INTRODUCTION
Substance use disorder (SUD) is a mental disorder that affects nearly 20.4 million Americans[1]. SUD is defined as the inability of a person to control their use of substances such as legal or illegal drugs or medications[2]. Among the 20.4 million people with SUD, 40.7% have illicit drug disorder. Illicit drug overdoses have increased steadily in the last three decades, claiming over 900000 lives in the United States since 1999[3]. In 2020 alone, 92000 people died from illicit drug overdose in the country. Thus, SUD has been acknowledged as one of the public health priorities in the United States Opioids have recently been the largest contributor to SUD-related mortality in the country, accounting for about 75% of all drug overdose deaths in 2020[4]. Collectively, these finds make the study of the opioid epidemic a priority.
National data on SUD show that the epidemic is not homogenously distributed within the country. Overdose rates are highest and have increased in specific regions of the country, particularly in Appalachia, New England, Florida, eastern Kentucky, and the Southwest[5,6]. The type of substance contributing to most deaths also varies across the United States, with a large share of drug overdoses in the Northeast attributed to synthetic opioids (fentanyl), whereas heroin overdoses are most prevalent in New Mexico and the Midwest[7,8]. Several studies examining the attributes of the addiction epidemic in the United States have described significant demographic and spatial heterogeneities[9]. These heterogeneities have been partially attributed to the concomitant spatial heterogeneity that the United States exhibits for socioeconomic status, race and ethnicity, and comorbidities[9]. The reasons behind the geospatial heterogeneity of SUD incidence in the United States, however, are still not completely understood[10].
Socioeconomic status, accessibility to primary and mental health care, unemployment rate, urbanicity, and availability of substances have been proposed to be some of the main drivers of this heterogeneity[11-13]. In addition, rates of prescribing patterns and the accessibility of treatments to reverse overdose episodes (e.g., naloxone) have been identified as important factors associated with the uneven spatial and demographical distributions of SUD-related mortality[14-16]. Furthermore, the epidemiological attributes of the SUD public health emergency remain understudied. There is little information about where (location) and who (demographic groups) are at higher risk of developing SUD and dying of related overdoses[17]. In this perspective, spatial statistics and geospatial epidemiological models are key tools for recognizing the temporal and geographical dynamics of the epidemic[18]. The identification of the key spatiotemporal dynamics of the SUD challenge will provide significant information to identify geographic areas where vulnerable populations are located as well as potential socioeconomic drivers of the epidemic. Geospatial statistical and spatial epidemiological models can be used to develop strategies for mitigating the SUD crisis in the most affected areas and preventing future outbreaks in vulnerable communities.
This narrative minireview aims to summarize and discuss the advances in the study of the spatial distribution of the SUD epidemic in the United States. Geospatial analyses have been foundational to the study and management of many global epidemics [e.g., human immunodeficiency virus (HIV)]. However, the use of geospatial analysis to aid in the study of the SUD crisis has been limited. This minireview begins with a concise summary of the general concepts and advances in the use of geospatial methods applied in epidemiology. Then, we discuss the spatial structure of the SUD epidemic in the United States, with a detailed emphasis on Ohio because it is one of the most affected states in the country. Finally, we discuss the challenges and the future of the implementation of spatial epidemiology in the study of the SUD epidemic.
GEOGRAPHICAL INFORMATION SYSTEMS IN EPIDEMIOLOGY
Epidemiology entails the study of the distribution and determinants of health challenges in populations. Epidemiological studies have centered on recognizing the type and extent of diseases affecting human health and identifying the causes associated to disease incidence[19]. In epidemiology, it is common to assess the associations that arise among the host, the agent, and the environment (the epidemiologic triangle) to identify the primary triggers of the health challenge and produce strategies for control and prevention[20]. Conventional epidemiology has traditionally centered on persons and time, and less on place[21]. Not long ago, the spatial place at which epidemics emerge and disperse has become a critical element for understanding the dynamics of an epidemic. As a result, the interconnected fields of spatial epidemiology and health geography, which focus on explaining spatial heterogeneity of diseases by examining spatially explicit health outcomes and predictors, have emerged as novel approaches for the understanding and controlling epidemics.
The ability to understand and study the function of geographical places in health outcome dynamics has significantly improved in the past several years. This progress is mainly associated to innovations in geospatial methods such as spatial analysis and Geographical Information Systems (GIS)[22]. Together with the fast development of geospatial tools such as spatial analysis and GIS, vast quantities of spatial social, environmental and health data are currently available[23,24]. Geospatial analysis can be used to identify spatial information by recognizing relationships and drivers of disease distribution.
Epidemiological research has been fundamental for understanding health disparities and preventing an increasing incidence of major diseases. In epidemiological research, GIS has been used to study basic health and epidemiological indicators and tendencies among populations and regions. Such information is used for planning, implementation, and monitoring targeted health interventions[25,26]. GIS can also assess changes in resource allocation or environmental exposures in addition to mapping epidemiological measures such as incidence, prevalence and mortality, as well as risk factors and treatment options[26]. GIS can identify trends in access and uptake of healthcare interventions; it can also reveal unanticipated factors impacting vulnerable populations. Consequently, GIS identifies healthcare disparities and aids in equitable resource reallocation[27], and it is also used to characterize health-related economic and behavioral traits in specific populations to design geographically targeted interventions[28].
Spatial analysis in epidemiological research and disease surveillance has become a critical component of the decision-making process in the design and implementation of control interventions and prevention programs[29]. Spatial epidemiology has been used mostly for studying communicable, and relatively indirectly, non-communicable diseases. However, recently, its application has been expanded to study other public health and social issues, such as suicide and sexual violence[30-32].
EXAMPLES OF THE IMPLEMENTATION OF SPATIAL EPIDEMIOLOGY TO STUDY DISEASE BURDEN
Spatial epidemiology is now a critical tool in the battle against harmful epidemics such as HIV and malaria. The quantitative methods for assessing the impact of geographical hotspots (areas suffering an excessively large burden of the health challenge) and determinants of the ecological and individual-level transmission have facilitated the control of these diseases[33]. The detection of these areas can reveal the locations of high-risk populations in addition to exposing the causes that enable the spread and persistence of epidemics[34].
One of the most successful examples of the implementation of spatial epidemiology and GIS is the Malaria Atlas Project (MAP)[35], a project funded by the Bill and Melinda Gates Foundation and developed by Oxford University. MAP has focused on understanding the spatial distribution of malaria, particularly in sub-Saharan Africa (SSA). Using spatial epidemiology and disease mapping techniques, MAP has uncovered the spatial distribution of malaria with a high level of detail. The spatial information provided by MAP has become a key tool in the fight against malaria in SSA identifying geographical regions that should be targeted through control efforts. Similarly, successful approaches like the “Know your epidemic, know your response”; a framework implemented for counteracting HIV epidemics in the world[36], have centered on the development of targeted prevention strategies based on detailed knowledge of the spatial dynamics of the epidemic. Healthcare providers have developed and used high-resolution maps of the HIV distribution in SSA to implement geographically-targeted, cost-effective interventions[37,38].
SPATIAL EPIDEMIOLOGY OF SUD
Despite spatial epidemiology’s positive impact, there is limited research focused on how it can be used to manage the SUD epidemic in the United States. Unlike the previous examples of malaria and HIV, SUD is not an infectious disease. However, the incidence of SUD is dependent on several socioeconomic and demographic health determinants such as gender, age, income, education, and access to healthcare among others, factors that are strongly connected to the geographical location of individuals and communities[39]. In this context, geographical place provides a foundation for understanding how substance use-related behaviors, treatment, and prevention relate to spatial features that compose the geographical space, from the individual to the community and regional scale. Within this framework, SUD is a negative health behavior shaped by a spatial context that includes local access and cost of substances, access to resources and services, emerging social networks, economic conditions and cultural norms, and other specific socioeconomic characteristics that either enhance or reduce the exposure to substance use in a given geographical place[40]. Moreover, the intensity and effectiveness of treatment and prevention strategies for SUD vary from place to place, reflecting social, economic, and political factors that intersect around the community environment. Thus, spatial research on SUD requires analysis in a geographical context at different scales.
GIS and geospatial analyses can be used as powerful tools in the study of the SUD epidemic. For example, the place of prescribing and dispensing opioids can be mapped and spatially analyzed, though illicit substance distribution is more complex as drugs can be transported between areas. Still, both licit and illicit distribution and demand can be locally defined, and thus could exhibit specific spatial patterns[41]. The location of identified harms can be used as a sign of where substances are used, which can be linked to the location of the markets. Such information can be used to identify flows of the substances from the moment of dispensing to the point of use. Some studies have mapped the locations of such harms[42], as well as to find spatial hotspots of harms[43], how these harms diffuse in space[44] and their relationships with several individual and area-level predictors[45]. Analyzing changes in the spatial patterns of SUD dynamics over time is also important for understanding the impact of policy adjustments on substance use. For example, how is SUD-related mortality linked to environmental and social risk factors? How do social and economic factors influence the prevalence of drug users? Are rates of specific drug use elevated around drug production markets? These fundamental inquiries about the epidemiology of SUD can be addressed using a spatial epidemiology approach. For example, this approach was implemented in a report from North Carolina that observed an ecological correlation between rates of admission to Emergency Departments from opioid overdoses and rates of opioid sales[45].
The common understanding that addiction does not discriminate and everyone is at risk ignores the fact that the frequency of SUD cases varies significantly in space and that cases are commonly clustered in places characterized by specific socioeconomic and demographic factors such as income, education, crime levels, access to care, drug availability among others. Thus, while the underlying physiological processes linked to addiction may not discriminate, several socioeconomic and environmental factors that expose individuals and communities to increased risk of substance use are not spatially random. Therefore, the identification of vulnerable populations and locations at higher risk of SUD, as well as the drivers of SUD epidemics, are key to improving health policies and developing effective spatially-targeted prevention strategies.
SPATIAL EPIDEMIOLOGY OF SUD IN THE UNITED STATES
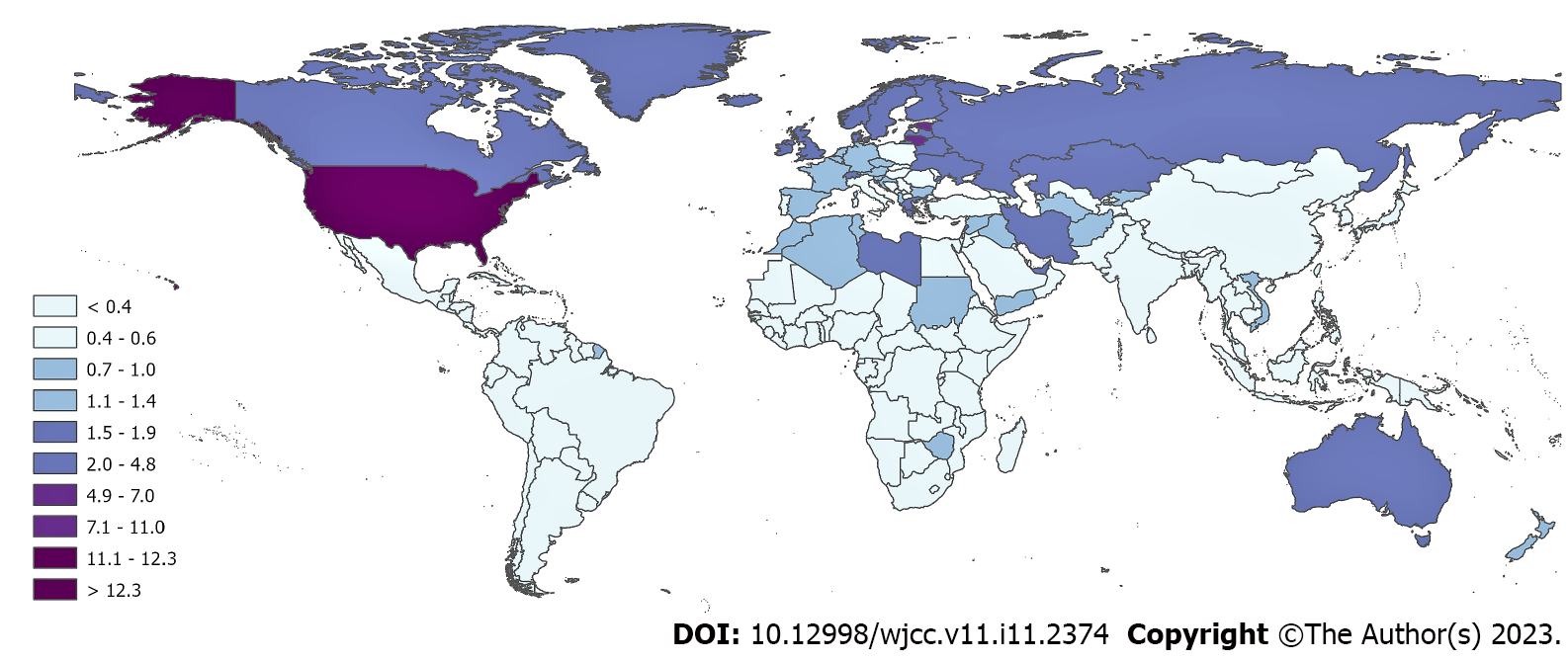
The United States is the country with the highest incidence of SUD and the highest burden of opioid overdose-related mortality in the world (Figure 1). As a result, SUD has been declared a top public health priority in the country[46]. In an attempt to understand the reasons behind this burden, numerous studies have investigated multiple attributes of the SUD epidemic in the United States. A growing body of evidence has shown associations between demographic and socioeconomic factors with SUD outcomes[47-49]. Other studies have found a strong connection between drug supply and a rise in drug mortality rates. These data suggest that the SUD crisis in the United States has been driven by changes in the dynamics of drug supply, availability, and distribution. For example, the opioids overdose crisis can be explained by the rise in prescription opioids in the late 1990s and 2000s, more than by social or economic conditions[8,50]. As a result, policymakers in the United States have applied several strategies to reduce SUD-related mortality levels. These measures have focused on restrictions to drug availability, including regulating the prescription of opioids, attempts to restrict the influx of illicit opioids, and increasing access to naloxone, a medicine that rapidly reverses an opioid overdose[51-54]. Although these efforts have been moderately effective in reducing SUD-related mortality rates in general, other strategies like identifying the areas and vulnerable populations that are suffering the highest burden of the epidemic in the United States would improve the capacity to implement prevention strategies, which have been shown to be more effective in controlling other diseases than coercive intervention strategies alone[36].
Figure 1 Death rates (number of deaths per 100000 individuals in 2019) from opioid overdoses in the world.
Source: IHME, Global Burden of Disease, 2019 (https://www.healthdata.org/gbd/2019). Maps were generated using ArcGIS Pro. 2.8[86].
National data on SUD-related mortality have shown that the epidemic is not uniformly distributed within the United States[55]. The reasons behind the heterogeneous spatial distribution of the SUD epidemic within the country are relatively unknown. Although a link between illegal and prescription drug availability and SUD-related deaths has been described, the major reasons behind the sharp increase in the epidemic in specific areas remain incomplete[10]. In addition, the epidemiological characteristics of the SUD epidemic remain underexplored, what factors are boosting the epidemic, and where and what demographical groups are at higher risk in recent years[17,18], particularly at the local level[56,57]. Understanding the geographical distribution of SUD at this level of specificity may enable the implementation of public health intervention strategies and elucidate geographically specific risk management responses. It also facilitates the identification of contextual factors that contribute to and may increase the risk of drug misuse, including health-related, economic, socio-cultural, and local policy-relevant attributes. Geospatial analyses at this more granular local level could contextualize these individual and community factors linked to SUD and other risk behaviors[43].
Aligned with the “Know your epidemic, know your response” approach that has been successfully implemented to tackle the HIV epidemic[36], we previously conducted a detailed spatial analysis to identify the vulnerable populations and locations at higher risk of SUD-related mortality as well as the drivers of the current SUD epidemic in the United States[58]. Using a repertoire of interdisciplinary methods, including spatial epidemiology, disease mapping, and statistical modeling, we examined data provided by the Centers for Disease Control and Prevention on more than 22 million deaths from 2005 to 2017[59]. We obtained information about drug overdose deaths for persons aged five to 84 years to estimate SUD mortality rates in the United States. These rates included deaths caused by heroin, methadone, cocaine, opioids, synthetic narcotics, and unspecified narcotics. The main finding of this study is that the SUD epidemic in the United States is typified by the occurrence of several micro-epidemics of distinct intensities across geographical locations and demographic groups within the country. We found that White males, particularly those aged 25-34 years, had the highest risk of SUD-related death. Recently, there has been a rapid rise of the SUD epidemic in the Black male population, with a rapid increase in the SUD-related mortality rate in this group since 2014, reaching a death rate similar to that for White males in 2017. The temporal dynamics of the epidemic can be the result of changes in the substances driving the epidemic, switching from prescription opioids mostly affecting the White male population to more readily available synthetic opioids leading to the latest phase of the epidemic and affecting the Black male population.
The notable disparity among gender and racial groups could be associated with the temporal trend associated with three different waves in the SUD epidemic[60]. Briefly, the first epidemic wave from 1970 to 1999 was driven by heroin overdoses, which affected the Black population at higher rates than other racial populations. Prescription opioids frequently used for pain management therapy served as the primary driver of the second wave, which spanned the years from 1999 to 2010 and caused a more pronounced rise in death rates among White people[61,62]. The emergence of synthetic opioids and the combination of prescription opioids are primarily blamed for the third and most current wave[63]. This most recent wave has revealed a comparable increase in both racial groupings across the country (White and Black)[61].
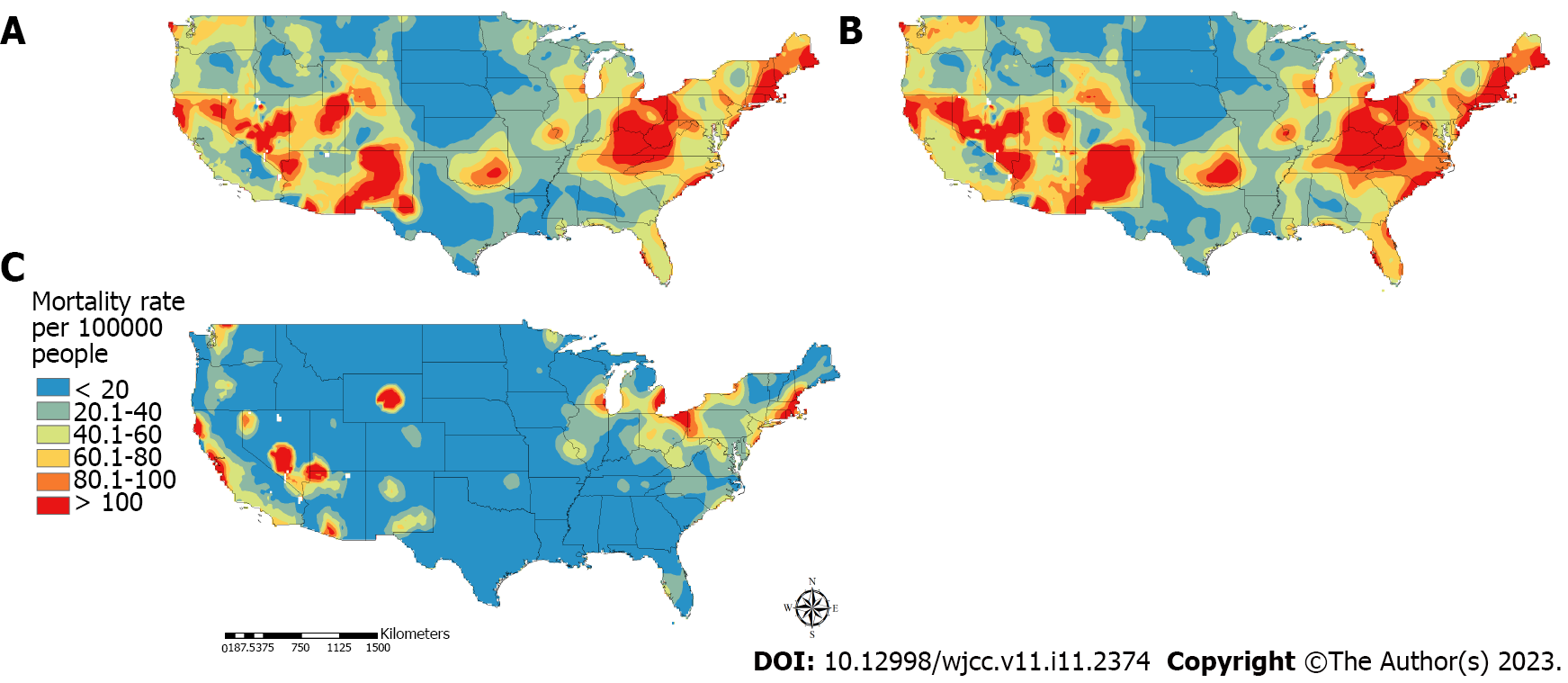
Further analysis revealed that the epidemic is concentrated in specific geographic areas located in the West and Midwest regions (Figure 2A). The majority of SUD-related deaths occurred in regions of the Midwest around the tri-state border of Kentucky, Ohio, and West Virginia. Southern Pacific and mountain states, including California, Colorado, Nevada, New Mexico, and Utah, are other regions with a high proportion of SUD-related mortality. The spatial structure of the epidemic in the White population had a similar pattern as observed for the general population (Figure 2B). In contrast, the epidemic in the Black population was concentrated in the mid-Atlantic and Northeast (e.g., Connecticut, Rhode Island, Massachusetts, and New Hampshire) and the West (e.g., California, Nevada, and Arizona) (Figure 2C).
Figure 2 Spatial distribution of the substance use disorder related mortality.
A: The general population; B: White population; C: Black population in the contiguous United States. Maps were generated using ArcGIS Pro. 2.8[86].
It is important to note that, as the United States Department of Health and Human Services declared in 2018[64], overdoses caused by synthetic opioids (such as fentanyl and analogs) are developing into a nationwide public health disaster. Opioid overdose deaths frequently result from prior drug use, which frequently starts between the ages of 18 and 25[63]. Teenagers who have a history of substance abuse are 10 times more likely than other teenagers to have drug use disorders in the future[60]. People between the ages of 25 and 44 may start taking opioids for recreational or therapeutic purposes before switching to more affordable drugs like fentanyl[65]. Our findings, which indicate that the young adult population (25–39 years) was bearing the greatest burden of opioid overdose deaths and was likely in the latter stage of an opioid use disorder history, are consistent with this early onset of substance addiction.
These comprehensive geographical and epidemiological descriptions of the vulnerable populations at high risk of the SUD epidemic in the United States can be applied to generate spatially targeted prevention strategies and intervention campaigns. Geospatial approaches and data visualization technologies (e.g., GIS maps) generate unique opportunities for the early detection of the impacts of highly affected areas and then assess, diagnose, and treat those vulnerable communities affected by this health challenge. Geospatial data acquired from GIS maps support the visualization of SUD events that can be rapidly analyzed, permitting the detection of patterns and the creation of plans to monitor trends in data and co-locate needs and resources[66]. The development of targeted, integrated, preventive strategies for the early identification of substance use in the vulnerable populations nationwide would be made possible by micro-targeting strategies based on an understanding of the spatial assembly and the multifactorial characterization of the addiction epidemic[6,67]. Such strategies have been shown to be successful in areas in New York City and Cambridge, MA, that are highly affected by SUD. In these areas, geospatial analyses have been used to identify priority targets for the deployment of naloxone as a key element of their SUD intervention programs[68,69].
GEOGRAPHICAL PROFILE OF THE OPIOID OVERDOSE EPIDEMIC IN OHIO
Spatial variation of health outcomes occurs at different scales, from a large national level to a local scale. Similarly, the drivers of disease distribution can influence the spatial structure of epidemics at different scales. As we have shown in the previous section, the SUD crisis in the United States is not homogeneously distributed across the country. For example, national data on SUD overdose mortality rates have shown that 20 states and the District of Columbia have reported SUD-related mortality rates that are statistically higher than the national rate. In particular, West Virginia (57.8 SUD-related deaths per 100000 persons), Ohio (46.3), Pennsylvania (44.3), the District of Columbia (44.0), and Kentucky (37.2) experienced the highest death rates in 2017[70]. Therefore, a more detailed local description of the epidemic can uncover local drivers of the epidemic in each of these affected areas. As a result, a more thorough local description of the epidemic can reveal the outbreak's regional causes in each of these impacted locations. As previously indicated, opioids are the leading cause of SUD-related mortality in the nation, accounting for over 75% of all drug overdose deaths in 2020[4]. Ohio is one of eight states where the opioid mortality rate doubled between 1999 and 2019, with data being released every three years. Unintentional drug overdose deaths in Ohio have reached record highs, especially those caused by synthetic opioids[7,71].
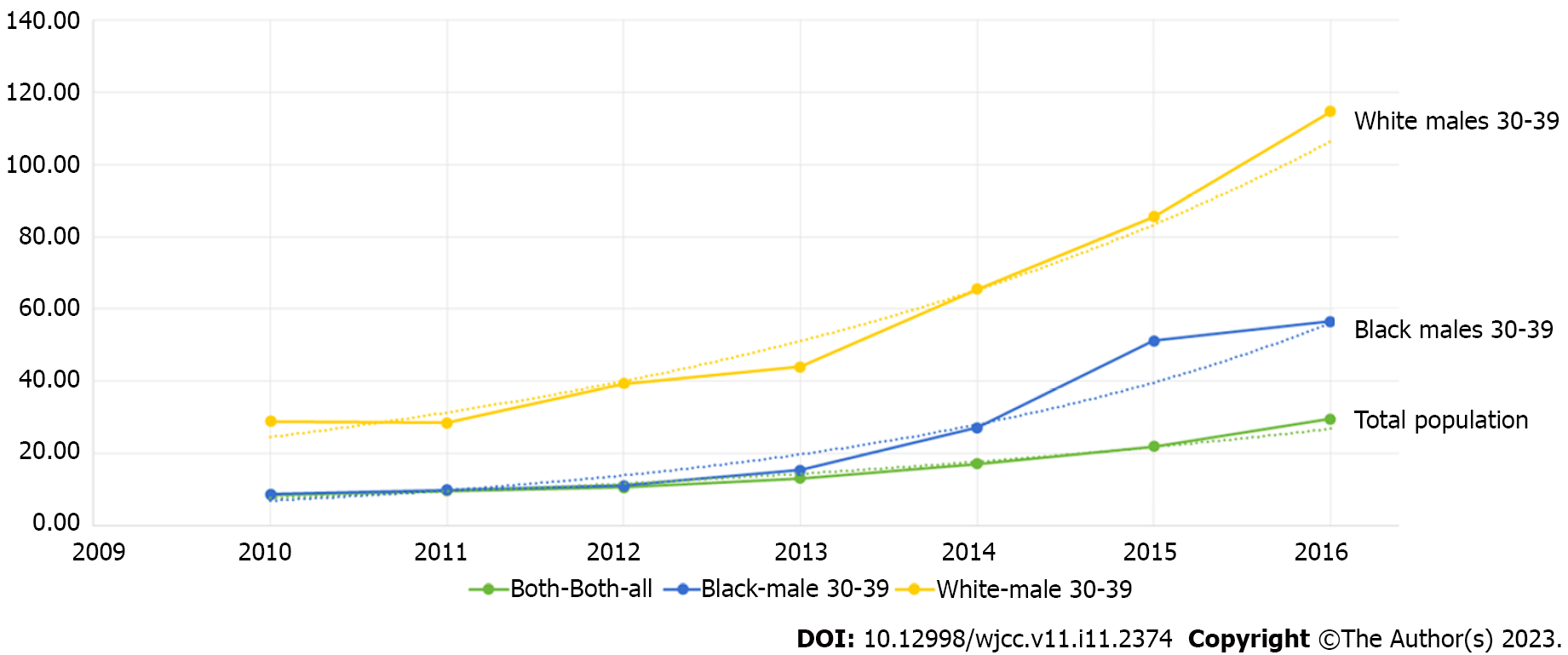
In a previous study[72], we analyzed the geographical and temporal dynamics of the opioid overdose epidemic in Ohio using data from the Ohio Department of Health. We examined data on more than 11000 opioid related death cases in Ohio occurring from 2010 to 2016. We found that the opioid overdose epidemic in Ohio was located in specific areas (hotspots) and affected limited demographic groups during this time period. There was a fast surge in prescription opioid death rates among the White male population aged 30-39 years and a rise of the epidemic in the Black male population. White males had the highest mortality rate caused by opioid overdose deaths with 43.7 deaths/100000 persons, followed by Black males with 27.3 deaths/100000 persons, and in general, the opioid overdose mortality rate was exponentially increasing in all of these groups from 2010 to 2016 (Figure 3).
Figure 3 Temporal dynamics of the opioids overdose epidemic in Ohio (2010–2016) in the total population and in the most affected populations.
The highest prescription opioid overdose mortality rates were found in the White male population aged 30-39 years, with 125 deaths/100000 persons, followed by Black males of same age, with 57 deaths/100000 persons compared to the 29 deaths/100000 persons for the total population in 2016. Dashed lines illustrated the fitted exponential curve for each growth rate. Plot was created using the software environment R[87].
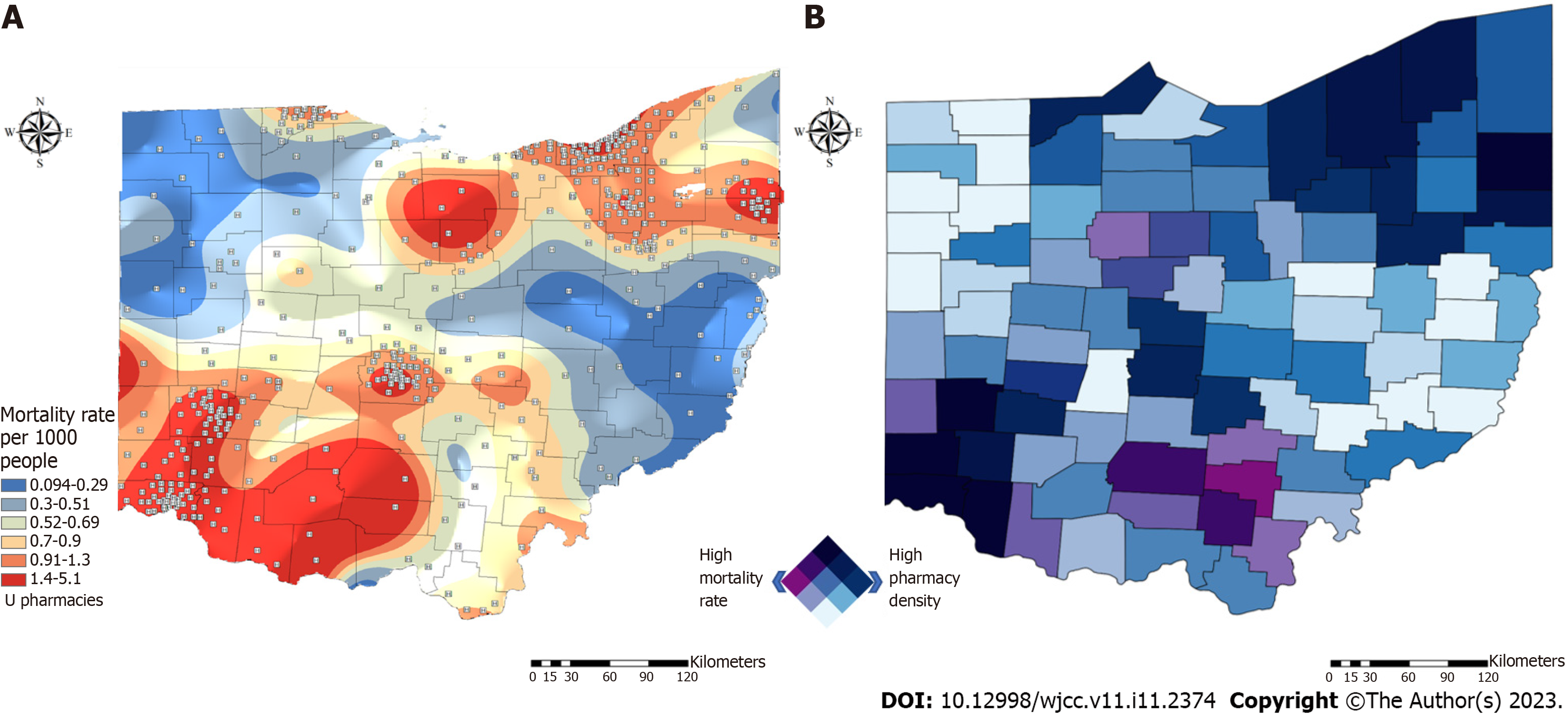
The geospatial analysis conducted suggested that most of the deaths were geographically clustered within the Ohio counties of Butler, Clark, Clermont, Cuyahoga, Franklin, Hamilton, Marion, and Montgomery (Figure 4A), where the average mortality rate caused by opioid overdose was more than eight times higher (199/100000 persons) than the state average (29/100000 persons). These results support our observations that, comparable to the national patterns observed, the opioid overdose epidemic in Ohio is concentrated in geographic hotspot areas and vulnerable populations at risk of opioid overdose. Figure 4A also illustrates the distribution of pharmacies that dispense naloxone in Ohio. There is a high density of pharmacies in the main cities and metropolitan areas of Cincinnati, Columbus, and Cleveland. In further analyses, we found that the average distance between opioid overdose death locations and the nearest pharmacy dispensing naloxone was 3.15 km (1.96 mi). We estimated that in 14% of Ohio, the nearest pharmacy with an established protocol for naloxone dispensing was located more than 10 km (6.2 mi) away from the location of the opioid overdose death. We also identified counties (e.g., Ross, Hocking, Pike, Jackson, Vinton, and Gallia) that had high mortality rates but low density of pharmacies (Figure 4B). These results identified specific underserved areas for naloxone distribution characterized by high SUD mortality rates that would benefit from an increase in the response capacity for these areas.
Figure 4 Spatial distribution of the opioid overdose epidemic in Ohio.
A: Spatial distribution of opioids overdose mortality rate in Ohio; B: Bivariate map illustrating counties with high opioid overdose mortality rate (purple) and high density of pharmacies (blue). Counties in dark color have both high opioids overdose mortality and density of pharmacies dispensing naloxone. Maps were generated using ArcGIS Pro. 2.8[86].
Overall, these findings highlight the necessity of concentrating local public health initiatives on vulnerable populations and high-risk locations in order to not only contain the current SUD epidemic in Ohio but also to educate other states across the nation experiencing comparable local epidemics. It's possible that the opioid overdose epidemic will keep growing. Therefore, to combat the epidemic's present rising phase, it is essential to recognize economic, social, and health determinants[73]. The opioid crisis is a complicated epidemic that may have been started by unchecked prescribing of painkillers. Nevertheless, it has also recently been fueled by the introduction of synthetic opioids intended for recreational use, particularly fentanyl and its analogs. It's important to emphasize that in order to highlight the local spatial differences of the SUD epidemic, we only included data from January 2011 to December 2016 in the instances presented here. According to reports, there was a decline in opioid overdose deaths in Ohio beginning in the final semester of 2017 and early 2018, followed by a rebound in 2019 and 2020. This is thought to be due to the availability of more potent drugs such as carfentanyl on the state's and the nation's black market[74,75].
CONCLUSION
The role of spatial epidemiology and geographic methods for the study of drug abuse continues to grow. The combination of geographical and epidemiological research methods focused on human and social environment interactions is essential to gain a better understanding of drug use issues and their inherent complexities. The use of geospatial analysis to target areas with high SUD risk can allow for a more comprehensive understanding of the socioeconomic and demographic drivers of the SUD epidemic in the United States. While the SUD epidemic still disproportionately affects higher-poverty areas and racial minorities, SUD-associated deaths have become more dispersed across broader geographic areas and sociodemographic groups.
In this narrative minireview, we summarized current research that applied geospatial techniques to the study of the ongoing SUD epidemic in the United States. SUD rates may continue to increase over time, and different areas and populations are affected with different intensities by this epidemic in the country. While socioeconomic or geographic characteristics of specific neighborhoods can contribute to the impact of the SUD epidemic in vulnerable communities in the country at different intensities[42,76,77], specific social, geographical, and economic determinants are numerous and the ability to isolate one variable is still challenging[77-79]. Therefore, identifying who is most likely to be affected and where they are located is critical to effectively confront this epidemic[73].
Strategies to tackle the SUD epidemic include identifying the demographic and socioeconomic drivers of the epidemic and targeting improved interventions and access to them (e.g., access to naloxone). Furthermore, the establishment of safe places for regulated drug use can help to prevent death and avoid the spread of other diseases[73,80]. There are several challenges, however, such as the constrained geography of most of the studies: Most have been conducted in major metropolitan areas, which have been heavily affected by the epidemic. Still, substance abuse is certainly not limited to these places. The impact of the SUD epidemic in small towns and rural areas is understudied. Spatial techniques such as GIS are needed to learn more about these areas[81]. Measuring the SUD epidemic at the local level is a challenge that has significant consequences on resource allocation.
Furthermore, geospatial analyses are usually ecologic studies that cannot account for decedent characteristics, including duration of county residence, and data aggregation precludes the inclusion of information such as race/ethnicity, sex, and age and the subsequent identification of important demographic variation in the epidemic[82]. Associations between the risk factors and SUD-related mortality rates may vary across groups[83]. Likewise, adults and adolescents may display distinct spatial trends and need unique interventions and resources, making it important to examine the problem at different demographic scales[84]. Promising advances in geospatial methods are making this possible, but more work is necessary to identify the methods and to analyze the results of their applications.
The federal, state, and local governments in the United States have implemented a number of intervention strategies to lower the mortality rates associated with SUD, including initiatives to reduce the flow of illegal opioids, restrictions on the prescription of opioids, and increased access to naloxone. While efforts like these and others have been somewhat successful in lowering overdose mortality rates overall, pinpointing the regions and populations most vulnerable to the various sub-epidemics would make it easier to plan prevention and control campaigns, which have been shown to be more successful in combating other diseases than broad intervention strategies alone[36]. Furthermore, identifying the extent to which geographical factors and social context are interrelated is a key step to generate a more comprehensive understanding of the SUD epidemic. All domains of the SUD epidemic including demand, supply, harms and harm reduction, can have a distinct geographic dimension[41]. As a result, the geographical and epidemiological identification of vulnerable groups in the United States at high risk of SUD-related mortality presented in this minireview can be used to develop geotargeted preventative strategies and intervention initiatives. Targeted tactics based on a knowledge of the geographical structure and multidimensional character of the addiction epidemic would aid in the development of coherent preventive treatments for early diagnosis in the young adult population[6,67,85,86]. Nonetheless, there is an undeniable need for more comprehensive initiatives targeted at understanding the epidemic, such as a focus on possible disparities among demographic groups and locations with vulnerable populations at high risk of drug use.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): A, A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Long X, China; Wang T, China; Welter J, Switzerland S-Editor: Fan JR L-Editor: A P-Editor: Fan JR