Published online Apr 6, 2023. doi: 10.12998/wjcc.v11.i10.2329
Peer-review started: December 26, 2022
First decision: January 5, 2023
Revised: January 11, 2023
Accepted: March 6, 2023
Article in press: March 6, 2023
Published online: April 6, 2023
Processing time: 94 Days and 1.9 Hours
Thoracolithiasis is a rare benign condition that manifests with one or more small nodules in the pleural cavity. In most cases, it is asymptomatic and found incidentally on chest imaging or during thoracic surgery. The thoracolithiasis formation process is rarely documented. Herein, we present a case of a rare, large, curve-shaped thoracolith, the formation of which was documented on serial computed tomography (CT) images.
A 46-year-old male patient who denied any prior systemic disease was evaluated due to intermittent right-sided lateral chest pain lasting for a year. Chest radiography and CT revealed a circumscribed calcified nodule measuring 3.5 mm in the right lower lung lobe. Nodule biopsy revealed fungal infection, which was treated with antifungal medication. After 2 years of follow-up, the patient developed intermittent chest discomfort caused by pleural adhesions, and underwent video-assisted thoracic surgery with pneumolysis. Postoperatively, he developed empyema, which fully resolved with antibiotic therapy. Thereafter, he was followed up at the outpatient clinic and underwent chest CT twice per year. Over time, we observed thickening of the right distal pleura near the lower posterior mediastinum, and several sporadic calcified nodules with gradually increasing intensity, which eventually merged into a single calcified curve-shaped thoracolith measuring approximately 9 cm in length during the 5-year follow-up.
This study documented the formation of a rare thoracolith shape observed for the first time.
Core Tip: Thoracolithiasis, a rare benign condition manifesting with one or more small nodules in the pleural cavity, is usually asymptomatic and discovered incidentally on imaging or during surgery. We present the case of a 46-year-old man who was treated for lung fungal infection and subsequently underwent video-assisted thoracic surgery with pneumolysis due to pleural adhesions. The serial chest computed tomography images obtained during the 5-year follow-up showed right pleural thickening near the lower posterior mediastinum with formation of a large curve-shaped thoracolith from sporadic calcified nodules. Thoracolithiasis formation is rarely observed, and this is the first case of such thoracolith shape.
- Citation: Hsu FC, Huang TW, Pu TW. Formation of a rare curve-shaped thoracolith documented on serial chest computed tomography images: A case report. World J Clin Cases 2023; 11(10): 2329-2335
- URL: https://www.wjgnet.com/2307-8960/full/v11/i10/2329.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i10.2329
Thoracolithiasis, also known as pleurolithiasis, intrathoracic calculosis, or pleural stones, is a rare benign condition manifesting with one or more small nodules in the pleural cavity[1]. In most cases, it is asymptomatic and is usually found incidentally on chest imaging or during thoracic surgery. To the best of our knowledge, there have been no reported cases of symptomatic thoracolithiasis[2]. In addition, its formation process has rarely been documented.
Herein, we report the formation of a curve-shaped thoracolith in a 46-year-old male patient over a 5-year period, documented on serial computed tomography (CT) images.
A 46-year-old male patient presented with a complaint of intermittent right-sided lateral chest pain.
His symptoms started approximately 1 year previously and occurred intermittently. The patient experienced mild dull pain that occurred occasionally with exertion or forced expiration over the right lateral chest, but he was unable to point its exact location. The chest had no skin lesions and expanded symmetrically. The discomfort increased in frequency within a month, which bothered his exercise habit. No history of trauma was mentioned.
The patient denied any prior systemic diseases.
The patient had smoked for a year but had quit for 30 years and denied using alcohol or medications. The family history revealed nothing noteworthy.
The patient had clear breathing sounds with symmetrical chest wall expansion.
A serum test revealed leukocytosis with elevated white blood cell and C-reactive protein levels of 15.73 (103/uL) and 10 mg/dL, respectively, during the course of the emphysema. All lab results were found to be normal during the follow-up interval.
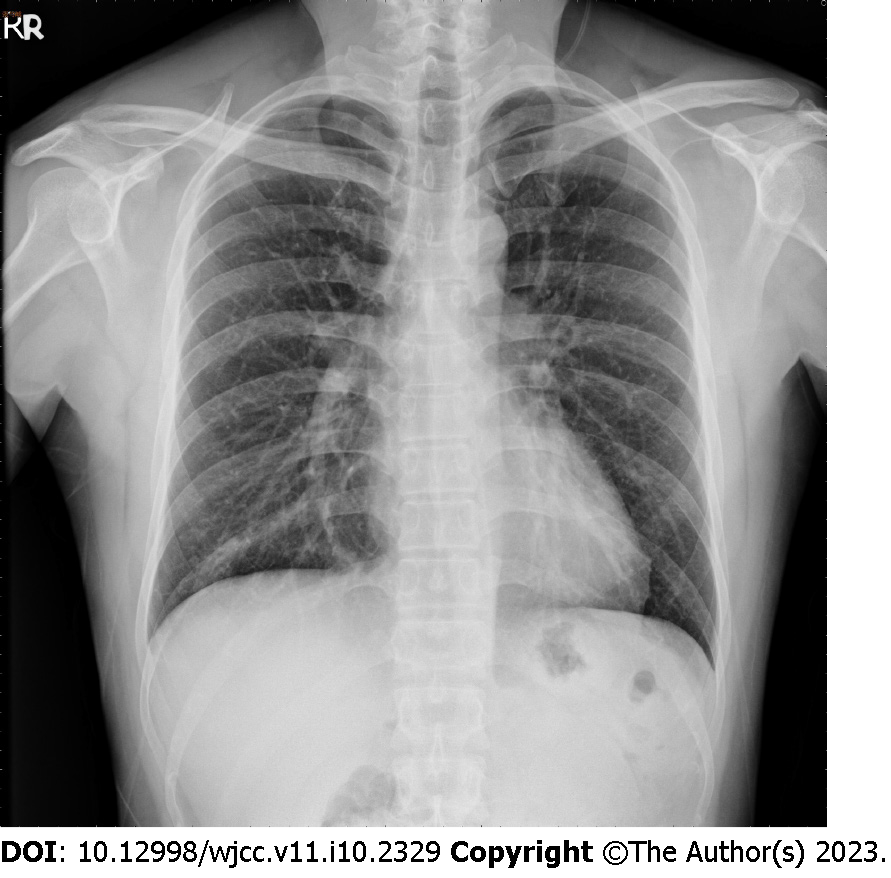
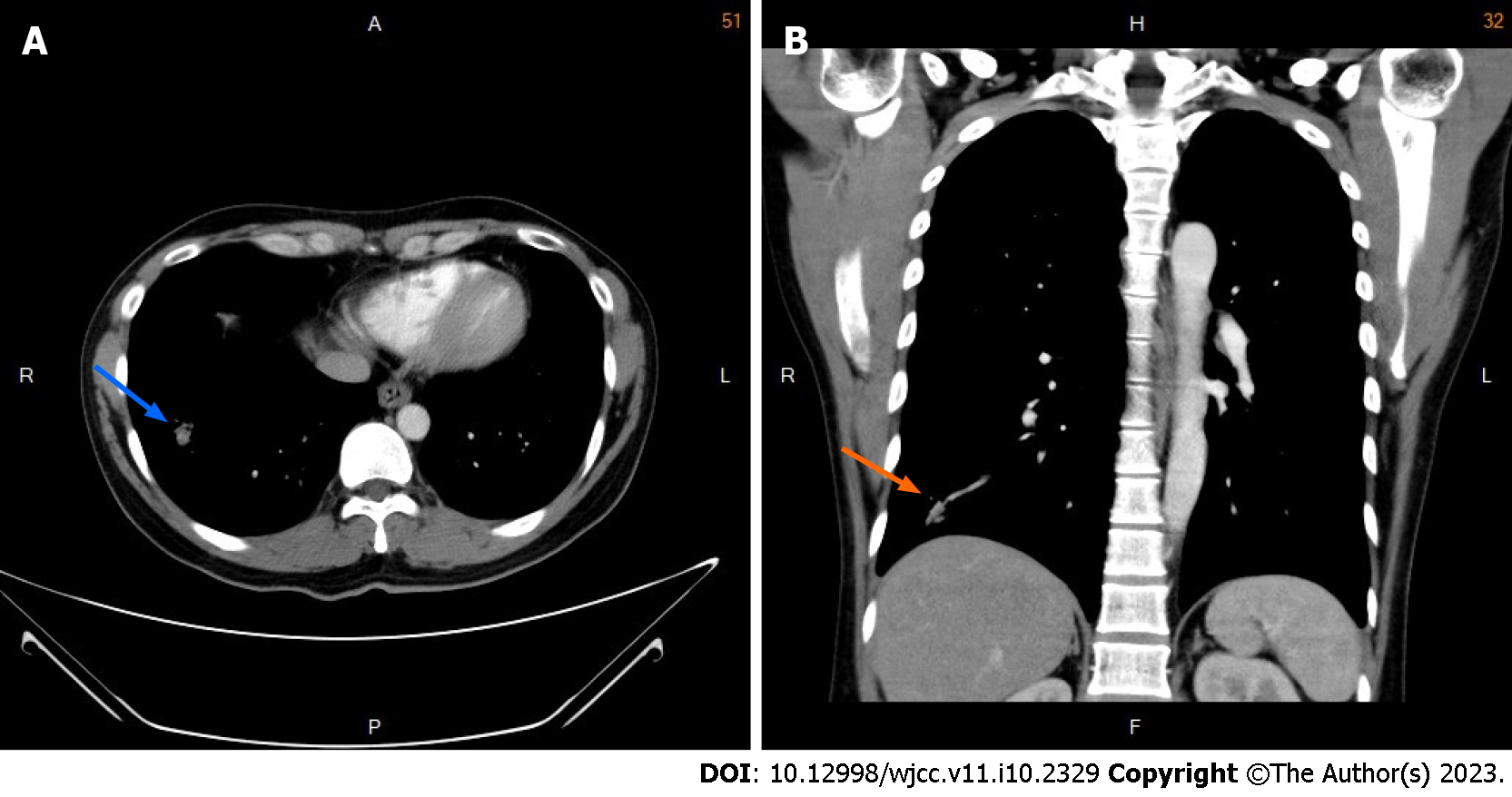
Chest radiography showed increased lung markings with peribronchial wall thickening in the bilateral lower lung fields (Figure 1), while chest CT revealed a circumscribed calcified nodule measuring 3.5 mm in the right lower lung lobe (Figure 2). Since an infection with an unknown pathogen or malignancy was suspected, a CT-guided biopsy was performed. The histopathological examination of the biopsy specimen revealed a fungal infection.
Based on the clinical, imaging, and histopathological findings, the patient was diagnosed with fungal infection of the lungs.
The patient was prescribed an antifungal medicine, fluconazole 50 mg per day for 6 mo.
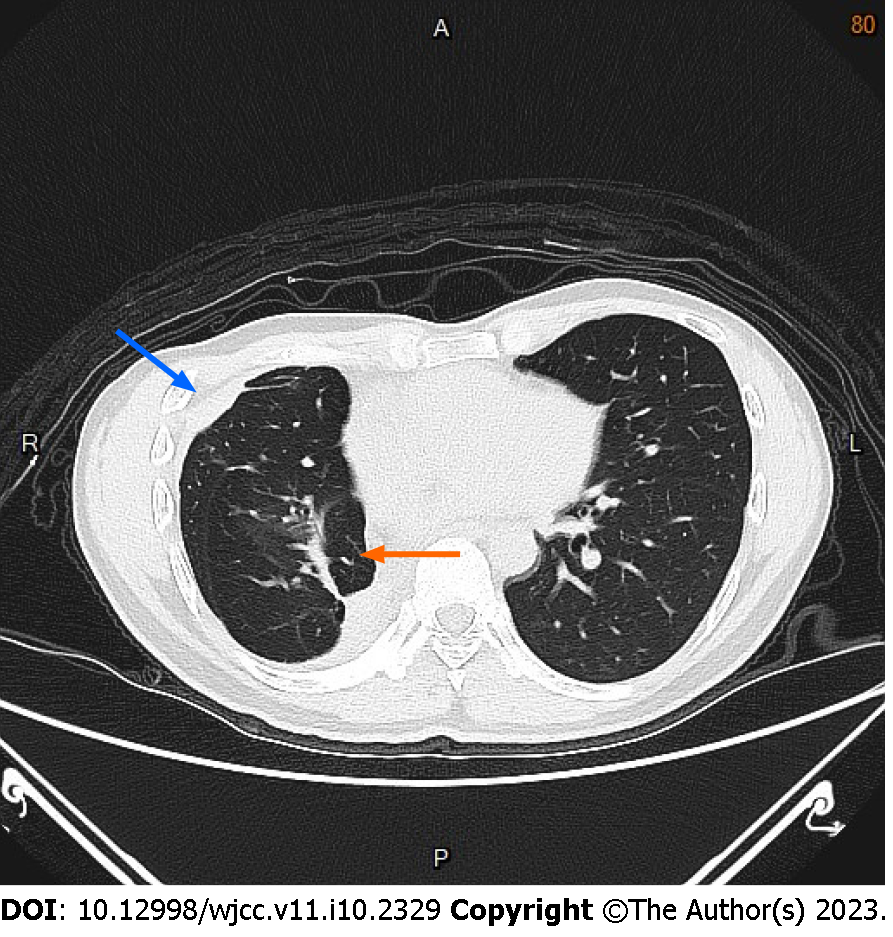
Following the completion of therapy, the patient regularly followed-up at the outpatient clinic every month for the next two years. A follow-up chest CT was performed every 6 mo for 2 years due to complaints of occasional chest discomfort with a mild pricking pain after the last discharge, which revealed a thickening of the right pleura with focal atelectasis in the right middle lung lobe (Figure 3). We suspected that the chest pain was caused by pleural adhesions and performed video-assisted thoracic surgery with pneumolysis. Postoperatively, turbid pleural fluid was discharged from the chest tube inserted into the right chest cavity. The culture test revealed methicillin-resistant Staphylococcus aureus. The patient was administered antibiotic therapy, which resulted in resolution of the empyema. He was discharged from the hospital and followed up at the outpatient clinic.
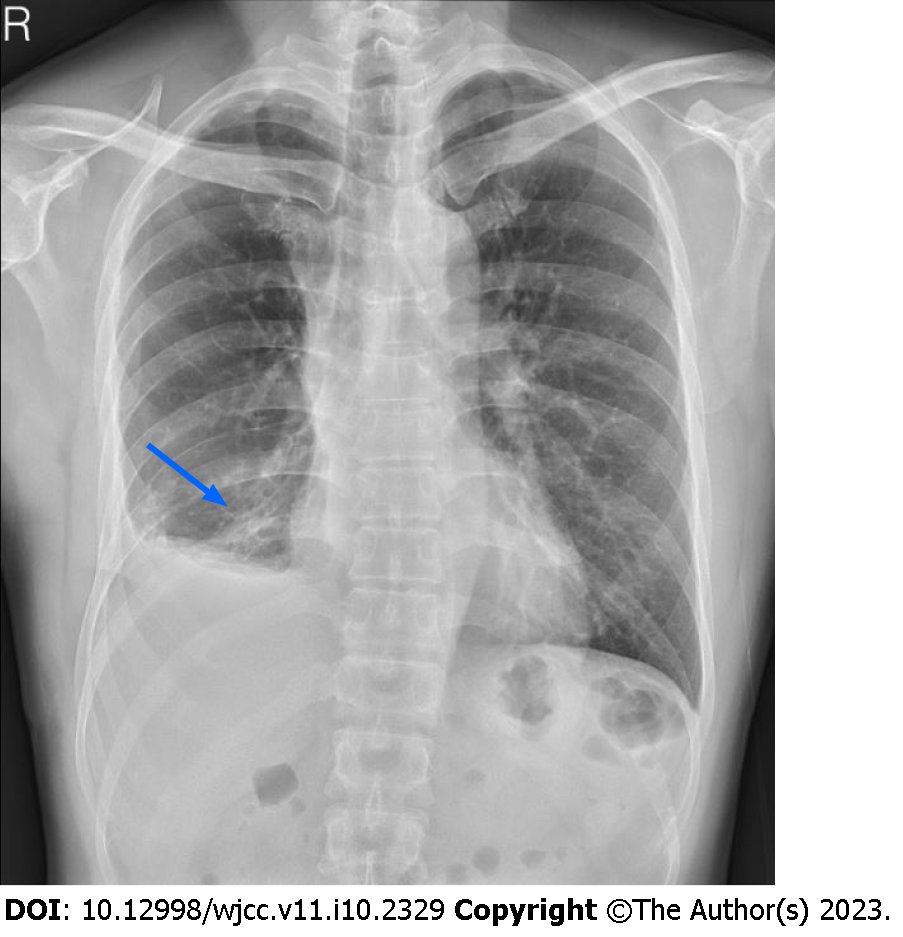
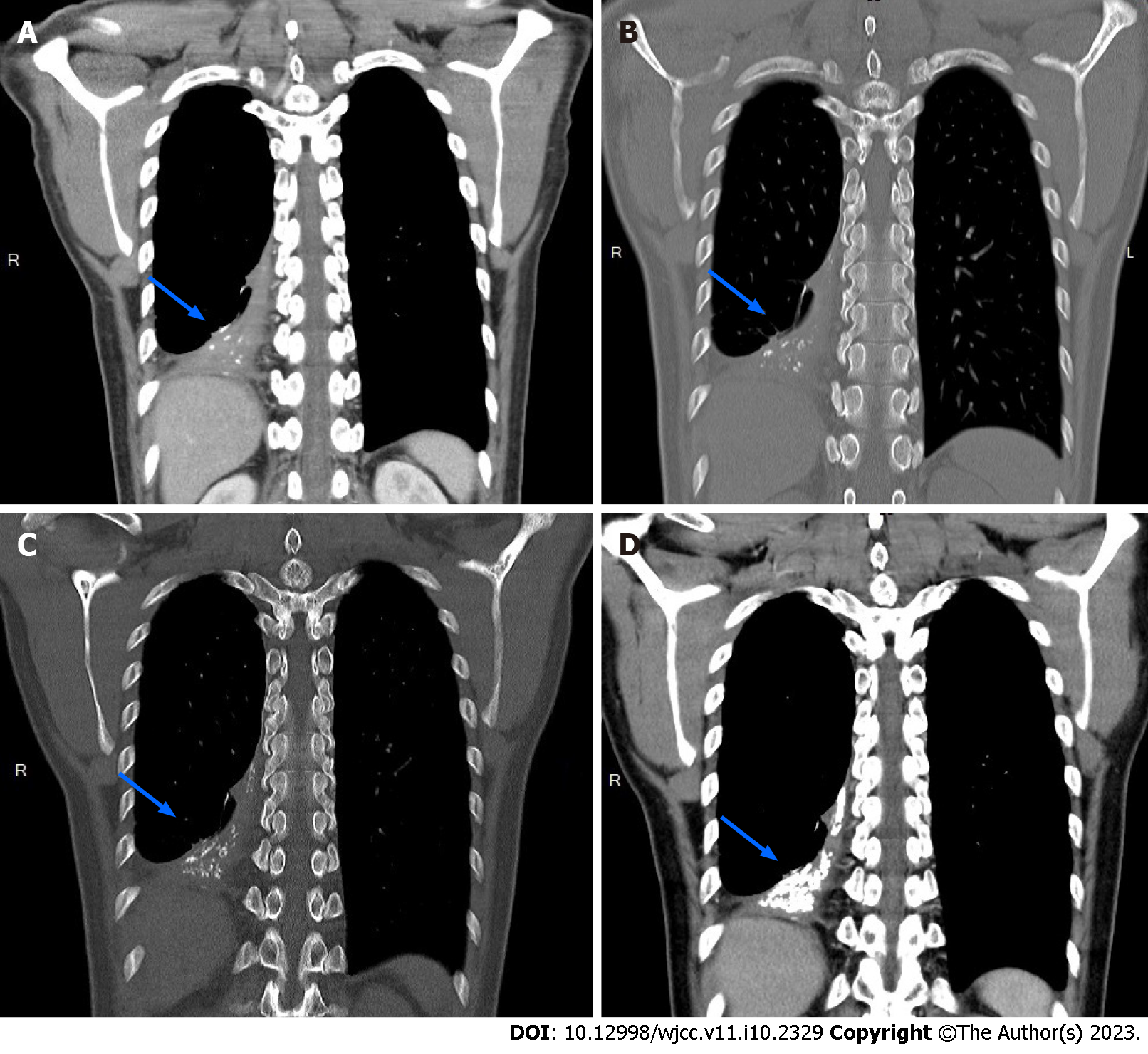
During the follow-up, the patient continued to experience intermittent chest discomfort, and occasionally, a cough, which could be relieved with medicines. The follow-up chest radiographs showed calcified shadows in the right lower lung field (Figure 4). Follow-up chest CT was performed twice per year, with loss to follow-up from 2019 to 2021. In reviewing the serial CT images obtained during the 5-year follow-up, we observed gradual thickening of the right pleura near the lower posterior mediastinum, and several sporadic calcified nodules in the same region with increasing intensity, which became intensive and curved calcified lesions, and eventually formed a large curve-shaped thoracolith measuring approximately 9 cm in length (Figure 5). Despite the progression of thoracolithiasis on CT images, the patient only reported intermittent chest discomfort and denied symptoms such as dyspnea, dysphagia, or hemoptysis. Therefore, no further treatment was prescribed and the patient continued to be followed up on outpatient basis.
Thoracolithiasis is a rare benign condition with a very low incidence in the general population of 0.086%[3]. It was first reported in 1968 by Dias et al[4]. Since then, approximately 70 cases have been reported in the literature, and in many of these the pleural nodules were surgically resected to rule out neoplasia[3,5,6]. No age or sex preference has been reported, although a slight female advantage was observed in a previous report by Kinoshita et al[3]. In most cases, thoracolithiasis is asymptomatic and discovered incidentally on chest imaging or during surgery. Pleural stones are most commonly found in the pendent portion of the pleural cavity, possibly as a result of gravity, particularly on the surface of the diaphragm, along the chest wall near the lower lung fields, next to the left heart border, or near the paravertebral spaces[8].
In a recent major series, all nodules with calcification were reported on CT images[3]. However, although they can be calcified, in some cases, thoracoliths can be indistinguishable from intrapulmonary nodules on CT images[9]. In fact, in one-third of cases, immobile nodules were preoperatively diagnosed as peripheral pulmonary tumors[10]. In some cases, the nodules contained areas of calcification with spotty, central, peripheral, or diffuse patterns[3]. Furthermore, some thoracoliths can be difficult to distinguish from malignant lesions because they enlarge over time[4,11]. Less calcified or immobile thoracoliths are often misdiagnosed, resulting in unnecessary surgical treatment; therefore, accurate diagnosis is important[12].
When thoracolithiasis is suspected, it is difficult to obtain a diagnosis by transthoracic or endobronchial biopsy due to the firm consistency of thoracolith lesions and their loose fixation in the pleural cavity[13]. Based on the unique radiological findings, major surgery is usually not required and not recommended[14]. If they are not calcified or enlarged on follow-up images or the lesion nature is indeterminate, surgical resection should be considered to confirm the diagnosis[4,11,15]. Thoracoscopy, which has the advantage of a minimally invasive procedure that can be performed under local anesthesia, can be used to confirm the diagnosis[16]. The differential diagnosis of thoracoliths includes foreign body granulomas and, rarely, extravasated gallstones after laparoscopic cholecystectomy that have migrated into the pleural cavity[17-19].
Although the etiology of thoracolithiasis is unknown, several hypotheses have been proposed regarding the pathological processes underlying their formation: pericardial fat necrosis and shedding in the pleural cavity, old tuberculosis lesions, or clusters of macrophages phagocytizing dust, which over time form calcified lesions shaped under the impact of long-term breathing movements[10,11,15]. Thoracolithiasis may also develop from inflammation, which facilitates fibrosis[10].
In previously reported cases, thoracoliths ranged in size from 5 to 15 mm (mean size, 8 mm)[3], and in most cases, presented as multiple small ovoid nodules located in the left pleura[3,4,11,20]. In our case, the thoracolith measured approximately 9 cm in length. In addition, this case demonstrated the 5-year formation process of the large curve-shaped thoracolith. Multiple sporadic calcified nodules accumulated in the pleura over time, abutting each other, and eventually assembled into a large thoracolith. The sporadic calcified nodules increased in size on follow-up CT images and were seen in the pendant portion of the pleural cavity, possibly secondary to gravity. Based on their growth pattern and imaging characteristics, the lesions were not consistent with tumor lesions. In our patient, thoracolithiasis may have resulted from pericardial or right mediastinal fat necrosis, reflecting the prior episodes of fungal infection and empyema. The exact etiology of thoracolithiasis is unknown; we hypothesize that a previous pleural infection, fungal or bacterial, could facilitate inflammation and fibrosis, which would further lead to the formation of calcified masses.
The present case provided a rare opportunity to observe the formation process of a large curve-shaped thoracolith. This thoracolith shape was observed for the first time as opposed to the commonly encountered multiple small ovoid thoracoliths. Pericardial or right mediastinal fat necrosis may have resulted in its formation.
The authors would like to express their gratitude to Fu-Chieh Hsu, MD, for his contributions in drafting the article as well as the conception and design of the study; Ta-Wei Pu, MD, for his role in critically reviewing the manuscript for keu intellectual content; and Tsai-Wang Huang, MD, PhD, for overseeing the study and endorsing the data.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Jian X, China; Liu S, China; Zhao JW, China S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Peungjesada S, Gupta P, Mottershaw AM. Thoracolithiasis: a case report. Clin Imaging. 2012;36:228-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Kang N, Choi Y, Im Y, Choe J, Kim J, Han J, Kim TJ, Kim H. A rare case of numerous thoracolithiasis with chest discomfort. Respir Med Case Rep. 2018;25:264-266. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 3. | Kinoshita F, Saida Y, Okajima Y, Honda S, Sato T, Hayashibe A, Hiramatsu S. Thoracolithiasis: 11 cases with a calcified intrapleural loose body. J Thorac Imaging. 2010;25:64-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Dias AR, Zerbini EJ, Curi N. Pleural stone. A case report. J Thorac Cardiovasc Surg. 1968;56:120-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Tsuchiya T, Ashizawa K, Tagawa T, Tsutsui S, Yamasaki N, Miyazaki T, Hayashi T, Nagayasu T. A case of migrated thoracolithiasis. J Thorac Imaging. 2009;24:325-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Strzelczyk J, Holloway BJ, Pernicano PG, Kelly AM. Rolling stones in the pleural space: thoracoliths on CT, and a review of the literature. Clin Radiol. 2009;64:100-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Kim Y, Shim SS, Chun EM, Won TH, Park S. A Pleural Loose Body Mimicking a Pleural Tumor: A Case Report. Korean J Radiol. 2015;16:1163-1165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Hamanaka R, Masuda R, Iwazaki M. A Case of Thoracolithiasis Extracted with a Thoracoscope. Tokai J Exp Clin Med. 2021;46:162-165. [PubMed] |
| 9. | Cornellas L, Soler-Perromat JC, Vollmer I. Thoracolithiasis: A Rare Cause of Migratory Thoracic Mass. Arch Bronconeumol (Engl Ed). 2019;55:534. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Iwasaki T, Nakagawa K, Katsura H, Ohse N, Nagano T, Kawahara K. Surgically removed thoracolithiasis: report of two cases. Ann Thorac Cardiovasc Surg. 2006;12:279-282. [PubMed] |
| 11. | Kosaka S, Kondo N, Sakaguchi H, Kitano T, Harada T, Nakayama K. Thoracolithiasis. Jpn J Thorac Cardiovasc Surg. 2000;48:318-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Gayer G. Thoracolithiasis-Computed Tomography Findings of Intrapleural Loose Bodies. Semin Ultrasound CT MR. 2017;38:634-640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Komatsu T, Sowa T, Fujinaga T. A case of thoracolithiasis diagnosed thoracoscopically. Int J Surg Case Rep. 2012;3:415-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Motamedi P, Palacio D, Campion J. Mobile Thoracolithiasis. Am J Med. 2018;131:e251-e252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 15. | Hochhegger B, Camargo SM, Nascimento D, Zanetti G, Marchiori E. Thoracolithiasis: A Rare Cause of Multiple Nodules. Am J Respir Crit Care Med. 2018;197:1212-1213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Nakagawa H, Ohuchi M, Fujita T, Ozaki Y, Nakano Y, Inoue S. Thoracolithiasis diagnosed by thoracoscopy under local anesthesia. Respirol Case Rep. 2015;3:102-104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Oestmann JW, Bridenbaugh S, Eggeling I. Gallstone migration into the pleural space. Am J Gastroenterol. 2000;95:836-837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 18. | Brazinsky SA, Colt HG. Thoracoscopic diagnosis of pleurolithiasis after laparoscopic cholecystectomy. Chest. 1993;104:1273-1274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 19. | Quail JF, Soballe PW, Gramins DL. Thoracic gallstones: a delayed complication of laparoscopic cholecystectomy. Surg Infect (Larchmt). 2014;15:69-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Tanaka D, Niwatsukino H, Fujiyoshi F, Nakajo M. Thoracolithiasis--a mobile calcified nodule in the intrathoracic space: radiographic, CT, and MRI findings. Radiat Med. 2002;20:131-133. [PubMed] |