | t value | P value | |
| Character problems | 0.65 ± 0.11 | 0.61 ± 0.08 | 1.973 | 0.052 |
| Learning problems | 0.88 ± 0.25 | 0.81 ± 0.11 | 1.719 | 0.089 |
| Psychosomatic problems | 3.35 ± 1.05 | 3.21 ± 0.77 | 0.721 | 0.437 |
| Impulsivity-hyperactivity | 1.02 ± 0.51 | 0.87 ± 0.12 | 1.921 | 0.058 |
| Anxiety | 1.98 ± 1.21 | 1.87 ± 0.89 | 0.491 | 0.625 |
| Hyperactivity index | 0.85 ± 0.36 | 0.79 ± 0.35 | 0.802 | 0.425 |
After treatment, the family score in the pharmacological group (0.78 ± 0.52) and non-pharmacological group (0.46 ± 0.41) were statistically significantly different (t = 3.242, P < 0.05). There was a statistically significant difference (t = 5.335, P < 0.05) in the life skills score of the pharmacological group (0.99 ± 0.38) and the non- pharmacological group (0.69 ± 0.31). In addition, the difference in the self-concept score of the pharmacological group (0.95 ± 0.42) and the non-pharmacological group (0.65 ± 0.35) was statistically significant (t = 3.436, P < 0.05). However, there was no significant difference in Weiss scores between the two groups in learning/school, social activities, and risk-taking activities (P > 0.05). Family, life skills, and self-concept scores indicated that the non-pharmacological treatment group scored significantly better than the pharmacotherapy group (Table 4).
| Pharmaceutical group (n = 45) | Non-pharmaceutical group (n = 45) | t value | P value | |
| Family | 0.78 ± 0.52 | 0.46 ± 0.41 | 3.242 | 0.002 |
| Learning/school | 0.52 ± 0.44 | 0.42 ± 0.35 | 1.193 | 0.236 |
| Life skills | 0.99 ± 0.38 | 0.69 ± 0.31 | 5.335 | < 0.001 |
| Self-concept | 0.95 ± 0.42 | 0.65 ± 0.35 | 3.436 | 0.001 |
| Social activities | 0.45 ± 0.51 | 0.32 ± 0.21 | 1.581 | 0.117 |
| Adventure activities | 0.22 ± 0.21 | 0.20 ± 0.18 | 0.485 | 0.629 |
ADHD is a psychiatric disorder with significant symptoms that interfere with the child's daily life and learning. ADHD belongs to the categories of "forgetfulness", "deafness", and "false annoyance" in TCM. Approximately 20%–25% of children with ADHD exhibit symptoms that continue into adulthood. Early intervention once symptoms are detected is important to alleviate the symptoms and reduce the impairment of social functioning of the patients[13]. Pharmacotherapy is an effective treatment for ADHD that significantly relieves the core symptoms but is associated with adverse effects[7,14]. The efficacy of non-pharmacological interventions is more stable and efficient than pharmacological treatment.
This study found that the compliance of the non-pharmaceutical group (95.56%) was significantly higher than that of the pharmaceutical group (71.11%) after treatment. This difference in compliance suggests that, after treatment, patients in the non-pharmacological group, could follow their parents' advice and actively cooperate with the treatment, leading to significant improvements in their emotions and physical discomfort. Moreover, there were no significant differences in the SNAP-IV scores, PSQ scores, and the learning/school, social activities, and adventure activities of the WFIRS scores between the two groups. Patients who received non-pharmacological therapies had higher WFIRS ratings for family, life skills, and self-concept than those who received drugs. Compared to pharmaceutical therapies, non-pharmacological interventions provide more enrichment for children's competence development, family connection improvement, and self-evaluation. This finding contrasts with previous research findings, which may be attributed to personalized variances from the small sample size of this study.
In this study, non-pharmacological interventions included parent training, behavior modification, sensory integration therapy, and sand tray therapy. Parenting training is an established treatment for children with ADHD, whereas behavioral therapies focus on the functional recovery of ADHD children. Prior research has demonstrated marked symptom alleviation with parenting treatments for ADHD, and this correlation remains significant when trials with concurrent medication are omitted[15]. Different parenting behavior training programs have been proven effective, such as the 3P Positive Parenting Program[16], the New Forest Parenting Program[17], and the Barkley Program[18]. Some patients with ADHD experience perceptual problems and hand-eye coordination deficits. Research has shown that sensory-motor training could correct hyperactivity, impulsivity, and attention deficit, and adjust the vestibular response deficits of sensory integration disorders (vestibular balance organs form vague images and effects in the brain), tactile defenses (frontal cortical sensory acuity and control difficulties), use disorders in children (blurred body image formed in the brain by proprioceptive kinesthesia and vestibular balance organs, causing clumsy coordination of the five senses, especially hand-eye coordination and reading and writing difficulties), visuospatial shape perception disorder (the same principle as the use disorder, coupled with a lack of dexterity in the visual cortical coordination of the brain), and gravitational insecurity, which were reflected in the results of the current study.
In addition, sand tray therapy improves the ADHD hyperactivity index, character problems, hyperactivity/impulsivity, and anxiety in children. The reason may be that during the sand tray game, children with ADHD focus on the sand in their hands under the supervision of the host tester, which may gradually waken the children's inner ability of self-healing and self-development, effectively reducing anxiety and improving their emotional stability. The succession of sandbox imagery portrayed in the sandbox produces a continual dialogue between the sandbox player's conscious and unconscious thoughts, resulting in an effective improvement of character issues closely associated with personality. The combination of the above non-pharmacological interventions promotes emotional stability, gradually improves former interpersonal sensitivity, personality paranoia, and impulsive and aggressive behavior, and enhances self-esteem and self-confidence, which in turn facilitate the full recovery of patients' social functioning.
According to TCM theory, normal life activities and the mental state of the human body is a state of calmness of Yin and Yang[19,20]. Children's internal organs are delicate and vigorous and frequently suffer from a relative lack of essence, blood, fluid, and other material bases, predisposing them to a state of excitement, hyperactivity, impatience, irritability, and mental disturbance[21,22]. In TCM, treatment for ADHD lies on nourishing Yin and Yang, tonifying the liver, and benefiting the kidneys, for which Tiaoshen Yizhi Decoction was developed in our hospital for ADHD patients. The combination of drugs in the decoction focused on nourishing Yin and Yang without harming the spleen, and Angelicae Sinensis Radix was used to invigorate the blood. In addition, some herbs with sedative functions were used to prevent drowsiness in the children. Moreover, calm and warm medicines were used to avoid damage to the spleen and stomach, and protection of the righteous energy was emphasized in the use of drugs[23].
Our study has some limitations. The diversity of non-pharmacologic treatments increases the difficulty in controlling the operational criteria. Assessing the effectiveness of such non-pharmacologic treatments is closely related to the complexity of the intervention and the influence of different operational providers. Despite our rigorous control of the means and measures of non-pharmacological interventions, uncontrollable variation in the implementation of the treatment may still occur. Second, non-pharmacologic treatment alone is slow and time-consuming, so it is crucial that non-pharmacologic treatment be combined with appropriate pharmacologic treatments. The primary outcome measure in this study was based on self-reported symptoms and function. Therefore, we lacked more objective clinician-based measures. In addition, the sample size of ADAH patients in the study was not large enough, and future studies could be based on a larger sample size. Finally, long-term follow-up information could also be included in future studies to assess the long-term effects of non-pharmacological treatments on patients with ADAH.
No precise etiology or pathogenesis of ADHD has been identified to date, and a growing body of data suggests that the syndrome involves a combination of biopsychosocial factors. Therefore, combining pharmacological and non-pharmacological treatments is more appreciated for the biopsychosocial model. Compared with foreign studies, research in this area in China is still in its initial stage, and there are many problems to be addressed. Therefore, further promotion of research on the non-pharmacological treatment of ADHD in China is required.
In contrast to the potential risks of adverse events after long-term medication, non-pharmacological interventions improve the treatment compliance of patients, alleviate patients' behavioral symptoms of attention, impulsivity, and hyperactivity, and improve patients' cognitive ability, thereby enhancing family relationships and patient self-evaluation.
Long-term treatment of attention-deficit hyperactivity disorder (ADHD) is associated with adverse events. Therefore, non-pharmacological treatment has attracted a lot of attention as a new treatment, but its impact on the full recovery of social functioning of ADHD patients is still unknown.
Clarifying the effects of non-pharmacological treatments on the social functioning of ADAH patients is of great value and long-term significance to ADHD patients and their families.
This study aimed to investigate the impact of non-pharmacological treatments on the full recovery of social functioning in patients with ADHD.
A total of 90 patients diagnosed with ADHD were enrolled in the study and randomly assigned to either the pharmacological group or the non-pharmacological group, with 45 cases in each group. Treatment adherence, Swanson, Nolan and Pelham Fourth Edition (SNAP-IV) scores, Connors Parental Symptom Questionnaire (PSQ) scores, and Weil Functional Impairment Rating Scale (WFIRS) scores were measured.
Non-pharmacological interventions resulted in significantly higher compliance in patients compared to pharmacological intervention. No significant differences in the SNAP-IV scores, PSQ scores, and the learning/school, social activities, and adventure activities of the WFIRS scores were observed between the two groups. Patients in the non-pharmacological group showed higher WFIRS scores of family, daily life skills, and self-concept compared to those in the pharmacological group.
In contrast to the potential risks of adverse events after long-term medication, non-pharmacological interventions improve patient treatment compliance, alleviate patients' behavioral symptoms of attention, impulsivity, and hyperactivity, and improve their cognitive ability, thereby improving family relationships and patient self-evaluation.
This study demonstrates the positive impact of non-pharmacological treatment compared to long-term medication on the full recovery of social functioning in patients with ADAH.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Joshipura KJ, United States; Sanz M, Spain S-Editor: Wang JL L-Editor: A P-Editor: Yuan YY
| 1. | Polanczyk GV, Willcutt EG, Salum GA, Kieling C, Rohde LA. ADHD prevalence estimates across three decades: an updated systematic review and meta-regression analysis. Int J Epidemiol. 2014;43:434-442. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1344] [Cited by in RCA: 1100] [Article Influence: 100.0] [Reference Citation Analysis (0)] |
| 2. | Drechsler R, Brem S, Brandeis D, Grünblatt E, Berger G, Walitza S. ADHD: Current Concepts and Treatments in Children and Adolescents. Neuropediatrics. 2020;51:315-335. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 115] [Cited by in RCA: 149] [Article Influence: 29.8] [Reference Citation Analysis (0)] |
| 3. | Sobanski E, Banaschewski T, Asherson P, Buitelaar J, Chen W, Franke B, Holtmann M, Krumm B, Sergeant J, Sonuga-Barke E, Stringaris A, Taylor E, Anney R, Ebstein RP, Gill M, Miranda A, Mulas F, Oades RD, Roeyers H, Rothenberger A, Steinhausen HC, Faraone SV. Emotional lability in children and adolescents with attention deficit/hyperactivity disorder (ADHD): clinical correlates and familial prevalence. J Child Psychol Psychiatry. 2010;51:915-923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 225] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 4. | Biederman J, Petty CR, Dolan C, Hughes S, Mick E, Monuteaux MC, Faraone SV. The long-term longitudinal course of oppositional defiant disorder and conduct disorder in ADHD boys: findings from a controlled 10-year prospective longitudinal follow-up study. Psychol Med. 2008;38:1027-1036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 176] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 5. | Sonuga-Barke EJ, Brandeis D, Cortese S, Daley D, Ferrin M, Holtmann M, Stevenson J, Danckaerts M, van der Oord S, Döpfner M, Dittmann RW, Simonoff E, Zuddas A, Banaschewski T, Buitelaar J, Coghill D, Hollis C, Konofal E, Lecendreux M, Wong IC, Sergeant J; European ADHD Guidelines Group. Nonpharmacological interventions for ADHD: systematic review and meta-analyses of randomized controlled trials of dietary and psychological treatments. Am J Psychiatry. 2013;170:275-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 732] [Cited by in RCA: 683] [Article Influence: 56.9] [Reference Citation Analysis (0)] |
| 6. | Pliszka S; AACAP Work Group on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2007;46:894-921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1130] [Cited by in RCA: 1068] [Article Influence: 59.3] [Reference Citation Analysis (0)] |
| 7. | Subcommittee on Attention-Deficit/Hyperactivity Disorder; Steering Committee on Quality Improvement and Management, Wolraich M, Brown L, Brown RT, DuPaul G, Earls M, Feldman HM, Ganiats TG, Kaplanek B, Meyer B, Perrin J, Pierce K, Reiff M, Stein MT, Visser S. ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128:1007-1022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1183] [Cited by in RCA: 1165] [Article Influence: 83.2] [Reference Citation Analysis (0)] |
| 8. | National Collaborating Centre for Mental Health (UK). Attention Deficit Hyperactivity Disorder: Diagnosis and Management of ADHD in Children, Young People and Adults. Leicester (UK): British Psychological Society (UK), 2009. [PubMed] |
| 9. | Harpin VA. The effect of ADHD on the life of an individual, their family, and community from preschool to adult life. Arch Dis Child. 2005;90 Suppl 1:i2-i7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 427] [Cited by in RCA: 442] [Article Influence: 22.1] [Reference Citation Analysis (0)] |
| 10. | Biederman J, Petty CR, Fried R, Kaiser R, Dolan CR, Schoenfeld S, Doyle AE, Seidman LJ, Faraone SV. Educational and occupational underattainment in adults with attention-deficit/hyperactivity disorder: a controlled study. J Clin Psychiatry. 2008;69:1217-1222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 98] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 11. | Miklós M, Futó J, Komáromy D, Balázs J. Executive Function and Attention Performance in Children with ADHD: Effects of Medication and Comparison with Typically Developing Children. Int J Environ Res Public Health. 2019;16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 12. | Sprich SE, Safren SA, Finkelstein D, Remmert JE, Hammerness P. A randomized controlled trial of cognitive behavioral therapy for ADHD in medication-treated adolescents. J Child Psychol Psychiatry. 2016;57:1218-1226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 67] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 13. | Felt BT, Biermann B, Christner JG, Kochhar P, Harrison RV. Diagnosis and management of ADHD in children. Am Fam Physician. 2014;90:456-464. [PubMed] |
| 14. | Manos MJ, Giuliano K, Geyer E. ADHD: Overdiagnosed and overtreated, or misdiagnosed and mistreated? Cleve Clin J Med. 2017;84:873-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | Coates J, Taylor JA, Sayal K. Parenting Interventions for ADHD: A Systematic Literature Review and Meta-Analysis. J Atten Disord. 2015;19:831-843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 58] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 16. | Sanders MR. Triple P-Positive Parenting Program: towards an empirically validated multilevel parenting and family support strategy for the prevention of behavior and emotional problems in children. Clin Child Fam Psychol Rev. 1999;2:71-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 737] [Cited by in RCA: 460] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 17. | Sonuga-Barke EJ, Daley D, Thompson M, Laver-Bradbury C, Weeks A. Parent-based therapies for preschool attention-deficit/hyperactivity disorder: a randomized, controlled trial with a community sample. J Am Acad Child Adolesc Psychiatry. 2001;40:402-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 280] [Cited by in RCA: 218] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 18. | Storebø OJ, Elmose Andersen M, Skoog M, Joost Hansen S, Simonsen E, Pedersen N, Tendal B, Callesen HE, Faltinsen E, Gluud C. Social skills training for attention deficit hyperactivity disorder (ADHD) in children aged 5 to 18 years. Cochrane Database Syst Rev. 2019;6:CD008223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 19. | Schein J, Childress A, Gagnon-Sanschagrin P, Maitland J, Bedard J, Cloutier M, Guérin A. Treatment Patterns Among Patients with Attention-Deficit/Hyperactivity Disorder and Comorbid Anxiety and/or Depression in the United States: A Retrospective Claims Analysis. Adv Ther. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (1)] |
| 20. | Fu D, Guo HL, Hu YH, Chen F. A precision medication study of atomoxetine in children with attention deficit hyperactivity disorder: CYP2D6 genetic testing and therapeutic drug monitoring. Zhongguo Dang Dai Er Ke Za Zhi. 2023;25:98-103. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 21. | Çelik HEA, Küçükgöncü S, Erdoğan A, Özerdem A. Response Inhibition and Interference Control in Adult Attention Deficit Hyperactivity Disorder. Noro Psikiyatr Ars. 2023;60:3-8. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 22. | Chen SC, Cheng HL, Han LF, Wu GT, Zhang RY, Suen LK, Chen X, Yeung WF. Parent-administered pediatric tuina for the treatment of attention deficit hyperactivity disorder symptoms: Process evaluation of a pilot randomized controlled trial. Complement Ther Med. 2022;70:102854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 23. | Pauli-Pott U, Skoluda N, Nater UM, Becker K, Derz F, Kaspar E, Kasperzack D, Kehm K, Kött M, Mann C, Schurek P, Pott W, Schloß S. Long-term cortisol secretion in attention deficit hyperactivity disorder: roles of sex, comorbidity, and symptom presentation. Eur Child Adolesc Psychiatry. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 5.0] [Reference Citation Analysis (0)] |