Published online Apr 6, 2023. doi: 10.12998/wjcc.v11.i10.2321
Peer-review started: December 15, 2022
First decision: January 20, 2023
Revised: February 8, 2023
Accepted: March 6, 2023
Article in press: March 6, 2023
Published online: April 6, 2023
Processing time: 104 Days and 21.1 Hours
Periprosthetic joint infection (PJI) and periprosthetic fracture (PPF) are among the most serious complications following total knee arthroplasty. Herein, we present one patient with these two complications with details on the characteristics, treatment strategy, and outcome.
A 69-year-old female patient who suffered from PJI and PPF following total knee arthroplasty was treated by a two-stage revision surgery. After thorough foreign material removal and debridement, we used a plate that was covered with antibiotic-loaded bone cement to link with a hand-made cement spacer to occupy the joint space and fix the fracture. Although the infection was cured, the fracture did not heal and caused bone defect due to the long interval between debridement and revision. In the revision surgery, a cemented stem and cortical allogenic splints were used to reconstruct the fracture and bone defect. At the final follow-up 27 mo after revision, the patient was satisfied with postoperative knee functions with satisfactory range of motion (104º) and Hospital for Special Surgery knee score (82 points). The radiographs showed no loosening of the prosthesis and that the bone grafts healed well with the femur.
Our two-stage revision surgery has proved to be successful and may be considered in other patients with PJI and PPF.
Core Tip: Periprosthetic joint infection (PJI) and periprosthetic fracture (PPF) are among the most serious complications of knee arthroplasty. A two-stage revision surgery should be progressively performed in the treatment of PJI and coexistent PPF with bone loss. In the first-stage operation, a T-shaped cement spacer made from a rectangular vancomycin laden cement block and a cement coated plate was used after debridement. In the second-stage operation, the combination of cemented prosthesis and freeze-dried cortical allogenic splints were used for knee revision and fixation of PPF. Our approach offers an option for successful treatment of PJI and PPF.
- Citation: Hao LJ, Wen PF, Zhang YM, Song W, Chen J, Ma T. Treatment of periprosthetic knee infection and coexistent periprosthetic fracture: A case report and literature review. World J Clin Cases 2023; 11(10): 2321-2328
- URL: https://www.wjgnet.com/2307-8960/full/v11/i10/2321.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i10.2321
For patients with posttraumatic osteoarthritis, the presence of periarticular hardware complicates total knee arthroplasty (TKA) and increases the incidence of periprosthetic joint infection (PJI)[1-3]. Meanwhile, PJI may significantly prolong the treatment period, resulting in longer hospitalization, more complications, higher medical costs, and lower quality of life[4-6]. Periprosthetic fracture (PPF) is also one of the most serious complications after TKA and usually results in joint dysfunctions or even disabilities[7]. Patients may suffer from both PJI and PPF simultaneously, which makes a therapeutic approach difficult to formulate because of different or contradicting treatment concepts. Once an infection occurs, all foreign materials including prosthesis and internal fixation need to be removed; however, PPF needs to be stabilized by internal fixation. Therefore, the most crucial question is how to deal with both fracture fixation and infection treatment appropriately.
In this case report, we describe a patient with concomitant PJI and PPF who was successfully treated and followed for 2 years.
A 69-year-old Chinese woman was admitted to our joint clinic with a complaint of right thigh pain and swelling for 3 d.
Symptoms started 3 d before presentation with severe thigh pain and swelling (July 2019).
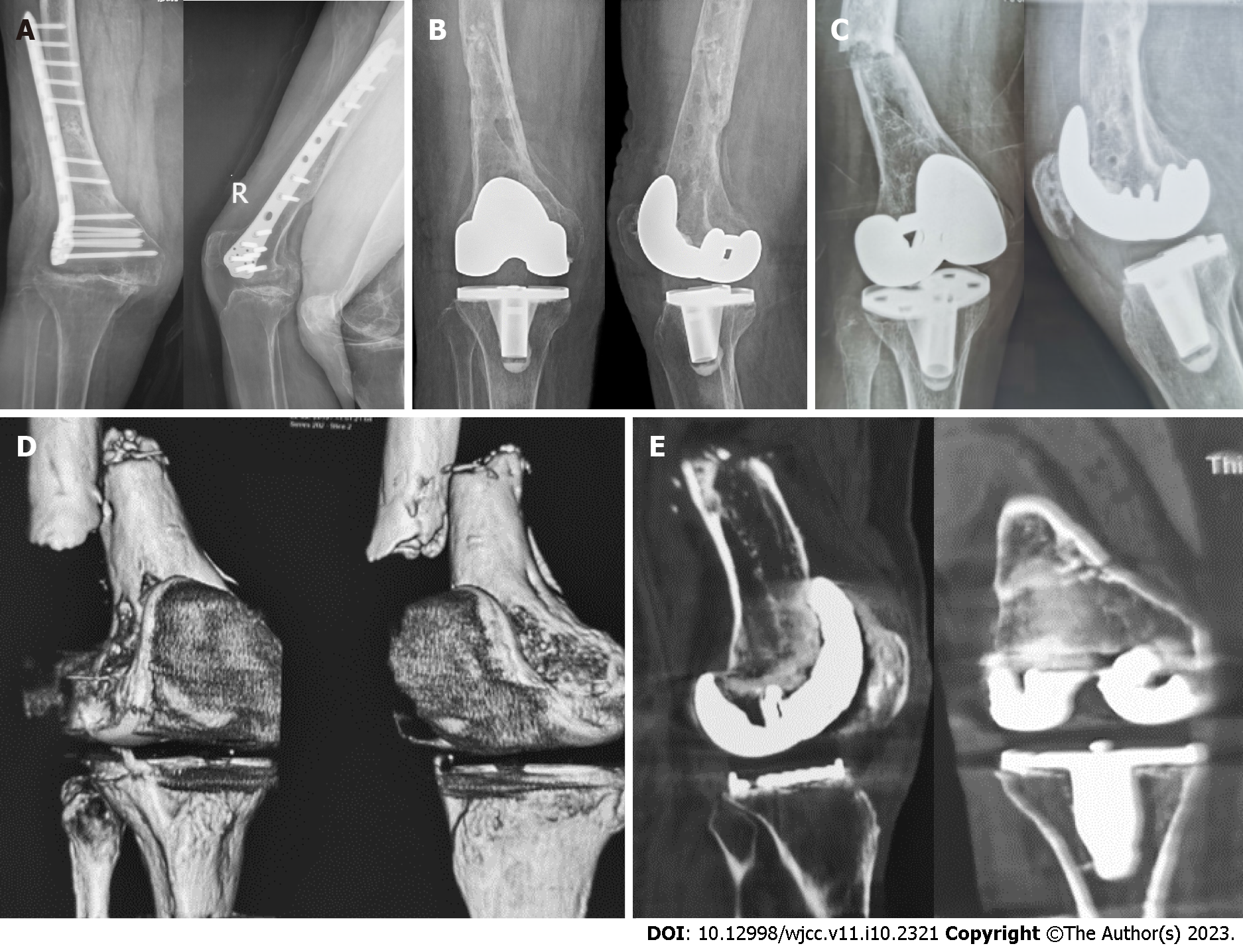
The patient fell and fractured her right distal femur in November 2017. She underwent an open reduction and internal fixation (ORIF) at a local hospital. In December 2018, the patient was diagnosed with posttraumatic osteoarthritis of the right knee, for which the removal of original internal fixation implants and TKA were simultaneously performed (Figure 1A and B). In April 2019, the patient suffered PJI of the right knee with a sinus formation and was treated with antibiotic suppression; however, the infection did not improve.
The patient had no personal or family history.
The right thigh was swollen and deformed. The right knee had a sinus tract and limited range of motion.
The serum erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), white blood cell (WBC) count, and neutrophil percentage were elevated (97 mm/h, 126.19 mg/L, 12.18 × 109/L, and 75.2%, respectively). The synovial fluid WBC count and synovial fluid polymorphonuclear neutrophil percentage were 12045/uL and 94%, respectively. Methicillin-resistant Staphylococcus aureus (MRSA) was detected on the synovial fluid culture.
The X-ray and computed tomography (CT) scan revealed a fracture of the right femur and loosening of the knee prosthesis (Figure 1C-E).
The patient was diagnosed with PJI and PPF (Rorabeck and Taylor[8] type II) of the right knee.
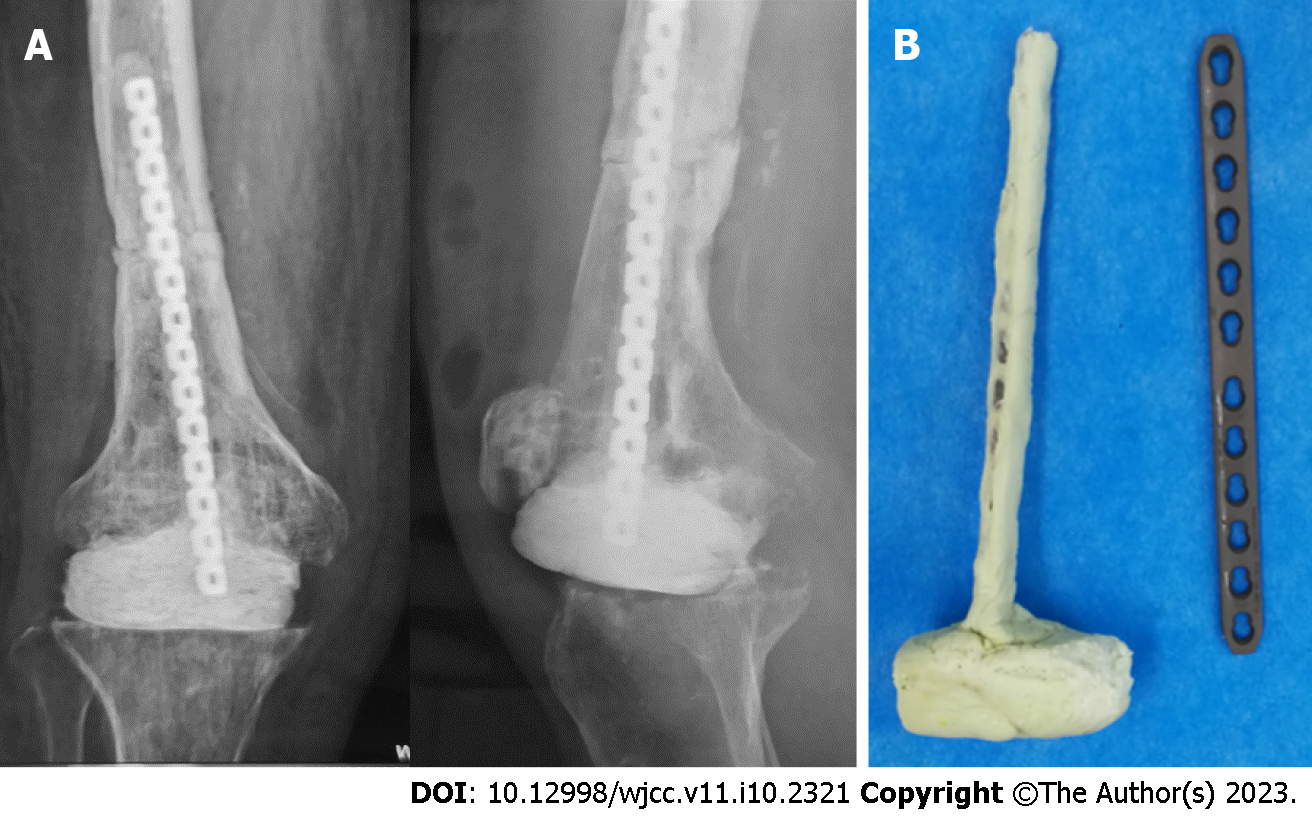
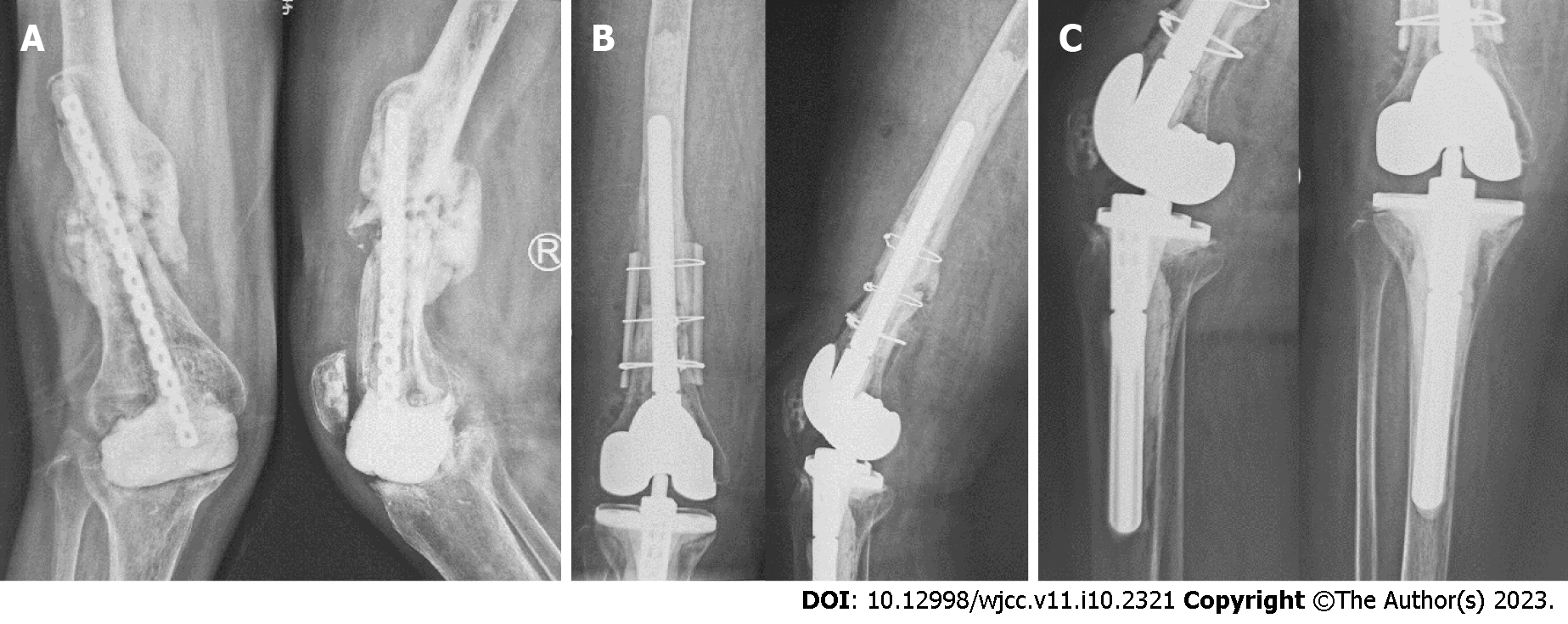
A two-stage revision surgery was planned with an interval of about 3 mo. The first-stage operation (Figure 2) was performed in two steps. The first step was resection of the prosthesis and debridement. The second step was the placement of an antibiotic cement spacer and fixation of PPF. We used a rectangular vancomycin laden cement (Palacos R+G, Heraeus Medical GmbH) block linking with a cement-coated plate (Limited contact dynamic compression plate, Synthes GmbH) to make a T-shaped spacer. A longer plate was not selected to avoid the spread of infection. Five different specimens around the prosthesis were sent for culture, and the detected pathogen was still MRSA. An infectious disease specialist prescribed a regimen of anti-MRSA drugs, consisting of intravenous drip of vancomycin and oral rifampicin at dosages of 1000 and 600 mg/d, respectively. After 2 wk, the regimen was changed to 300 mg/d of oral rifampicin and 500 mg/d of oral ciprofloxacin for 6 wk. After the operation, the patient was instructed to walk without weight-bearing. However, the patient was lost to follow-up and did not undergo the second-stage operation (Figure 3) in October 2019 as planned. In May 2020, she revisited our outpatient clinic. By this time, she had suffered severe functional impairment with a Hospital for Special Surgery (HSS) knee score of only 23 points. She was admitted into the hospital. After infection was ruled out through a series of blood tests and synovial fluid culture, the second-stage operation consisting of ORIF of PPF and revision TKA was performed in three steps. First, we performed debridement and removed any foreign material and sequestrum. Second, the fixation of periprosthetic femoral fracture was done. Two pieces of freeze-dried cortical allogenic splint (Shanxi Aorui Biomaterials Co. LTD) of approximately 10 centimeter in length were used for auxiliary fixation of the femur. Then, cables (Synthes Cable System) and wires were used to bundle bone splits, and autologous bone graft was applied to the bone defect. Finally, knee revision prosthesis (NexGen LCCK, Zimmer Inc.) was installed. A 150-millimeter-long stem with a diameter of 14 millimeters was used on the femoral side. A 100-millimeter-long stem with a diameter of 14 millimeters was used on the tibial side. A 5-millimeter-thick metal pad was added to both medial and lateral sides of the distal femoral prosthesis, and a 10-millimeter-thick metal pad was added to the posterior condyle of the femoral prosthesis. X-rays were taken at 3 d postoperatively. Postoperative rehabilitation exercise consisted of partial weight bearing of the right lower limb for 6 wk. The antibiotic therapy was continued according to the instructions of the infectious disease specialist. A timeline of the clinical course and management is provided in Table 1.
| Date | Diagnosis | Treatment |
| November 17 | Right femoral fracture | ORIF |
| December 18 | Posttraumatic osteoarthritis of right knee | Removal of internal fixation and TKA |
| April 19 | PJI | Antibiotic suppression |
| July 19 | PJI and PPF | Resection of prosthesis with placement of antibiotic spacer and fixation of fracture |
| May 20 | Post-operation of prosthesis removal | Revision knee arthroplasty and fixation of right PPF |
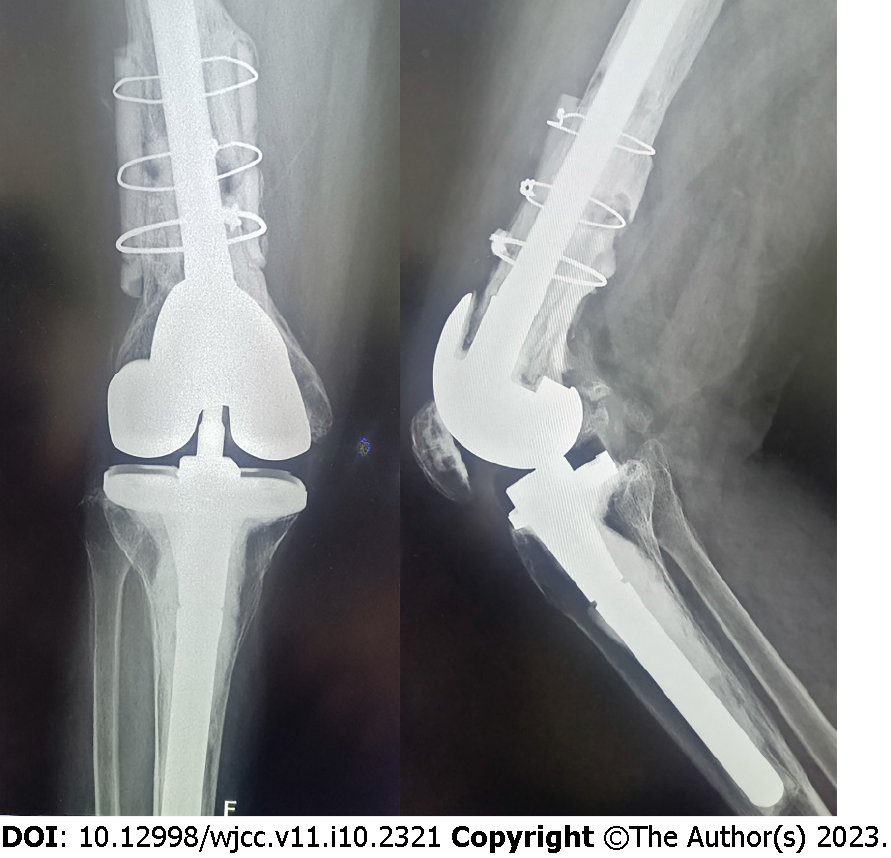
The patient was followed periodically (6, 12, and 24 wk and annually thereafter) after revision TKA. The wound healed well without redness or swelling. The serum CRP and ESR decreased continuously and returned to normal at 3 mo post-revision. The HSS score was 59, 69, and 85 points at 6, 12, and 24 wk after revision, respectively. At the final follow-up 27 mo after revision (Figure 4), the range of motion was 104º, the HSS score was 82 points, and the Western Ontario MacMaster Universities Osteoarthritis Index score was 36 points. The patient was satisfied with the course of treatment and postoperative knee function. There was no sign of infection recurrence or loosening of the prosthesis.
PJI and PPF are among the most serious complications following TKA and usually raise concern for both patients and surgeons[9-11]. The incidence of PJI after primary TKA is 0.7%-2%[12,13], while that after revision is 5.6%-35%[14-16]. Meanwhile, the incidence of PPF ranges from 0.3% to 2.5% after primary TKA and 1.6% to 38% after revision TKA[17-19]. Each complication needs precise assessment and specific care to prevent further serious issues. If PJI is simultaneous with PPF for one patient, it is going to be a very tricky situation. There is no optimal management strategy regarding this issue due to lack of standards and controversy over treatment effectiveness. The treatment of this patient for infection and fracture after TKA with periarticular internal fixators offers possible strategies for this condition.
The incidence of PJI in patients with a history of ORIF who underwent TKA is similar to that after revision[20]. Suzuki et al[21] reported that previous ORIF and remnants of previous internal fixation materials showed significant correlation with postoperative infections. A prospective matched cohort study conducted by Lizaur-Utrilla et al[22] found that the incidence of surgical site infection was higher in the posttraumatic group and recommended removal of hardware prior to TKA. In contrast, Klatte et al[23] found that the risk of developing periprosthetic knee infection was not significantly increased with pre-existing orthopaedic implants. In general, more and more studies identified previous fracture history and remnants of pre-existing fixation-devices as major risk factors for PJI after TKA[21,22,24] and suggested that complete removal of the fixators 4 to 6 mo before TKA could reduce the incidence of PJI[22,25]. For clinical implication, surgeons should be conscious of the infection potential when performing knee arthroplasty on patients with these risk factors.
From our point of view, fixing the fracture is the main difficulty for patients with both PJI and PPF and also is an important factor to ensure fracture union and prevent postoperative infection. In this study, the combination of antibiotic-laden cement spacer and cement-coated plate, which was used as an intramedullary nail, provided a solution. Bonacker et al[26] presented a two-stage surgical strategy conducted in a 69-year-old male patient with a periprosthetic tibia fracture, infectious nonunion, and loosening of the TKA due to ascending infection. After removing all implants, a deep debridement was performed, and a tibial nail connected with a hand-formed bone cement knee spacer including antibiotics and two additional antibiotic-impregnated chains was implanted. In the revision surgery, the tibial fracture site was stabilized with a long uncemented stem. Sanz-Ruiz et al[27] presented a biarticular cement spacer, made from a cephalomedullary nail, to treat infected hip arthroplasty with massive bone loss. They covered the nail with antibiotic-laden cement and obtained satisfactory results of infection control and functional retention. In this case, a cement-coated plate which can slowly release antibiotics, preventing bacterial adhesion and proliferation and biofilm formation, was also used to substitute a metal-exposed plate as intramedullary nail for fracture immobilization. In addition, a cemented femoral stem was used instead of cementless one during the revision, because a fully long cementless stem could not be implanted due to the anterior femoral curvature and large defect of the previous fracture. Meanwhile, the cemented one could stabilize the proximal and distal parts of femoral fracture. What needs illustration is that cement smeared at the fracture was strictly prohibited and measure of heat control was indispensable when the cement generate heat during solidification to avoid affecting the union of fracture.
Müller et al[28] reported a two-stage revision for the treatment of 8 patients with PPF and infection. The fractures were fixed by three strategies: 2 patients by plate, 3 by intramedullary rod/pin, and 3 by plate and rod/pin. At the final follow-up, one infection recurred, and three individuals developed nonunion of fracture, getting a high nonunion rate. A systematic review conducted by Ebraheim et al[29] concluded that the complication rate of PPF after TKA separately treated with intramedullary nail/rod or locking plate is as high as 53% and 35%, respectively, and the most common complication is non/delayed union. Therefore, to ensure fracture healing, it is necessary not only to cure infection, but also to obtain the fixation stability of the fracture. In such revision surgery, extramedullary auxiliary fixation is often required if intramedullary stem cannot guarantee the fixation stability of fracture. Except for plates, bone splints are commonly used. Carta et al[30] reported that cortical allogenic splints should be considered the use instead of metal plates for the treatment of periprosthetic femoral fracture, which usually has bone loss and/or a potential mechanical instability. In a cadaveric study, Peters et al[31] concluded that allograft cortical splints offer biomechanical advantages as an alternative to metal plates for the fixation of femur fracture below a well-fixed femoral component. In this study, we used titanium cable and wires to fix the two splints which were placed on the medial and lateral aspects of the femur. Then, bone graft was also performed. Comparing with using single metal plates, we could get potential benefits from the use of cortical allogenic splints, which can increase bone quantity and quality, decrease stress shielding, stabilize the entirety, so as to reduce fracture nonunion occurrence and other complications, and improve the patients’ quality of life by accelerating function recovery. However, the potential disadvantages of the customized transplant, such as transmission of infectious diseases, risks of infections, longer surgical time, and more complex surgical procedures, must be taken into consideration.
Another aspect that we have learned from this case is the importance of strengthening patients’ management and guidance to avoid similar incidents. In the future, we should establish a more diversified and convenient follow-up system, strengthen the patient education on the post-discharge process, urge patients who need special care to attend follow-up visits regularly, and involve family members in the patient care.
The main limitation of this study is that it is a report of a single case, which is due to the low incidence of the coexistence of PJI and PPF.
PJI, PPF, and nonunion with bone defect individually pose a challenge in orthopedics and trauma surgery. We present a highly complex case on account of the consecutive occurrence of these complications. The lack of standards resulted in the requirement of an individualized strategy under this circumstance, and the key to success was synergistic execution of simultaneous fracture stabilization and infection eradication. Our approach offers an option for successful treatment, upon which future strategies can be developed. Highly specialized interdisciplinary centers are needed for desirable therapeutic outcomes.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Oommen AT, India; Primadhi RA, Indonesia S-Editor: Liu JH L-Editor: Wang TQ P-Editor: Liu JH
| 1. | Best MJ, Amin RM, Raad M, Kreulen RT, Musharbash F, Valaik D, Wilckens JH. Total Knee Arthroplasty after Anterior Cruciate Ligament Reconstruction. J Knee Surg. 2022;35:844-848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Farfalli LA, Farfalli GL, Aponte-Tinao LA. Complications in total knee arthroplasty after high tibial osteotomy. Orthopedics. 2012;35:e464-e468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | El-Galaly A, Haldrup S, Pedersen AB, Kappel A, Jensen MU, Nielsen PT. Increased risk of early and medium-term revision after post-fracture total knee arthroplasty. Acta Orthop. 2017;88:263-268. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 4. | Parvizi J, Zmistowski B, Berbari EF, Bauer TW, Springer BD, Della Valle CJ, Garvin KL, Mont MA, Wongworawat MD, Zalavras CG. New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res. 2011;469:2992-2994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1212] [Cited by in RCA: 1453] [Article Influence: 103.8] [Reference Citation Analysis (1)] |
| 5. | Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J. Economic burden of periprosthetic joint infection in the United States. J Arthroplasty. 2012;27:61-5.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1101] [Cited by in RCA: 1225] [Article Influence: 94.2] [Reference Citation Analysis (0)] |
| 6. | Zingg M, Kheir MM, Ziemba-Davis M, Meneghini RM. Reduced Infection Rate After Aseptic Revision Total Knee Arthroplasty With Extended Oral Antibiotic Protocol. J Arthroplasty. 2022;37:905-909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 28] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 7. | Kurtz SM, Lau EC, Ong KL, Adler EM, Kolisek FR, Manley MT. Which Clinical and Patient Factors Influence the National Economic Burden of Hospital Readmissions After Total Joint Arthroplasty? Clin Orthop Relat Res. 2017;475:2926-2937. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 176] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 8. | Rorabeck CH, Taylor JW. Classification of periprosthetic fractures complicating total knee arthroplasty. Orthop Clin North Am. 1999;30:209-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 195] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 9. | Postler A, Lützner C, Beyer F, Tille E, Lützner J. Analysis of Total Knee Arthroplasty revision causes. BMC Musculoskelet Disord. 2018;19:55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 130] [Cited by in RCA: 238] [Article Influence: 34.0] [Reference Citation Analysis (0)] |
| 10. | Sukhonthamarn K, Strony JT, Patel UJ, Brown SA, Nazarian DG, Parvizi J, Klein GR. Distal Femoral Replacement and Periprosthetic Joint Infection After Non-Oncological Reconstruction: A Retrospective Analysis. J Arthroplasty. 2021;36:3959-3965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 11. | Meyer JA, Zhu M, Cavadino A, Coleman B, Munro JT, Young SW. Infection and periprosthetic fracture are the leading causes of failure after aseptic revision total knee arthroplasty. Arch Orthop Trauma Surg. 2021;141:1373-1383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 12. | Pulido L, Ghanem E, Joshi A, Purtill JJ, Parvizi J. Periprosthetic joint infection: the incidence, timing, and predisposing factors. Clin Orthop Relat Res. 2008;466:1710-1715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 903] [Cited by in RCA: 1000] [Article Influence: 58.8] [Reference Citation Analysis (0)] |
| 13. | Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991-2010. JAMA. 2012;308:1227-1236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 674] [Cited by in RCA: 734] [Article Influence: 56.5] [Reference Citation Analysis (0)] |
| 14. | Schroer WC, Berend KR, Lombardi AV, Barnes CL, Bolognesi MP, Berend ME, Ritter MA, Nunley RM. Why are total knees failing today? J Arthroplasty. 2013;28:116-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 309] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 15. | Srivastava K, Bozic KJ, Silverton C, Nelson AJ, Makhni EC, Davis JJ. Reconsidering Strategies for Managing Chronic Periprosthetic Joint Infection in Total Knee Arthroplasty: Using Decision Analytics to Find the Optimal Strategy Between One-Stage and Two-Stage Total Knee Revision. J Bone Joint Surg Am. 2019;101:14-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 16. | Di Benedetto P, Di Benedetto ED, Salviato D, Beltrame A, Gissoni R, Cainero V, Causero A. Acute periprosthetic knee infection: is there still a role for DAIR? Acta Biomed. 2017;88:84-91. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 17. | Mortazavi SM, Kurd MF, Bender B, Post Z, Parvizi J, Purtill JJ. Distal femoral arthroplasty for the treatment of periprosthetic fractures after total knee arthroplasty. J Arthroplasty. 2010;25:775-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 84] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 18. | Agarwal S, Sharma RK, Jain JK. Periprosthetic fractures after total knee arthroplasty. J Orthop Surg (Hong Kong). 2014;22:24-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 19. | Dyrhovden GS, Lygre SHL, Badawy M, Gøthesen Ø, Furnes O. Have the Causes of Revision for Total and Unicompartmental Knee Arthroplasties Changed During the Past Two Decades? Clin Orthop Relat Res. 2017;475:1874-1886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 99] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 20. | Schwarz EM, Parvizi J, Gehrke T, Aiyer A, Battenberg A, Brown SA, Callaghan JJ, Citak M, Egol K, Garrigues GE, Ghert M, Goswami K, Green A, Hammound S, Kates SL, McLaren AC, Mont MA, Namdari S, Obremskey WT, O'Toole R, Raikin S, Restrepo C, Ricciardi B, Saeed K, Sanchez-Sotelo J, Shohat N, Tan T, Thirukumaran CP, Winters B. 2018 International Consensus Meeting on Musculoskeletal Infection: Research Priorities from the General Assembly Questions. J Orthop Res. 2019;37:997-1006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 194] [Article Influence: 32.3] [Reference Citation Analysis (0)] |
| 21. | Suzuki G, Saito S, Ishii T, Motojima S, Tokuhashi Y, Ryu J. Previous fracture surgery is a major risk factor of infection after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2011;19:2040-2044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 67] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 22. | Lizaur-Utrilla A, Collados-Maestre I, Miralles-Muñoz FA, Lopez-Prats FA. Total Knee Arthroplasty for Osteoarthritis Secondary to Fracture of the Tibial Plateau. A Prospective Matched Cohort Study. J Arthroplasty. 2015;30:1328-1332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 54] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 23. | Klatte TO, Schneider MM, Citak M, Oloughlin P, Gebauer M, Rueger M, Gehrke T, Kendoff D. Infection rates in patients undergoing primary knee arthroplasty with pre-existing orthopaedic fixation-devices. Knee. 2013;20:177-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 24. | Ge DH, Anoushiravani AA, Kester BS, Vigdorchik JM, Schwarzkopf R. Preoperative Diagnosis Can Predict Conversion Total Knee Arthroplasty Outcomes. J Arthroplasty. 2018;33:124-129.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 25. | Ehlinger M, D'Ambrosio A, Vie P, Leclerc S, Bonnomet F, Bonnevialle P, Lustig S, Parratte S, Colmar M, Argenson JN; French Society of Orthopedic Surgery, Traumatology (SoFCOT). Total knee arthroplasty after opening- versus closing-wedge high tibial osteotomy. A 135-case series with minimum 5-year follow-up. Orthop Traumatol Surg Res. 2017;103:1035-1039. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 26. | Bonacker J, Darowski M, Haar P, Westphal T, Bergschmidt P. Periprosthetic Tibial Fracture with Nonunion and Ascending Prosthetic Joint Infection: A Case Report of an Individual Treatment Strategy. J Orthop Case Rep. 2018;8:3-8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 27. | Sanz-Ruiz P, Matas-Diez JA, Villanueva-Martinez M, Carbo-Laso E, Lopez-Torres II, Vaquero-Martín J. A new biarticular cement spacer technique for infected total hip and knee arthroplasty with massive bone loss. Hip Int. 2021;31:242-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 28. | Müller M, Winkler T, Märdian S, Trampuz A, Renz N, Perka C, Karczewski D. The worst-case scenario: treatment of periprosthetic femoral fracture with coexistent periprosthetic infection-a prospective and consecutive clinical study. Arch Orthop Trauma Surg. 2019;139:1461-1470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 29. | Ebraheim NA, Kelley LH, Liu X, Thomas IS, Steiner RB, Liu J. Periprosthetic Distal Femur Fracture after Total Knee Arthroplasty: A Systematic Review. Orthop Surg. 2015;7:297-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 87] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 30. | Carta S, Fortina M, Riva A, Meccariello L, Manzi E, Di Giovanni A, Ferrata P. The Biological Metallic versus Metallic Solution in Treating Periprosthetic Femoral Fractures: Outcome Assessment. Adv Med. 2016;2016:2918735. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 31. | Peters CL, Bachus KN, Davitt JS. Fixation of periprosthetic femur fractures: a biomechanical analysis comparing cortical strut allograft plates and conventional metal plates. Orthopedics. 2003;26:695-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 1.4] [Reference Citation Analysis (0)] |