Published online Apr 26, 2023. doi: 10.12998/wjcc.v11.i12.2708
Peer-review started: December 27, 2022
First decision: January 5, 2023
Revised: January 19, 2023
Accepted: March 29, 2023
Article in press: March 29, 2023
Published online: April 26, 2023
Processing time: 119 Days and 5.1 Hours
Risk stratification for patients with gastric precancerous lesions for endoscopic surveillance remains controversial.
To analysis of patients having developed gastric adenocarcinoma during the period of follow-up.
We conducted a retrospective study on patients having undergone upper endoscopy prior to the development of gastric adenocarcinoma. The presence and stage of precancerous lesions as well as subtype of intestinal metaplasia at the baseline endoscopy got evaluated. Literature mini-review was performed.
Out of 1681 subjects in the Biobank, gastric adenocarcinoma was detected in five cases in whom previous endoscopy data with biopsies either from the corpus or antral part were available. All of the patients had incomplete intestinal metaplasia during the baseline endoscopy; all three subjects in whom intestinal metaplasia subtyping was performed according to Filipe et al, had Type III intestinal metaplasia. Two of the five cases had low Operative Link on Gastritis Assessment (OLGA) and Operative Link on Gastritis Intestinal Metaplasia Assessment (OLGIM) stages (I-II) at the baseline.
The presence of incomplete intestinal metaplasia, in particular, that of Type III is a better predictor for gastric adenocarcinoma development than OLGA/OLGIM staging system. Subtyping of intestinal metaplasia have an important role in the risk stratification for surveillance decisions.
Core Tip: We present a retrospective case series and analysis of the available literature evidence on gastric mucosal precancerous lesion characteristics preceding gastric adenocarcinoma development. The obtained data are strongly suggesting that subtyping of gastric intestinal metaplasia, in particular that of Type III is an important predictor for the development of adenocarcinoma. The subtype of intestinal metaplasia appears to be a better predictor for cancer than Operative Link on Gastritis Assessment and Operative Link on Gastritis Intestinal Metaplasia Assessment staging system, however larger studies would be required to confirm this.
- Citation: Bogdanova I, Polaka I, Aleksandraviča I, Dzērve Z, Anarkulova L, Novika V, Tolmanis I, Leja M. Role of pre-existing incomplete intestinal metaplasia in gastric adenocarcinoma: A retrospective case series analysis. World J Clin Cases 2023; 11(12): 2708-2715
- URL: https://www.wjgnet.com/2307-8960/full/v11/i12/2708.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i12.2708
Atrophy, intestinal metaplasia and dysplasia are defined as precancerous lesions for gastric cancer, however the magnitude of risk for developing cancer may be substantially variable[1]. Surveillance strategies, i.e. repeated endoscopies in patients with such lesions is recommended in Europe[2]; yet substantial differences between the currently existing guidelines have to be noted[3]. The Operative Link on Gastritis Assessment (OLGA) and Operative Link on Gastritis Intestinal Metaplasia Assessment (OLGIM) have been suggested for easier use, and claimed to be a tool for better risk-stratification[4,5].
Based on a long-term follow-up study on 7436 patients in Italy, OLGA staging system was suggested to be a good predictor for gastric cancer development since most of the overall 28 incident neoplasia occurred in stages III and IV[6]. In another cohort study by the Italian investigators involving 1755 consecutive patients incident neoplastic lesions (prevalence - 0.4%; low-grade intraepithelial neoplasia - 4; high-grade intraepithelial neoplasia - 1; gastric cancer - 2) developed exclusively in patients with OLGA stages III-IV. A prospective, longitudinal multicenter study in Singapore involving 2980 subjects undergoing screening upper endoscopy with standardized gastric mucosal biopsy sampling has suggested patients with OLGIM III-IV lesions to be the highest risk-group for gastric neoplasia development (adjusted hazard ratio 20.7; 95%CI: 5.04-85.6) whereas OLGIM II group was identified to bear an intermediate risk[7].
A meta-analysis of six case-control studies and two cohort studies, comprising 2700 subjects has also demonstrated a significant association between the OLGA/OLGIM stages III/IV and gastric cancer risk[8].
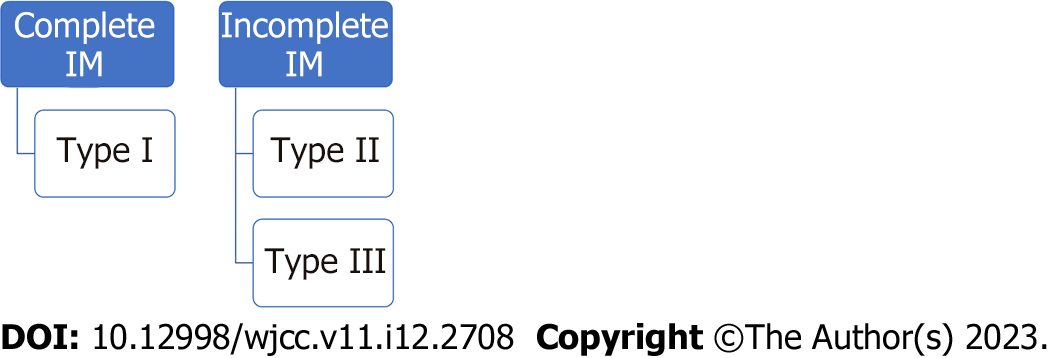
The potential role of gastric intestinal metaplasia subtyping has been debated for decades. The landmark study by Filipe et al[9] has suggested the role of a specific high-iron diamine alcian-blue (HID-AB) staining technique for assessing the presence of sialomucins and sulfomucins. However, currently the HID-AB method is available only in a few specialized laboratories. Intestinal metaplasia can be more broadly subtyped in complete and incomplete metaplasia based on the standard hematoxylin and eosin (H&E) staining method. Incomplete intestinal metaplasia corresponds to Type II and Type III intestinal metaplasia by Filipe taken together (Figure 1).
Based on the above, we have decided to check in our retrospective surveillance cohort the role of intestinal metaplasia subtypes in gastric cancer development as well as to review the studies in the literature that have assessed subtypes of intestinal metaplasia prior to cancer development. The secondary objective was to assess the correlation to high-risk OLGA/OLGIM stages for assuring whether OLGA and/or OLGIM staging system could serve as the single reliable parameter for risk assessment.
We requested data on gastric cancer (C16) entries to the Cancer Registry of Latvia from individuals having been enrolled to the Biobank of the Clinical and Preventive Medicine, University of Latvia and having undergone upper endoscopy in the Digestive Diseases Centre GASTRO, Riga, Latvia. Patient enrolment to the biobank was initiated in 2007, the follow-up period according to the Registry data was ending December 2020. At the time of enrolment to the Biobank all the study subjects have provided their signed consent allowing their data to be analysed following the enrolment.
For the selected cases, the medical history available in the Digestive Diseases Centre GASTRO was analysed; this included preceding and follow-up endoscopy data. Only patients having undergone upper endoscopy prior to the diagnosis of gastric cancer and having been biopsied from the corpus and antrum during the endoscopy were included to the analysis. Those having been diagnosed with other type of malignancies than gastric adenocarcinoma were excluded.
Consequently, in the selected group of patients, endoscopy biopsy results were re-evaluated in the Academic Histology Laboratory, Riga, Latvia.
Only cases with biopsies available from the corpus and antrum were included to the analysis; incisura biopsy was also available as the standard. Routinely, staining with H&E was used for the clinical work-up. Whenever available, all the slides from the selected cases were re-analysed. Whenever the paraffin blocks were available, additional slides for HID-AB staining were produced, and the subtypes of intestinal metaplasia according to Filipe et al[9] were analysed.
Complete intestinal metaplasia is known also as small intestinal type, is characterized by the presence of absorptive cells with brush borders, goblet cells and occasionally Paneth cells, while incomplete intestinal metaplasia, known also as colonic type intestinal metaplasia – by the presence of hybrid mucous cells with large vacuoles of different sizes, without features of absorptive cells or goblet cells[10]. When both subtypes are present (mixed intestinal metaplasia), the case is classified according the lesions of the highest risk, i.e. incomplete metaplasia.
According to the HID-AB stain, in Type I intestinal metaplasia sialomucins are present in goblet cells with no mucins in columnar cells; in Type II – sialomucins are present in goblet and columnar cells, while in Type III - sulfomucins predominate in columnar cells, and goblet cells may contain sialomucins or sulfomucins[11].
Out of 1681 subjects in the Biobank (median age 59 years, 68% women, Helicobacter pylori (H. pylori) positivity – 56.8% according to histology, 13% had reported gastric cancer among the 1st degree relatives, median follow-up period 9.1 years), gastric adenocarcinoma was detected in five cases fulfilling the inclusion criteria described above. Of those, 4 were women, 1 man, one woman was a current smoker, while another one – past smoker; three have reported modest use of alcohol, one had a first degree relative with a gastric cancer; the mean age at cancer development was 75.6 years (range 53-90 years). The mean period of cancer detection was 52 mo (range 25-70 mo) following the initial endoscopy. In all, but one case several upper endoscopies have been performed during the follow-up period. Four of the five cases were H. pylori positive according to the histology of the preceding endoscopy, the only H. pylori – negative subject was not self-reporting previous eradication therapy. For more details, see Table 1.
| No. | Gender | Age at cancer development | Year of enrolment | Year of cancer diagnosis | Year of death | No. of preceding upper endoscopies | Number of months of the reference endoscopy prior to cancer development | Reference endoscopy (highest risk lesion in the case of several preceding endoscopies) | Grade of the cancer | ||||
| Dysplasia | OLGA stage | OLGIM stage | Complete/incomplete intestinal metaplasia | Intestinal metaplasia according to Filipe et al[9] (highest grade) | |||||||||
| 1 | Female | 88 | 2008 | 2012 | 2013 | 1 | 52 | No | II | II | Incomplete | NA | NA |
| 2 | Male | 53 | 2011 | 2016 | Alive | 3 | 70 | High-grade | III | III | Incomplete | III | Grade 1 |
| 3 | Female | 72 | 2010 | 2014 | 2015 | 3 | 48 | High-grade | I | I | Incomplete | NA | Grade 3 |
| 4 | Female | 90 | 2008 | 2019 | 2020 | 4 | 65 | No | III | II | Incomplete | III | Grade I |
| 5 | Female | 75 | 2007 | 2021 | Alive | 2 | 25 | No | II | II | Incomplete | III | Grade 1 |
Patient No. 2 was the only case in which early gastric cancer was diagnosed, got the diagnosis set within a surveillance program, and was successfully managed by endoscopic submucosal resection.
At the reference endoscopy, i.e. an endoscopy prior to the cancer diagnosis with the highest-risk lesion, two patients were diagnosed with a high-grade dysplasia while the remaining three did not have any degree of dysplasia. One of the two with high-grade dysplasia was also classified as OLGA and OLGIM Stage III, while the other one – OLGA and OLGIM Stage I only. In the entire group, only two patients were stages as OLGA III (one of them – OLGIM II), whereas the majority, i.e. three cases were low OLGA and OLGIM risk stages (I and II).
In three cases in the group the material was available for an additional HID-AB staining: All three cases were diagnosed as Type III intestinal metaplasia according to Filipe et al[9].
Our retrospective cohort analysis was suggesting that incomplete intestinal metaplasia of the stomach mucosa, in particular, that of Type III according to Filipe et al[9], is a key predictor of gastric adenocarcinoma development.
The results in our case series of five patients having developed gastric cancer during the follow-up period is confirming the rationale for endoscopic surveillance strategies of patients with gastric precancerous lesions as suggested by the current guidelines[2]. Three of these patients had clearly high-risk precancerous lesions (high grade dysplasia in two cases, and an addition subject with a high-risk OLGA/OLGIM stage) at the initial investigations, whereas in two cases surveillance would not been indicated unless considering the subtype of intestinal metaplasia. Both were diagnosed as OLGA and OLGIM II stage cases at the enrolment. In all the five cases incomplete intestinal metaplasia was present at the enrolment, and in all the subjects in whom HID-AB staining was available – the intestinal metaplasia was subtyped as Type III. Therefore, based on this very small cohort, subtyping of intestinal metaplasia seems to be a more important factor for risk stratification that OLGA and OLGIM staging.
Increasing evidence is becoming available on the role of intestinal metaplasia subtyping for gastric cancer risk stratification. A 20-year follow-up study of the population-based cohort in Colombia has suggested that the presence of incomplete intestinal at baseline substantially increased the risk (OR, 13.4; 95%CI: 1.8-103.8) for gastric cancer development when compared to subjects with a complete intestinal metaplasia at the enrolment[12].
In the Spanish multi-center study having involved 649 patients with gastric precancerous lesions at baseline 24 patients had developed gastric adenocarcinoma during the mean follow-up period of 12 years. The hazards ratio of progression to gastric cancer was 2.75 (95%CI: 1.06-6.26) for those with incomplete compared with those with complete intestinal metaplasia at baseline, after adjusting for sex, age, smoking, family history of gastric cancer and the use of non-steroidal anti-inflammatory medication[10]. HID-AB staining was not used in the study.
These observations are supported by other studies. In France, a low gastric cancer risk country, progression towards gastric cancer was observed in two cases, both of them – had antrum limited disease (one was OLGA II, the other, - OLGA III stage), but incomplete intestinal metaplasia at the initial endoscopy[13].
In a study from Japan altogether 4 patients have been progressing to gastric cancer during the observational period following H. pylori eradication; all of these patients had incomplete intestinal metaplasia in the antral part of the stomach at the enrolment[14]. This group of researchers were using immunohistochemical staining for differentiating between the subtypes of intestinal metaplasia. Interestingly, the key objective of the study was addressing the reversibility of intestinal metaplasia; the obtained results were suggesting that incomplete intestinal metaplasia in the antrum was regressing within a 10-year period following the eradication whereas complete intestinal metaplasia did not regress either in the antrum or corpus[14].
The study that has been conducted by our group in healthy individuals from Kazakhstan, a country with high incidence of gastric cancer, has suggested that limiting the patient surveillance of those with high OLGA or OLGIM stages may result in substantial downgrading of the risk, and therefore missing patients with high risk for surveillance as a substantial proportion of subjects with low stages according to the above classifications had incomplete intestinal metaplasia[15].
Recently two meta-analysis on the subtypes of gastric intestinal metaplasia and neoplasia risk have been published by researchers from China – Du et al[16] has been including cohort studies (published until May 15, 2021) while Wei et al[17] included also case-control studies, and the analysis period was ending March 2020. Both analysis obtained similar findings. Pooled relative risk for gastric cancer development of incomplete intestinal metaplasia when compared to complete type was 5.16 (95%CI: 3.28-8.12) in the study by Du et al[16], and 4.96 (95%CI: 2.72-9.04) in the study by Wei et al[17] Both studies revealed the highest risk of progression to cancer in Type III intestinal metaplasia, i.e. 6.27 (95%CI: 1.89-20.77) in the analysis by Wei et al[17] when compared Types I and II combined, while 6.42 (95%CI: 3.03-13.62) in the analysis by Du et al[16] when compared to Type I intestinal metaplasia.
There are certain limitations to our and other studies. The numbers of study subjects either in our case series or in other cohorts, including the study from France[13], are low. Besides, there is a very limited number of laboratories that are currently using the HID-AB staining method; also in some of our patients the material was not available to apply this staining method in all. Larger series would be required for definite conclusions; European-level data collaborative for pooling the results from various studies whether published or unpublished, would be a powerful tool for the purpose.
Finally, the relevance of intestinal metaplasia subtyping has been gradually acknowledged by international guidelines. There is limited awareness among gastroenterologists of the potential prognostic value of the histological subtyping of IM[11], and therefore, the pathologists are frequently not reporting the subtypes even though this would be important for setting the most appropriate surveillance endoscopy intervals. The latest version of MAPS (II) guideline acknowledges the role of incomplete intestinal metaplasia[2], while this was discouraged in the initial version[18]. Although referring to MAPS II, the recent Maastricht VI guideline suggests subtyping of intestinal metaplasia is clinically redundant if using OLGA/OLGIM staging systems[5], which actually contradicts our findings and the above discussed evidence. We expect that increasing knowledge in the field should result in changes to upcoming editions of these guidelines.
Proper risk stratification of precancerous lesions of the stomach mucosa is important for determining the optimal surveillance strategies. The presence of incomplete intestinal metaplasia, in particular that of Type III is a better predictor for gastric adenocarcinoma development than OLGA/OLGIM staging system. Subtyping of intestinal metaplasia may have an important role in the risk stratification for surveillance decisions. Large-scale international data collaborative may be of importance to address the above issues.
Gastric cancer is still remaining an important burden of the global health. Proper stratification of precancerous lesions is of significant importance for scheduling surveillance endoscopic investigations.
To address the role of intestinal metaplasia subtyping in clinical settings.
To investigate the subtypes of intestinal metaplasia during an endoscopy that was performed prior to cancer development in a retrospective cohort.
Retrospective analysis of patients having been diagnosed with gastric cancer following a past endoscopic assessment (without cancer).
Incomplete type intestinal metaplasia was present in all patients having developed cancer. In all three patients in whom the subtyping of intestinal metaplasia was performed according to Filipe et al, Type III intestinal metaplasia was present.
Subtyping of gastric intestinal metaplasia is important for clinical practice.
Larger-scale case-controlled studies would be required to support the conclusions.
We acknowledge the patients having supported their longitudinal data to be analysed as well as the services of the Biobank commonly run by the Institute of Clinical and Preventive Medicine, University of Latvia and Riga East University Hospital. Our thanks to Maria Blanca Piazuelo who has supported the implementation of high-iron diamine alcian-blue staining at the Academic Histology Laboratory and Sergejs Isajevs for the implementation of the method.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Latvia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bakır M, Turkey; Cheng H, China S-Editor: Liu JH L-Editor: A P-Editor: ChenYX
| 1. | de Vries AC, van Grieken NC, Looman CW, Casparie MK, de Vries E, Meijer GA, Kuipers EJ. Gastric cancer risk in patients with premalignant gastric lesions: a nationwide cohort study in the Netherlands. Gastroenterology. 2008;134:945-952. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 483] [Cited by in RCA: 583] [Article Influence: 34.3] [Reference Citation Analysis (0)] |
| 2. | Pimentel-Nunes P, Libânio D, Marcos-Pinto R, Areia M, Leja M, Esposito G, Garrido M, Kikuste I, Megraud F, Matysiak-Budnik T, Annibale B, Dumonceau JM, Barros R, Fléjou JF, Carneiro F, van Hooft JE, Kuipers EJ, Dinis-Ribeiro M. Management of epithelial precancerous conditions and lesions in the stomach (MAPS II): European Society of Gastrointestinal Endoscopy (ESGE), European Helicobacter and Microbiota Study Group (EHMSG), European Society of Pathology (ESP), and Sociedade Portuguesa de Endoscopia Digestiva (SPED) guideline update 2019. Endoscopy. 2019;51:365-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 712] [Cited by in RCA: 666] [Article Influence: 111.0] [Reference Citation Analysis (0)] |
| 3. | Matysiak-Budnik T, Camargo MC, Piazuelo MB, Leja M. Recent Guidelines on the Management of Patients with Gastric Atrophy: Common Points and Controversies. Dig Dis Sci. 2020;65:1899-1903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Rugge M, Capelle LG, Cappellesso R, Nitti D, Kuipers EJ. Precancerous lesions in the stomach: from biology to clinical patient management. Best Pract Res Clin Gastroenterol. 2013;27:205-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 83] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 5. | Malfertheiner P, Megraud F, Rokkas T, Gisbert JP, Liou JM, Schulz C, Gasbarrini A, Hunt RH, Leja M, O'Morain C, Rugge M, Suerbaum S, Tilg H, Sugano K, El-Omar EM; European Helicobacter and Microbiota Study group. Management of Helicobacter pylori infection: the Maastricht VI/Florence consensus report. Gut. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 744] [Cited by in RCA: 630] [Article Influence: 210.0] [Reference Citation Analysis (0)] |
| 6. | Rugge M, Genta RM, Fassan M, Valentini E, Coati I, Guzzinati S, Savarino E, Zorzi M, Farinati F, Malfertheiner P. OLGA Gastritis Staging for the Prediction of Gastric Cancer Risk: A Long-term Follow-up Study of 7436 Patients. Am J Gastroenterol. 2018;113:1621-1628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 98] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 7. | Lee JWJ, Zhu F, Srivastava S, Tsao SK, Khor C, Ho KY, Fock KM, Lim WC, Ang TL, Chow WC, So JBY, Koh CJ, Chua SJ, Wong ASY, Rao J, Lim LG, Ling KL, Chia CK, Ooi CJ, Rajnakova A, Yap WM, Salto-Tellez M, Ho B, Soong R, Chia KS, Teo YY, Teh M, Yeoh KG. Severity of gastric intestinal metaplasia predicts the risk of gastric cancer: a prospective multicentre cohort study (GCEP). Gut. 2022;71:854-863. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 68] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 8. | Yue H, Shan L, Bin L. The significance of OLGA and OLGIM staging systems in the risk assessment of gastric cancer: a systematic review and meta-analysis. Gastric Cancer. 2018;21:579-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 114] [Article Influence: 16.3] [Reference Citation Analysis (1)] |
| 9. | Filipe MI, Muñoz N, Matko I, Kato I, Pompe-Kirn V, Jutersek A, Teuchmann S, Benz M, Prijon T. Intestinal metaplasia types and the risk of gastric cancer: a cohort study in Slovenia. Int J Cancer. 1994;57:324-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 298] [Cited by in RCA: 294] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 10. | González CA, Sanz-Anquela JM, Companioni O, Bonet C, Berdasco M, López C, Mendoza J, Martín-Arranz MD, Rey E, Poves E, Espinosa L, Barrio J, Torres MÁ, Cuatrecasas M, Elizalde I, Bujanda L, Garmendia M, Ferrández Á, Muñoz G, Andreu V, Paules MJ, Lario S, Ramírez MJ; Study group, Gisbert JP. Incomplete type of intestinal metaplasia has the highest risk to progress to gastric cancer: results of the Spanish follow-up multicenter study. J Gastroenterol Hepatol. 2016;31:953-958. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 70] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 11. | Shah SC, Gawron AJ, Mustafa RA, Piazuelo MB. Histologic Subtyping of Gastric Intestinal Metaplasia: Overview and Considerations for Clinical Practice. Gastroenterology. 2020;158:745-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 53] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 12. | Piazuelo MB, Bravo LE, Mera RM, Camargo MC, Bravo JC, Delgado AG, Washington MK, Rosero A, Garcia LS, Realpe JL, Cifuentes SP, Morgan DR, Peek RM Jr, Correa P, Wilson KT. The Colombian Chemoprevention Trial: 20-Year Follow-Up of a Cohort of Patients With Gastric Precancerous Lesions. Gastroenterology. 2021;160:1106-1117.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 80] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 13. | Chapelle N, Péron M, Quénéhervé L, Bourget A, Leroy M, Touchefeu Y, Cauchin E, Coron E, Mosnier JF, Matysiak-Budnik T. Long-Term Follow-up of Gastric Precancerous Lesions in a Low GC Incidence Area. Clin Transl Gastroenterol. 2020;11:e00237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 14. | Wada Y, Kodama M, Mizukami K, Okimoto T, Fuchino T, Tsutsumi K, Fukuda M, Hirashita Y, Fukuda K, Okamoto K, Ogawa R, Kushima R, Murakami K. Differences in Regression Patterns of Complete and Incomplete Intestinal Metaplasia at Ten Years after Helicobacter pylori Eradication. Acta Histochem Cytochem. 2021;54:185-194. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Isajevs S, Savcenko S, Liepniece-Karele I, Piazuelo MB, Kikuste I, Tolmanis I, Vanags A, Gulbe I, Mezmale L, Samentaev D, Tazedinov A, Samsutdinov R, Belihina T, Igissinov N, Leja M. High-risk individuals for gastric cancer would be missed for surveillance without subtyping of intestinal metaplasia. Virchows Arch. 2021;479:679-686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 16. | Du S, Yang Y, Fang S, Guo S, Xu C, Zhang P, Wei W. Gastric Cancer Risk of Intestinal Metaplasia Subtypes: A Systematic Review and Meta-Analysis of Cohort Studies. Clin Transl Gastroenterol. 2021;12:e00402. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Wei N, Zhou M, Lei S, Zhong Z, Shi R. A meta-analysis and systematic review on subtypes of gastric intestinal metaplasia and neoplasia risk. Cancer Cell Int. 2021;21:173. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Dinis-Ribeiro M, Areia M, de Vries AC, Marcos-Pinto R, Monteiro-Soares M, O'Connor A, Pereira C, Pimentel-Nunes P, Correia R, Ensari A, Dumonceau JM, Machado JC, Macedo G, Malfertheiner P, Matysiak-Budnik T, Megraud F, Miki K, O'Morain C, Peek RM, Ponchon T, Ristimaki A, Rembacken B, Carneiro F, Kuipers EJ; European Society of Gastrointestinal Endoscopy; European Helicobacter Study Group; European Society of Pathology; Sociedade Portuguesa de Endoscopia Digestiva. Management of precancerous conditions and lesions in the stomach (MAPS): guideline from the European Society of Gastrointestinal Endoscopy (ESGE), European Helicobacter Study Group (EHSG), European Society of Pathology (ESP), and the Sociedade Portuguesa de Endoscopia Digestiva (SPED). Endoscopy. 2012;44:74-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 442] [Cited by in RCA: 486] [Article Influence: 37.4] [Reference Citation Analysis (0)] |