Published online Apr 16, 2023. doi: 10.12998/wjcc.v11.i11.2535
Peer-review started: December 28, 2022
First decision: February 8, 2023
Revised: February 22, 2023
Accepted: March 15, 2023
Article in press: March 15, 2023
Published online: April 16, 2023
Processing time: 99 Days and 1.3 Hours
Carpal tunnel syndrome (CTS) has been associated with gout and type 2 diabetes mellitus (T2DM). However, due to insufficient clinical understanding of gout-related CTS and reliance on the diagnostic importance of elevated serum uric acid levels, such cases are prone to missed diagnosis, misdiagnosis, and delayed treatment. In addition, the effect of T2DM on gout - induced carpal tunnel syndrome has not been reported.
Herein, we present an unusual case of CTS and motor dysfunction caused by miliary tophaceous gout and T2DM. The patient presented to the hand and foot clinic with paresthesia of the fingers of both hands, especially at night. The patient was diagnosed with type 2 diabetes a month ago. Ultrasonography revealed bilateral transverse carpal ligament thickening with median nerve compression during hospitalization. The patient was successfully treated with carpal tunnel decompression and tendon release. The postoperative pathological examination revealed typical gout nodules. This case suggests that the presence of T2DM could accelerate tophi formation and worsen CTS symptoms, although no definitive proof in this regard has been described previously.
Tophi formation may most likely cause the co-occurrence of CTS and flexor dysfunction in gout and incipient diabetes patients.
Core Tip: The onset of diabetes in patients with a previous history of hyperuicemia would likely accelerate urate deposition and lead to the exacerbation of carpal tunnel syndrome.
- Citation: Zhang GF, Rong CM, Li W, Wei BL, Han MT, Han QL. Bilateral carpal tunnel syndrome and motor dysfunction caused by gout and type 2 diabetes: A case report. World J Clin Cases 2023; 11(11): 2535-2540
- URL: https://www.wjgnet.com/2307-8960/full/v11/i11/2535.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i11.2535
Carpal tunnel syndrome (CTS) is the most common form of compressive neuropathy that develops due to the compression of the median nerve in the constrained space of the carpal tunnel. It is typically a chronic and progressive condition, with an incidence of approximately 1%−3% per year[1]. The co-occurrence of CTS and motor dysfunction caused by gout, which has been reported as a cause of CTS in 0.6% of cases, is extremely rare in clinical practice[2]. Herein, we report an unusual case of bilateral CTS associated with tophaceous gout and type 2 diabetes mellitus (T2DM).
A 51-year-old male patient presented to the hand and foot clinic with paresthesia and motor dysfunction of the fingers of both hands for the last 1 mo.
Symptoms started 1 mo with paresthesia and motor dysfunction of the radial fingers of both the hands.
The patient had a history of hyperuricemia for more than 10 years, and his serum uric acid levels were recorded up to 13.44 mg/dL. Accordingly, he was regularly taking febuxostat for two years. One month prior, the patient was found to have elevated blood glucose levels during a physical examination in our hospital and was diagnosed with T2DM, for which he was not receiving treatment.
The patient’s father had a history of diabetes and hyperlipidemia, and the patient denied any family history of hyperuricemia.
Physical examination revealed bilateral thenar muscle atrophy and palmar hypoesthesia on the radial side of both the hands. The wrist flexion test was positive bilaterally, and Tinel’s sign was positive on the left and mildly positive on the right.
Laboratory testing showed uric acid levels within the normal range (5.59 mg/dL) and a fasting blood glucose level of 12.0 mmol/L. In addition, the glycosylated hemoglobin was at 10.0%.
Ultrasound examination showed narrowing of the bilateral carpal canal as well as median nerve compression, with a diameter of 0.13 cm on the left and 0.17 cm on the right at the narrowest points. Electromyography revealed bilateral median nerve neuropathy, which was more pronounced on the left (Supplementary material). No abnormalities were found in X-rays of both the wrists. During hospitalization, improved electromyography revealed neurogenic lesions in bilateral abductors pollicis brevis. Furthermore, the nerve conduction velocity displayed that the latency of motor branches was prolonged, which confirmed bilateral median nerve damage. Greater severity on the left side was noted.
Combined with the patient’s medical history, a final diagnosis of bilateral carpal tunnel syndrome was determined.
Celecoxib and febuxostat were administered to maintain the patient’s uric acid at a normal level. Further, dapagliflozin and acarbose were used to adjust the blood glucose level below 11 mmol/L.
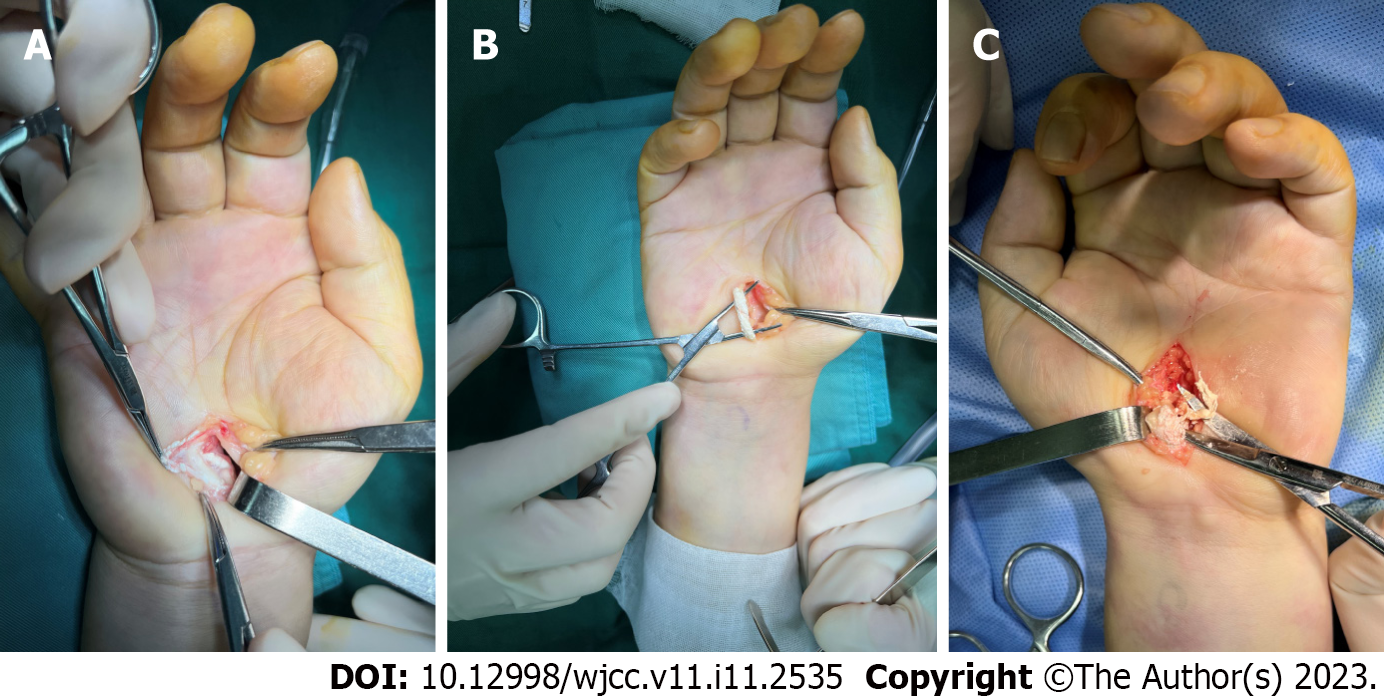
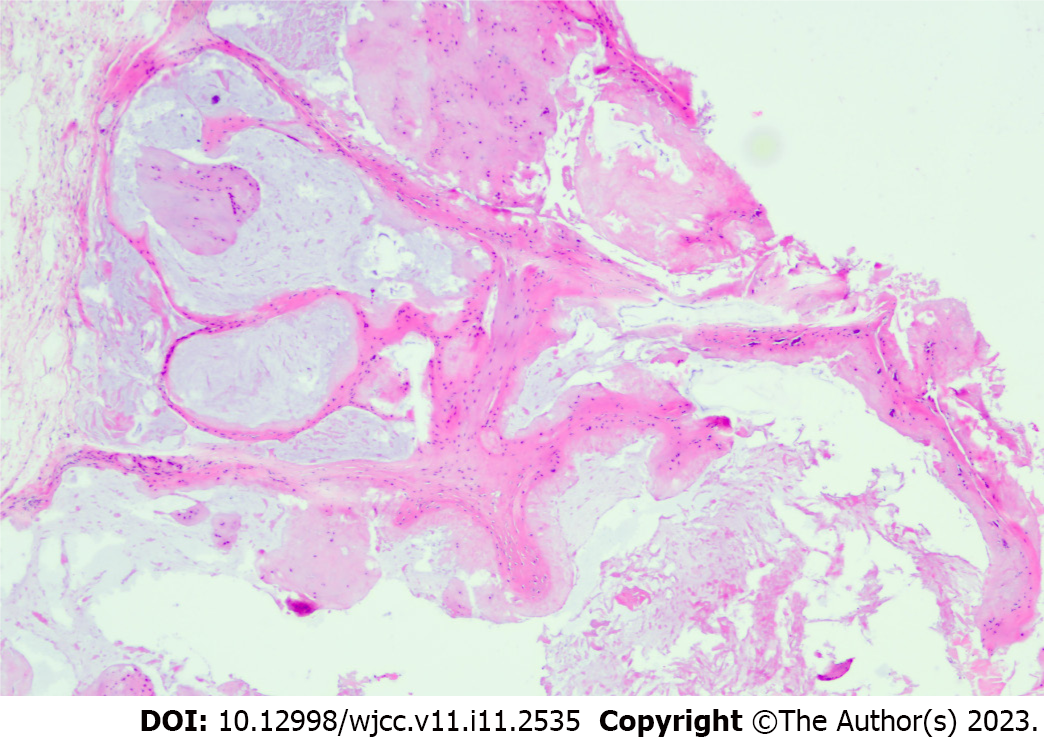
Intraoperatively, multiple white calcareous crystals were observed in the bilateral carpal tunnel, and the median nerves were decompressed by excision of tophi from the carpal canal. Bilaterally, there were multiple miliary tophi in the perineurium of median nerve. They were deposited throughout the superficial flexor tendon of the middle finger and the deep flexor tendon of the ring finger of the left hand as well as the deep flexor tendon of the ring and little fingers of the right hand(Figure 1). Longitudinal incisions were made to expose these urate crystals. We cleaned it with a small curette and rinsed the remaining urate crystals with a sodium bicarbonate solution. In addition, we found that sterile sodium bicarbonate solution was more beneficial to rinse urate crystals off than normal saline. Therefore, we suggest that rinsing with sodium bicarbonate solution is necessary. After trimming, those damaged tendon bands were improved with a 5-0 absorbable suture. The postoperative histopathological findings were consistent with gout nodules (monosodium urate crystals), confirming the diagnosis (Figure 2).
Postoperatively, the patient developed a fever despite colchicine and naproxen treatment; however, the fever subsided within 3 d. At the 4-wk follow-up, the hand numbness improved significantly, and the wrist range of motion returned to normal. Three months following the surgery, there was a partial improvement in the thenar muscle atrophy. At the 6-mo follow-up, the numbness was completely resolved, with a marked improvement in the thenar muscle atrophy.
The carpal tunnel is an osteoligamentous structure with poor extension ability. It protects the median nerve and nine tendons that act to flex the fingers. The median nerve enters the volar surface of the hand through the carpal tunnel, which runs under the flexor retinaculum. Once the tunnel is narrowed or its content is increased, the median nerve is vulnerable to compression, resulting in the development of CTS.
Gout-related CTS is mainly due to the deposition of tophi on the ligaments or content of the carpal tunnel, such as the tendon surface[3,4]. In 1958, Ward et al[5] reported the first case of CTS caused by gout, and suggested that the underlying mechanism could be the deposition of tophi on the wrist flexor tendons that resulted in the compression of the median nerve within the carpal tunnel. In subsequent years, few cases of gout-related CTS have been reported successively. This apparent rarity of the association between gout and CTS is likely to have been fallacious, owing to the failure of recognition and lack of adequate awareness. Our literature search in the PubMed database for articles published in English using the terms “carpal tunnel syndrome,” “gout,” and “diabetes” showed that the cases of gout-related CTS were reported more frequently in recent decades; however, they remained scarce at large. This suggests that the association between CTS and gout has been gradually discovered over the years and has received increasing attention from doctors. However, the effect of T2DM on gout-induced carpal tunnel syndrome has not been reported.
Gout is a metabolic disorder, and is one of the most common inflammatory arthritic conditions worldwide that is caused by persistent hyperuricemia. The global prevalence of gout is increasing, possibly due to trends in global dietary habits and the increasing gout-associated chronic diseases. Specifically, gout affects more than 41 million worldwide[6]. Both gout and T2DM are metabolic diseases clearly associated with insulin resistance, which generally refers to the reduced role of insulin in the uptake and clearance of glucose from surrounding tissues. T2DM has a promoting effect on the development of gout. A key factor may be that in the proximal convoluted tubules of the glomerulus, glucose and uric acid share the same carriers of reabsorption,with resultant competition between them. In the early stage of T2DM, hyperglycemia and hyperinsulinemia inhibit the urinary excretion of uric acid, thus increasing the blood uric acid level[7,8]. In addition, the microvascular lesions and microcirculation disorder in patients with T2DM accelerate the deposition of urates. The specific anatomical characteristics of the carpal tunnel and the metabolic characteristics of its dense connective tissue make the deposition of gout crystals more likely. In our patient, T2DM and CTS appeared successively, which supports that early diabetes is likely to lead to the development of gout associated carpal tunnel syndrome.
Lack of timely medical or surgical treatment of gout can lead to the development of CTS. Reducing the uric acid level within the normal range and anti-inflammatory treatment with allopurinol, probenecid, colchicine or other agents has been shown to alleviate the associated CTS symptoms in patients with gout. Surgical removal of covert tophi and median nerve decompression is another effective option for eliminating CTS symptoms[9]. Jacoulet reported a case in which multiple gout nodules oppressed the median nerve in the carpal canal and the ulnar nerve in the carpal and cubital canals, resulting in severe ulnar nerve palsy[10]. In such cases, standard open tunnel release would not adequately address any of these factors without appropriate medical treatment. Thus, we opted for surgical treatment after the blood glucose and uric acid levels were stabilized within normal ranges.
In patients with a history of gout and T2DM, the formation of tophi should be considered the most probable reason for the co-occurrence of CTS and flexor dysfunction. If patients have persistent neurological symptoms, conservative treatment may lead to irreversible neurological damage; therefore, early surgical treatment is recommended. Furthermore, a complete course of uric acid-lowering and anti-inflammatory treatment is necessary to prevent an acute gout attack and irritable nerve syndrome. Based on the patient’s history and findings in the present case, we speculate that early-stage T2DM could accelerate tophi formation and aggravate CTS symptoms, although no definitive proof has been described to date.
I would like to acknowledge Professors Qing-Luan Han and Wei Li for inspiring my interest in scientific research.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fazilat-Panah D, Iran; Nguyen B, Viet Nam S-Editor: Li L L-Editor: A P-Editor: Li L
| 1. | Ashworth NL. Carpal tunnel syndrome, 2022. 2022 Jan 31 [cited 1 March 2023]. Available from: http://emedicine.medscape.com/article/327330-overview. |
| 2. | Rich JT, Bush DC, Lincoski CJ, Harrington TM. Carpal tunnel syndrome due to tophaceous gout. Orthopedics. 2004;27:862-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Milandri A, Farioli A, Gagliardi C, Longhi S, Salvi F, Curti S, Foffi S, Caponetti AG, Lorenzini M, Ferlini A, Rimessi P, Mattioli S, Violante FS, Rapezzi C. Carpal tunnel syndrome in cardiac amyloidosis: implications for early diagnosis and prognostic role across the spectrum of aetiologies. Eur J Heart Fail. 2020;22:507-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 113] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 4. | Chuang HL, Wong CW. Carpal tunnel syndrome induced by tophaceous deposits on the median nerve: case report. Neurosurgery. 1994;34:919; discussion 920. [PubMed] |
| 5. | WARD LE, BICKEL WH, CORBIN KB. Median neuritis (carpal tunnel syndrome) caused by gouty tophi. J Am Med Assoc. 1958;167:844-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Safiri S, Kolahi AA, Cross M, Carson-Chahhoud K, Hoy D, Almasi-Hashiani A, Sepidarkish M, Ashrafi-Asgarabad A, Moradi-Lakeh M, Mansournia MA, Kaufman JS, Collins G, Woolf AD, March L, Smith E. Prevalence, Incidence, and Years Lived With Disability Due to Gout and Its Attributable Risk Factors for 195 Countries and Territories 1990-2017: A Systematic Analysis of the Global Burden of Disease Study 2017. Arthritis Rheumatol. 2020;72:1916-1927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 116] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 7. | Lin KC, Tsai ST, Lin HY, Chou P. Different progressions of hyperglycemia and diabetes among hyperuricemic men and women in the kinmen study. J Rheumatol. 2004;31:1159-1165. [PubMed] |
| 8. | Li C, Hsieh MC, Chang SJ. Metabolic syndrome, diabetes, and hyperuricemia. Curr Opin Rheumatol. 2013;25:210-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 307] [Article Influence: 25.6] [Reference Citation Analysis (0)] |
| 9. | Janssen T, Rayan GM. Gouty tenosynovitis and compression neuropathy of the median nerve. Clin Orthop Relat Res. 1987;203-206. [PubMed] |
| 10. | Jacoulet P. [Double tunnel syndrome of the upper limb in tophaceous gout. Apropos of a case]. Ann Chir Main Memb Super. 1994;13:42-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |