Published online Apr 6, 2023. doi: 10.12998/wjcc.v11.i10.2355
Peer-review started: December 26, 2022
First decision: January 30, 2023
Revised: February 5, 2023
Accepted: March 9, 2023
Article in press: March 9, 2023
Published online: April 6, 2023
Processing time: 94 Days and 5 Hours
We report a rare case of full neurological recovery from severe nonexertional heat stroke in a 67-year-old woman with an initial Glasgow Coma Scale of 3. This report raises awareness among doctors that when heatstroke is diagnosed, comprehensive treatment should be implemented as soon as possible. Moreover, targeted temperature management, combination therapy with hemodialysis and hemoperfusion, and hyperbaric oxygen therapy may alleviate multiorgan failure and prevent neurological sequelae caused by heatstroke.
A previously healthy 67-year-old woman with an initial Glasgow Coma Scale of 3 was found lying prone on the road at noon on a summer day. Laboratory tests revealed multiorgan failure. As soon as heatstroke was diagnosed, comprehensive treatment was implemented. On hospital Day 3, the patient was extubated. Her initial Sequential Organ Failure Assessment score at hospitalization was 14 and decreased to 2 on hospital Day 4. On the seventh day following hospital admission, as the patient’s general condition improved, the levels of laboratory test findings decreased rapidly. Finally, the patient gradually recovered with no other neurological symptoms (the Glasgow Coma Scale at discharge was 15, and her ability to walk independently was restored).
This case demonstrated that targeted temperature management, combination therapy with hemodialysis and hemoperfusion, and hyperbaric oxygen therapy may alleviate multiorgan failure and prevent neurological sequelae caused by heatstroke.
Core Tip: We report a rare case of full neurological recovery from severe nonexertional heat stroke in a 67-year-old woman. As soon as heatstroke was diagnosed, comprehensive treatment was implemented. Laboratory tests revealed multiorgan failure. However, the patient gradually recovered consciousness with no other neurological symptoms. This case demonstrated that targeted temperature management, combination therapy with hemodialysis and hemoperfusion, and hyperbaric oxygen therapy may alleviate multiorgan failure and prevent neurological sequelae caused by heatstroke.
- Citation: Du F, Zheng JW, Zhao YB, Yang K, Li HN. Full neurological recovery from severe nonexertional heat stroke with multiple organ dysfunction: A case report. World J Clin Cases 2023; 11(10): 2355-2362
- URL: https://www.wjgnet.com/2307-8960/full/v11/i10/2355.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i10.2355
Among all heat-related illnesses, heatstroke is the most severe and is defined by a condition in which the core body temperature exceeds 40℃ following a tremendous environmental heat load that overrides the body’s heat dissipation efforts[1]. It is accompanied by clinical central nervous system dysfunction (such as delirium, convulsions, or coma) and/or multiorgan failure[2]. With delayed therapy, the mortality rate can be as high as 70%, especially among elderly patients. Early diagnosis and management with immediate cooling can reduce the mortality rate to 10%[3].
There are no therapeutic strategies to prevent further injury after the rapid cooling of the core body temperature to 39℃ following heat stroke. Studies have demonstrated that early initiation of the targeted temperature management (TTM) technique can reduce free radicals that are produced during the cerebral hypoxia ischemia and reperfusion process, as well as the energy expenditure and metabolic rate of the brain[4,5]. Most researchers believe that the target temperature should be set at 32 to 34℃, and the duration of TTM is usually < 72 h[6]. However, there are no standard guidelines or unified management methods for TTM. Thus, the previous cooling method of just falling below 39℃ may not be adequate to treat heatstroke, and more aggressive cooling measures, similar to the TTM (< 36℃ for 24 h) that is routinely administered to patients in postcardiac arrest, are recommended. Continuous renal replacement therapy can effectively lower body temperature, inhibit the inflammatory cascade reaction, and reduce the concentration of toxic metabolites in serum[7]. Hyperbaric oxygen therapy utilizes high-pressure oxygen to create a therapeutic effect for ischemia reperfusion injury in cells. Through hyperbaric oxygen therapy, the oxygen content and diffusing capacity of brain tissue are increased[8]. Consequently, for the management of heatstroke patients, we propose a method that includes inducing TTM (34℃) for 24 h, hemodialysis in combination with hemoperfusion, and hyperbaric oxygen therapy to prevent neurological sequelae and alleviate multiorgan failure caused by heatstroke. It is possible that patients who suffer from heatstroke would have a better prognosis by implementing this approach.
Unconsciousness, accompanied by high fever and convulsions for more than 5 h.
The patient denied a history of present illness.
The patient denied a history of medical illness.
The patient had no relevant personal or family history.
Upon arrival of the emergency physician, the patient suffered from convulsions and dyspnea; at that time, the axillary temperature was measured at 42℃. She was immediately transferred to our emergency department (ED) by an ambulance. Physical examination revealed a deep coma with a Glasgow Coma Scale of 3, blood pressure of 91/55 mmHg, heart rate of 120 beats/min, respiratory rate of 28 breaths per minute, and her rectal core temperature was as high as 41℃.
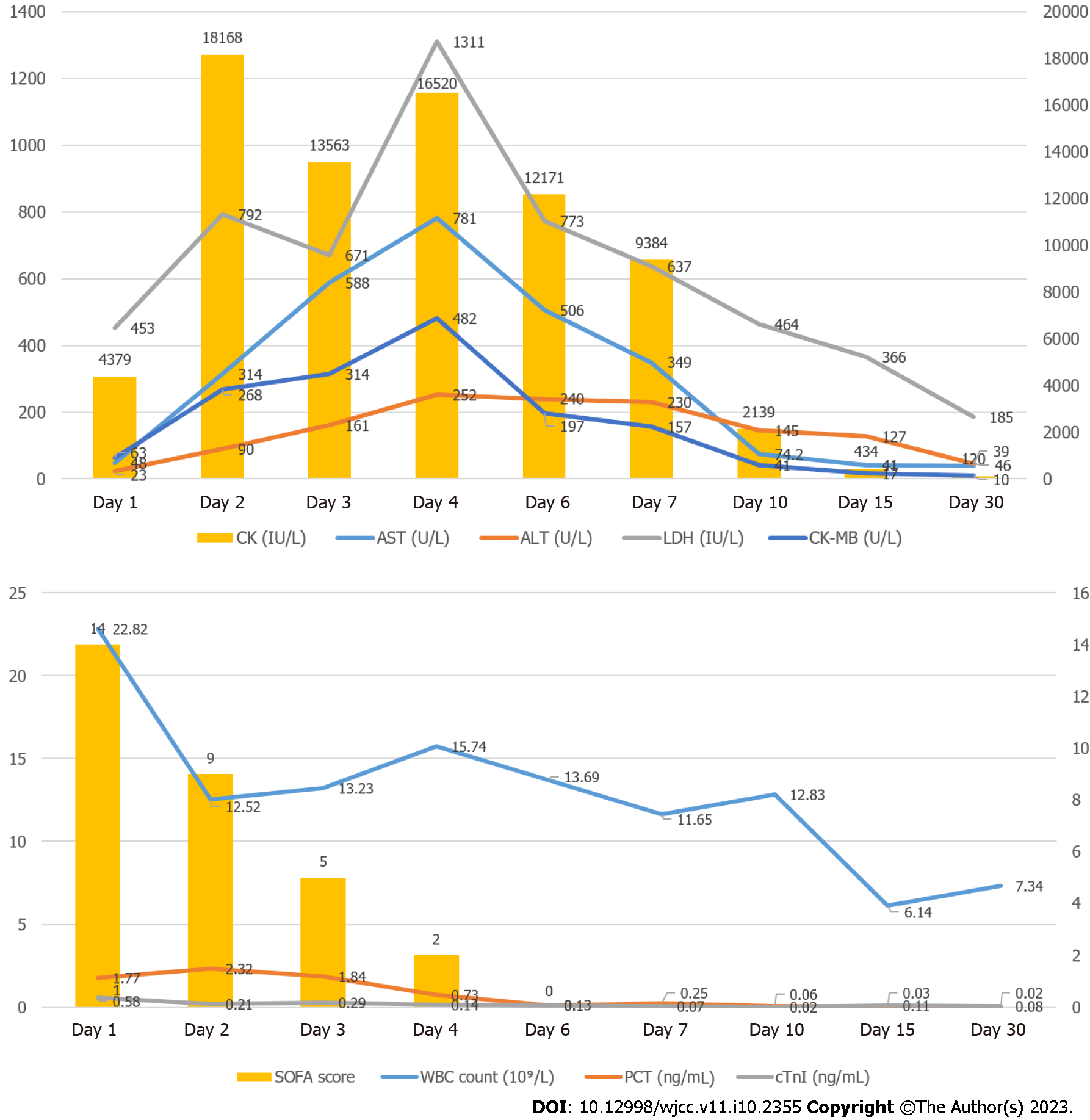
The initial laboratory test findings are shown in Table 1 and Figure 1. Abnormal findings included elevated white blood cell count 22.82 × 109/L, serum creatine kinase (CK) 4379 IU/L, as well as elevated creatine-kinase-MB (CK-MB), procalcitonin (PCT), blood urea nitrogen (BUN), and positive troponin-T. Her initial Sequential Organ Failure Assessment score at hospitalization was 14 and decreased to 2 on hospital Day 4.
| Laboratory finding | Day 1 | Day 2 | Day 3 | Day 4 | Day 6 | Day 7 | Day 10 | Day 15 | Day 30 |
| WBC count (109 /L) | 22.82 | 12.52 | 13.23 | 15.74 | 13.69 | 11.65 | 12.83 | 6.14 | 7.34 |
| Hemoglobin (g/dL) | 10.5 | 11.2 | 10.4 | 10.4 | 10.0 | 9.6 | 9.4 | 9.6 | 10.0 |
| Platelet count (109/L) | 169 | 115 | 79 | 80 | 96 | 106 | 252 | 305 | 280 |
| PCT (ng/mL) | 1.77 | 2.32 | 1.84 | 0.73 | 0.13 | 0.25 | 0.06 | 0.03 | 0.02 |
| PT (s) | 17.2 | 22.1 | 16.7 | 12.1 | — | 11.1 | 12.1 | 10.9 | 11.1 |
| APTT (s) | 26.5 | 44.3 | 30.7 | 27.7 | — | 26.6 | 25.6 | 28.6 | 26.0 |
| Fibrinogen (g/L) | 3.02 | 2.91 | 3.07 | 4.83 | — | 4.35 | 3.85 | 2.95 | 3.08 |
| D-dimer level (mg/L) | 3.23 | 1.71 | 2.23 | 1.25 | 1.45 | 1.10 | 1.15 | 1.85 | 1.02 |
| BUN (mmol/L) | 4.95 | 1.54 | 3.73 | 4.07 | 4.09 | — | 3.67 | 3.67 | 4.34 |
| Creatinine (umol/L) | 129.6 | 47.0 | 69.2 | 57.4 | 46.7 | — | 36.0 | 36.0 | 61.7 |
| AST (U/L) | 48.0 | 314.0 | 588.0 | 781.0 | 506.0 | 349.0 | 74.2 | 41.0 | 39.0 |
| ALT (U/L) | 23.0 | 90.0 | 161.0 | 252.0 | 240.0 | 230.0 | 145.0 | 127.0 | 46.0 |
| TBil (umol/L) | 35.1 | 43.7 | 25.6 | 27.1 | 27.1 | 22.8 | 14.0 | 11.0 | 15.0 |
| LDH (IU/L) | 453.0 | 792.0 | 671.0 | 1311.0 | 773.0 | 637.0 | 464.0 | 366.0 | 185.0 |
| CK (IU/L) | 4379 | 18168 | 13563 | 16520 | 12171 | 9384 | 2139 | 434 | 120 |
| CK-MB (U/L) | 63 | 268 | 314 | 482 | 197 | 157 | 41 | 17 | 10 |
| cTnI (ng/mL) | 0.58 | 0.21 | 0.29 | 0.14 | 0.10 | 0.07 | 0.02 | 0.11 | 0.08 |
| SOFA score | 14 | 9 | 5 | 2 | 0 | - | - | - | - |
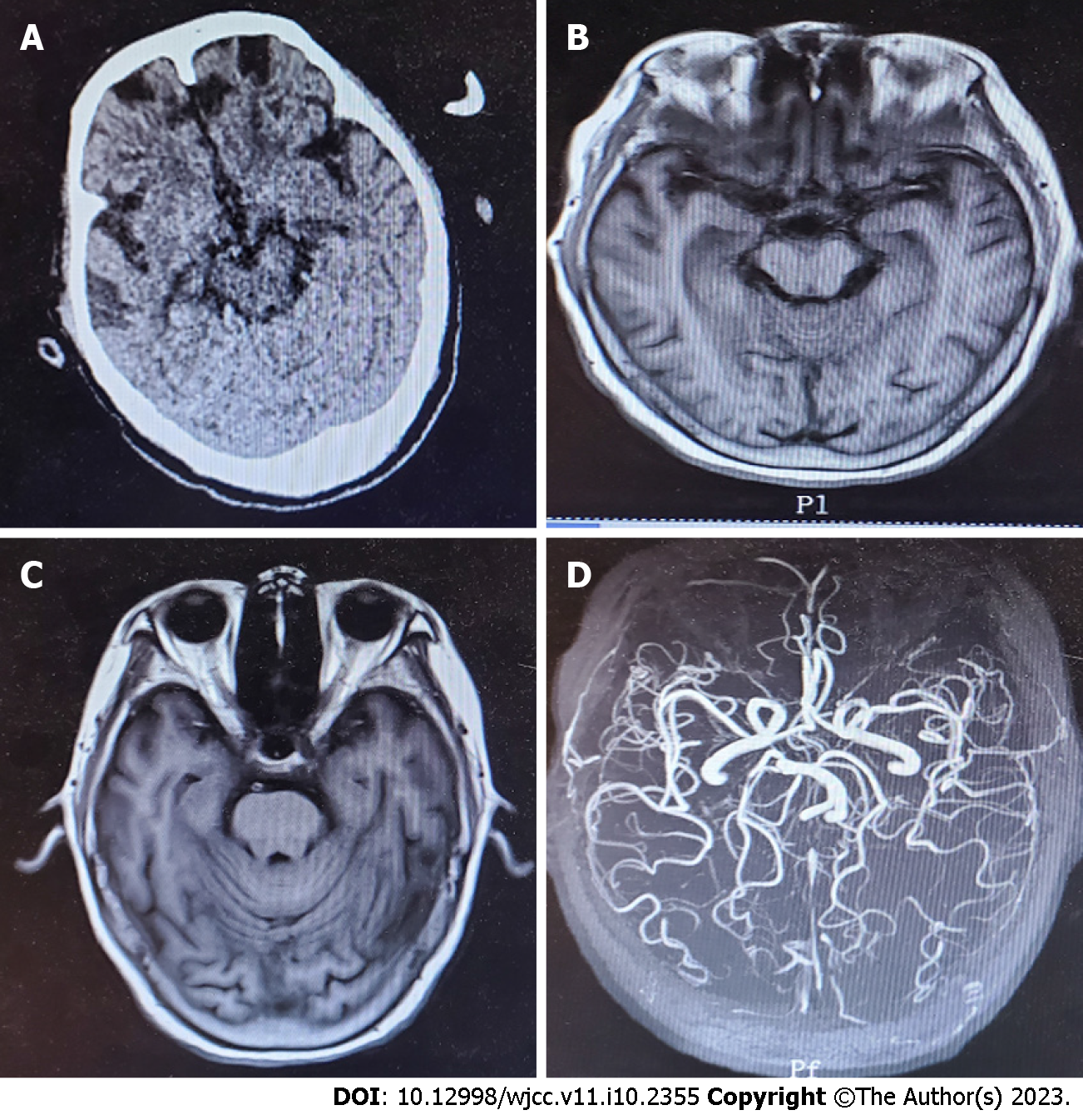
Head computed tomography (CT) and magnetic resonance imaging (MRI) scans did not reveal any abnormal findings (Figure 2A and B).
The patient did not undergo a multidisciplinary consultation.
Heat stroke, multiorgan failure.
She was immediately transferred to our ED by an ambulance. Endotracheal intubation and ventilator-assisted breathing were immediately performed. To decrease body temperature, intravenous cold saline was administered, as well as external cooling by ice packs and water spray. After fluid and norepinephrine administration, her cardiovascular status stabilized.
Based on these findings, the patient was admitted to the Emergency Intensive Care Unit (EICU). Initial treatment in the EICU included intravenous fluid, cooling and antibiotic administration. Consciousness disturbance and a Glasgow Coma Scale level of 3 were reported upon clinical evaluation. Her rectal core temperature was 37.8℃. The laboratory test findings, shown in Table 1, suggested acute hepatic injury, myocardial injury, and rhabdomyolysis, and the patient met the criteria for multiple organ dysfunction syndrome[9,10].
On the first day in the EICU, immediate treatment included intravenous fluid administration, cooling, combination therapy with hemodialysis and hemoperfusion, broad-spectrum antibiotics, tracheal intubation and mechanical ventilation. The TTM protocol for the initial 24 h included monitoring of continuous core temperature with a rectal probe, and cooling measures continued until the target temperature of 34℃ was reached. Therapeutic cooling methods included the use of cooling blankets, cooling caps, ice packs, and bladder irrigation with ice-cold saline. In addition, the patient underwent continuous renal replacement therapy because she showed rhabdomyolysis (hypercreatine kinase emia 18168 IU/L). Simultaneously, continuous renal replacement therapy can effectively lower body temperature. We combined therapy with hemodialysis and hemoperfusion; this involved connecting a perfusion device in series before the dialyzer.
On hospital Day 2, the patient was no longer receiving sedation with midazolam. Despite discontinuation, she remained unconscious for the subsequent 24 h, and re-examination of the head MRI and magnetic resonance angiography showed no obvious lesions (Figure 2C and D). At that point, enteral nutrition was administered with nasal feeding of 300 mL short-peptide enteral nutrition and alanyl glutamine and probiotics were added to promote the recovery of gastrointestinal function.
On hospital Day 3, the patient’s consciousness improved; however, she showed poor responses to verbal stimuli. Re-examination of the head CT showed no cerebral hemorrhage or brain swelling, and the condition of the lungs was acceptable. The patient was extubated and administered high-flow oxygen. She was lying awake but unresponsive, except for head movements and eye blinking. Cranial nerve examination was normal, with normal limb muscle strength and muscle tone but a positive Babinski sign bilaterally. Sensation was unimpaired. Cerebellar examination was grossly abnormal, with severe dysarthria and ataxic gait, requiring two people to assist wirh ambulation. Next, she was scheduled to undergo hyperbaric oxygen therapy once a day.
On hospital Day 8, the elderly patient complained of abdominal pain, and physical examination revealed abdominal distention, abdominal softness, abdominal tenderness, negative shifting dullness, and weak bowel sounds. Whole abdominal CT showed pneumatosis and effusion in the small intestine. She was given a 120 mL glycerin enema (bid), and mosapride (5 mg per tablet, one tablet each time, tid) was administered to promote intestinal peristalsis.
After 15 d, the patient was discharged and was able to complete activities of daily living and walk independently. She was scheduled for outpatient follow-up at one month following the acute event. At the follow-up assessment, the patient's laboratory parameters were normalized, and the patient was clinically stable.
Heat stroke (HS) is a life-threatening condition characterized by hyperthermia and multiple organ failure. It can result from exposure to high environmental temperatures (classic HS), especially for elderly or chronically ill patients, or from strenuous physical activity (exertional HS). While the mechanisms underlying heatstroke remain largely unknown, a study has shown that high temperatures can directly cause cytotoxicity and trigger sepsis-like inflammatory cascades that lead to systemic complications and neurological sequelae in heatstroke[11]. Here, we report a case of an elderly patient with severe heatstroke with multiple organ dysfunction.
To maximize the chances of survival after heatstroke, it is critical to rapidly lower the core body temperature, support the central nervous system as well as the pulmonary, cardiovascular, and renal systems, and effectively manage late or postcooling complications[12-14]. Prompt cooling is the cornerstone of treatment and seems to be the most important prognostic measure[15-17]. The patient’s body temperature dropped to approximately 38℃ 60 min after she was admitted to our ED. Our TTM protocol involves administering cooling measures until the target core temperature of 34℃ is achieved for the subsequent 24 h. Upon completion of this maintenance phase, patients are rewarmed at a rate of 0.25℃/h with adequate sedation and analgesia for seizure prevention and shivering control.
Other mechanisms of heat stroke include heat stress, endotoxemia caused by heat exposure, systemic inflammatory response syndrome, and immune dysfunction. This pathological process is defined as the heat stroke “sepsis-like response”. In this case study, abnormal findings included an elevated white blood cell count of 22.82 × 109/L, a CK level of 4379 IU/L, elevated CK-MB, BUN, PCT, and positive troponin-T. Laboratory investigations showed persistent metabolic acidosis with an increase in CK levels (18168 IU/L). Thus, we administered a combination therapy of hemodialysis and hemoperfusion with a perfusion device connected in series before the dialyzer. Hemodialysis removes small molecular toxins, and the perfusion device removes medium and large molecular toxins, simulating the working principle of the kidney. This approach to therapy can effectively lower body temperature, inhibit the inflammatory cascade reaction, and reduce the concentration of toxic metabolites in serum. On the seventh day following hospital admission, as the patient’s general condition improved, the levels of creatine kinase, aspartate aminotransferase, alanine aminotransferase, lactate dehydrogenase, and white blood cells decreased rapidly.
Heat adversely affects almost all organ systems; the central nervous system is particularly vulnerable, and the cerebellum is most susceptible, followed by the cerebral cortex, spinal cord and brainstem[18]. It was reported that patients with marked cerebellar dysfunction may be radiologically normal with cerebellar atrophy appearing months or years later on CT or MRI scans[19]. In the current case, the duration of exposure to hyperthermia in a 67-year-old woman was not well established, but was characterized by gross cerebellar dysfunction with no acute radiographic changes. After early-stage targeted temperature management and a period of hyperbaric oxygen and nutritional nerve therapy, the patient had normal clinical and laboratory results and was clinically stable at discharge on Day 15, and throughout the remainder of the month following the acute event; this outcome is suggestive of nonprogressive cerebellar damage.
Myocardial damage caused by heatstroke has been well documented in the literature[3]. In our case, laboratory data showed elevated serum CK, CK-MB, and positive troponin-T (Table 1). Electrocardiogram (ECG) results revealed tachycardia (sinus rhythm). ECG did not reveal significant subthemes (ST) -T wave changes, and the echocardiogram showed normal left ventricular function without obvious structural heart disease. After treatment, CK, CK-MB, and troponin-T levels gradually declined. It was reported that ST elevation and positive troponin-T in heatstroke patients may not necessarily be the result of atherosclerotic heart disease[20]. However, since most heatstroke patients do not undergo coronary angiography, it is possible that some such patients complicated with atherosclerotic heart disease are not assessed.
Mild to moderate liver injury is relatively familiar and reversible in heat stroke, and liver function usually returns to normal in 2-16 d, but serious acute lung injury and acute liver failure are rare[21]. Hepatocellular injury may be delayed, as observed in some patients who presented with nonsuspicious liver function tests on admission[22], similar to our case. During heatstroke, when blood is transferred vigorously from core to peripheral circulation, reduction of splanchnic blood flow causes hypoxic/ischemic injuries in the hepatocellular and gastrointestinal system[23]. On hospital Day 8, our patient complained of abdominal pain and abdominal distension, and whole abdominal CT results showed pneumatosis and effusion in the small intestine. Considering the possibility of gastrointestinal function impairment, poor peristalsis, and intestinal obstruction caused by indigestion, the patient was given a 120-mL glycerin enema, and mosapride was administered to promote intestinal peristalsis.
Similar cases have been reported in the literature. Sagisaka et al[24] demonstrated that the prognosis of patients with heatstroke may be unrelated to poor EEG findings, laboratory data, unknown causes of sympathetic hyperactivity, or poor state of consciousness. Prompt cooling is the cornerstone of treatment and seems to be the most important prognostic measure[16], as it has been shown that the major determinant of outcome in heatstroke is the degree and duration of hyperthermia[2]. Sagisaka et al[24] initiated immediate cooling and intensive care after detailed examination. In the present case, although the duration of exposure to hyperthermia in the elderly woman was not established, she underwent rapid cooling. In the EICU, her rectal core temperature was 37.8℃. Therefore, the patient recovered under our comprehensive management.
We recognize the limitations of our study. The primary limitation was whether our TTM process could be improved (maintenance phase longer than 24 h and goal temperature lower than 34℃). This requires more clinical research.
In conclusion, we report our first experience of full recovery of a nonexertional heatstroke case with gross cerebellar dysfunction complicated by multiple organ dysfunction. For the management of heatstroke patients, we propose the adoption of our novel method of inducing TTM (34℃) for 24 h, in combination with hemodialysis and hemoperfusion, and hyperbaric oxygen therapy to prevent neurological sequelae and alleviate multiorgan failure caused by heatstroke. Further clinical research is needed to reduce complications and mortality caused by heatstroke.
We would like to thank our colleagues in Emergency and Critical Care Center for collecting the case data and analysis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Critical care medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Pantelis AG, Greece; Tangsuwanaruk T, Thailand S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Lian P, Braber S, Garssen J, Wichers HJ, Folkerts G, Fink-Gremmels J, Varasteh S. Beyond Heat Stress: Intestinal Integrity Disruption and Mechanism-Based Intervention Strategies. Nutrients. 2020;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 108] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 2. | People’s Liberation Army Professional Committee of Critical Care Medicine. Expert consensus on standardized diagnosis and treatment for heat stroke. Mil Med Res. 2016;3:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (1)] |
| 3. | Yeo TP. Heat stroke: a comprehensive review. AACN Clin Issues. 2004;15:280-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 69] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 4. | Chen X, Li L, Hu J, Zhang C, Pan Y, Tian D, Tang Z. Anti-inflammatory effect of dexmedetomidine combined with hypothermia on acute respiratory distress syndrome in rats. J Surg Res. 2017;216:179-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Feng RY, Chen Q, Yang WJ, Tong XG, Sun ZM, Yan H. Immune Tolerance Therapy: A New Method for Treatment of Traumatic Brain Injury. Chin Med J (Engl). 2018;131:1990-1998. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Sadaka F, Veremakis C. Therapeutic hypothermia for the management of intracranial hypertension in severe traumatic brain injury: a systematic review. Brain Inj. 2012;26:899-908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 66] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 7. | Rimmelé T, Kellum JA. High-volume hemofiltration in the intensive care unit: a blood purification therapy. Anesthesiology. 2012;116:1377-1387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 60] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 8. | Yang L, Li D, Chen S. Hydrogen water reduces NSE, IL-6, and TNF-α levels in hypoxic-ischemic encephalopathy. Open Med (Wars). 2016;11:399-406. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:801-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15803] [Cited by in RCA: 17221] [Article Influence: 1913.4] [Reference Citation Analysis (2)] |
| 10. | Fry DE. Sepsis, systemic inflammatory response, and multiple organ dysfunction: the mystery continues. Am Surg. 2012;78:1-8. [PubMed] |
| 11. | Epstein Y, Roberts WO. The pathopysiology of heat stroke: an integrative view of the final common pathway. Scand J Med Sci Sports. 2011;21:742-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 136] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 12. | Bouchama A, Dehbi M, Chaves-Carballo E. Cooling and hemodynamic management in heatstroke: practical recommendations. Crit Care. 2007;11:R54. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 134] [Cited by in RCA: 135] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 13. | Lee BC, Kim JY, Choi SH, Yoon YH. Use of an external-cooling device for the treatment of heat stroke. Clin Exp Emerg Med. 2014;1:62-64. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Pryor RR, Roth RN, Suyama J, Hostler D. Exertional heat illness: emerging concepts and advances in prehospital care. Prehosp Disaster Med. 2015;30:297-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | Epstein Y, Yanovich R. Heatstroke. N Engl J Med. 2019;380:2449-2459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 345] [Article Influence: 57.5] [Reference Citation Analysis (0)] |
| 16. | Casa DJ, Armstrong LE, Kenny GP, O'Connor FG, Huggins RA. Exertional heat stroke: new concepts regarding cause and care. Curr Sports Med Rep. 2012;11:115-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 149] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 17. | Glazer JL. Management of heatstroke and heat exhaustion. Am Fam Physician. 2005;71:2133-2140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Mahajan S, Schucany WG. Symmetric bilateral caudate, hippocampal, cerebellar, and subcortical white matter MRI abnormalities in an adult patient with heat stroke. Proc (Bayl Univ Med Cent). 2008;21:433-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | Koller WC, Glatt SL, Perlik S, Huckman MS, Fox JH. Cerebellar atrophy demonstrated by computed tomography. Neurology. 1981;31:405-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 35] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Chen WT, Lin CH, Hsieh MH, Huang CY, Yeh JS. Stress-induced cardiomyopathy caused by heat stroke. Ann Emerg Med. 2012;60:63-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 21. | Ward MD, King MA, Gabrial C, Kenefick RW, Leon LR. Biochemical recovery from exertional heat stroke follows a 16-day time course. PLoS One. 2020;15:e0229616. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 22. | Davis BC, Tillman H, Chung RT, Stravitz RT, Reddy R, Fontana RJ, McGuire B, Davern T, Lee WM; Acute Liver Failure Study Group. Heat stroke leading to acute liver injury & failure: A case series from the Acute Liver Failure Study Group. Liver Int. 2017;37:509-513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 54] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 23. | Lambert GP. Role of gastrointestinal permeability in exertional heatstroke. Exerc Sport Sci Rev. 2004;32:185-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 100] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 24. | Sagisaka S, Tamune H, Shimizu K, Kashiyama T. A rare case of full neurological recovery from severe nonexertional heatstroke during a bedrock bath. J Gen Fam Med. 2018;19:136-138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |