Published online Apr 16, 2023. doi: 10.12998/wjcc.v11.i11.2489
Peer-review started: December 18, 2022
First decision: January 20, 2023
Revised: February 2, 2023
Accepted: March 20, 2023
Article in press: March 20, 2023
Published online: April 16, 2023
Processing time: 108 Days and 19.5 Hours
There are few reported cases of intracranial large artery embolism due to carotid thrombosis caused by a neck massager. Herein we report such a case.
A 49-year-old woman presented with left limb weakness and dysarthria after a history of neck massage for 1 mo. Neurological examination showed left central facial paralysis and left hemiparesis with a National Institutes of Health Stroke Scale score of 12. Brain magnetic resonance imaging revealed restricted diffusion on diffusion-weighted imaging in the right parietal and temporal lobes. Computed tomography angiography (CTA) indicated M3 segment embolism of the right middle cerebral artery. Neck CTA revealed thrombosis of the bilateral common carotid arteries. Carotid ultrasound showed thrombosis in the bilateral common carotid arteries (approximately 2 cm below the proximal end of the carotid sinus), and contrast-enhanced ultrasound did not suggest enhancement. No hypertension, diabetes, heart disease, vasculitis, or thrombophilia was found after admission. After 1 wk of treatment with aspirin 200 mg and atorvastatin 40 mg, a carotid ultrasound reexamination showed that the thrombosis had significantly reduced.
Neck massager may cause carotid artery thrombosis.
Core Tip: It has been reported that stroke caused by a neck massager is mainly related to arterial dissection due to the tearing of the inner vessel. Herein we report a rare case of intracranial large artery embolism due to carotid thrombosis caused by a neck massager. Combined with the analysis of the cases indexed in PubMed, only one case of a free thrombus in the carotid artery has been reported, although the etiology is unclear. We found that an intracranial large artery embolism was due to carotid thrombosis caused by a neck massager, which was treated effectively by antiplatelet therapy. In the future, it may be necessary to study further and propose stricter quality management standards for massagers.
- Citation: Pan J, Wang JW, Cai XF, Lu KF, Wang ZZ, Guo SY. Intracranial large artery embolism due to carotid thrombosis caused by a neck massager: A case report. World J Clin Cases 2023; 11(11): 2489-2495
- URL: https://www.wjgnet.com/2307-8960/full/v11/i11/2489.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i11.2489
The probability of stroke caused by a neck massager is 1/300–1/400000, which is mostly related to arterial dissection due to the tearing of the vascular inner layer (mainly involving the vertebral artery, followed by the carotid artery)[1-3]. Cerebral infarction caused by arterial embolism after a massager is rare[4,5].
A neck massager stimulates the neck according to the principle of pulsed microcurrents to promote blood circulation and alleviate fatigue. In this report, we describe an intracranial large artery embolism due to carotid thrombosis caused by a neck massager.
Left lower limb weakness for more than 5 h.
More than five hours prior, left lower limb weakness suddenly occurred in a 49-year-old female patient; the left upper limb could move autonomously, but the lower limb could only shift on the bed surface. She had slurred speech, no nausea or vomiting, limb twitching, and urinary incontinence. She was given thrombolytic therapy with alteplase (50 mg) at 11:50 am in another hospital, and her symptoms did not worsen after thrombolytic treatment.
The patient had no history of hypertension, diabetes, hyperlipidemia, heart disease, smoking, or drinking.
The patient denied any family history of malignant tumors.
The patient’s vital signs were: Body temperature, 37.1 °C; blood pressure, 122/82 mmHg; heart rate, 82 beats per min; and respiratory rate, 18 breaths per min. The cardiopulmonary examination was normal. Her cognition seemed normal; her speech was a little vague; the neck showed soft passivity; the Kernig sign was negative; the pupils were symmetrical and 3 mm in diameter; the light reflex was normal; eye movement was normal; there was no nystagmus; bilateral hearing was symmetrical; bilateral nasolabial folds were symmetrical; and the tongue could be stuck out on request in the center.
Her left lower limb muscle strength was level 1, left upper limb muscle strength was level 5, right lower and upper limb muscle strength was level 5, and the tendon reflexes of the extremities were normal; the muscle tone of the extremities was normal; Babinski sign was positive on the left, but negative on the right; and bilateral acupuncture sensations and deep sensations were symmetrical. The bilateral finger-nose touch, rotation, heel, knee, and tibia tests were stable and accurate, and the closed eyes sign could not be combined. Her initial National Institutes of Health Stroke Scale (NIHSS) score was 4, the modified Rankin Scale (mRS) score was 4, and her water swallow test grade was 2.
Laboratory results were normal except for the D-dimer level at 4410.0 μg/L. In addition, her thrombophilia genes were investigated, and the results suggested two risk factors: A 2 KB heterozygous mutation upstream of PAI-1 (NM_000602.5) and a homozygous missense mutation in MTHFR (NM_005957.5).
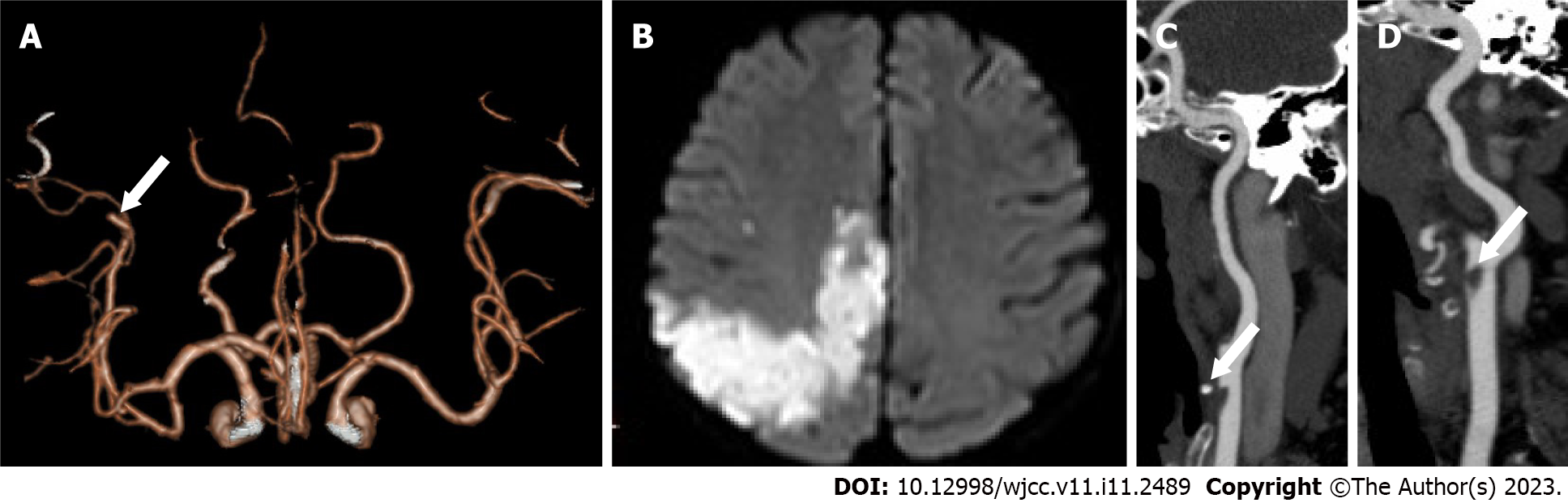
Computed tomography (CT) of the head showed no brain hemorrhage. CT angiography (CTA) revealed occlusion of the M3 segment of the right middle cerebral artery (MCA) (Figure 1A).
The next day, the patient was transferred to the neurology ward; however, the left limb weakness worsened. The NIHSS score was 12, and the mRS was 4. After 4 d of treatment, the left limb weakness improved. At discharge, the patient had improved; her NIHSS score was 2, and her mRS score was 1.
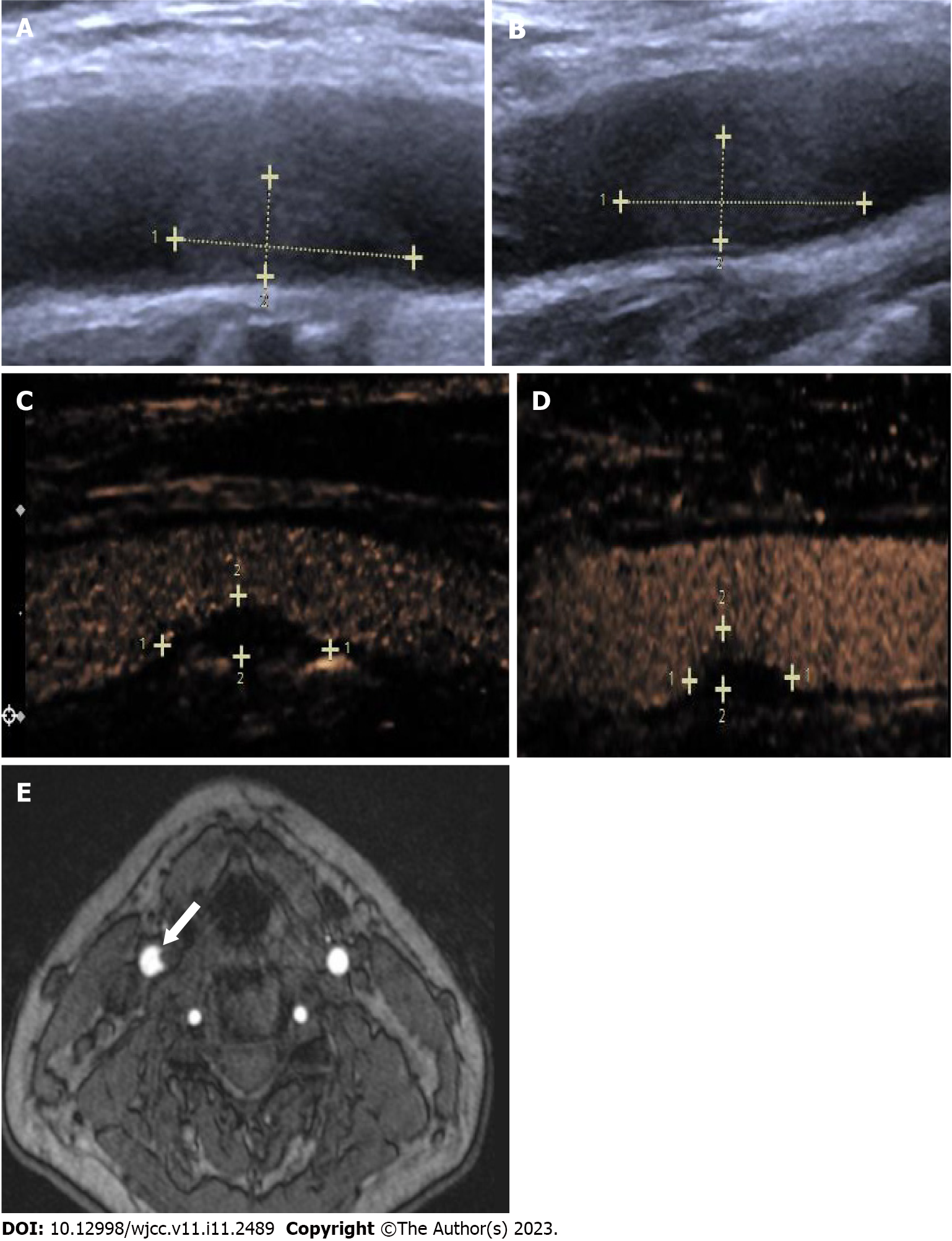
Brain magnetic resonance imaging (MRI) showed limited diffusion on diffusion-weighted imaging of the right parietal and temporal lobes (Figure 1B). CTA (Figure 1C and D) and ultrasonography (Figure 2A and B) showed bilateral common carotid artery (CCA) thrombosis. Color Doppler carotid angiography (Figure 2C and D) and high-resolution enhanced MRI (Figure 2E) suggested bilateral CCA local thrombosis. On the eighth (Figure 3A and B) and 21st (Figure 3C and D) day, carotid ultrasound was repeated, which revealed that the thrombosis was reduced in size.
Four months prior, the patient started to use a neck physiotherapy instrument for 1 mo (Figure 4) (twice a day, 15 min each time) because of neck muscle tension. Pulse massager is different from ordinary roller massager, which is simple to relax muscles, while pulse massager is a massage method that simulates electric moxibustion. Pulse electric moxibustion was carried out by electromagnetic frequency of electrode. Deep into the skin of the human body, a pulse massager carries out acupoint massage of the strain points and stimulates the shoulder and neck pain area and acupoints, so as to dredge the cervical vertebra, break up the nodules, dilate blood vessels, promote blood circulation, and improve strain, dizziness, and neck pain.
Intracranial large artery embolism due to carotid thrombosis caused by a neck massager.
The patient received intensive statin treatment (atorvastatin 40 mg).
Oral aspirin 200 mg and atorvastatin 40 mg daily were prescribed at discharge. After discharge, the aspirin was reduced to 100 mg once a day and the atorvastatin to 20 mg once a day.
After 6 mo of follow-up, there was no stroke recurrence, the patient’s NIHSS score was 1, and her mRS score was 1. No symptoms were aggravated, no complications occurred, and no adverse events were recorded. The patient is satisfied with the treatment and can now continue with normal life.
To our knowledge, this report is the first to document a stroke caused by carotid thrombosis due to a neck massager. The brain MRI of the patient showed multiple acute infarcts in the right cerebral cortex, similar to arterial embolization. The cranial CTA showed that the M3 segment of the upper trunk of the right MCA was occluded. Carotid ultrasound showed symmetrical thrombosis of the bilateral common carotid arteries. At the same time, other etiologies, such as cardiogenic, immune, infectious, and hematological diseases, were ruled out. After antiplatelet therapy, dynamic reexamination by carotid artery ultrasound showed that the thrombus had significantly reduced and eliminated 21 d after stroke onset. We believe that the neck massager destroyed the vascular endothelial cells in this patient, thus forming carotid artery thrombosis and causing an intracranial arterial embolism.
Cerebral infarction caused by neck massage is often secondary to vascular dissection[1-3]. Only one case of a free thrombus in the carotid artery has been reported, and the specific etiology is unclear[4]. Another case documented vertebral artery dissection after repetitive use of a handheld massage gun[5]. The literature has suggested that massager can make the blood in the carotid artery swirl[6]. Long-term changes in blood flow and acute injury of the artery may lead to changes in the structure of endothelial cells. The lipids exposed after plaque rupture activate platelets and the coagulation system to form thrombi, reducing the blood supply to the brain. In addition, endothelial damage may impact plaques on the arterial wall, causing them to break and fall off. Plaque shedding may lead to distal vascular embolism, which may cause vasospasm, intimal hyperplasia, and accelerated arteriosclerosis, resulting in intracranial arterial embolism[7].
The massager used by the patient in this report is based on the principle of pulsed microcurrents to stimulate local muscles and acupoints by fixing electrodes in the bilateral anterior cervical regions. Carotid and contrast-enhanced ultrasound in this patient suggested that the intima was intact, and the evidence for plaque rupture was insufficient. The possibility of endothelial damage was considered, which may be related to her mutations in MTHFR[8].
The treatment of carotid artery dissection may include antiplatelet therapy, anticoagulation therapy, or surgical treatment according to the incidence, clinical symptoms, and vascular conditions[9]. Emergency endovascular treatment may be selected for patients with acute intracranial large artery occlusion and hypoperfusion[10]. However, the intracranial occlusive segment of this patient was the M3 segment of the MCA, and there was no indication for emergency treatment. Carotid artery thrombosis is usually caused by atherosclerosis or carotid artery dissection; however, there is no clear guidance on drug treatment[11]. The patient's clinical symptoms improved after antiplatelet therapy, and the thrombus disappeared 21 d later, indicating that antiplatelet treatment was effective.
This patient had a stroke after starting to use a neck massager for 1 mo. Bilateral symmetrical thrombus signals occurred at the location of the CCA stimulated by the electric pulse, and the local intima was intact. The thrombus disappeared 21 d after antiplatelet treatment. The development of the thrombus was considered to be related to local endothelial injury after electric pulse stimulation. Different electric pulse frequencies may have varying effects on endothelial cells, and further research is needed to explore a more suitable safety frequency for users and establish a better approach to evaluating the safety of massagers.
The limitation of this case is that although the mechanism of intimal injury is proposed through ultrasound findings, there is no further pathology confirmation. In the future, more research is needed to find a safe massage power and formulate stricter quality management standards.
Neck massage may cause carotid artery thrombosis.
We would like to thank the patient and her family for their informed cooperation and support in our work.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Hui P, China; Park HK, South Korea; Sudevan R, India S-Editor: Li L L-Editor: Wang TQ P-Editor: Li L
| 1. | Kaur J, Singla M, Singh G. Frequent neck massage leading to bilateral anterior cerebral artery infarction. BMJ Case Rep. 2017;2017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Chen WJ, Qiao HY, Fang GT, Zhong X. Vertebral Artery Dissection Probably Caused by Massage: A Case Report. Chin Med Sci J. 2019;34:65-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 3. | Dutta G, Jagetia A, Srivastava AK, Singh D, Singh H, Saran RK. "Crick" in Neck Followed by Massage Led to Stroke: Uncommon Case of Vertebral Artery Dissection. World Neurosurg. 2018;115:41-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Tan AP, Taneja M, Seah BH, Leong HN, Venketasubramanian N. Acute free-floating carotid artery thrombus causing stroke in a young patient: unique etiology and management using endovascular approach. J Stroke Cerebrovasc Dis. 2014;23:e437-e439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Sulkowski K, Grant G, Brodie T. Case Report: Vertebral Artery Dissection After Use of Handheld Massage Gun. Clin Pract Cases Emerg Med. 2022;6:159-161. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 6. | Collins NA, Higgins GL 3rd. Reconsidering the effectiveness and safety of carotid sinus massage as a therapeutic intervention in patients with supraventricular tachycardia. Am J Emerg Med. 2015;33:807-809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Suwaidi JA, Hamasaki S, Higano ST, Nishimura RA, Holmes DR Jr, Lerman A. Long-term follow-up of patients with mild coronary artery disease and endothelial dysfunction. Circulation. 2000;101:948-954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1336] [Cited by in RCA: 1357] [Article Influence: 54.3] [Reference Citation Analysis (0)] |
| 8. | Çaytemel C, Topaloğlu Demir F, Büyükbabani N, Türkoğlu Z, Uzuner EG. Multifactorial Painful Leg Ulcers Due to Hyperhomocysteinemia, Plasminogen Activator Inhibitor-1 4G/5G Heterozygote Gene Mutation, and Beta Thalassemia Minor: A Case Report. Int J Low Extrem Wounds. 2019;18:339-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Keser Z, Chiang CC, Benson JC, Pezzini A, Lanzino G. Cervical Artery Dissections: Etiopathogenesis and Management. Vasc Health Risk Manag. 2022;18:685-700. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 34] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 10. | Hoving JW, Marquering HA, Majoie CBLM. Endovascular treatment in patients with carotid artery dissection and intracranial occlusion: a systematic review. Neuroradiology. 2017;59:641-647. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 11. | Singh RJ, Chakraborty D, Dey S, Ganesh A, Al Sultan AS, Eesa M, Wong JH, Goyal M, Hill MD, Menon BK. Intraluminal Thrombi in the Cervico-Cephalic Arteries. Stroke. 2019;50:357-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |