Published online Apr 16, 2023. doi: 10.12998/wjcc.v11.i11.2510
Peer-review started: December 23, 2022
First decision: January 3, 2023
Revised: January 14, 2023
Accepted: March 21, 2023
Article in press: March 21, 2023
Published online: April 16, 2023
Processing time: 104 Days and 9.2 Hours
Primary schwannoma is a rare submucosal tumor of the esophagus, which is most often benign, and surgery is the only effective treatment. So far, only a few cases have been reported. Herein, we reported a single case diagnosed with primary esophageal schwannoma that was totally removed by submucosal tunneling endoscopic resection (STER).
A 62-year-old man presented to the hospital with a history of resection of a malignant gastric tumor and mild dysphagia. Endoscopic examination revealed a large submucosal elevated lesion in the esophagus 25-30 cm from the incisors. Endoscopic ultrasonography detected a 45 mm × 35 mm × 31 mm hypoechoic lesion; chest computed tomography showed a mass of approximately 55 mm × 35 mm × 29 mm. A preliminary examination showed features suggestive of a stromal tumor. Pathological findings indicated esophageal schwannoma. Next, STER alone was performed to completely resect the mass, and the patient recovered well post-surgery. Afterward, the patient was discharged and showed no tumor recurrence at 33 mo of follow-up.
Endoscopic resection is still an effective treatment for large esophageal schwannomas (> 30 mm) under meticulous morphological evaluation.
Core Tip: Primary esophageal schwannoma is a rare esophageal submucosal tumor that is usually benign. The final diagnosis requires histopathological and immunohistochemical examinations. The surgical method depends on the morphology and size of the lesion. Submucosal tunneling endoscopic resection appears to be a feasible treatment for a subset of large esophageal schwannomas with large supero-inferior diameter but the smaller antero-posterior diameter and left-right diameters, which may benefit patients intolerant to surgical treatment.
- Citation: Mu YZ, Zhang Q, Zhao J, Liu Y, Kong LW, Ding ZX. Total removal of a large esophageal schwannoma by submucosal tunneling endoscopic resection: A case report and review of literature. World J Clin Cases 2023; 11(11): 2510-2520
- URL: https://www.wjgnet.com/2307-8960/full/v11/i11/2510.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i11.2510
Primary esophageal schwannomas are very rare tumors. In most cases, they are benign, while only a few malignant cases have been reported[1,2]. Imaging findings can reveal the specific location of the lesion, blood supply, and the relationship between the mass and the surrounding tissues, which are useful to determine whether the tumor is benign or malignant, and subsequently choose the appropriate treatment[3]. As one of imaging tools, endoscopic ultrasonography (EUS) can clearly display the layers of the esophageal wall[3] as well as reveal the location and origin of lesions[4,5]. Preoperative diagnosis of schwannoma is difficult[6,7], and the final diagnosis requires histopathological and immunohistochemical examinations[7]. Immunohistochemical staining is currently the only reliable diagnostic method and S100 protein is a specific molecular marker of schwannomas[7,8].
Esophageal schwannoma is insensitive to medical treatments such as radiotherapy and chemotherapy. Hence, resection remains the only effective treatment, especially if the tumor is detected in the early stage[8]. The maximum diameter of most endoscopically resected masses over the past 12 years was less than 30 mm[1,2,6-36], but these cases only discussed endoscopic resection according to the maximum diameter of the tumor and did not analyze the three diameter lines of the mass. In this paper, we reported single submucosal tunnel endoscopic resection for an esophageal schwannoma with 55 mm in supero-inferior diameter.
A 62-year-old Asian male presented with mild dysphagia lasting for five months.
The patient suffered from mild dysphagia for five months when swallowing solid food. There was no associated chest pain, nausea, vomiting, or abdominal pain.
The patient underwent Billroth II subtotal gastrectomy six years ago due to the presence of stomach cancer, as well as exploratory laparotomy, intestinal adhesiolysis, and inguinal hernia repair two years ago. The patient also completed eight cycles of XELOX adjunctive therapy. His blood pressure was elevated for about one year, and he regularly took oral nifedipine 10 mg daily.
There was no clinically significant family history; the patient had no smoking or drinking habits, and neither did he have a history of exposure to toxic substances.
The patient was 177 cm tall and weighed 63.1 kg. His temperature was 36.1 °C, heart rate was 61 beats per minute, respiratory rate was 17 breaths per minute, and blood pressure was 153/84 mmHg. Lung and abdominal tests were normal. Neurological examination revealed no obvious abnormalities. There was no edema in the bilateral lower limbs.
Levels of anti-thyroid peroxidase antibodies were elevated. Glycosylated hemoglobin level (7.1%), total bilirubin (21.2 μmol/L), and indirect bilirubin (14.2 μmol/L) were increased, while aspartate aminotransferase (11 U/L) was decreased. Tumor markers CYFRA21-13 (40 ng/mL) were elevated. All other laboratory tests were within normal range.
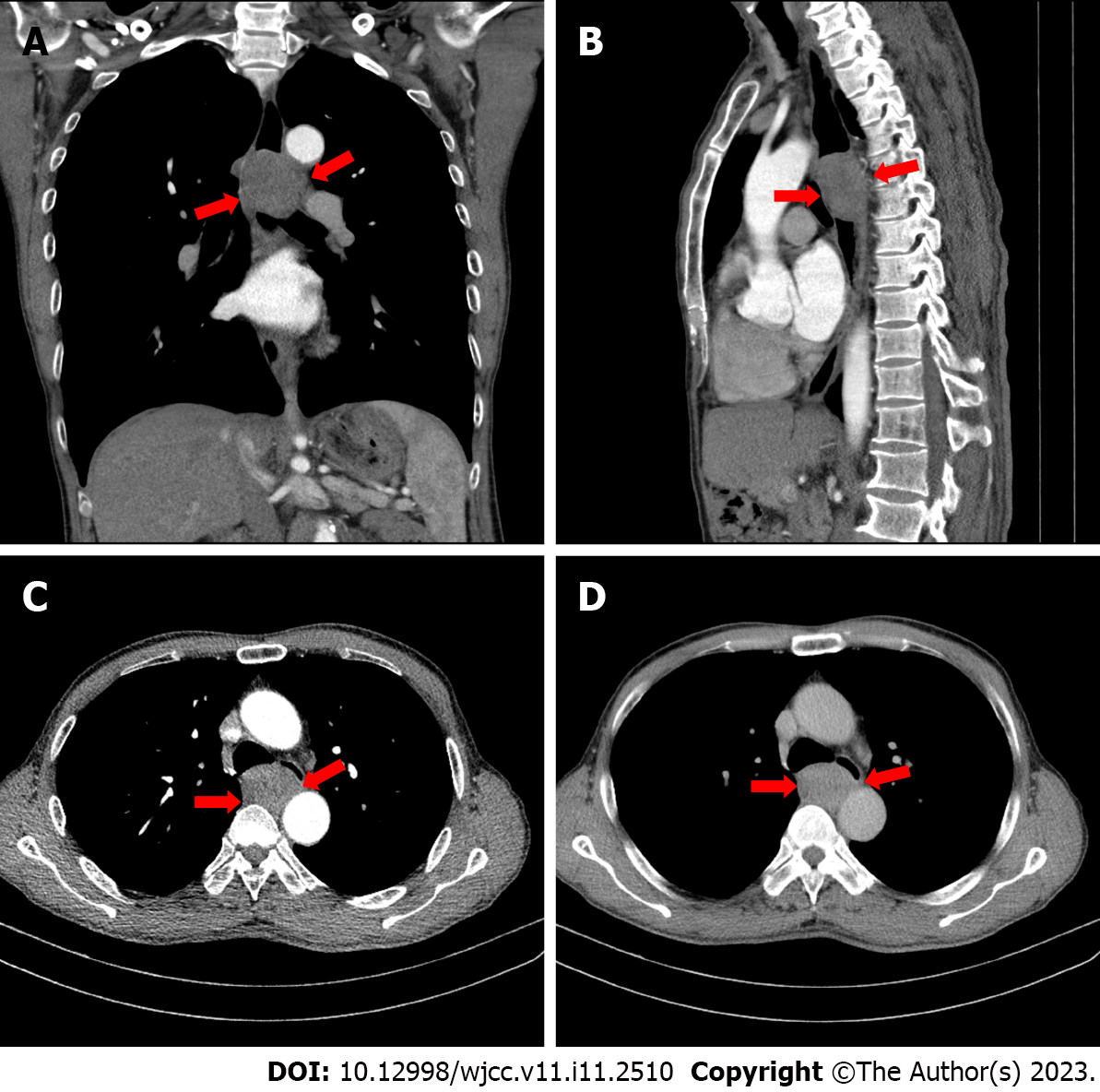
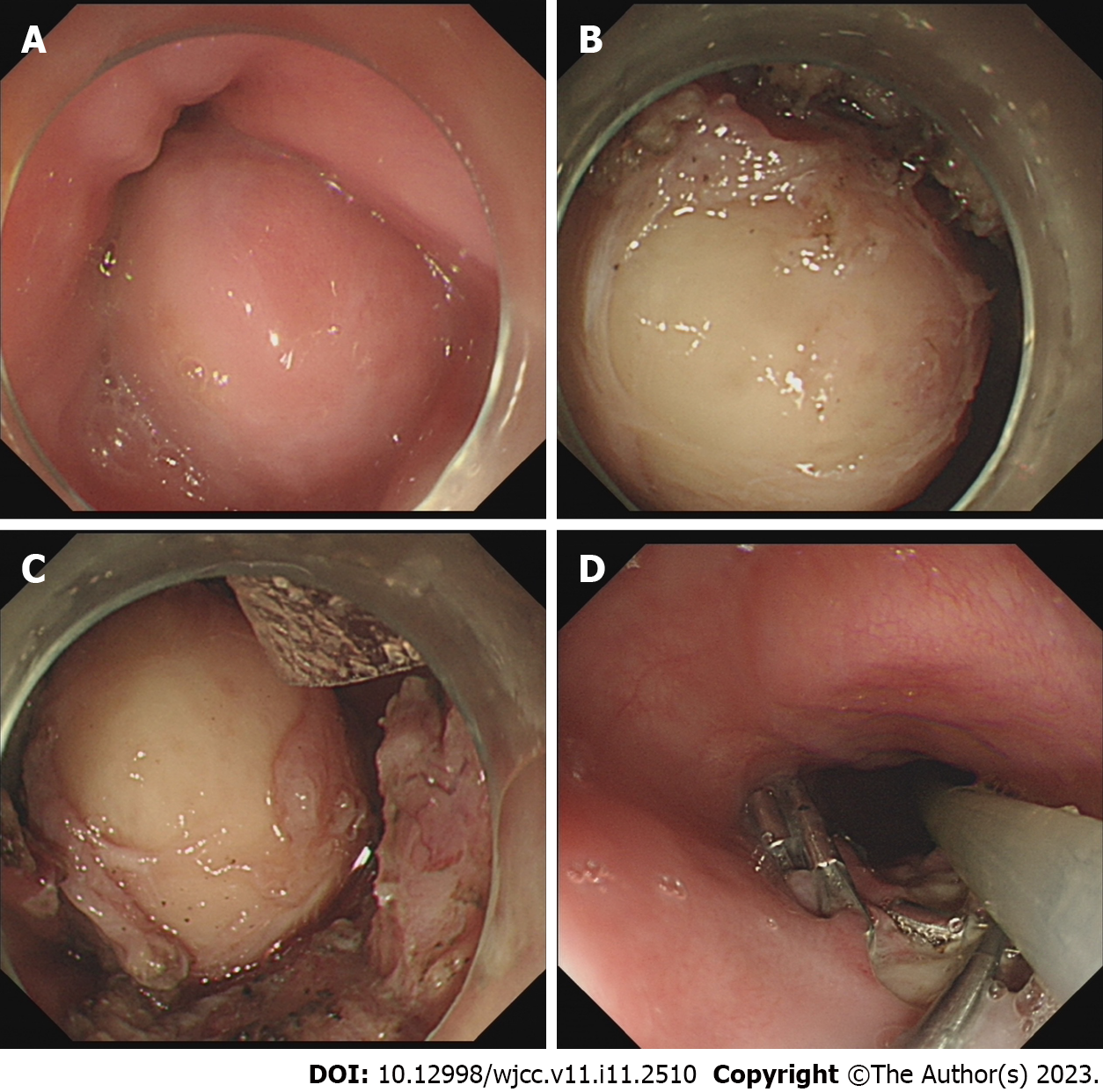
Plain and contrast-enhanced chest computed tomography revealed a round lesion of 55 mm × 35 mm × 29 mm in the middle and upper esophagus, with homogeneous enhancement and esophageal lumen stenosis (Figure 1). Upper gastrointestinal endoscopy indicated a lesion in the esophagus about 25-30 cm from the incisor, and the esophageal mucosa was intact (Figure 2A). EUS demonstrated a hypoechoic and homogeneous mass originating from the muscularis propria (MP), with a diameter of about 41 mm. It was provisionally diagnosed as a stromal tumor.
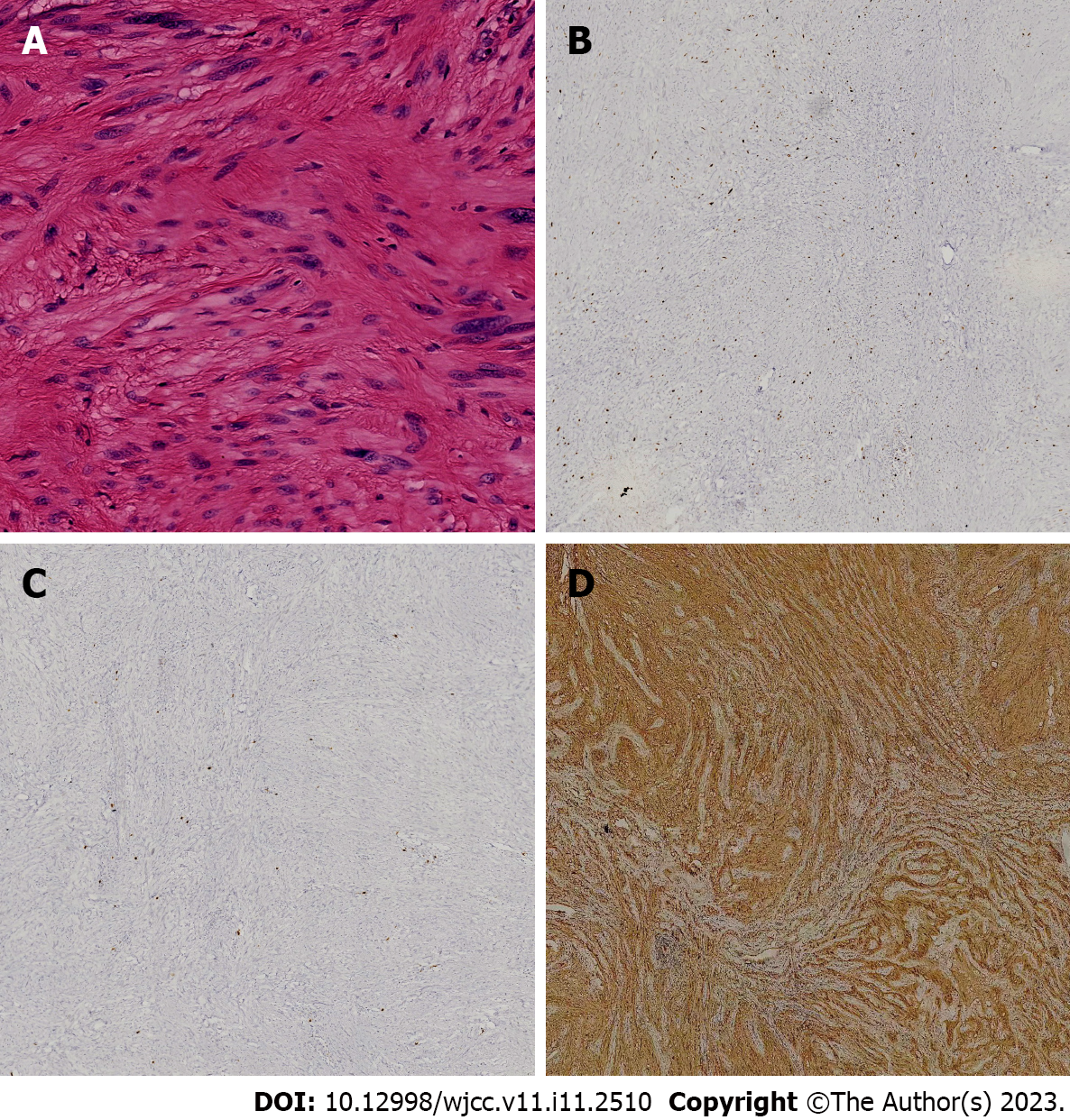
Microscopy showed a dense proliferation of spindle cells without mitosis and atypia. In addition (Figure 3A), immunohistochemical staining was positive for S-100 protein (Figure 3D), the expression level of Ki-67 was < 5% (Figure 3B), and negative for CD34, Desmin, CD117 (Figure 3C), DOG-1, and SMA. These findings were strongly suggestive of a benign esophageal schwannoma.
The patient underwent submucosal tunneling endoscopic resection (STER). The tumor with the size of 45 mm × 35 mm × 31 mm was finally resected with the intact fibrous capsule. The entire procedure lasted for about five hours. STER was performed under general anesthesia with intravenous propofol (2 mg/kg). Intraoperative findings showed that the lesion was located in the esophagus about 25-30 cm from the incisor, and the esophageal mucosa was intact (Figure 2A). EUS demonstrated a hypoechoic and homogeneous mass originating from the MP, with a diameter of about 41 mm.
The STER procedure was as follows: after the submucosal injection of glycerol fructose, a submucosal tunnel was created, and a 20 mm longitudinal mucosal incision was made with a Hook knife. Then a submucosal tunnel was created with an IT knife between the mucosal and muscular layers. The tunnel was continued downwards with the dual knife until the tumor was exposed. Within the submucosal tunnel, the tumor was separated from the MP layer as much as possible. Next, circumferential full-thickness MP resection was performed using the IT knife and snare for the tumor involving the deep layer of MP. The tumor was finally resected with the intact fibrous capsule. Hot hemostatic forceps were applied to treat blood vessels in surgical wounds. IT knife was used to incise the mucosal surface of the tumor that was difficult to remove, and multiple snares and stone extractors were used to completely remove the lesion (Figure 2B-D). The mucosal entry incision was closed with 16 vascular clips and 10 tissue clips.
After surgery, the patient’s dysphagia disappeared. On follow-up endoscopy at three months, the wound was fully healed. Follow-up did not reveal local tumor recurrence or metastasis at 33 mo post-operation.
Primary schwannomas are rare esophageal submucosal tumors accounting for less than 2% of all esophageal tumors[5,7,9]. Most of these tumors are benign, but a few malignant cases have been reported[1,2]. Typically, dyspnea and dysphagia are the most common complaints; other reported signs and symptoms include chest pain, stridor, hematemesis, cough, and palpable neck mass[10]. A literature search in the PubMed database identified 40 reported cases[1,2,6-36] published between 2011 and October 2022, which are listed in Table 1. Statistical analysis of baseline information, clinical symptoms, tumor size, and management methods are shown in Tables 2-4.
| Case | Ref. | Year | Age | Sex | Location | Tumor size (mm) | Symptoms | Management | Malignant findings |
| 1 | Choo et al[10] | 2011 | 22 | M | Ut | 80 × 60 × 30 | Cough, dyspnea and dysphagia | Enucleation | Benign |
| 2 | Wang et al[2] | 2011 | 44 | F | Lt | 55 × 44 | Progressive dysphagia | Surgical enucleation | Malignant |
| 3 | Liu et al[16] | 2013 | 62 | F | NA | 90 × 40 × 30 | Dysphagia and dyspnea | Partial esophagectomy and esophagogastrostomy | Benign |
| 4 | Liu et al[17] | 2013 | NA | NA | NA | < 30 | NA | STER | Benign |
| 5 | Kitada et al[6] | 2013 | 55 | F | UM | 75 × 57 × 80 | Palpitations and dysphagia | Mini thoracotomy | Benign |
| 6 | Gu et al[18] | 2014 | 39 | M | UM | 35 × 32 × 12 | Obstructive sensation | VATS | Benign |
| 7 | Jeon et al[19] | 2014 | 63 | M | Ut | 94 × 89 | No symptoms | Thoracotomy | Benign |
| 8 | Jeon et al[19] | 2014 | 32 | F | Ut | 60 × 85 × 40 | Intermittent chest pain | VATS | Benign |
| 9 | Tomono et al[20] | 2015 | 59 | M | Mt | 109 × 72 × 71 | Dysphagia, dyspnea, disturbed | Subtotal esophagectomy | Benign |
| 10 | Wang et al[21] | 2015 | 53 | F | NA | NA | NA | Surgical excision | Benign |
| 11 | Wang et al[21] | 2015 | 52 | F | NA | NA | NA | Surgical excision | Benign |
| 12 | Zhang et al[22] | 2015 | 67 | F | NA | NA | Dysphagia | Surgical excision | Benign |
| 13 | Mishra et al[1] | 2016 | 27 | F | Mt | 120 × 100 × 101 | Dysphagia and palpitations | Surgical enucleation | Malignant |
| 14 | Watanabe et al[23] | 2016 | 39 | F | Ut | 55 × 45 × 24 | Epigastric pain, difficulty swallowing | Surgical excision | Benign |
| 15 | Chen et al[24] | 2016 | 46 | M | Mt | 30 × 20 × 17 | Discomfort during swallowing | VATS | Benign |
| 16 | Chen et al[24] | 2016 | 42 | F | Ut | 30 × 40 × 40 | Dysphagia | Enucleation | Benign |
| 17 | Chen et al[24] | 2016 | 58 | F | Ut | 80 × 60 × 60 | Dysphagia | Enucleation | Benign |
| 18 | Onodera et al[12] | 2017 | 47 | F | Ut | 60 | Dysphagia | Thoracoscopic + endoscopic excision | Benign |
| 19 | Moro et al[25] | 2017 | 66 | M | Ut | 52 × 40 × 31 | Dysphagia | Surgical excision | Benign |
| 20 | Zhang et al[13] | 2018 | 48 | F | Mt | 69 × 36 | Dysphagia | Robot-assisted enucleation | Benign |
| 21 | Iwata et al[26] | 2018 | 74 | F | Ut | 80 × 42 | Loss of consciousness | Surgical excision | Benign |
| 22 | Zhu et al[27] | 2019 | 55 | F | Mt | 25 × 25 × 20 | Dysphagia and chest pain | Left thoracotomy with subtotal esophagectomy | Benign |
| 23 | Souza et al[28] | 2019 | 43 | M | Ut | 70 | Pharyngitis, odynophagia, hemoptysis | Surgical excision | Benign |
| 24 | Ramos et al[29] | 2019 | 40 | F | Ut | 80 × 45 × 20 | Pharyngitis, odynophagia, dysphagia | Surgical excision | Benign |
| 25 | Degheili et al[30] | 2019 | 50 | F | Ut | 78 × 54 × 105 | Dyspnea and dysphagia | Surgical excision | Benign |
| 26 | Matteo et al[31] | 2020 | 22 | M | Lt | 37 × 28 × 70 | Dysphagia | Subtotal esophagectomy | Benign |
| 27 | Wu et al[7] | 2020 | 67 | F | Ut | 61 × 46 × 60 | Dysphagia and dyspnea | Surgical excision | Benign |
| 28 | Li et al[11] | 2020 | 59 | M | Lt | 14 × 5 | Upper abdominal distension | Endoscopic submucosal excision | Benign |
| 29 | Li et al[11] | 2020 | 51 | F | Mt | 18 × 20 | Heartburn | STER | Benign |
| 30 | Li et al[11] | 2020 | 49 | M | Lt | 28 × 22 | Dysphagia | STER | Benign |
| 31 | Wang et al[8] | 2021 | 62 | M | Lt | 53 × 39 × 50 | Severe dysphagia | VATS | Benign |
| 32 | Matsui et al[32] | 2021 | 50 | M | Lt | 20 | Asymptomatic | VATS | Benign |
| 33 | Khalayleh et al[33] | 2021 | 61 | F | Ut | 50 × 30 | Dysphagia | VATS | Benign |
| 34 | Zackria et al[15] | 2021 | 78 | F | Ut | 30 | Dysphagia | FNA | Benign |
| 35 | Khan et al[34] | 2021 | 60 | F | Lt | 76 × 46 × 66 | Dysphagia | Right-sided VATS | Benign |
| 36 | Wang et al[35] | 2022 | 70 | F | Ut | 32 × 40 × 54 | Dysphagia | VATS | Benign |
| 37 | Froiio et al[14] | 2022 | 55 | F | Ut | 65 × 47 | Dysphagia | Robotic enucleation | Benign |
| 38 | Gupta et al[9] | 2022 | 62 | F | Mt | 51 × 31 | Dysphagia | FNA | Benign |
| 39 | Nashed et al[36] | 2022 | 72 | F | Mt | 29 × 29 × 21 | Dysphagia | STER | Benign |
| 40 | Current article | 2022 | 62 | M | Mt | 55 × 35 | Dysphagia | STER | Benign |
| Characteristics | n (%) s (Total 40) | Characteristics | n (%) s (Total 40) | mean ± SD | ||
| Location | Upper/middle | 28 (70) | Sex | Male | 13 (32.5) | |
| Lower | 7 (17.5) | Female | 26 (65.0) | |||
| NA | 5 (12.5) | NA | 1 (2.5) | |||
| Malignant findings | Benign | 38 (95) | Age (yr) | 55.92 ± 2.17 | ||
| Malignant | 2 (5) |
| Symptoms | n (%) s (Total 40) |
| Dysphagia/odynophagia | 31 (88.57) |
| Epigastric pain/upper abdominal distension | 3 (8.57) |
| Palpitations/chest pain | 4 (11.43) |
| Dyspnea | 5 (14.29) |
| Cough | 1 (2.86) |
| Hemoptysis | 1 (2.86) |
| Loss of consciousness | 1 (2.86) |
| Pharyngitis/pharyngodynia | 2 (5.71) |
| Asymptomatic | 2 (5.71) |
| NA | 5 (14.29) |
| n (%) s | Maximum diameter (mm) | ||||
| Total | 40 | mean: 67.25 (± 4.72) | |||
| The largest | The smallest | mean ± SD | |||
| Management | Surgical excision/VATS | 29 (72.5) | 120 | 20 | 67.25 ± 4.72 |
| Endoscopic excision/STER | 5 (12.5) | 29 | 14 | 22.75 ± 3.54 | |
| Current article (STER) | 1 (2.5) | 55 | |||
| Robot-assisted excision | 2 (5) | 69 | 65 | ||
| FNA | 2 (5) | 51 | 30 | ||
| Thoracoscopic + endoscopic excision | 1 (2.5) | 60 | |||
Tables 1 and 2 show that the mean age of schwannoma patients was 52.92 years, with a standard deviation of 2.17 years, the minimum age was 22 years, and the maximum age was 78 years. The male-to-female ratio was 1:2 in the adult population. Of the 40 esophageal schwannomas, 2 (5%) were malignant, and 38 (95%) were benign. Of these, 28 (70%) tumors were located in the upper or middle esophagus, while 7 (17.5%) were in the lower third of the esophagus. In middle-aged women, tumors were located in the middle and upper esophagus and were mostly benign, in accordance with the description of the esophageal nerve mentioned in the previous literature[11].
The clinical symptoms are summarized in Table 3. Some patients had corresponding clinical symptoms, so we analyzed 40 patients with esophageal schwannoma, 31 (88.6%) of whom had dysphagia, which appears to be the most important symptom that may be caused by the expansive growth of the tumor in the esophagus. Five (14.29%) patients presented with dyspnea, perhaps due to tracheal compression by a tumor, and another patient presented with loss of consciousness. In addition, some patients presented with symptoms of dyspnea, chest pain, palpitation, chest tightness, abdominal distention, etc. A sore throat was observed in 2 patients, a cough in 1 patient, and hemoptysis in 1 patient. These findings are consistent with previous reports[10].
Most cases of esophageal schwannoma are found incidentally during a physical examination and are commonly misdiagnosed[6,24]. Previous reports on esophageal schwannoma have failed to correctly diagnose the tumor preoperatively[6,7]. We believe that the two main reasons for the misdiagnosis are the following: first, diagnosing esophageal schwannoma using imaging alone remains a challenging task; the tumor is often misdiagnosed as other submucosal tumors, such as esophageal leiomyoma and esophageal, gastrointestinal stromal tumors. Second, since esophageal schwannomas are very rare, most physicians do not consider it as the first diagnosis or differential diagnosis, highlighting the need to improve doctors' understanding of esophageal schwannoma.
Hence, meticulous radiographic evaluation of esophageal schwannoma is necessary. This can help identify the lesion's specific location, blood supply, relationship with surrounding tissues, and esophageal layer in which the lesion originated, which provide a crucial reference for distinguishing benign from malignant tumors and the choice of surgical methods.
Esophageal schwannomas are mainly treated by surgical resection[13]. Literature reports published in the past 12 years (Table 4) revealed that the average maximum diameter of all 40 tumors was 67.25 (± 4.72) mm, of which 29 (72.5%) cases underwent surgical resection or thoracoscopic resection, and the largest diameter reached 120 mm, the smallest was 20 mm, and the average maximum diameter was 67.25 ± 4.72 mm. Five (12.5%) esophageal schwannomas were resected via endoscopic surgical approach (including STER), with a maximum diameter of 29 mm, a minimum of 14 mm, a mean maximum diameter of 22.75 ± 3.54 mm, and maximum diameters of these masses were less than 30 mm. In our reported case, complete resection of esophageal schwannoma was performed using STER alone, and the size of this tumor exceeded the maximum size of esophageal schwannomas in all previously reported cases. Only one reported mass with a maximum diameter of 60 mm[12] was larger than our case; however, that case was managed by using thoracoscopy combined with endoscopic surgery rather than endoscopic surgery alone. In addition, there were other management methods, including robot-assisted resection of tumors with maximum diameters of 69 mm[13] and 65 mm[14] in two cases, and no further treatment measures were taken in the other two cases[9,15] after FNA puncture to obtain pathology.
Surgery may be performed by open thoracotomy or video-assisted thoracoscopy[13]. Small lesions in a suitable location can be removed endoscopically by experienced endoscopists using endoscopic submucosal excision or STER[11]. Compared with the first two surgeries, endoscopic resection causes less trauma and fewer complications and reduces the risk of anesthesia, leading to faster recovery and shorter hospitalization[11]. Although no specific cutoff for size could be identified, most tumors > 70 mm were removed by thoracotomy[7,37]. Most of the reported endoscopically resectable submucosal tumors were < 30 mm[11].
However, in all these reports, including cases of esophageal schwannomas treated endoscopically over the past 12 years[11,12,17,36], the size discussed was the maximum diameter of the tumor, while the supero-inferior diameter, antero-posterior diameter, and left-right diameter of the tumor were not analyzed separately. Due to the narrow structure of the esophagus, many schwannomas are limited by the wall of the esophagus and typically have a narrow shape, which often leads to smaller antero-posterior diameter and left-right diameters of the masses although the long diameter is very large, and gives more operating space for endoscopic surgery.
In the present case, the maximum diameter of the lesion was > 50 mm, and postoperative esophageal fistula and pneumothorax may have occurred if endoscopic surgery had been performed. Hence, we recommended thoracoscopic surgery or an open surgical approach[11]. However, the patient refused to undergo surgery again and requested endoscopic minimally invasive resection. After carefully examining the morphology of the mass, we found that this tumor had a large supero-inferior diameter but also smaller antero-posterior and left-right diameters, which meant that the mucosal tunnel only needed to withstand a width of > 30 mm, not 50 mm. Hence, we concluded that there is a certain but controllable risk in treating this patient by endoscopic surgery, and then proposed STER for this patient under the premise of controllable risk and fully considering the possible complications and corresponding solutions.
To the best of our knowledge, this is the first report of using STER alone for the successful removal of an esophageal schwannoma > 30 mm. It is also the first report on the specific analysis of the relationship between the shape of esophageal schwannoma, different diameter lines, and surgical options. Therefore, if the morphological factors of the mass are included, endoscopic treatment could be used for esophageal schwannomas with a maximum diameter of > 30 mm. Hence, risk-controlled STER appears to be a feasible and effective treatment for a subset of large esophageal schwannomas with large supero-inferior diameter but smaller antero-posterior and left-right diameters, which may benefit patients intolerant to surgical treatment.
Primary schwannoma is a rare submucosal tumor of the esophagus. Imaging findings can provide useful information, including the location, size, morphology, density, and relationships with the surrounding tissues, particularly the size and morphology, which could influence the treatment choice. We reported a successful resection of the esophageal schwannoma by STER, with a maximum diameter of 55mm and a minimum diameter of 29 mm. In our case, the tumor's small antero-posterior and left-right diameter were important factors for successful removal by STER. Therefore, the morphological features of a mass, especially the three diameters, should be meticulously analyzed. STER appears to be an effective treatment method for a subset of large esophageal schwannomas with large supero-inferior diameter but smaller antero-posterior and left-right diameters, thus benefiting the patients intolerant to surgical treatment.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Head and Neck Professional Committee of Chinese Society of Radiology.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Al-Ani RM, Iraq; Hakimi T, Afghanistan S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Mishra B, Madhusudhan KS, Kilambi R, Das P, Pal S, Srivastava DN. Malignant Schwannoma of the Esophagus: A Rare Case Report. Korean J Thorac Cardiovasc Surg. 2016;49:63-66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 2. | Wang S, Zheng J, Ruan Z, Huang H, Yang Z. Long-term survival in a rare case of malignant esophageal schwannoma cured by surgical excision. Ann Thorac Surg. 2011;92:357-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Karaca C, Turner BG, Cizginer S, Forcione D, Brugge W. Accuracy of EUS in the evaluation of small gastric subepithelial lesions. Gastrointest Endosc. 2010;71:722-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 132] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 4. | Reddymasu SC, Oropeza-Vail M, Pakseresht K, Moloney B, Esfandyari T, Grisolano S, Buckles D, Olyaee M. Are endoscopic ultrasonography imaging characteristics reliable for the diagnosis of small upper gastrointestinal subepithelial lesions? J Clin Gastroenterol. 2012;46:42-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Morales-Maza J, Pastor-Sifuentes FU, Sánchez-Morales GE, Ramos ES, Santes O, Clemente-Gutiérrez U, Pimienta-Ibarra AS, Medina-Franco H. Clinical characteristics and surgical treatment of schwannomas of the esophagus and stomach: A case series and systematic review. World J Gastrointest Oncol. 2019;11:750-760. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (1)] |
| 6. | Kitada M, Matsuda Y, Hayashi S, Ishibashi K, Oikawa K, Miyokawa N. Esophageal schwannoma: a case report. World J Surg Oncol. 2013;11:253. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | Wu CX, Yu QQ, Shou WZ, Zhang K, Zhang ZQ, Bao Q. Benign esophageal schwannoma: A case report and brief overview. Medicine (Baltimore). 2020;99:e21527. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 8. | Wang TY, Wang BL, Wang FR, Jing MY, Zhang LD, Zhang DK. Thoracoscopic resection of a large lower esophageal schwannoma: A case report and review of the literature. World J Clin Cases. 2021;9:11061-11070. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 2] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Gupta P, Rana S, Dey P. Cytomorphological and immunocytochemical diagnosis of an oesophageal mass in a 62-year-old female with dysphagia. Cytopathology. 2022;33:281-284. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Choo SS, Smith M, Cimino-Mathews A, Yang SC. An early presenting esophageal schwannoma. Gastroenterol Res Pract. 2011;2011:165120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Li B, Wang X, Zou WL, Yu SX, Chen Y, Xu HW. Endoscopic resection of benign esophageal schwannoma: Three case reports and review of literature. World J Clin Cases. 2020;8:5690-5700. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Onodera Y, Nakano T, Takeyama D, Maruyama S, Taniyama Y, Sakurai T, Heishi T, Sato C, Kumagai T, Kamei T. Combined thoracoscopic and endoscopic surgery for a large esophageal schwannoma. World J Gastroenterol. 2017;23:8256-8260. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Zhang Y, Han Y, Xiang J, Li H. Robot-assisted enucleation of large dumbbell-shaped esophageal schwannoma: a case report. BMC Surg. 2018;18:36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Froiio C, Berlth F, Capovilla G, Tagkalos E, Hadzijusufovic E, Mann C, Lang H, Grimminger PP. Robotic-assisted surgery for esophageal submucosal tumors: a single-center case series. Updates Surg. 2022;74:1043-1054. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 15. | Zackria R, Choi EH. Esophageal Schwannoma: A Rare Benign Esophageal Tumor. Cureus. 2021;13:e15667. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 16. | Liu T, Liu H, Yang C, Zhang X, Xu S, Liu B. Benign esophageal schwannoma compressing the trachea requiring esophagectomy: a case report. Thorac Cardiovasc Surg. 2013;61:505-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (1)] |
| 17. | Liu BR, Song JT, Kong LJ, Pei FH, Wang XH, Du YJ. Tunneling endoscopic muscularis dissection for subepithelial tumors originating from the muscularis propria of the esophagus and gastric cardia. Surg Endosc. 2013;27:4354-4359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 71] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 18. | Gu MJ, Choi JH. Microcystic/reticular schwannoma of the esophagus: the first case report and a diagnostic pitfall. BMC Gastroenterol. 2014;14:193. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Jeon HW, Kim KS, Hyun KY, Park JK. Enucleation of giant esophageal schwannoma of the upper thoracic esophagus: reports of two cases. World J Surg Oncol. 2014;12:39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | Tomono A, Nakamura T, Otowa Y, Imanishi T, Tanaka Y, Maniwa Y, Kakeji Y. A Case of Benign Esophageal Schwannoma Causing Life-threatening Tracheal Obstruction. Ann Thorac Cardiovasc Surg. 2015;21:289-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Wang YL, Sun JG, Wang J, Wei WJ, Zhu YX, Wang Y, Sun GH, Xu K, Li H, Zhang L, Ji QH. Schwannoma of the cervical esophagus: Report of 2 cases and a review of the literature. Ear Nose Throat J. 2015;94:E10-E13. [PubMed] |
| 22. | Zhang Q, Lu G, Li D. [The resection of the huge mediastinal schwannoma by the jugulal approach: one case report]. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2016;30:329-330. [PubMed] |
| 23. | Watanabe T, Miyazaki T, Saito H, Yoshida T, Kumakura Y, Honjyo H, Yokobori T, Sakai M, Sohda M, Kuwano H. Resection of an esophageal schwannoma with thoracoscopic surgery: a case report. Surg Case Rep. 2016;2:127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 24. | Chen X, Li Y, Liu X, Fu H, Sun H, Zhang R, Wang Z, Zheng Y. A report of three cases of surgical removal of esophageal schwannomas. J Thorac Dis. 2016;8:E353-E357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Moro K, Nagahashi M, Hirashima K, Kosugi SI, Hanyu T, Ichikawa H, Ishikawa T, Watanabe G, Gabriel E, Kawaguchi T, Takabe K, Wakai T. Benign esophageal schwannoma: a brief overview and our experience with this rare tumor. Surg Case Rep. 2017;3:97. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 26. | Iwata Y, Tanaka C, Komori S, Nagao N, Kawai M, Yoshida K, Kunieda K. Lobulated esophageal schwannoma resected with concurrent approach from the thorax and cervix. World J Surg Oncol. 2018;16:29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 27. | Zhu L, Li W, Zhu Z, Chai Y. Benign esophageal schwannoma: A case report and review of literature. Niger J Clin Pract. 2019;22:731-733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 28. | Souza LCA, Pinto TDA, Cavalcanti HOF, Rezende AR, Nicoletti ALA, Leão CM, Cunha VC. Esophageal schwannoma: Case report and epidemiological, clinical, surgical and immunopathological analysis. Int J Surg Case Rep. 2019;55:69-75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 29. | Sanchez-Garcia Ramos E, Cortes R, de Leon AR, Contreras-Jimenez E, Rodríguez-Quintero JH, Morales-Maza J, Aguilar-Frasco J, Irigoyen A, Reyes F, Alfaro-Goldaracena A. Esophageal schwannomas: A rarity beneath benign esophageal tumors a case report. Int J Surg Case Rep. 2019;58:220-223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 30. | Degheili JA, Sfeir P, Khalifeh I, Hallal AH. Large esophageal schwannoma: En-bloc resection with primary closure by esophagoplasty. Int J Surg Case Rep. 2019;61:77-81. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 31. | Matteo MV, Sassorossi C, Lococo F, Ricci R, Margaritora S, Gasbarrini A, Zileri Dal Verme L. A huge esophageal Schwannoma occurring in a Caucasian young male: a case report. Eur Rev Med Pharmacol Sci. 2020;24:10703-10707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 32. | Matsui S, Yamazaki T, Shiraishi O, Kudo M. Efficacy of endoscopic ultrasound-guided fine-needle aspiration for esophageal schwannoma. Ann Gastroenterol. 2021;34:597. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 33. | Khalayleh H, Mashni I, Bar I, Pines G. Semi-prone position for thoracoscopic resection of a rare oesophageal tumour. Interact Cardiovasc Thorac Surg. 2021;33:646-648. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 34. | Khan U, Simone C, Safieddine N, Gazala S. Video-assisted thoracoscopic resection of a giant esophageal schwannoma: A case report. Int J Surg Case Rep. 2021;85:106202. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 35. | Wang H, Li Y, Wu M, Cui H. Benign esophageal schwannoma: A case report. Asian J Surg. 2023;46:1437-1438. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 36. | Nashed B, Ayas MF, Gharib H, Issa M, Fatouh K, Sebastian F, Backer Z, Mahat K, Barawi M. Esophageal Schwannoma: An Important Differential Diagnosis for Esophageal Subepithelial Lesions. Cureus. 2022;14:e27168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 37. | Kent M, d'Amato T, Nordman C, Schuchert M, Landreneau R, Alvelo-Rivera M, Luketich J. Minimally invasive resection of benign esophageal tumors. J Thorac Cardiovasc Surg. 2007;134:176-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 84] [Article Influence: 4.7] [Reference Citation Analysis (0)] |