Published online Apr 16, 2023. doi: 10.12998/wjcc.v11.i11.2576
Peer-review started: February 19, 2023
First decision: February 28, 2023
Revised: March 7, 2023
Accepted: March 17, 2023
Article in press: March 17, 2023
Published online: April 16, 2023
Processing time: 45 Days and 21.5 Hours
Primary cancer of the appendix is rare and often difficult to diagnose preoperatively due to the lack of specific clinical symptoms. Autoimmune encephalitis (AIE) is the most common cause of non-infectious encephalitis. The etiologies of AIE include tumors (paraneoplastic), infections (parainfections), or recessive infections. The tumors that have been reported to cause AIE include thymomas, ovarian teratomas, lung cancers, and breast cancers. However, there are no reports of AIE occurring after surgery for appendiceal cancer. This report describes the diagnosis and treatment of a patient with an appendiceal cancer and postoperative AIE.
We report the case of a 47-year-old man who was transferred to our hospital due to a recurrent low intestinal obstruction. Abdominal enhanced computed tomography was used to consider the possibility of a terminal ileal tumor with serous infiltration and lymph node metastasis. A right hemi-colectomy was performed under general anesthesia with an ileo-transcolon anastomosis and laparoscopic exploration. The postoperative pathologic evaluation revealed a high-grade goblet cell carcinoma of the appendix, accompanied by mesangial and abdominal lymph node metastases, and neural tube and vascular infiltration. The operation was completed without complication. The patient developed restlessness on postoperative day 4, and gradually developed a disturbance of consciousness on postoperative day 6. He was transferred to West China Hospital of Sichuan University and diagnosed with AIE.
Albeit rare, the occurrence of neurologic and psychiatric symptoms in patients with an appendiceal cancer postoperatively suggests the possibility of AIE.
Core Tip: Tumors (paraneoplastic) are one of the etiologies of autoimmune encephalitis (AIE). However, there are no reports of AIE occurring after surgery for appendiceal cancer. This report we describes a 47-year-old man who was transferred to our hospital due to a recurrent low intestinal obstruction and a right hemi-colectomy was performed with an ileo-transcolon anastomosis and laparoscopic exploration. But he developed a disturbance of consciousness on postoperative day 6, and diagnosed with AIE at last. We report this case in the hope of giving some guidance to clinicians with similar challenging cases.
- Citation: Mao YH, Li L, Wen LM, Qin JM, Yang YL, Wang L, Wang FR, Zhao YZ. Autoimmune encephalitis after surgery for appendiceal cancer: A case report. World J Clin Cases 2023; 11(11): 2576-2581
- URL: https://www.wjgnet.com/2307-8960/full/v11/i11/2576.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i11.2576
Primary appendiceal cancer is rare and an incidental finding after an appendectomy for acute appendicitis in most cases[1]. Autoimmune encephalitis (AIE) is considered one of the most common causes of non-infectious acute encephalitis[2]; however, AIE after an appendectomy has not been reported. In this case report, a 47-year-old man with appendiceal cancer developed a disturbance of consciousness postoperatively and was diagnosed with AIE. The purpose of this report was to detail the evolution and diagnosis of the patient.
A 47-year-old male was admitted to our hospital for evaluation of abdominal distension, and difficulty exhaling and defecating for > 1 mo.
The patient had repeated intestinal obstruction for > 1 mo. Plain abdominal radiographs and an enhanced abdominal computed tomography (CT) indicated a low intestinal obstruction. A gastroendoscopy did not reveal abnormal findings. The patient was treated with fasting, fluid rehydration, and enemas. The symptoms improved and the patient was discharged to home; however, the symptoms recurred again 1 wk before admission in addition to vomiting. The patient was re-admitted to our hospital for further evaluation and treatment. The patient underwent a right hemi-colectomy under general anesthesia with an ileointestine-transverse colon anastomosis and laparoscopic exploration. The operation was completed without complications. On day 4 postoperatively the patient developed restlessness and gradually exhibited a disturbance of consciousness on day 6 postoperatively. Laboratory testing and imaging studies did not reveal the underlying cause. Based on our experience and a review of the literature, this case appeared to be unique.
The medical history was negative for cancer, surgery (other than the right hemi-colectomy with ileointestine-transverse colon anastomosis), hypertension, diabetes, and hyperlipidemia.
The patient admitted to smoking five cigarettes daily for > 20 years. The remaining personal and family histories were non-contributory.
The abdomen was flat and no peristaltic wave was observed. The right lower abdomen was tender without rebound pain or muscle tension. No obvious air or water sounds were heard during auscultation; the bowel sounds were approximately 6 times/min.
The routine hematologic and biochemistry profiles, and the tumor marker, carcinoembryonic antigen, were all in the normal range. The gamma interferon release test results were as follows: McCl-ifn (N): 24.52 pg/mL; McCl-ifn (T): 39.6 pg/mL; McCl-ifn (P): 5000 pg/mL; γ-interferon (IFN) (T-N): 15.08 pg/mL; γ-IFN (P-N): 4975.48 pg/mL; TB-TGRA (+); PPD (-); and TB antibody (-). On day 2 postoperatively, routine hematologic testing revealed the following: White blood cell, 12.38 × 109; and neutrophils, 85%. The blood gas analysis and electrolytes were normal. On day 4 postoperatively, electroencephalogram (EEG) with epileptic or slow-wave activity involving the temporal lobes.
When transferred to West China Hospital of Sichuan University, antibodies against intraneuronal antigens (INAab), a well-characterized autoantibodies was found in cerebrospinal fluid (CSF).
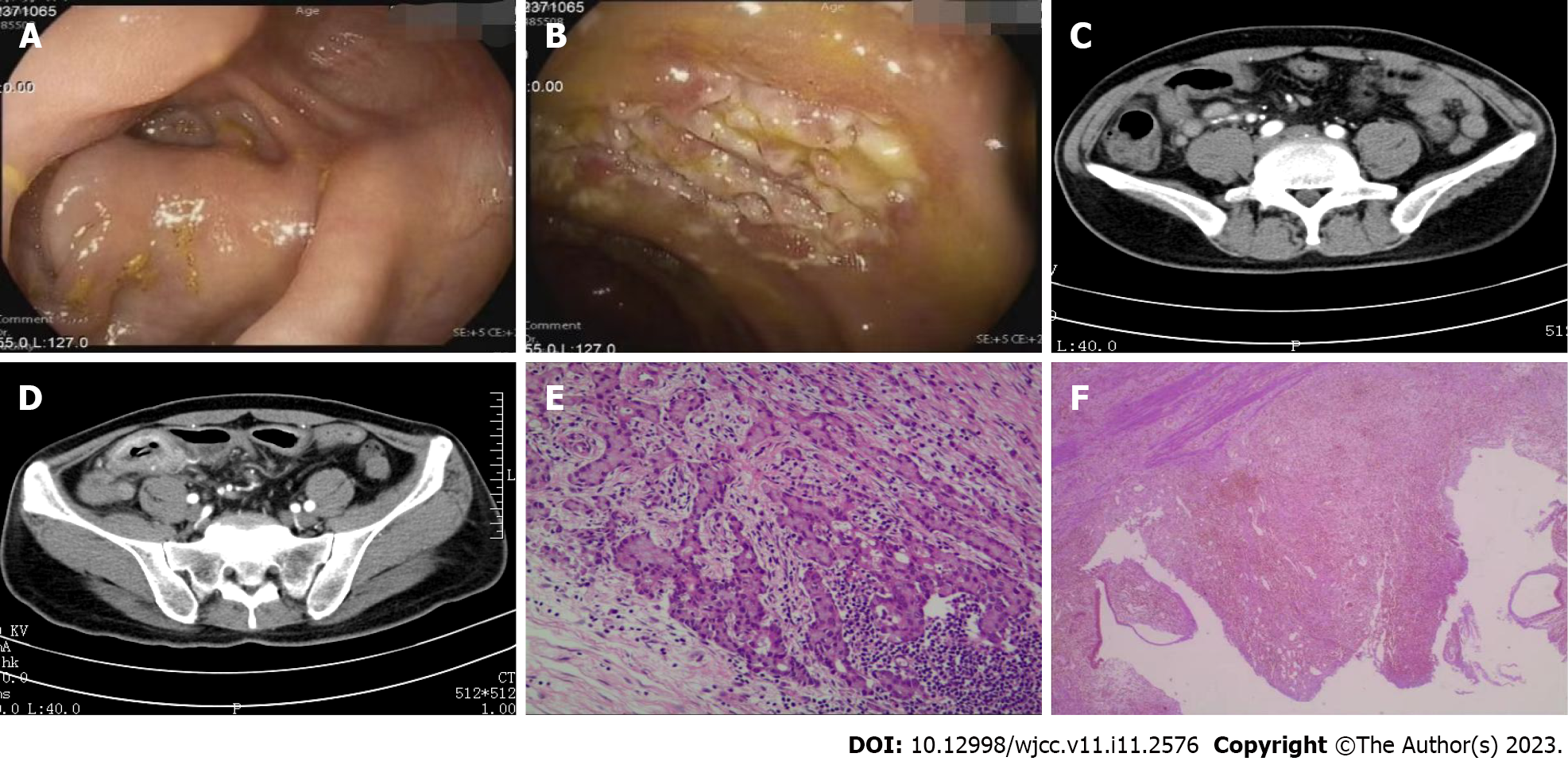
Colonoscopy revealed no abnormalities in the ileocecum (Figure 1A), but multiple ulcers were noted in the distal ileum (Figure 1B), consistent with inflammation on pathologic evaluation. A whole-abdominal enhanced CT indicated that the wall of the distal ileum was thickened with abnormal enhancement with multiple enlarged lymph nodes (Figure 1C). The possibility of neoplastic lesions involving the serous surface and the fat space were considered (Figure 1D).
The postoperative pathologic evaluation indicated high-grade goblet cell adenocarcinoma of the appendix, invasion of the mesangium of the appendix, and involvement of the cecum wall. Metastases were noted in six of 21 peri-ileal lymph nodes and one of two peri-ileocecal lymph nodes (Figure 1E). The terminal ileum was characterized by chronic active inflammation, necrosis, granulation tissue hyperplasia, and chronic ulcer formation (Figure 1F). A cranial CT scan showed no abnormalities. A cranial magnetic resonance imaging (MRI) indicated abnormal symmetric signals of the bilateral para-median thalamus, and midbrain aqueduct and brain stem adjacent to the fourth ventricle, which was consistent with a metabolic encephalopathy; however, the cranial CT and MRI did not fully explain the consciousness disorder.
The final diagnosis was therefore a goblet cell adenocarcinoma of the appendix with multiple metastases (T4N2Mx), AIE, incomplete ileus, and multiple ulcers in the terminal ileum.
Based on the patient signs and symptoms, physical examination, medical history, and auxiliary examinations, the patient underwent a right hemi-colectomy under general anesthesia with an ileointestine-transverse colon anastomosis and laparoscopic exploration. The operation was completed without complication. On postoperative day 2, the blood gas analysis and electrolyte levels were normal. A routine hematologic profile showed white blood cell count of 12.38 × 109 with 85% neutrophils. Despite no symptoms suggestive of an infection, such as a fever, anti-infection treatment was initiated. The hematologic profile returned to normal after the follow-up review. The patient had no specific complaints, but was uncomfortable. On postoperative day 4, the patient became noticeably restless. A complete cranial CT showed no abnormalities. A neurology consultation was obtained to rule out epilepsy; a sedative was administered. After brief improvement, the symptoms worsened until postoperative day 6 when the patient appeared to have a disorder of consciousness. The postoperative pathologic evaluation indicated a high-grade goblet cell adenocarcinoma of the appendix, invasion of the mesangium of the appendix, and involvement of the cecum wall. Metastases were noted in 6 of 21 peri-ileal lymph nodes and 1 of 2 peri-ileocecal lymph nodes. The terminal ileum revealed chronic active inflammation, necrosis, granulation tissue hyperplasia, and chronic ulcer formation. After a multidisciplinary meeting, it was concluded that encephalitis, metabolic encephalopathy, and tumor brain metastases could not be excluded. Thus, a CSF examination and EEG were recommended; however, the patient and the patient’s family requested further treatment at a higher authority hospital. After the patient was transferred to West China Hospital, antibodies against INAab, a well-characterized autoantibodies was found in CSF, the diagnosis of AIE was confirmed. The patient received methylprednisolone (1 g × 5 d) and immunoglobulin (0.4 g/kg/day × 5 d).
At the West China Hospital, the patient’s level of consciousness returned to baseline, but functional limitations persisted. Due to financial reasons, further review and chemotherapy were not performed. The patient died 10 mo later.
Primary appendiceal cancer is rare and most often an incidental finding on a surgical specimen from an appendectomy for acute appendicitis[1]. The 5-year survival rate of appendiceal cancer is 57.0%-64.0%; the prognosis is slightly worse than the prognosis for colon and rectal cancers[3]. The prognosis for primary appendiceal cancer mainly reflects the lack of specific clinical symptoms and early diagnostic methods. Indeed, primary appendiceal cancer is not easy to diagnose in the early stage or even preoperatively, and the symptoms are similar to acute appendicitis. The clinical manifestations of appendicitis account for 37.2% of patients with appendiceal cancer, and 23% of patients with appendiceal cancer are diagnosed after surgery[4]. Second, due to the anatomic characteristics of the appendix, the local muscular layer and submucosa are thin and rich in lymphatic tissue, which may lead to early lymph node metastases[5]. Appendiceal cancer can be classified into four subtypes: Colonic-type adenocarcinoma; mucinous neoplasms; goblet cell carcinoma (GCC); and neuroendocrine neoplasm[1]. GCC occurs almost exclusively in the appendix and is characterized by epithelial (adenocarcinoma) and neuroendocrine components containing goblet cells. GCC produces neuroendocrine markers and mucin. GCC is often asymptomatic and is often an incidental finding during the routine management of acute appendicitis. The clinical presentation is variable and can be an acute right fossa iliac syndrome or a more chronic abdominal pain syndrome with a palpable pelvic mass[6]. In the present case, repeated ileus was the main manifestation, which has not been reported previously.
Endoscopy is not expected to be sufficient for detection of early appendiceal cancer. It has been reported that there is a low detection rate of 11% for appendiceal abnormalities and 19% for cecal abnormalities in patients with appendiceal cancer[7]. CT findings of appendiceal cancer include appendiceal enlargement ≥ 15 mm, wall thickening, a soft tissue mass, and peri-appendiceal fat[8]. When a possibly submucosal invasive tumor is noted in the cecum, it is important to carefully observe around the appendix orifice. In the present case, multiple ulcers were observed in the terminal ileum during endoscopy. A neoplastic lesion was considered based on CT findings. The endoscopic findings were consistent with the CT findings, so we initially suspected a terminal ileal tumor. A retrospective review of the endoscopic and CT images showed swelling around the appendiceal foramen (Figure 1A and C); however, careful inspection of the appendiceal orifice was not performed. Some endoscopists do not pay attention to the appendiceal orifice drawing, which should be noted in future work.
AIE is one of the most common causes of non-infectious encephalitis. Suggested mechanisms that may trigger AIE include tumors (paraneoplastic), infections (parainfectious), or cryptogenic infections[8], which predominantly affects children and young females. Studies have shown that tumor-induced AIE is likely due to the production of antibodies against INAab, which are probably not directly pathogenic, but an epiphenomenon of a T-cell-mediated immune response[9]. The tumors that induce AIE which have been reported in the literature include thymomas, ovarian teratomas, lung cancer, and breast cancer; however, AIE induced by appendiceal cancer has not been reported. Experts agree that if relevant tumors are found, tumor treatment (chemotherapy or tumor resection) is essential, and all patients with AIE should be screened for tumors at the time of disease onset[9]. This patient subsequently discontinued chemotherapy; it is possible that chemotherapy can prolong survival. Unlike cases, the patient described herein developed AIE after radical tumor resection. The underlying mechanism is unclear, perhaps because the tumor was removed, while some cytokines were released into the blood during the process, thus inducing an immune chain effect. This possible explanation warrants further analysis with a large-scale corollary study. We report this case in the hope of giving some guidance to clinicians with similar challenging cases.
Albeit rare, the occurrence of neurologic and psychiatric symptoms in patients with an appendiceal cancer postoperatively suggests the possibility of AIE. The underlying mechanism of AIE in this patient after radical tumor resection is unclear, and that's what we need to figure out in the future.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Chinese Society of Gastroenterology.
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Glumac S, Croatia; Rocha R, Brazil S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Van de Moortele M, De Hertogh G, Sagaert X, Van Cutsem E. Appendiceal cancer : a review of the literature. Acta Gastroenterol Belg. 2020;83:441-448. [PubMed] [DOI] [Full Text] |
| 2. | Dutra LA, Abrantes F, Toso FF, Pedroso JL, Barsottini OGP, Hoftberger R. Autoimmune encephalitis: a review of diagnosis and treatment. Arq Neuropsiquiatr. 2018;76:41-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 71] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 3. | Ko YH, Park SH, Jung CK, Won HS, Hong SH, Park JC, Roh SY, Woo IS, Kang JH, Hong YS, Byun JH. Clinical characteristics and prognostic factors for primary appendiceal carcinoma. Asia Pac J Clin Oncol. 2010;6:19-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Benedix F, Reimer A, Gastinger I, Mroczkowski P, Lippert H, Kube R; Study Group Colon/Rectum Carcinoma Primary Tumor. Primary appendiceal carcinoma--epidemiology, surgery and survival: results of a German multi-center study. Eur J Surg Oncol. 2010;36:763-771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 111] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 5. | Katayama R, Aoki T, Tomioka K, Tashiro Y, Fujimasa K, Ono K, Kitajima T, Yoshizawa S, Ozawa Y, Matsuda K, Kusano T, Koizumi T, Watanabe M, Murakami M. A rare case of synchronous appendiceal and cecal cancer. Clin J Gastroenterol. 2021;14:1443-1447. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Vincenti L, Andriola V, Cazzato G, Colagrande A, Fiore F. Goblet Cell Carcinoma of the Appendix with Synchronous Adenocarcinoma of the Cecum: Distinct or Related Entities? Diseases. 2022;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Trivedi AN, Levine EA, Mishra G. Adenocarcinoma of the appendix is rarely detected by colonoscopy. J Gastrointest Surg. 2009;13:668-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 50] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 8. | Chiou YY, Pitman MB, Hahn PF, Kim YH, Rhea JT, Mueller PR. Rare benign and malignant appendiceal lesions: spectrum of computed tomography findings with pathologic correlation. J Comput Assist Tomogr. 2003;27:297-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 40] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | van Coevorden-Hameete MH, de Graaff E, Titulaer MJ, Hoogenraad CC, Sillevis Smitt PA. Molecular and cellular mechanisms underlying anti-neuronal antibody mediated disorders of the central nervous system. Autoimmun Rev. 2014;13:299-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 46] [Article Influence: 4.2] [Reference Citation Analysis (0)] |