Published online May 16, 2023. doi: 10.12998/wjcc.v11.i14.3128
Peer-review started: December 3, 2022
First decision: February 8, 2023
Revised: March 2, 2023
Accepted: April 6, 2023
Article in press: April 6, 2023
Published online: May 16, 2023
Processing time: 163 Days and 13.1 Hours
The growing diabetic epidemic has created a substantial burden, not only on the people with diabetes but also on society at large. This mini-review discussed the limitations and patterns of disability in type 2 diabetes mellitus and put forward a case for the moderating effects of physical activity (PA) in the management of diabetes. The limitations and impairments associated with diabetes include vascular, neurological, cardiac, and renal impairments. Moreover, individuals participate less in their daily lives and in their instrumental activities of daily living, which negatively impacts the quality of life of individuals with diabetes. This often leads to a loss of quality of life due to disabilities, resulting in an increased rate of disability-adjusted life years among people with type 2 diabetes mellitus. Moreover, there are psychosocial sequelae of diabetes mellitus. This necessitates looking for moderating factors that may reduce the burden of the disease. PA has been shown to be one of the factors that can mitigate these burdens. PA does this in several ways, including through the benefits it confers, such as a reduction of hemoglobin A1c, a reduction of excess fat in the liver and pancreas, and the reduction of cardiovascular risk factors, all of which favorably affect glycemic parameters. Specifically, PA regulates or moderates diabetes disability through two mechanisms: The regulation of glucolipid metabolism disorders and the optimization of body mass index and systemic conditions. Therefore, efforts should be directed at PA uptake through identified strategies. This will not only prevent diabetes or diabetes complications but will reduce its burden.
Core Tip: There has been a growing epidemic of diabetes resulting in a substantial burden, not only on the people with diabetes but on society at large. This mini-review focused on the burden of disability in type 2 diabetes mellitus and discussed how physical activity moderates the burden.
- Citation: Oyewole OO, Ale AO, Ogunlana MO, Gurayah T. Burden of disability in type 2 diabetes mellitus and the moderating effects of physical activity. World J Clin Cases 2023; 11(14): 3128-3139
- URL: https://www.wjgnet.com/2307-8960/full/v11/i14/3128.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i14.3128
Diabetes remains a public health concern globally, with the epidemic growing in the last decade[1]. It is one of the leading causes of death globally[2]. In 2017, the global prevalence of diabetes was estimated to be 476 million people, which is projected to reach 570.9 million by 2025[2] and 693 million people by 2045[3]. There was a prevalence rate of 6059 cases per 100000 in 2017, projected to rise to 7079 cases per 100000 by 2030[4]. Diabetes, coupled with its complications, imposes several burdens on individuals affected by the disease, including economic and psychological limitations[5-7].
The cost of treating diabetes and its complications is a great burden globally[8-10]. Globally, the annual average cost (both direct and indirect) per person for treating type 2 diabetes mellitus (T2DM) ranged from USD 29.91 to USD 237.38 (direct costs USD 106.53-USD 293.79 and indirect costs USD 1.92-USD 73.4)[11]. This amounts to USD 25.51 billion in economic loss in Africa[12]. Similar economic loss was reported in other parts of the world, including Asia and Europe[6,7,13-16].
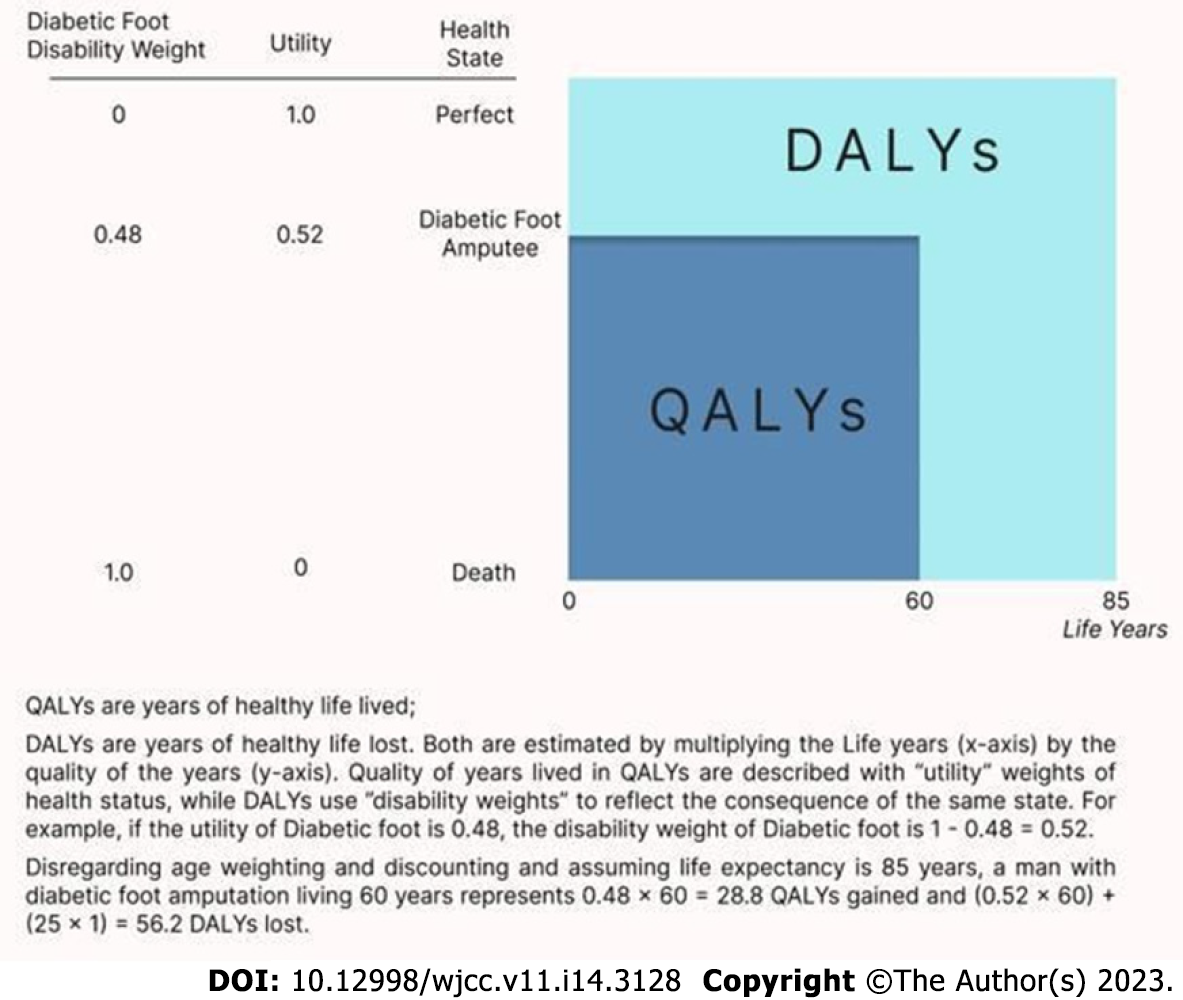
Diabetes and its complications cause severe disabilities in individuals with the condition and often lead to the loss of a healthy life due to disability[17]. Disability-adjusted life years (DALYs), an indicator to measure the burden of disease, have been reported to have increased among people with T2DM[17,18]. Globally, the age-standardized DALY rates increased by 5.07% from 2007 to 2017[18]. In 2017, 67.9 million DALYs were associated with diabetes, with a projection to 79.3 million by 2025[2].
To address the psychosocial issues that may arise from these burdens[5,19], it is necessary to look for moderating factors that may reduce the burden of the disease. Physical activity (PA) has been shown to be one of the factors that can mitigate these burdens[20]. PA does this in several ways through the benefits it confers, such as a reduction of excess fat in the liver and pancreas[21], the reduction of cardiovascular risk factors, and by favorably affecting glycemic parameters[20], thereby ultimately improving hemoglobin A1c[20,22]. Patient education is another key factor in reducing the burden of diabetes. Individuals with T2DM who are well-informed and motivated are more successful in maintaining good control of their risk factors and can eventually reduce their cardiovascular risk and slow the progression of microvascular disease[23]. This communication should be client-centered as it moderates the relationship between the burden of diabetes and diabetes distress[24]. Thus, this mini-review discussed the burden of disability in T2DM and the moderating effects of PA.
Diabetes was ranked ninth in the 2019 WHO global estimates of the leading causes of mortality, showing a 70% increase since the year 2000[25]. Moreover, it is one of the five leading conditions impacting years lived with disability in the Americas[26]. Diabetes is also implicated in the etiology of other conditions. Table 1 shows the percentages of comorbid conditions associated with diabetes in the National Burden of Disease study in South Africa[27].
| Diabetic-related comorbid conditions | Percent contribution to national burden of diseases in South Africa |
| Ischemic heart disease | 14% |
| Stroke | 10% |
| Hypertension | 12% |
| Renal disease | 12% |
There are numerous indicators and markers of disability in individuals with T2DM. One of these markers is weight management. It has been found that a significant proportion (around 85%) of diabetic adults are overweight[28], having a body mass index (BMI) of 25.0 to 29.9; while others are obese, with a BMI over 30. Individuals with a BMI over 40 at baseline were found to gain weight over a 10-year period. Moreover, there was a high proportion of insulin users in this group, confirming the link between insulin use and weight accumulation[29,30].
Keeping an individual’s weight stable and within the normal range acts to slow the increase of limitations in diabetic adults[31]. A study by Ferraro et al[32] found that the risk of disability was higher for obese individuals but not always for overweight individuals. Research has shown that 13.6% of patients with T2DM will develop some limitation in at least one activity of daily living (ADL) 6 years post diagnosis; and 38.3% will develop a functional decline at a rate of 1.0% mean decline in function per year[33,34].
It has been suggested that complications related to diabetes are avoidable[35]. This is contingent upon maintaining optimal hemoglobin A1c control in the range between 6.5% and 7.0% (48-53 mmol/mol)[36]. However late diagnosis, failure meeting the targeted DM treatment goals, and non-compliance with treatment can lead to severe complications such as nephropathy, neuropathy, retinopathy, amputations, and stroke[37]. A recurring finding is the physical limitations in both sexes, relating to the loss of function in the lower limbs, which impacts mobility, and is a predictor of the loss of autonomy[38,39].
The global epidemic of T2DM has been characterized by the early onset of the disease, typically in people below 40 years of age, who are obese, and who belong to an ethnic minority group. These characteristics are associated with decreased physical fitness and reduced muscle mass[40]. Moreover, there are specific markers of accelerated metabolic aging in T2DM, which leads to a ripple effect of functional decline, reduced physical capacity, and increased falls and fractures, typically seen in elderly people[41]. This leads to poorer functional outcomes and prognosis and a decreased quality of life. Specific limitations are discussed below and are shown in Table 2.
| Ref. | Type of disability | Summary/remark |
| Dhamoon et al[33], 2014 | Decline in function | 1% mean decline in function per year was reported |
| Sakurai et al[34], 2012 | ADL, IADL disability and functional impairment | After 6 years of follow-up, 13.6% of patients had developed a new ADL disability, and 38.3% had developed a new functional impairment |
| Gregg et al[70], 2000 | Physical disability | Among subjects ≥ 60 yr of age with diabetes, 32% of females and 15% of males reported an inability to walk one-fourth of a mile, climb stairs, or do housework compared with 14% of females and 8% of males without diabetes |
| Gregg et al[38], 2002 | Functional disability | The yearly incidence of any functional disability was 9.8% among females with diabetes and 4.8% among females without diabetes |
| Volpato et al[39,41], 2002; Volpato et al[41], 2010 | Functional/lower extremity disability | Females with diabetes showed a greater prevalence of mobility disability, disabilities in ADLs, and severe walking limitation; their summary mobility performance score (0-12 scale, based on balance, gait speed, chair stands) was 1.4 points lower than in nondiabetic women |
| Maggi et al[42], 2004 | ADLs and physical performance | The association between severe and/or total disability on the basis of physical performance tests and diabetes was strong in both sexes |
| Thein et al[44], 2018 | ADL and IADL disability | Diabetes was associated with a significantly higher prevalence of CI and/or PF. PF and/or CI were associated with a considerably higher prevalence of IADL |
| Ahmad et al[47], 2022 | Impaired physical function | Impaired physical function is a growing problem |
| Wong et al[48], 2013 | Physical disability | Diabetes is associated with a strong increase in the risk of physical disability |
| Godino et al[63], 2017 | Functional disability | Diabetes patients had a significantly greater burden of functional disability compared to those without diabetes |
| Malavige and Levy[64], 2009 | Erectile dysfunction | A prevalence of erectile dysfunction from 35% to 90% among diabetic males was reported |
| Omidvar et al[67], 2013 | Sexual dysfunction | The prevalence of sexual dysfunction was 32.3%. Low sexual desire was seen in 81.8%, disorders of arousal in 78.3%, orgasm disorder in 47.5%, and 35.1% had disorders in resolution areas |
Muscle wasting is a condition associated with aging and diabetes and is negatively associated with physical functioning[42]. As there is vascular and neurological impairment in diabetes, there may also be a vulnerability to depressive symptoms and dementia. Cognitive impairment has been shown to be increased in diabetic individuals[43]. In tandem with physical frailty, cognitive impairment is associated with a higher risk of mortality in diabetic individuals[44].
Frailty has been defined as the increased vulnerability to physical and psychological stressors due to decreased physiological reserves in multiple organ systems, which impact the body’s ability to maintain homeostasis[45]. Frailty can be diagnosed by confirming three of the following five criteria: Unintentional weight loss; low energy expenditure; slowness; weakness; and exhaustion[46]. While frailty is associated with elderly people, the frailty phenotype in T2DM is typically a younger obese individual with multiple comorbidities[47]. Frailty, accompanied by decreased physical function, has emerged as the third complication of T2DM after the micro- and macrovascular complications[48]. This is confirmed by the increased prevalence of frailty in 32% to 48% of individuals with diabetes aged 65 years and older, compared to only 5% to 10% of individuals in the general population[49].
Regular PA is one of the key factors in maintaining optimum blood sugar control in diabetic individuals[22]. However, individuals with cardiovascular conditions may avoid PA out of fear of hurting themselves[50]. This may be attributed to diabetic-related complications and comorbidities such as peripheral neuropathy, foot or leg pains, poor vision, and impaired renal function[51]. However, most individuals in the diabetic population lead sedentary lifestyles[52,53], which may have been exacerbated during the coronavirus disease 2019 pandemic as people’s movements were restricted.
It has been found that individuals with T2DM experience musculoskeletal pains twice as often as people in the general population[54]. Meanwhile, common reasons cited for the lack of regular exercise include having little time, bad weather, health problems, a lack of social support and professional coaching, safety considerations, limited access, prohibitive costs of a gym membership, and decreased self-efficacy[55,56]. Furthermore, the fear of stigma regarding their weight and feelings of shame, inferiority, and inadequacy may be a barrier to regular PA[57]. Obese individuals may be hypersensitive to people looking at them or making comments regarding their weight, while others feel they are too obese to exercise or experience discomfort related to their obesity, such as chafing of their thighs or becoming breathless[58].
There are likely to be greater functional limitations and disabilities in individuals with diabetes due to the comorbidities associated with diabetes. They are usually reported as limitations and impairments in ADLs, which relate to self-care activities such as feeding, bathing, toileting, and grooming. Impairments in ADLs are reported in research studies as they are predictors of morbidity and mortality[38,39]. The ability to perform ADLs and instrumental ADLs (IADL) is contingent upon the interplay of multiple physiological and organ systems, such as the musculoskeletal, neurological, vascular, and cardiorespiratory systems[59]. Being capable of independence in self-care, or ADLs and IADLs, is essential for independent community living and is directly associated with an individual’s quality of life[59,60]. Diabetes in Africa usually affects people between the ages of 40 years and 60 years, impacting their working lives negatively, and resulting in absenteeism, sick days, and decreased productivity[61].
An exploratory study by Huang et al[62] of the self-reported goals of individuals with T2DM who were 65 years and older revealed that they rated being independent and maintaining their functionality in terms of ADLs (71.0%) higher than maintaining their optimal blood glucose levels (3.5%), avoidance of symptoms (3.5%), or losing weight (14.0%). A cross-sectional study by Godino et al[63] revealed a pattern of diabetic-related disability across four domains in decreasing order, namely ADL, followed by IADL, lower limb mobility, and decreased physical function.
There are many changes that occur in the autonomic nervous systems of diabetic individuals, including the genitourinary system. There is a higher incidence of erectile dysfunction in the diabetic population, affecting 35% to 90% of men[64]. Pathophysiology has implicated multiple factors, including endothelial dysfunction, diabetic comorbidities, and psychological factors[65]. Moreover, erectile dysfunction may be an important marker of silent coronary heart disease and can predict future cardiovascular events in both diabetic and non-diabetic individuals[65]. As erectile dysfunction can affect self-esteem and trigger anxiety and depression, it is important to address the psychological factors as part of a holistic intervention program.
In females with diabetes, the patterns of sexual dysfunction are more varied and appear less prevalent[66]. However, they may still present with a low level of arousal and sexual drive, decreased vaginal lubrication, orgasmic dysfunction, dyspareunia, or painful intercourse[67]. These problems have been attributed to neuropathy, vascular impairment, and psychological factors. Other studies have identified all the aforementioned factors, as well as anxiety, decreased sexual satisfaction, and recurrent vaginal infections, which may negatively affect the sexual experiences of females with diabetes[68].
Disability in diabetes can be visible or hidden. Disability is the experience of any condition that makes it more difficult for a person to do certain activities or have equitable access within a given society. Diabetes is considered a disability under the federal law of the United States of America[69]. This is because it limits the functioning of the endocrine system. Hence, diabetes may be described as a hidden disability when its complications are not obvious.
Certain disabilities may predispose people to diabetes[69]. It is thought that disability could contribute to diabetes risk through an increase in sedentary behavior, muscle disuse, and a change in the ratio of lean-to-fat mass affecting insulin sensitivity in vulnerable adults[69]. However, it is commonly reported that diabetes leads to several disabilities that are said to be sex-specific[70]. Obesity, congestive heart diseases, lower extremity diseases, stroke, and depression appear to be the most prominent conditions that heighten the disability risk among people with and without diabetes[41].
All health interventions for people with diabetes aim to improve their quality of life as a health outcome. People with diabetes have a poorer quality of life than people with no chronic illnesses but a better quality of life than people with most other serious chronic diseases. Complications of diabetes are the most important disease-specific determinant of quality of life[71]. The complications of diabetes are the major pointers to the nature of disability that are visible and are important for describing the burden of diabetic disease. Jing et al[72], in a systematic review and meta-analysis, classified the factors associated with the quality of life of individuals with diabetes as characteristics related to the disease (the presence of complications, comorbidities like hypertension, the duration of diabetes, and insulin use), lifestyles (frequency of physical exercise, dietary controls including consumption of red meat, and the frequency of glucose checks), and mental factors (the presence of depression, anxiety, and worries).
The global burden of disease estimates that the use of information on mortality and morbidity, which are described as quality-adjusted life years and DALY, has been useful in quantifying the extent of disability in a disease like diabetes (Figure 1). These two constructs are used in estimating the burden of diseases like diabetes, and they are widely accepted as a reference standard in cost-effectiveness analyses[18,73].
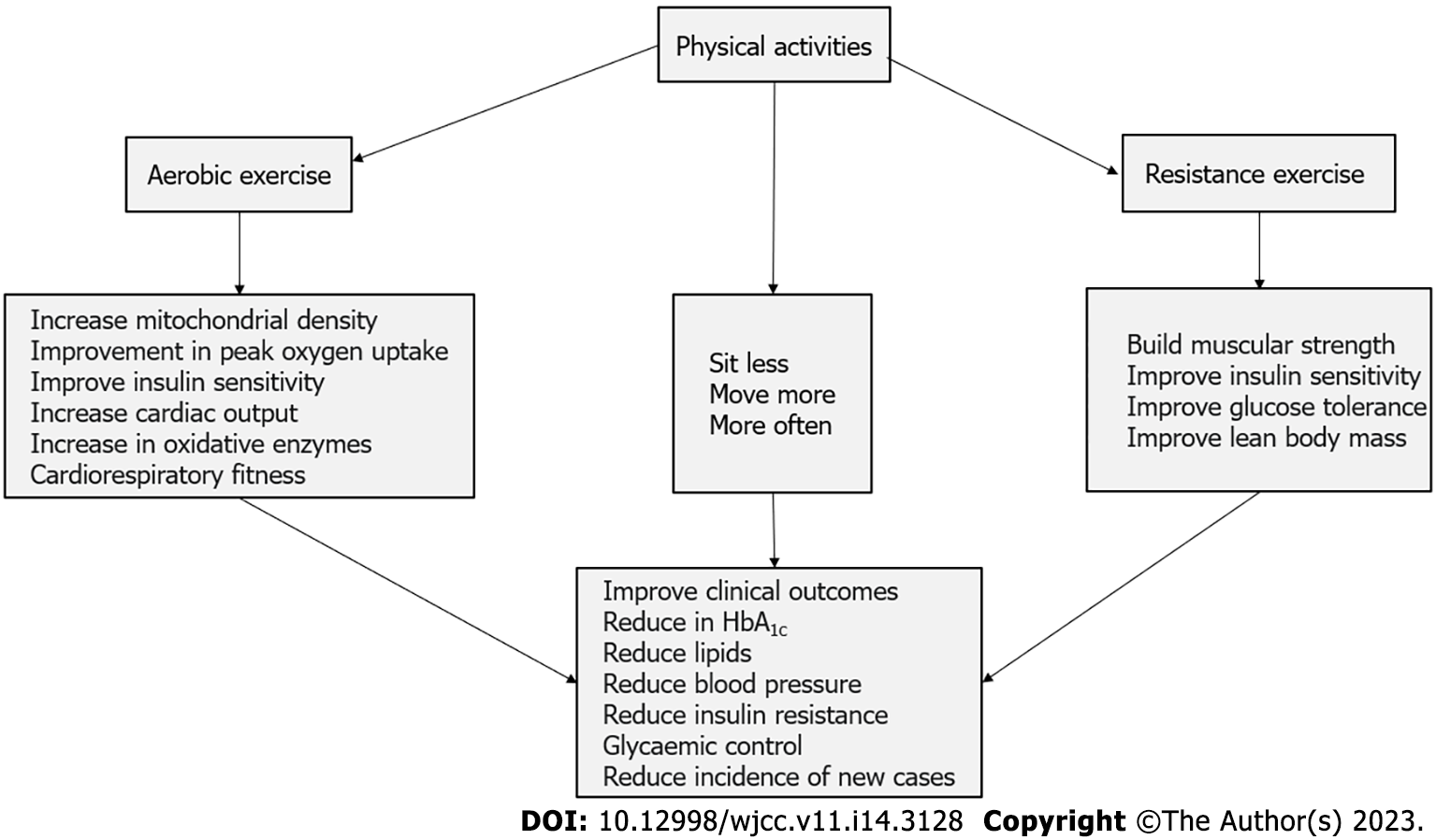
PA is a core element in DM management and in mitigating its complications. PA plays a key role in maintaining good glycemic control and other associated metabolic parameters. PA, coupled with diet and medical therapy, has been shown to reduce the complications of DM and improve quality of life. PA is defined as any bodily movement that substantially increases energy expenditure[22]. The American College of Sports Medicine recommended at least 150 min of moderately intensive aerobic activity or at least 75 min per week of vigorous aerobic activity or a combination of both, preferably spread throughout the week[22].
A high prevalence of physical inactivity has been reported worldwide among diabetic individuals, ranging from 31.0% to 61.0% in the United States, 30.7% in Brazil, 31.9% in Malaysia, and 38.4% in Saudi Arabia[74-76]. Nigeria reported a prevalence between 31% and 62%[77,78]. Many benefits are derived from regular PA (Figure 2). PA improves not only physical health but also metabolic control and mental and social-economic well-being. PA is an effective tool in DM management and aids in reducing the incidence of T2DM in people with impaired glucose tolerance, improving glucose control, blood pressure, lipids, and weight control in T2DM, and promoting better bone health. Increased fitness and function, enhanced feelings of well-being, a reduced risk of depression, and a reduction in morbidity and mortality culminate in lower healthcare expenditure[22,79-81]. In contrast, low PA levels lead to an increased risk of overall and cardiovascular disease mortality in people with diabetes[81].
The mechanism by which PA improves or confers these benefits has been explained through the regulation of glycolipid metabolism disorder. Mechanisms resulting from PA, which improve glucolipid metabolism, include an increase of glucose uptake and utilization in metabolic tissues, such as the skeletal muscle, liver, and adipose tissues, thereby enhancing insulin sensitivity, protecting pancreatic β cell function, increasing lipid hydrolysis oxidation, alleviating systemic inflammation, and optimizing BMI and systemic condition[82].
Studies have shown that pain, poor health, lack of willpower, lack of energy, lack of skills, lack of social support, and the fear of injury are the top obstacles to PA among DM individuals[83]. Identification with and acceptance of the new lifestyle, social support, support from healthcare professionals, achievement of results, and coping with ongoing challenges have been identified as motivation to maintain PA[84].
The importance of PA in the prevention and management of T2DM cannot be overemphasized[85]. Evidence has shown that reducing and frequently breaking up prolonged sitting with light-intensity PA and standing are among the practical strategies for improving T2DM prevention and management[86]. Thus, moderately intense PA (60 min to 75 min per day) eliminates the increased risk of death associated with prolonged sitting time[87]. Individuals with T2DM are more likely to experience a decline in physical function, especially in mid-life[88]. Regular PA has been shown to reduce the decline in function among the population of T2DM individuals[88].
PA has a direct influence on disability and quality of life. It decreases the self-reported levels of disability and maintains health-related quality of life (HRQoL)[89]. Fatigue, a common disabling clinical complaint among people with T2DM, is also documented to be positively influenced when sitting is regularly interrupted by brief activity breaks[90]. Beyond the effect of PA on an individual’s disability and HRQoL, PA has demonstrated a moderating effect on the relationship between disability and HRQoL among older adults[91]. For older adults with high levels of PA, the moderating effects on physical disability and HRQoL are significant, suggesting that improved PA reduces the negative impact of a poor quality of life and disability[91].
Although the moderating effects of PA on the relationship between disability and quality of life[91,92] have been studied in the older adult population, there are few or limited studies exploring the moderating and mediating effect of PA on the relationship between disability and quality of life in the T2DM population. This may suggest the focus or direction of future research into PA among people with T2DM. It will be of interest to explore the dose-response of PA on the relationship between disability and quality of life as well other factors that may enhance this moderating effect.
Despite expanded data on the benefits of diet, lifestyle modification, and PA in diabetes prevention and management, routine PA has declined in recent decades among individuals with diabetes[93]. Therefore, efforts should be directed at increasing PA uptake among this population. The Centers for Disease Control and Prevention identified ten strategies to improve PA in the community to prevent non-communicable diseases that may predispose individuals to developing diabetes[94]. These strategies include community-wide campaigns, point-of-decision prompts to encourage the use of stairs, individually adapted health behavior change program, enhanced school-based physical education, social support interventions in community settings, the creation of, or enhanced, access to places for PA combined with informational outreach activities, street-scale urban design and land-use policies and community-scale urban design and land-use policies, active transport to school and transportation and travel policies and practices[94]. It is essential to approach these strategies with a predictive, preventive, personalized, and participatory novel approach[93]. In another commentary, strategies to increase PA included measuring PA as a vital sign, encouraging individuals to be physically active at least 150 min per week, creating healthy environments by making it easier to be physically active where we live, learn, work, play, and pray, monitoring the disease incidence in individuals who are physically active compared to those who are not physically active, and spread best practices[95].
Evidence abounds regarding increasing the active use of stairs with point-of-decision prompts[94,96,97]. “Point-of-decision prompts are motivational signs placed on or near stairwells or at the base of elevators and escalators encouraging people to use the stairs”[97]. It is a community-based intervention for behavioral change that has increased PA[96]. It has been established that ascending stairs is a vigorous-intensity activity, while descending stairs is moderately intense, based on mean heart rate and perceived exertion responses to self-chosen, continuous stair use[98]. Thus, making use of stairs through point-of-decision prompts may help satisfy the daily recommendation for moderate or vigorous activity. Emerging data is also suggesting that climbing escalators may have similar health benefits or consequences as climbing stairs when compared to standing on escalators[99]. Thus, promoting point-of-decision prompts to encourage escalator climbing rather than standing on the escalator could promote energy expenditure. However, psychological barriers such as anxiety and depression, which have been associated with the perceived difficulty in using stairs, must be addressed for maximum PA uptake[98].
Attractive, personalized, and tailored smartphone-based mHealth PA interventions have been shown to increase PA uptake[100-103]. They positively affect an individual’s engagement and perception. Smartphone apps and self-monitoring devices are evolving technologies that promote PA uptake[104,105]. It has been suggested that video games that require gross motor activity, such as Exergames on Nintendo Wii, Xbox, and PlayStation promote healthy weight and PA in the general population[104,106]. The use of social media to jumpstart PA has also been documented[104,105].
One of the strategies to improve PA uptake is education and counseling[95]. An assessment of PA at each visit to a physician or health provider will facilitate proper education and counseling. Asking a client the number of minutes per week she or he participated in PA will reinforce the notion that exercise is a vital part of health just like other vital signs of health, such as blood pressure[95]. A conversation about the importance of PA in health can begin if the individual does not meet exercise goals. The focus should be on letting them understand what is expected of them and teaching them how to change their behavior from inactivity to daily PA. Lehr et al[107] proposed the ABCD of lifestyle counseling to improve individual health, including daily PA uptake. The acronym ABCD represents assess, barriers, commit, and demonstrate. The ABCD framework for lifestyle counselling starts with: (1) Assessing a patient’s readiness for change; (2) identifying potential barriers to change; (3) encouraging patients to commit to measurable goals; and (4) helping them demonstrate progress by selecting an appropriate self-monitoring strategy[107].
This article explored the limitations and complications that can result from poorly managed T2DM. These limitations relate to obesity, cardiac complications, renal, vascular, and neurological problems, sexual dysfunction, and decreased participation in ADL, IADL, and work. However, PA, in tandem with a healthy diet, appears to be an effective strategy in reducing the long-term complications of T2DM. It will also curb spending in terms of non-communicable diseases, including diabetes. Specifically, PA regulates or moderates diabetes disability through two mechanisms: The regulation of glucose and lipid metabolism disorders and the optimization of BMI and systemic condition. It is, therefore, imperative to include a prescription of regular, moderate physical exercise/activity in the treatment regimen of all people with T2DM to improve their medical and functional prognosis and quality of life. Exercise can also be used as a health promotion and prevention strategy in population-level interventions.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Endocrinology and metabolism
Country/Territory of origin: Nigeria
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Balbaa ME, Egypt; Lee S, South Korea; Long P, China S-Editor: Chen YL L-Editor: Filipodia P-Editor: Yu HG
| 1. | Lovic D, Piperidou A, Zografou I, Grassos H, Pittaras A, Manolis A. The Growing Epidemic of Diabetes Mellitus. Curr Vasc Pharmacol. 2020;18:104-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 244] [Article Influence: 48.8] [Reference Citation Analysis (0)] |
| 2. | Lin X, Xu Y, Pan X, Xu J, Ding Y, Sun X, Song X, Ren Y, Shan PF. Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Sci Rep. 2020;10:14790. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 695] [Cited by in RCA: 909] [Article Influence: 181.8] [Reference Citation Analysis (1)] |
| 3. | Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, Malanda B. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3709] [Cited by in RCA: 4372] [Article Influence: 624.6] [Reference Citation Analysis (0)] |
| 4. | Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J. Epidemiology of Type 2 Diabetes-Global Burden of Disease and Forecasted Trends. J Epidemiol Glob Health. 2020;10:107-111. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 523] [Cited by in RCA: 1638] [Article Influence: 409.5] [Reference Citation Analysis (2)] |
| 5. | Kangethe A, Lawrence DF, Touya M, Chrones L, Polson M, Evangelatos T. Incremental burden of comorbid major depressive disorder in patients with type 2 diabetes or cardiovascular disease: a retrospective claims analysis. BMC Health Serv Res. 2021;21:778. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Köster I, Huppertz E, Hauner H, Schubert I. Direct costs of diabetes mellitus in Germany-CoDiM 2000-2007. Exp Clin Endocrinol Diabetes. 2011;119:377-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 59] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 7. | Sortsø C, Green A, Jensen PB, Emneus M. Societal costs of diabetes mellitus in Denmark. Diabet Med. 2016;33:877-885. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 63] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 8. | Alzaid A, Ladrón de Guevara P, Beillat M, Lehner Martin V, Atanasov P. Burden of disease and costs associated with type 2 diabetes in emerging and established markets: systematic review analyses. Expert Rev Pharmacoecon Outcomes Res. 2021;21:785-798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 9. | Cannon A, Handelsman Y, Heile M, Shannon M. Burden of Illness in Type 2 Diabetes Mellitus. J Manag Care Spec Pharm. 2018;24:S5-S13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 78] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 10. | Andersson E, Persson S, Hallén N, Ericsson Å, Thielke D, Lindgren P, Steen Carlsson K, Jendle J. Costs of diabetes complications: hospital-based care and absence from work for 392,200 people with type 2 diabetes and matched control participants in Sweden. Diabetologia. 2020;63:2582-2594. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 51] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 11. | Afroz A, Alramadan MJ, Hossain MN, Romero L, Alam K, Magliano DJ, Billah B. Cost-of-illness of type 2 diabetes mellitus in low and lower-middle income countries: a systematic review. BMC Health Serv Res. 2018;18:972. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 70] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 12. | Mapa-Tassou C, Katte JC, Mba Maadjhou C, Mbanya JC. Economic Impact of Diabetes in Africa. Curr Diab Rep. 2019;19:5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 13. | Catic T, Popovic SP, Asimi ZV, Hlavinkova L. Costs of Diabetes Mellitus and Its Complications in Bosnia and Herzegovina. Mater Sociomed. 2022;34:149-154. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 14. | Eshwari K, Kamath VG, Rao CR, Kamath A. Economic burden of type 2 diabetes mellitus management: Epidemiological determinants from a coastal community of Southern India. WHO South East Asia J Public Health. 2021;10:84-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 15. | Ganasegeran K, Hor CP, Jamil MFA, Loh HC, Noor JM, Hamid NA, Suppiah PD, Abdul Manaf MR, Ch'ng ASH, Looi I. A Systematic Review of the Economic Burden of Type 2 Diabetes in Malaysia. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 16. | Al-Maskari F, El-Sadig M, Nagelkerke N. Assessment of the direct medical costs of diabetes mellitus and its complications in the United Arab Emirates. BMC Public Health. 2010;10:679. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 74] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 17. | Kotwas A, Karakiewicz B, Zabielska P, Wieder-Huszla S, Jurczak A. Epidemiological factors for type 2 diabetes mellitus: evidence from the Global Burden of Disease. Arch Public Health. 2021;79:110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (1)] |
| 18. | Yu M, Zhan X, Yang Z, Huang Y. Measuring the global, regional, and national burden of type 2 diabetes and the attributable risk factors in all 194 countries. J Diabetes. 2021;13:613-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 19. | Hussain S, Habib A, Singh A, Akhtar M, Najmi AK. Prevalence of depression among type 2 diabetes mellitus patients in India: A meta-analysis. Psychiatry Res. 2018;270:264-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 51] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 20. | Amanat S, Ghahri S, Dianatinasab A, Fararouei M, Dianatinasab M. Exercise and Type 2 Diabetes. Adv Exp Med Biol. 2020;1228:91-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 83] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 21. | Taylor R, Valabhji J, Aveyard P, Paul D. Prevention and reversal of Type 2 diabetes: highlights from a symposium at the 2019 Diabetes UK Annual Professional Conference. Diabet Med. 2019;36:359-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 22. | Kanaley JA, Colberg SR, Corcoran MH, Malin SK, Rodriguez NR, Crespo CJ, Kirwan JP, Zierath JR. Exercise/Physical Activity in Individuals with Type 2 Diabetes: A Consensus Statement from the American College of Sports Medicine. Med Sci Sports Exerc. 2022;54:353-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 371] [Article Influence: 123.7] [Reference Citation Analysis (0)] |
| 23. | Rachmani R, Slavachevski I, Berla M, Frommer-Shapira R, Ravid M. Teaching and motivating patients to control their risk factors retards progression of cardiovascular as well as microvascular sequelae of Type 2 diabetes mellitus- a randomized prospective 8 years follow-up study. Diabet Med. 2005;22:410-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Peimani M, Garmaroudi G, Stewart AL, Yekaninejad M, Shakibazadeh E, Nasli-Esfahani E. Type 2 Diabetes Burden and Diabetes Distress: The Buffering Effect of Patient-centred Communication. Can J Diabetes. 2022;46:353-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 25. | World Health Organization. The top 10 causes of death. 2020. [cited 7 March 2023]. Available from: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death. |
| 26. | Pan American Health Organization. Leading causes of mortality and health loss at regional, subregional, and country levels in the Region of the Americas. 2021. [cited 7 March 2023]. Available from: https://www.paho.org/en/enlace/Leading-causes-death-and-disability. |
| 27. | Bradshaw D, Norman R, Pieterse D, Levitt NS; South African Comparative Risk Assessment Collaborating Group. Estimating the burden of disease attributable to diabetes in South Africa in 2000. S Afr Med J. 2007;97:700-706. [PubMed] |
| 28. | Powell A. Obesity? Diabetes? We’ve been set up. Harvard Gazette. March 7, 2012. [cited 7 March 2023]. Available from: https://news.harvard.edu/gazette/story/2012/03/the-big-setup/. |
| 29. | Chaudhry ZW, Gannon MC, Nuttall FQ. Stability of body weight in type 2 diabetes. Diabetes Care. 2006;29:493-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 30. | Russell-Jones D, Khan R. Insulin-associated weight gain in diabetes--causes, effects and coping strategies. Diabetes Obes Metab. 2007;9:799-812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 356] [Cited by in RCA: 398] [Article Influence: 22.1] [Reference Citation Analysis (0)] |
| 31. | Chiu CJ, Wray LA, Lu FH, Beverly EA. BMI change patterns and disability development of middle-aged adults with diabetes: a dual trajectory modeling approach. J Gen Intern Med. 2013;28:1150-1156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 32. | Ferraro KF, Su YP, Gretebeck RJ, Black DR, Badylak SF. Body mass index and disability in adulthood: a 20-year panel study. Am J Public Health. 2002;92:834-840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 162] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 33. | Dhamoon MS, Moon YP, Paik MC, Sacco RL, Elkind MS. Diabetes predicts long-term disability in an elderly urban cohort: the Northern Manhattan Study. Ann Epidemiol. 2014;24:362-368.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 34. | Sakurai T, Iimuro S, Sakamaki K, Umegaki H, Araki A, Ohashi Y, Ito H; Japanese Elderly Diabetes Intervention Trial Study Group. Risk factors for a 6-year decline in physical disability and functional limitations among elderly people with type 2 diabetes in the Japanese Elderly Diabetes Intervention Trial. Geriatr Gerontol Int. 2012;12 Suppl 1:117-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 35. | Andrade CS, Ribeiro GS, Santos CAST, Neves RCS, Moreira ED Jr. Factors associated with high levels of glycated haemoglobin in patients with type 1 diabetes: a multicentre study in Brazil. BMJ Open. 2017;7:e018094. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 36. | American Diabetes Association. 5. Glycemic Targets. Diabetes Care. 2016;39 Suppl 1:S39-S46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 161] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 37. | Fox KM, Gerber Pharmd RA, Bolinder B, Chen J, Kumar S. Prevalence of inadequate glycemic control among patients with type 2 diabetes in the United Kingdom general practice research database: A series of retrospective analyses of data from 1998 through 2002. Clin Ther. 2006;28:388-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 101] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 38. | Gregg EW, Mangione CM, Cauley JA, Thompson TJ, Schwartz AV, Ensrud KE, Nevitt MC; Study of Osteoporotic Fractures Research Group. Diabetes and incidence of functional disability in older women. Diabetes Care. 2002;25:61-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 222] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 39. | Volpato S, Blaum C, Resnick H, Ferrucci L, Fried LP, Guralnik JM; Women's Health and Aging Study. Comorbidities and impairments explaining the association between diabetes and lower extremity disability: The Women's Health and Aging Study. Diabetes Care. 2002;25:678-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 161] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 40. | Magliano DJ, Sacre JW, Harding JL, Gregg EW, Zimmet PZ, Shaw JE. Young-onset type 2 diabetes mellitus-implications for morbidity and mortality. Nat Rev Endocrinol. 2020;16:321-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 279] [Article Influence: 55.8] [Reference Citation Analysis (0)] |
| 41. | Volpato S, Maraldi C, Fellin R. Type 2 diabetes and risk for functional decline and disability in older persons. Curr Diabetes Rev. 2010;6:134-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 68] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 42. | Maggi S, Noale M, Gallina P, Marzari C, Bianchi D, Limongi F, Crepaldi G; ILSA Group. Physical disability among older Italians with diabetes. The ILSA study. Diabetologia. 2004;47:1957-1962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 49] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 43. | Gregg EW, Engelgau MM, Narayan V. Complications of diabetes in elderly people. BMJ. 2002;325:916-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 64] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 44. | Thein FS, Li Y, Nyunt MSZ, Gao Q, Wee SL, Ng TP. Physical frailty and cognitive impairment is associated with diabetes and adversely impact functional status and mortality. Postgrad Med. 2018;130:561-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 60] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 45. | Bergman H, Ferrucci L, Guralnik J, Hogan DB, Hummel S, Karunananthan S, Wolfson C. Frailty: an emerging research and clinical paradigm--issues and controversies. J Gerontol A Biol Sci Med Sci. 2007;62:731-737. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 826] [Cited by in RCA: 781] [Article Influence: 43.4] [Reference Citation Analysis (0)] |
| 46. | Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA; Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146-M156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13384] [Cited by in RCA: 15897] [Article Influence: 662.4] [Reference Citation Analysis (1)] |
| 47. | Ahmad E, Sargeant JA, Yates T, Webb DR, Davies MJ. Type 2 Diabetes and Impaired Physical Function: A Growing Problem. Diabetology. 2022;3:30-45. [DOI] [Full Text] |
| 48. | Wong E, Backholer K, Gearon E, Harding J, Freak-Poli R, Stevenson C, Peeters A. Diabetes and risk of physical disability in adults: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2013;1:106-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 250] [Cited by in RCA: 311] [Article Influence: 25.9] [Reference Citation Analysis (0)] |
| 49. | Morley JE, Malmstrom TK, Rodriguez-Mañas L, Sinclair AJ. Frailty, sarcopenia and diabetes. J Am Med Dir Assoc. 2014;15:853-859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 218] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 50. | Rogerson MC, Murphy BM, Bird S, Morris T. "I don't have the heart": a qualitative study of barriers to and facilitators of physical activity for people with coronary heart disease and depressive symptoms. Int J Behav Nutr Phys Act. 2012;9:140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 60] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 51. | McCarthy MM, Davey J, Wackers FJ, Chyun DA. Predictors of physical inactivity in men and women with type 2 diabetes from the Detection of Ischemia in Asymptomatic Diabetics (DIAD) study. Diabetes Educ. 2014;40:678-687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 52. | Loprinzi PD, Hager KK, Ramulu PY. Physical activity, glycemic control, and diabetic peripheral neuropathy: a national sample. J Diabetes Complications. 2014;28:17-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 53. | Zhao G, Ford ES, Li C, Balluz LS. Physical activity in U.S. older adults with diabetes mellitus: prevalence and correlates of meeting physical activity recommendations. J Am Geriatr Soc. 2011;59:132-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 138] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 54. | Molsted S, Tribler J, Snorgaard O. Musculoskeletal pain in patients with type 2 diabetes. Diabetes Res Clin Pract. 2012;96:135-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 77] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 55. | Buckworth J, Lee RE, Regan G, Schneider LK, DiClemente CC. Decomposing intrinsic and extrinsic motivation for exercise: Application to stages of motivational readiness. Psychol Sport Exerc. 2007;8:441-461. [DOI] [Full Text] |
| 56. | Moschny A, Platen P, Klaassen-Mielke R, Trampisch U, Hinrichs T. Barriers to physical activity in older adults in Germany: a cross-sectional study. Int J Behav Nutr Phys Act. 2011;8:121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 230] [Cited by in RCA: 227] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 57. | Lidegaard LP, Schwennesen N, Willaing I, Faerch K. Barriers to and motivators for physical activity among people with Type 2 diabetes: patients' perspectives. Diabet Med. 2016;33:1677-1685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 53] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 58. | Bombak AE. Obese persons' physical activity experiences and motivations across weight changes: a qualitative exploratory study. BMC Public Health. 2015;15:1129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 59. | Garber CE, Greaney ML, Riebe D, Nigg CR, Burbank PA, Clark PG. Physical and mental health-related correlates of physical function in community dwelling older adults: a cross sectional study. BMC Geriatr. 2010;10:6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 102] [Cited by in RCA: 106] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 60. | Painter P, Stewart AL, Carey S. Physical functioning: definitions, measurement, and expectations. Adv Ren Replace Ther. 1999;6:110-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 133] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 61. | Peer N, Kengne AP, Motala AA, Mbanya JC. Diabetes in the Africa Region: an update. Diabetes Res Clin Pract. 2014;103:197-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 120] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 62. | Huang ES, Gorawara-Bhat R, Chin MH. Self-reported goals of older patients with type 2 diabetes mellitus. J Am Geriatr Soc. 2005;53:306-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 96] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 63. | Godino JG, Appel LJ, Gross AL, Schrack JA, Parrinello CM, Kalyani RR, Windham BG, Pankow JS, Kritchevsky SB, Bandeen-Roche K, Selvin E. Diabetes, hyperglycemia, and the burden of functional disability among older adults in a community-based study. J Diabetes. 2017;9:76-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 64. | Malavige LS, Levy JC. Erectile dysfunction in diabetes mellitus. J Sex Med. 2009;6:1232-1247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 271] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 65. | Phé V, Rouprêt M. Erectile dysfunction and diabetes: a review of the current evidence-based medicine and a synthesis of the main available therapies. Diabetes Metab. 2012;38:1-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 89] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 66. | Jackson G. Sexual dysfunction and diabetes. Int J Clin Pract. 2004;58:358-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 35] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 67. | Omidvar S, Niaki MT, Amiri FN, Kheyrkhah F. Sexual dysfunction among women with diabetes mellitus in a diabetic center in Amol. J Nat Sci Biol Med. 2013;4:321-324. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 68. | White L, Duncan G. Medical-surgical nursing: an integrated approach. 2nd ed. February 8, 2012. [cited 7 March 2023]. Available from: https://archive.org/details/medicalsurgicaln0000whit. |
| 69. | Bardenheier BH, Gregg EW, Zhuo X, Cheng YJ, Geiss LS. Association of functional decline with subsequent diabetes incidence in U.S. adults aged 51 years and older: the Health and Retirement Study 1998-2010. Diabetes Care. 2014;37:1032-1038. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 70. | Gregg EW, Beckles GL, Williamson DF, Leveille SG, Langlois JA, Engelgau MM, Narayan KM. Diabetes and physical disability among older U.S. adults. Diabetes Care. 2000;23:1272-1277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 377] [Cited by in RCA: 358] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 71. | Rubin RR, Peyrot M. Quality of life and diabetes. Diabetes Metab Res Rev. 1999;15:205-218. [PubMed] [DOI] [Full Text] |
| 72. | Jing X, Chen J, Dong Y, Han D, Zhao H, Wang X, Gao F, Li C, Cui Z, Liu Y, Ma J. Related factors of quality of life of type 2 diabetes patients: a systematic review and meta-analysis. Health Qual Life Outcomes. 2018;16:189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 145] [Cited by in RCA: 182] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 73. | Nord E, Daniels N, Kamlet M. QALYs: some challenges. Value Health. 2009;12 Suppl 1:S10-S15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 114] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 74. | Nelson KM, Reiber G, Boyko EJ; NHANES III. Diet and exercise among adults with type 2 diabetes: findings from the third national health and nutrition examination survey (NHANES III). Diabetes Care. 2002;25:1722-1728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 289] [Cited by in RCA: 287] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 75. | Duarte CK, Almeida JC, Merker AJ, Brauer Fde O, Rodrigues Tda C. Physical activity level and exercise in patients with diabetes mellitus. Rev Assoc Med Bras (1992). 2012;58:215-221. [PubMed] |
| 76. | Nor Shazwani MN Jr, Suzana S, Hanis Mastura Y, Lim CJ, Teh SC, Mohd Fauzee MZ, Lim HC, Dahlia S, Norliza M. Assessment of Physical Activity Level among Individuals with Type 2 Diabetes Mellitus at Cheras Health Clinic, Kuala Lumpur. Malays J Nutr. 2010;16:101-112. [PubMed] |
| 77. | Oyewole OO, Odusan O, Oritogun KS, Idowu AO. Physical activity among type-2 diabetic adult Nigerians. Ann Afr Med. 2014;13:189-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 78. | Oguntibeju OO, Odunaiya N, Oladipo B, Truter EJ. Health behaviour and quality of life of patients with type 2 diabetes attending selected hospitals in south western Nigeria. West Indian Med J. 2012;61:619-626. [PubMed] |
| 79. | Codogno JS, Fernandes RA, Sarti FM, Freitas Júnior IF, Monteiro HL. The burden of physical activity on type 2 diabetes public healthcare expenditures among adults: a retrospective study. BMC Public Health. 2011;11:275. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 80. | Chimen M, Kennedy A, Nirantharakumar K, Pang TT, Andrews R, Narendran P. What are the health benefits of physical activity in type 1 diabetes mellitus? A literature review. Diabetologia. 2012;55:542-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 288] [Article Influence: 22.2] [Reference Citation Analysis (0)] |
| 81. | Sigal RJ, Kenny GP, Wasserman DH, Castaneda-Sceppa C, White RD. Physical activity/exercise and type 2 diabetes: a consensus statement from the American Diabetes Association. Diabetes Care. 2006;29:1433-1438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 632] [Cited by in RCA: 584] [Article Influence: 30.7] [Reference Citation Analysis (0)] |
| 82. | Yang D, Yang Y, Li Y, Han R. Physical Exercise as Therapy for Type 2 Diabetes Mellitus: From Mechanism to Orientation. Ann Nutr Metab. 2019;74:313-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 77] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 83. | Thomas N, Alder E, Leese GP. Barriers to physical activity in patients with diabetes. Postgrad Med J. 2004;80:287-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 205] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 84. | Schmidt SK, Hemmestad L, MacDonald CS, Langberg H, Valentiner LS. Motivation and Barriers to Maintaining Lifestyle Changes in Patients with Type 2 Diabetes after an Intensive Lifestyle Intervention (The U-TURN Trial): A Longitudinal Qualitative Study. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 71] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 85. | Gao S, Yu L, Yi G, Li T, Chen Z, Ding J. Exercise Intervention as a Therapy in Patients with Diabetes Mellitus and Sarcopenia: A Meta-Analysis. Diabetes Ther. 2022;13:1311-1325. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 86. | Dempsey PC, Owen N, Yates TE, Kingwell BA, Dunstan DW. Sitting Less and Moving More: Improved Glycaemic Control for Type 2 Diabetes Prevention and Management. Curr Diab Rep. 2016;16:114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 120] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 87. | Ekelund U, Steene-Johannessen J, Brown WJ, Fagerland MW, Owen N, Powell KE, Bauman A, Lee IM; Lancet Physical Activity Series 2 Executive Committe; Lancet Sedentary Behaviour Working Group. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016;388:1302-1310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1462] [Cited by in RCA: 1666] [Article Influence: 185.1] [Reference Citation Analysis (0)] |
| 88. | Fritschi C, Bronas UG, Park CG, Collins EG, Quinn L. Early declines in physical function among aging adults with type 2 diabetes. J Diabetes Complications. 2017;31:347-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 89. | Brazo-Sayavera J, López-Torres O, Martos-Bermúdez Á, Rodriguez-Garcia L, González-Gross M, Guadalupe-Grau A. Effects of Power Training on Physical Activity, Sitting Time, Disability, and Quality of Life in Older Patients With Type 2 Diabetes During the COVID-19 Confinement. J Phys Act Health. 2021;18:660-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 90. | Dempsey PC, Dunstan DW, Larsen RN, Lambert GW, Kingwell BA, Owen N. Prolonged uninterrupted sitting increases fatigue in type 2 diabetes. Diabetes Res Clin Pract. 2018;135:128-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 91. | Hao W, Li J, Fu P, Zhao D, Jing Z, Wang Y, Yu C, Yuan Y, Zhou C. Physical frailty and health-related quality of life among Chinese rural older adults: a moderated mediation analysis of physical disability and physical activity. BMJ Open. 2021;11:e042496. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 92. | Hu W, Chu J, Chen X, Liu S, Sun N, Han Q, Li T, Feng Z, He Q, Shen Y. The role of depression and physical activity in the association of between sleep quality, and duration with and health-related quality of life among the elderly: a UK Biobank cross-sectional study. BMC Geriatr. 2022;22:338. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 22] [Reference Citation Analysis (0)] |
| 93. | Arena R, Sagner M, Byrne NM, Williams AD, McNeil A, Street SJ, Hills AP. Novel approaches for the promotion of physical activity and exercise for prevention and management of type 2 diabetes. Eur J Clin Nutr. 2017;71:858-864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 94. | Centers for Disease Control and Prevention. Strategies to Prevent Obesity and Other Chronic Diseases: The CDC Guide to Strategies to Increase Physical Activity in the Community. 2011. [cited 7 March 2023]. Available from: http://www.cdc.gov/obesity. |
| 95. | Tuso P. Strategies to Increase Physical Activity. Perm J. 2015;19:84-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 96. | Kaczynski AT, Wilhelm Stanis SA, Hipp JA. Point-of-decision prompts for increasing park-based physical activity: a crowdsource analysis. Prev Med. 2014;69:87-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 97. | Soler RE, Leeks KD, Buchanan LR, Brownson RC, Heath GW, Hopkins DH; Task Force on Community Preventive Services. Point-of-decision prompts to increase stair use. A systematic review update. Am J Prev Med. 2010;38:S292-S300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 96] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 98. | Gay JL, Cherof SA, LaFlamme CC, O'Connor PJ. Psychological Aspects of Stair Use: A Systematic Review. Am J Lifestyle Med. 2022;16:109-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 99. | Bellettiere J, Nguyen B, Liles S, Berardi V, Adams MA, Dempsey P, Benporat Y, Kerr J, LaCroix AZ, Hovell M. Prompts to increase physical activity at points-of-choice between stairs and escalators: what about escalator climbers? Transl Behav Med. 2019;9:656-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 100. | Domin A, Spruijt-Metz D, Theisen D, Ouzzahra Y, Vögele C. Smartphone-Based Interventions for Physical Activity Promotion: Scoping Review of the Evidence Over the Last 10 Years. JMIR Mhealth Uhealth. 2021;9:e24308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 47] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 101. | Coughlin SS, Whitehead M, Sheats JQ, Mastromonico J, Smith S. A Review of Smartphone Applications for Promoting Physical Activity. Jacobs J Community Med. 2016;2. [PubMed] |
| 102. | Stuckey MI, Carter SW, Knight E. The role of smartphones in encouraging physical activity in adults. Int J Gen Med. 2017;10:293-303. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 39] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 103. | Jee H. Review of researches on smartphone applications for physical activity promotion in healthy adults. J Exerc Rehabil. 2017;13:3-11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 104. | Chaddha A, Jackson EA, Richardson CR, Franklin BA. Technology to Help Promote Physical Activity. Am J Cardiol. 2017;119:149-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 105. | Tate DF, Lyons EJ, Valle CG. High-tech tools for exercise motivation: use and role of technologies such as the internet, mobile applications, social media, and video games. Diabetes Spectr. 2015;28:45-54. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 82] [Cited by in RCA: 67] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 106. | Woessner MN, Tacey A, Levinger-Limor A, Parker AG, Levinger P, Levinger I. The Evolution of Technology and Physical Inactivity: The Good, the Bad, and the Way Forward. Front Public Health. 2021;9:655491. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 79] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 107. | Lehr AL, Driver SL, Stone NJ. The ABCDs of Lifestyle Counseling. JAMA Cardiol. 2016;1:505-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |