Published online May 16, 2023. doi: 10.12998/wjcc.v11.i14.3167
Peer-review started: January 17, 2023
First decision: March 24, 2023
Revised: April 1, 2023
Accepted: April 10, 2023
Article in press: April 10, 2023
Published online: May 16, 2023
Processing time: 118 Days and 22.2 Hours
The incidence of lumbar tuberculosis is high worldwide, and effective treatment is a continuing problem.
To study the safety and efficacy of the multitrack and multianchor point screw technique combined with the contralateral Wiltse approach for lesion debri
The C-reactive protein (CRP) level, erythrocyte sedimentation rate (ESR), visual analogue scale (VAS) score, oswestry disability index (ODI) and American Spinal Injury Association (ASIA) grade were recorded and analysed pre- and postoperatively.
The CRP level and ESR returned to normal, and the VAS score and ODI were decreased at 3 mo postoperatively, with significant differences compared with the preoperative values (P < 0.01). Neurological dysfunction was relieved, and the ASIA grade increased, with no adverse events.
The multitrack, multianchor point screw fixation technique combined with the contralateral Wiltse approach for debridement is an effective and safe method for the treatment of lumbar tuberculosis.
Core Tip: Pedicle screw combined with cortical bone trajectory screw+ contralateral Wiltse approach is safe and effective in the treatment of lumbar tuberculosis and suitable for the case of heavier lesion on one side and no large or flow abscesses in front of the lumbar spine.
- Citation: Yuan YF, Ren ZX, Zhang C, Li GJ, Liu BZ, Li XD, Miao J, Li JF. Multitrack and multianchor point screw technique combined with the Wiltse approach for lesion debridement for lumbar tuberculosis. World J Clin Cases 2023; 11(14): 3167-3175
- URL: https://www.wjgnet.com/2307-8960/full/v11/i14/3167.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i14.3167
2020 Global Tuberculosis Report stated that tuber
At present, the choice of surgical approach for lumbar tuberculosis remains controversial[9]. The surgical app
Tuberculosis patients generally suffer from anaemia, hypoalbuminemia, and nutritional depletion[12], so surgical treatment should be as minimally invasive as possible to remove tuberculosis lesions while reducing damage to normal structures and reconstructing the spinal sequence[13]. Based on the above considerations, the author's team applied the posterior unilateral multitrack, multianchor screw technique combined with the contralateral Wiltse approach for lesion debridement in the treatment of lumbar tuberculosis.
An article in 2021 cited the pedicle screw as one of the top 10 inventions that shaped modern orthopaedics[14]. Pedicle screws were first used in vertebral fusion in 1959[15], and Roy-Camille first used pedicle screws for spinal fixation in 1963. Through the anterior column, pedicle screw placement can achieve three-column fixation of the spine, with excellent holding force and orthopaedic strength. In this study, the screw trajectory refers to the cortical bone trajectory (CBT) of the pedicle fixation technique, not the traditional technique. The CBT screw technique was first proposed by Santoni et al[16] in 2009; in this technique, the screw point is more inwards than the pedicle screw point, as it needs to be exposed to the isthmus of the lamina. The screw track runs from the medial-caudal to the lateral-cephalic direction. The screw is driven from the medial side of the lateral edge of the lamina into the posterior part of the superior endplate, and the screw path runs in the cortical bone. There are four cortical bone contact points to hold the screw, which results in a stronger screw holding force; thus, this technique is especially suitable for patients with osteoporosis and can be used for in revision surgery for adjacent segment disease[17] and in spinal orthopaedics[18].
Our research project was approved by the Ethics Committee of Handan Central Hospital. All patients signed informed consent forms. All methods were performed in accordance with the relevant guidelines and regulations.
The clinical data of patients with lumbar tuberculosis treated by unilateral pedicle screw combined with CBT screw fixation + the contralateral Wiltse approach for lumbar tuberculosis debridement from October 2014 to January 2021 were retrospectively analysed.
Inclusion criteria: X-ray, computed tomography (CT), magnetic resonance imaging (MRI), and other imaging examinations of patients showed vertebral and intervertebral space destruction, sequestrum formation, intervertebral and paravertebral cold abscess formation, spinal instability/deformity, etc., which were consistent with the characteristics of spinal tuberculosis; a caseous substance was present, consistent with the diagnosis of spinal tuberculosis by histopathology; the patient had symptoms such as night sweats, low fever in the afternoon, and fatigue; and the patient had intractable low back pain, progressive neurological impairment, and other symptoms. Exclusion criteria: huge abscess anterior to the lumbosacral spine; lumbar infusion abscess.
All patients were absolutely bedridden; high-energy and high-protein diets were given to improve the nutritional status, and anaemia and hypoproteinaemia were corrected before surgery. Low-molecular-weight heparin (4100 units 1/d) was injected subcutaneously to prevent deep vein thrombosis. All patients received standard combinations of 4 drugs for 2–4 wk (H, isoniazid: 300 mg/d, R, rifampicin: 450 mg/d, E, ethambutol: 750 mg/d, Z, pyrazinamide: 750 mg/d).
Two advanced surgeons performed the operations. The patient underwent general anaesthesia and tracheal intubation in the prone position. The target segment was positioned, a midline incision was made in the posterior lumbar spine, and the paraspinal muscle on the opposite side of the lesion was stripped. The spinous process, lamina, and facet joints were exposed, and the pedicle screws and CBT screws were inserted according to the preoperative plan. A prebent titanium rod was fixed and locked, and then the incision was closed. A wound incision was made on the opposite side, the original muscle space was separated to reach the intervertebral space, the channel was expanded step by step, a quadrant dilator was placed, the facet joint was exposed, and electrocautery was used to stop bleeding and peel the surface soft tissue. Osteotomy was used to remove part of the inferior and superior articular processes, and limited cleavage of the lamina was used to expose the spinal canal. Exposure and protection were performed under direct vision, and the dural sac and nerve root were retracted. Then, the intervertebral space was exposed, suction was performed to remove pus, and curettage of the infected vertebral body and intervertebral space abscess, sequestrum and caseous necrosis was performed with different angled spatulas until the surface of the healthy bone showed slight bleeding. After the lesions were completely removed, the dural sac was carefully checked to ensure that there was no damage, and a large amount of iodophor hydrogen peroxide and normal saline were injected through a syringe to flush the intervertebral space. After irrigation, 1.0 g of streptomycin was sprinkled into the wound, an indwelling negative-pressure drainage tube was placed in the deep paraspinal muscle, and the incision was closed. The culture results of samples from the removed lesions were consistent with the diagnosis of tuberculosis.
The motor and sensory functions of the legs of the patients were closely observed, and the patients were encouraged to perform straight leg raising exercises. When the drainage volume was less than 50 mL in 24 h, the drain was removed. Standard H/R/E/Z combinations were administered for at least 6 mo, and a lumbar brace was worn for at least 12-16 wk after surgery. It was recommended that the patients perform their daily activities without weight bearing. Routine blood examination results, liver and kidney function indicators, the C-reactive protein (CRP) level, and the erythrocyte sedimentation rate (ESR) were reviewed monthly according to the situation during the application of anti-tuberculosis drugs. X-rays were reviewed at 1, 3, 6, 9, and 12 mo after the operation and every year thereafter, and CT findings were reviewed every 3 mo. A trabecular bone connection between vertebrae as observed on CT reconstruction was considered to indicate bone fusion.
The CRP level and ESR were recorded and evaluated preoperatively and at the last follow-up. The Oswestry disability index (ODI), American Spinal Injury Association (ASIA) classification, and visual analogue scale (VAS) score of low back pain were documented and analysed preoperatively, 3 mo after the operation, and at the last follow-up. All patients underwent follow-up for at least one year, and the time of osseous fusion was recorded.
Statistical analysis was performed using SPSS 18.0 software (IBM, United States). The ESR and CRP level before surgery and at the last follow-up were continuous variables conforming to a normal distribution and were compared by paired t test. The ODI and VAS score before surgery, 3 mo after surgery, and at the last follow-up were analysed by one-way analysis of variance followed by the least significant difference test for comparisons between two groups. P < 0.05 was considered statistically significant.
Among a total of 13 patients, the male/female ratio was 5:8, and the average age was 60.15 ± 10.31 years (Table 1). Four patients also had pulmonary tuberculosis; 9 patients had symptoms of tuberculosis toxicity, such as low fever, night sweats, weight loss, and fatigue; and all patients had persistent low back pain in the passive position and different degrees of lower extremity nerve dysfunction. All patients underwent laboratory tests (routine blood examination, CRP, ESR) and imaging examinations (X-ray, CT, MRI).
| Case No. | Sex (M/F) | Age (year) | Bone fusion time (mo) | Operation | Follow-up (mo) | CRP (mg/L) | ESR (mm/h) | |||
| Time (min) | Blood loss (mL) | Preop | Final | Preop | Final | |||||
| 1 | M | 47 | 6 | 211 | 600 | 13 | 103.9 | 1.0 | 102 | 2 |
| 2 | M | 47 | 12 | 201 | 400 | 24 | 94.2 | 3.8 | 90 | 4 |
| 3 | M | 72 | 8 | 120 | 200 | 13 | 78.5 | 4.7 | 34 | 3.1 |
| 4 | F | 68 | 6 | 140 | 400 | 11 | 69 | 4.2 | 34.8 | 4 |
| 5 | F | 50 | 10 | 120 | 300 | 15 | 48.9 | 2.0 | 51 | 9 |
| 6 | F | 55 | 12 | 110 | 300 | 19 | 99 | 1.3 | 65 | 2.6 |
| 7 | M | 65 | 9 | 140 | 600 | 24 | 70 | 4.8 | 49 | 12 |
| 8 | F | 69 | 6 | 200 | 600 | 18 | 84 | 3.3 | 34 | 2 |
| 9 | F | 47 | 8 | 130 | 500 | 16 | 80 | 2.4 | 48 | 7 |
| 10 | F | 64 | 12 | 120 | 300 | 20 | 61 | 0.5 | 100 | 9 |
| 11 | F | 77 | 6 | 140 | 200 | 24 | 73 | 2.0 | 68 | 3 |
| 12 | F | 64 | 8 | 130 | 400 | 16 | 84 | 2.6 | 59 | 13 |
| 13 | M | 57 | 12 | 200 | 600 | 24 | 85 | 7 | 59 | 1.7 |
| mean ± SD | - | 60.15 ± 10.31 | 8.85 ± 2.51 | 150.92 ± 37.32 | 415.39 ± 151.91 | 18.23 ± 4.69 | 79.27 ± 15.23 | 3.05 ± 1.82a | 61.06 ± 23.58 | 5.57 ± 3.70a |
The mean operation time was 150.92 ± 37.32 min (110-210 min), the mean blood loss was 415.39 ± 151.91 mL (200-600 mL), and the mean follow-up time was 18.23 ± 4.69 mo (Table 1).
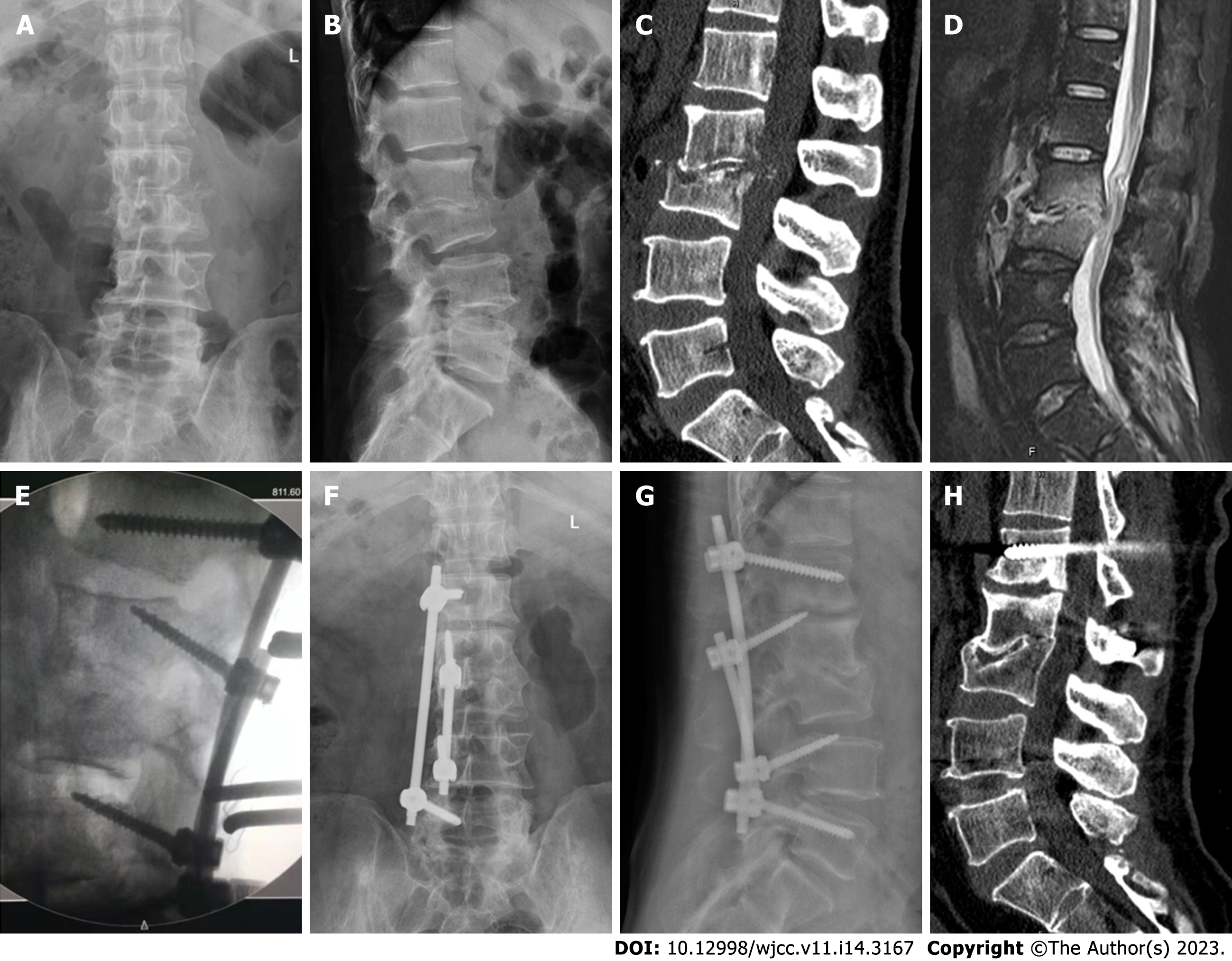
At the last follow-up, the CRP level and ESR in all patients decreased to the normal physiological range, and the difference was statistically significant compared with the preoperative values (CRP: t = 17.934, P < 0.001; ESR: t = 8.341, P < 0.001, Table 1). The average preoperative ODI of 80.31% ± 3.35% (86% - 74%) decreased to 29.08% ± 1.94% (26% - 32%, P < 0.05 compared with preoperation) 3 mo after the operation. By the last follow-up, the ODI further decreased to 19.54% ± 2.18% (16% - 24%, P < 0.05 compared with preoperation and P < 0.05 compared with 3 mo postoperation) (F = 2109.803, P < 0.001). The preoperative VAS score of 7.54 ± 0.97 (6-9) decreased to 2.23 ± 0.73 (1-3; P < 0.05 compared with preoperation) 3 mo after the operation and decreased to 0.54 ± 0.66 (0-2) by the last follow-up (P < 0.05 compared with preoperation and P < 0.05 compared with 3 mo postoperation) (F = 274.176, P < 0.001) (Table 2). The ASIA grade improved from grade C to D in one patient and from grade C to E in another patient at the last follow-up, and the ASIA grade improved from grade D to E in all 8 remaining patients at the last follow-up. The mean time to osseous fusion after surgery was 8.85 ± 2.51 mo. A retrospective case is shown in Figure 1. Two patients suffered from pneumonia, which was cured by the application of sensitive antibiotics postoperatively. There were no cases of intraoperative vascular or nerve injury or implant-related complications. The incision healed well in all patients, with no cases of sinus tract formation or tuberculosis recurrence.
The Wiltse approach is more accurate for removing lumbar tuberculosis lesions, with less intraoperative trauma and faster postoperative recovery[19]. Biomechanical studies have shown that the posterior bone structures of the spine act as anchor points for posterior muscles and ligaments, which can share the stress of internal fixation and increase the stability of the spine. The Wiltse approach has the following advantages: (1) The target lesion is entered through the original muscle space, retaining the attachment of the paraspinal muscle to the spinous process and maintaining the integrity of the muscle structure, additionally, dead space is not easily formed, reducing the risk of infection; (2) The Quadrant channel is fixed to expose the surgical area, reducing repeated pulling on the soft tissue, which is beneficial for the recovery of the soft tissue; and (3) The operation under the channel allows a single-person operation and reduces the workload of the assistant; additionally, reducing the degree of injury to the dorsal branch of the spinal nerve root reduces the risk of paraspinal muscle neuropathic atrophy, which is conducive to enhancing the recovery of patients after surgery.
The combined use of pedicle screws and CBT screws was first performed in patients with degenerative scoliosis by Professor Ueno et al[20] in 2013. The purpose of surgery for lumbar tuberculosis is to remove the infection foci, protect nerve function, and stabilize the spine. For tuberculosis lesions invading the anterior column and part of the central column of the vertebral body, CBT screws can be placed to avoid lesions and fix the spine through the posterior and central columns. Biomechanical studies have demonstrated that the insertion torque of CBT screws is 1.71 times that of pedicle screws[21], the uniaxial pullout resistance is increased by 30%[16]; additionally, the sagittal flexion and extension strength of CBT screws is better than that of pedicle screws. However, pedicle screws have strong resistance to axial rotation and coronal stress under lateral flexion[22], so we placed CBT screws in the middle and pedicle screws in the head and tail according to the characteristics of the lesion to achieve fixation with multiple tracks and anchors. In 2015, a study by Matsukawa et al[23] showed that the biomechanical strength of the same vertebral body after fixation with the cross-track technique was better than that after fixation with CBT and pedicle screws alone. Related studies have shown that short-term stabilization can be provided by an internal fixation system, while reconstruction with long-term stability requires bone fusion[24]. In this study, all patients were able to wear a brace to participate in daily activities. At the final follow-up, all patients showed bone fusion, with no cases of screw pullout or instrumentation failure. Thus, the authors speculate that multitrack, multianchor point screw technology provides outstanding fixation strength and a stable mechanical environment. However, the biomechanical strength of the fixed structure in this study needs to be further verified by biological models. Safety and efficacy of multitrack, multianchor point fixation combined with the Wiltse approach in the treatment of lumbar tuberculosis.
In this study, none of the patients experienced internal fixation-related neurological injury, and all achieved partial neurological recovery. At the last follow-up, the neurological function improved from ASIA grade D to grade E in 8 patients and ASIA grade C to grade E in 1 patient. The ODI and VAS score were also significantly improved at the last follow-up.
For MDR-TB with cavitation, adjuvant pneumonectomy is safe and effective[25]. Adjuvant therapeutic surgery can improve the quality of life of pulmonary tuberculosis patients, with more obvious benefits in women, those aged < 40 years, those with a body mass index ≥ 20 kg·m-2, and nonsmokers[26]. Pneumonectomy has been reported to have a 90% cure rate for MDR-TB, but the choice of surgical strategy requires the participation of both pulmonologists and cardiothoracic surgeons[27].
This was a retrospective study with a small sample size, no control group, and a short follow-up period, and a multicentre prospective randomized controlled trial with rich clinical data and a long follow-up period is needed. Due to the narrow operative field of the Wiltse approach under the channel, it is not suitable in cases where extensive debridement should be performed under direct anterior vision, such as in cases of large abscesses and infusion abscesses in front of the vertebra. Recurrence due to incomplete posterior debridement may occur in such cases. Due to the limitation of the surgical field, the surgeon needs to have sufficient patience to remove the lesion and repeatedly flush the intervertebral space.
Compared with other internal fixation techniques, fixation with pedicle screws combined with CBT screws and the contralateral Wiltse approach can be used to both effectively stabilize the spine and remove lesions with less trauma and is suitable in cases of larger lesions on one side and no large or only small abscesses in front of the lumbar spine.
The incidence of lumbar tuberculosis is high worldwide, and effective treatment is a continuing problem.
There are different methods for internal fixation in the treatment of lumbar tuberculosis, but method with less trauma are more beneficial for patients.
The objective of this study was to examine the efficacy of multitrajectory, multianchor fixation techniques combined with the contralateral Wiltse approach in the treatment of lumbar tuberculosis.
This retrospective analysis of patients diagnosed with lumbar tuberculosis compared the C-reactive protein (CRP) level, erythrocyte sedimentation rate (ESR), visual analogue scale (VAS) score of low back pain, Oswestry disability index (ODI) and American Spinal Injury Association (ASIA) grade as well as neurological recovery before and after surgery.
The CRP level, ESR, VAS score and ODI were decreased after surgery. Neurological dysfunction was relieved, and the ASIA grade was increased.
We propose that the multitrajectory, multianchor screw technique combined with the contralateral Wiltse approach for lesion removal is beneficial to improve the clinical symptoms and quality of life of patients with lumbar tuberculosis.
The multitrajectory, multianchor screw technique combined with the contralateral Wiltse approach for lesion removal is safe and effective in the treatment of lumbar tuberculosis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Elgafy H, United States; Keikha M, Iran; Vahedi P, Iran S-Editor: Liu XF L-Editor: A P-Editor: Zhang YL
| 1. | Sulis G, Adam P, Nafade V, Gore G, Daniels B, Daftary A, Das J, Gandra S, Pai M. Antibiotic prescription practices in primary care in low- and middle-income countries: A systematic review and meta-analysis. PLoS Med. 2020;17:e1003139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 125] [Cited by in RCA: 153] [Article Influence: 30.6] [Reference Citation Analysis (0)] |
| 2. | Chakaya J, Khan M, Ntoumi F, Aklillu E, Fatima R, Mwaba P, Kapata N, Mfinanga S, Hasnain SE, Katoto PDMC, Bulabula ANH, Sam-Agudu NA, Nachega JB, Tiberi S, McHugh TD, Abubakar I, Zumla A. Global Tuberculosis Report 2020 - Reflections on the Global TB burden, treatment and prevention efforts. Int J Infect Dis. 2021;113 Suppl 1:S7-S12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 421] [Cited by in RCA: 576] [Article Influence: 144.0] [Reference Citation Analysis (0)] |
| 3. | Millet JP, Moreno A, Fina L, del Baño L, Orcau A, de Olalla PG, Caylà JA. Factors that influence current tuberculosis epidemiology. Eur Spine J. 2013;22 Suppl 4:539-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 82] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 4. | Yang Z, Liu C, Niu N, Tang J, Shi J, Wang Z, Ding H. Selection of the fusion and fixation range in the intervertebral surgery to correct thoracolumbar and lumbar tuberculosis: a retrospective clinical study. BMC Musculoskelet Disord. 2021;22:466. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Martinez V, Rolland E, Bricaire F, Caumes E. Tuberculous paravertebral abscess. Lancet. 2004;363:615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Long W, Gong L, Cui Y, Qi J, Duan D, Li W. Single posterior debridement, interbody fusion, and fixation on patients with continuous multivertebral lumbar spine tuberculosis (CMLSTB). BMC Musculoskelet Disord. 2020;21:606. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 7. | Varatharajah S, Charles YP, Buy X, Walter A, Steib JP. Update on the surgical management of Pott's disease. Orthop Traumatol Surg Res. 2014;100:229-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Xu Z, Wang X, Liu Z. One-stage posterior debridement and single-segment interbody fusion for treating mono-segmental lumbar and lumbosacral spinal tuberculosis in adults following minimum 5-year follow-up. J Orthop Surg Res. 2020;15:473. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 9. | Hassan K, Elmorshidy E. Anterior vs posterior approach in surgical treatment of tuberculous spondylodiscitis of thoracic and lumbar spine. Eur Spine J. 2016;25:1056-1063. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 56] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 10. | Ukunda UNF, Lukhele MM. The posterior-only surgical approach in the treatment of tuberculosis of the spine: outcomes using cortical bone allografts. Bone Joint J. 2018;100-B:1208-1213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 11. | Li M, Huang J, Chen J, Liu S, Deng Z, Hu J, Cao Y, Wu T. Unilateral Limited Laminectomy for Debridement to Treat Localized Short-Segment Lumbosacral Spinal Tuberculosis: A Retrospective Case Series. Orthop Surg. 2021;13:1170-1180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Shah K, Kothari M, Nene A. Role of Frailty Scoring in the Assessment of Perioperative Mortality in Surgical Management of Tuberculous Spondylodiscitis in the Elderly. Global Spine J. 2018;8:698-702. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Yang X, Luo C, Liu L, Song Y, Li T, Zhou Z, Hu B, Zhou Q, Xiu P. Minimally invasive lateral lumbar intervertebral fusion vs traditional anterior approach for localized lumbar tuberculosis: a matched-pair case control study. Spine J. 2020;20:426-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Baig MN, Kearns SR, Shannon FJ, Devitt A. Ten Inventions That Shaped Modern Orthopedics. Cureus. 2021;13:e12819. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 15. | Boucher HH. A method of spinal fusion. J Bone Joint Surg Br. 1959;41-B:248-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 281] [Cited by in RCA: 255] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 16. | Santoni BG, Hynes RA, McGilvray KC, Rodriguez-Canessa G, Lyons AS, Henson MA, Womack WJ, Puttlitz CM. Cortical bone trajectory for lumbar pedicle screws. Spine J. 2009;9:366-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 381] [Cited by in RCA: 399] [Article Influence: 24.9] [Reference Citation Analysis (0)] |
| 17. | Rodriguez A, Neal MT, Liu A, Somasundaram A, Hsu W, Branch CL Jr. Novel placement of cortical bone trajectory screws in previously instrumented pedicles for adjacent-segment lumbar disease using CT image-guided navigation. Neurosurg Focus. 2014;36:E9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 71] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 18. | Ashayeri K, Nasser R, Nakhla J, Yassari R. The use of a pedicle screw-cortical screw hybrid system for the surgical treatment of a patient with congenital multilevel spinal non-segmentation defect and spinal column deformity: a technical note. Eur Spine J. 2016;25:3760-3764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine (Phila Pa 1976). 2003;28:S26-S35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 249] [Cited by in RCA: 336] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 20. | Ueno M, Imura T, Inoue G, Takaso M. Posterior corrective fusion using a double-trajectory technique (cortical bone trajectory combined with traditional trajectory) for degenerative lumbar scoliosis with osteoporosis: technical note. J Neurosurg Spine. 2013;19:600-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 21. | Matsukawa K, Yato Y, Kato T, Imabayashi H, Asazuma T, Nemoto K. In vivo analysis of insertional torque during pedicle screwing using cortical bone trajectory technique. Spine (Phila Pa 1976). 2014;39:E240-E245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 164] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 22. | Matsukawa K, Yato Y, Imabayashi H, Hosogane N, Asazuma T, Nemoto K. Biomechanical evaluation of the fixation strength of lumbar pedicle screws using cortical bone trajectory: a finite element study. J Neurosurg Spine. 2015;23:471-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 88] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 23. | Matsukawa K, Yato Y, Imabayashi H, Hosogane N, Asazuma T, Nemoto K. Biomechanical Evaluation of Cross Trajectory Technique for Pedicle Screw Insertion: Combined Use of Traditional Trajectory and Cortical Bone Trajectory. Orthop Surg. 2015;7:317-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 24. | Zheng G, Wang C, Wang T, Hu W, Ji Q, Hu F, Li J, Chaudhary SK, Song K, Song D, Zhang Z, Hao Y, Wang Y, Zheng Q, Zhang X. Relationship between postoperative lordosis distribution index and adjacent segment disease following L4-S1 posterior lumbar interbody fusion. J Orthop Surg Res. 2020;15:129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 25. | Vashakidze SA, Gogishvili SG, Nikolaishvili KG, Avaliani ZR, Chandrakumaran A, Gogishvili GS, Magee M, Blumberg HM, Kempker RR. Adjunctive surgery vs medical treatment among patients with cavitary multidrug-resistant tuberculosis. Eur J Cardiothorac Surg. 2021;60:1279-1285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Benito P, Vashakidze S, Gogishvili S, Nikolaishvili K, Despuig A, Tukvadze N, Shubladze N, Avaliani Z, Vilaplana C. Impact of adjuvant therapeutic surgery on the health-related quality of life of pulmonary tuberculosis patients. ERJ Open Res. 2020;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 27. | Alexander G, Perumal R. Do specialist pulmonologists appropriately utilise thoracic surgery for drug-resistant pulmonary tuberculosis? Afr J Thorac Crit Care Med. 2018;24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |