Published online Apr 6, 2023. doi: 10.12998/wjcc.v11.i10.2308
Peer-review started: December 16, 2022
First decision: January 31, 2023
Revised: February 16, 2023
Accepted: March 9, 2023
Article in press: March 9, 2023
Published online: April 6, 2023
Processing time: 104 Days and 5.1 Hours
Conservative treatments have been reported to diminish or resolve clinical symptoms of lumbar intervertebral disc herniation (LIDH) within a few weeks.
Computed tomography and magnetic resonance imaging (MRI) of the lumbar region of a 25-year-old male diagnosed with LIDH showed prolapse of the L5/S2 disc. The disc extended 1.0 cm beyond the vertebral edge and hung along the posterior vertebral edge. The patient elected a conservative treatment regimen that included traditional Chinese medicine (TCM), acupuncture, and massage. During a follow-up period of more than 12 mo, good improvement in pain was reported without complications. MRI of the lumbar region after 12 mo showed obvious reabsorption of the herniation.
A conservative treatment regimen of TCM, acupuncture, and massage promoted reabsorption of a prolapsed disc.
Core Tip: Lumbar intervertebral disc herniation is diagnosed worldwide. Generally, non-surgical treatments are recommended and may consist of physical therapy, complementary and alternative medicine options (e.g., acupuncture, acupotomy, Chinese massage, and Chinese herbal medicine), and pharmacotherapy. The latter can include muscle relaxants, systemic steroids, and steroid injections. We report a case of reabsorption of lumbar disc herniation following a conservative treatment regimen involving traditional Chinese medicine, acupuncture, and massage.
- Citation: Wang CA, Zhao HF, Ju J, Kong L, Sun CJ, Zheng YK, Zhang F, Hou GJ, Guo CC, Cao SN, Wang DD, Shi B. Reabsorption of intervertebral disc prolapse after conservative treatment with traditional Chinese medicine: A case report. World J Clin Cases 2023; 11(10): 2308-2314
- URL: https://www.wjgnet.com/2307-8960/full/v11/i10/2308.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i10.2308
Lumbar intervertebral disc herniation (LIDH) affects approximately 9% of the population worldwide, with 30%–40% of asymptomatic individuals diagnosed with LIDH upon imaging examination[1]. For the majority of affected patients, non-surgical treatment can achieve varying degrees of pain relief, as well as relief or cure of other symptoms[2]. Since Guinto et al[3] reported reabsorption of disc herniation in 1984[3], cases involving reabsorption of the nucleus pulposus have been reported more frequently[4]. In contrast, reports of reabsorption of seriously prolapsed discs following conservative traditional Chinese medicine (TCM) treatment have been rarer. The present case report describes a patient manifesting obvious disc nucleus pulposus reabsorption. Conservative treatment with TCM, including acupuncture, massage, and Chinese medicine, was elected and the results are described.
A 25-year-old man had low back pain with right lower limb pain for 15 d.
The patient presented with low back pain with right lower limb pain 15 d ago.
Past health denied any other medical history.
The patient denied any history of genetic disease or infection.
Vital signs for the patient upon admittance were: body temperature, 36.5 °C; blood pressure, 112/70 mmHg; heart rate, 84 beats per min; respiratory rate, 18 breaths per min. The patient presented in a forced position, was limping, and exhibited slight straightening of lumbar curvature. Obvious limited mobility of the lumbar region was noted, with marked tenderness present between the L4 and S1 spinous process and the right side of the spine. Radiating numbness in the right lower limb and negative knocking pain were further reported. A neurological examination revealed no abnormalities. Various physical tests were performed. Positive results were obtained for the right straight leg raising test (Lasegue) to 30°, strengthening test, right piriformis muscle tension test, cervical flexion test (Linder), and lying on the back with a straight stomach test. In contrast, the cross leg lifts test, right femoral nerve stretching test, and Patrick test were negative. Patellar tendon reflex, Achilles tendon reflex, and double lower limb muscle strength and tension were normal. There were no obvious abnormalities in depth sensation. Grade five bilateral hallux dorsalis extension muscle strength was observed and the bilateral Babinski sign was negative.
Routine blood work was performed: Neutrophilic granulocyte percentage, 75.54%; percentage of eosinophils, 0.24%; lymphocyte percentage, 17.92%; hypersensitive C-reactive protein, 11.89 mg/L. Routine examination of urine and stool showed no abnormalities. Liver function, erythrocyte sedimentation rate, and biochemical examinations were also within normal ranges.
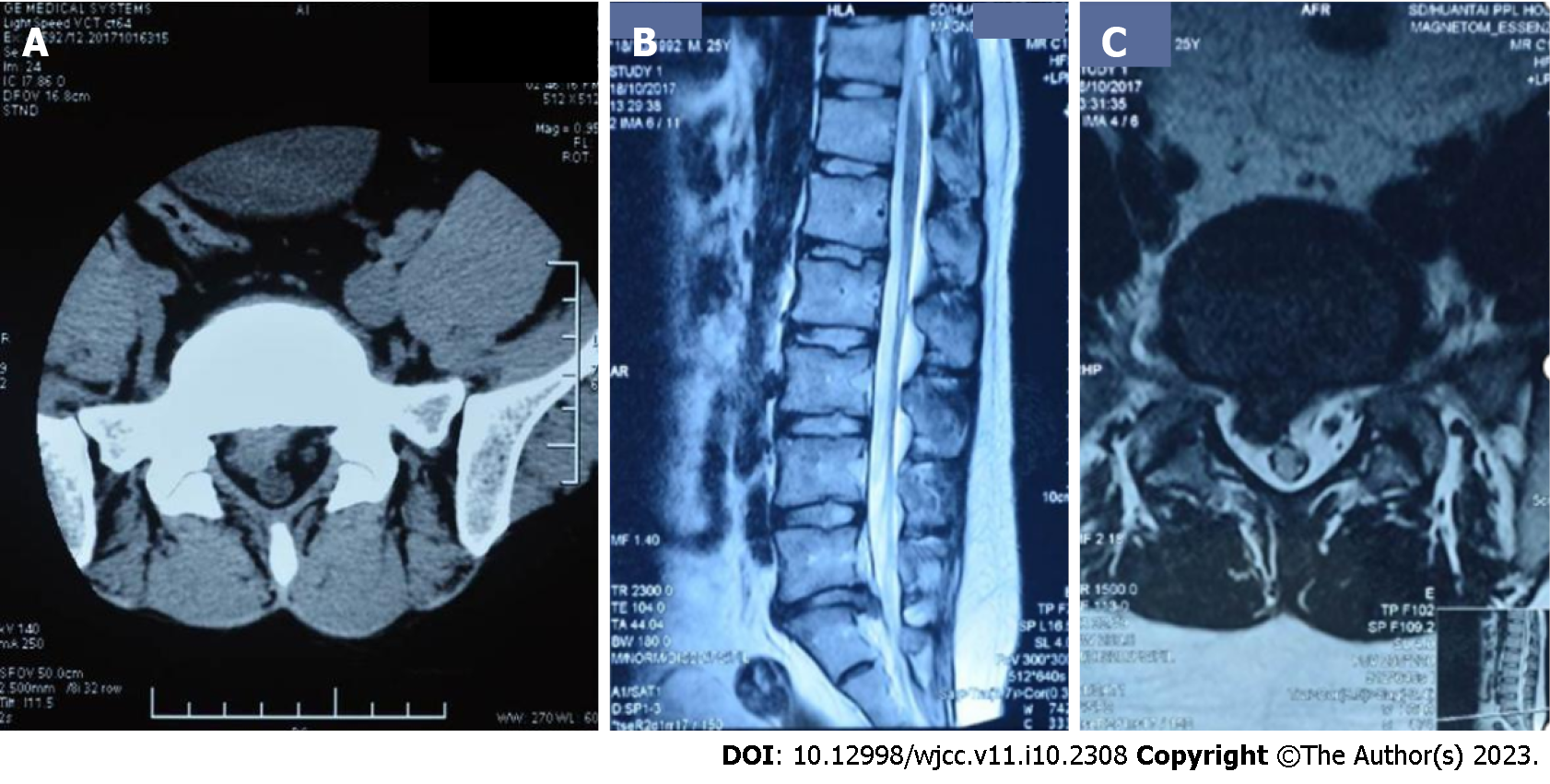
A computed tomography (CT) scan of the lumbar region was conducted in October 2017 and revealed a L5/S1 disc prolapse, nucleus pulposus detachment into the spinal canal, and compression of the right nerve root (Figure 1). The scan indicated a serious condition where protrusion could potentially cause damage to the spinal cord. To determine the extent of bone marrow compression, magnetic resonance imaging (MRI) was also performed of the lumbar region. Stenosis of the right lateral recess and compression of the right nerve root were found to be caused by a L5/S1 intervertebral disc prolapse (Figure 1). The disc was 1.0 cm beyond the vertebral edge and hung along the posterior vertebral edge. The effective sagittal diameter of the spinal canal was 0.7–0.8 cm (Figure 1). The patient was diagnosed with LIDH and surgical resection was recommended. However, the patient elected to undergo conservative treatment involving TCM.
The combination of symptoms and signs allowed the patient to be finally diagnosed as having LIDH.
The patient received an injection of 4 mg Lornoxicam (Hangzhou Aoya Biotechnology Company Limited; catalog No. H20043685) diluted in 250 mL 0.9% sodium chloride once daily for a total of six days.
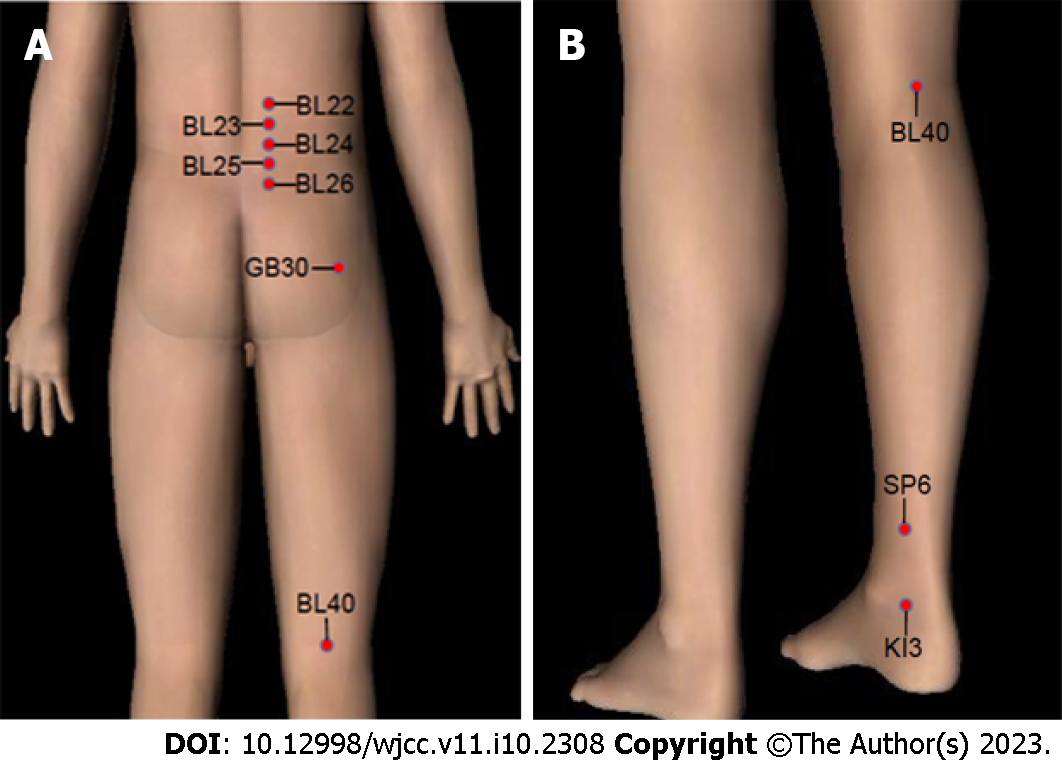
Multiple procedures were applied to the patient’s lumbar vertebra for a total of 10 d. (1) A palm rubbing method was applied to the patient's waist, buttocks, and right lower limb repeatedly in that order for approximately 5 min; (2) Pressure was applied to vertical pressure acupoints for 1 min with both hands applied to Sanjiaoshu (BL22), Shenshu (BL23), Qihaishu (BL24), Dachangshu (BL25), Guanyuanshu (BL26), Huantiao (GB30), and Weizhong (BL40), respectively (Figure 2); (3) A pulling and shaking method was applied while the patient had both hands extended outwards and upwards to hold the edge of the bed. The physician held the patient's ankles for 2 min to apply continuous traction. The patient's lower limbs were then lifted slightly and shaken gently five times to apply force to the waist; (4) A Pull waist method was applied with the doctor pressing on the lumbar area with both hands. The pressing maintained a rhythm consistent with the breathing pattern of the patient for 1 min, with pressing applied upon expiration and pressing relieved upon inspiration. The effect was to achieve a vibration in the lumbar region. When pressing and fixing the affected waist, the lower limbs were pulled backward (either one side was pulled back at a time, and then the same motion applied to the other side, or both sides could be pulled back at the same time). This manipulation was performed three times in succession; and (5) With the patient lying on their back, flexion and hip compression was performed two to three times. This induced the spine to flex forward and leave the vertebral back margin relatively open.
The acupuncture points used in this study were: Sanjiaoshu (BL22), Shenshu (BL23), Qihaishu (BL24), Dachangshu (BL25), Guanyuanshu (BL26), Huantiao (GB30), Weizhong (BL40), Sanyinjiao (SP6), and Taixi (KI3) (Figure 2). Briefly, the patient was placed in a prone position on the treatment bed and the acupoints were disinfected with iodine. A total of 18 bilateral punctures were made using sterile disposable acupuncture needles (34G, 0.25 mm × 40 mm, Hua Tuo, Suzhou Medical Supplies Factory Co. LTD., Jiangsu, China). Each needle was kept in the acupuncture point for 30 min. In addition, the waist and right hip were irradiated using a specific electromagnetic spectrum (TDP) magic lamp (Hengming Medical LTD., Sichuan, China).
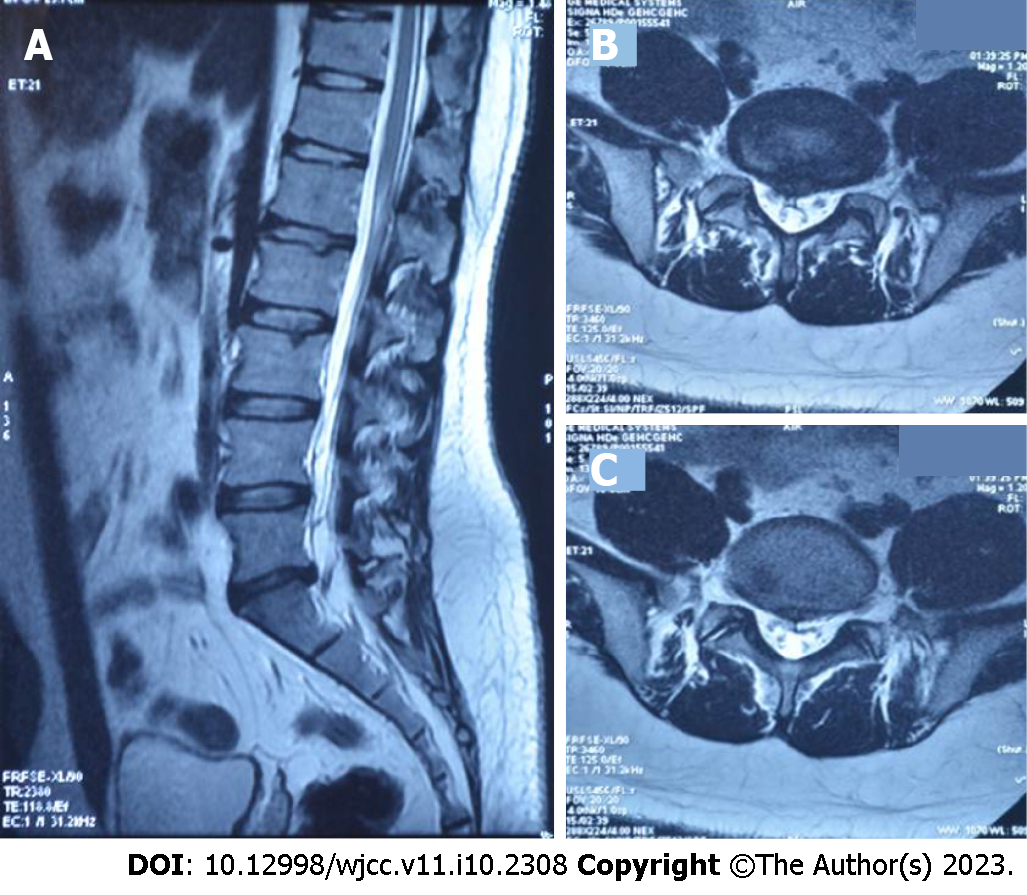
After the treatment period, the patient's lower back pain and numbness of the right lower limb were alleviated. Discharge instructions indicated that the patient was to keep warm and rested. Instructions for frequently exercising muscles in the lower back were also provided. For more than 12 mo, the patient demonstrated good improvement in pain without any complications. A second lumbar MRI was performed in November 2018. Significant reabsorption of the herniation was observed (Figure 3).
Both genetic and environmental factors can accelerate loss of nutrition and induce a mechanical imbalance of an intervertebral disc. As a result, the structure of the intervertebral disc can be compromised and lumbar disc herniation can occur[5]. Non-surgical treatment is primarily recommended for lumbar disc herniation[6,7], and this can include drug treatment, physiotherapy, acupuncture, and massage[6]. With advances in intervertebral disc imaging, an increasing number of cases have demonstrated absorption of herniated lumbar discs[7]. Furthermore, it has been demonstrated that the size of a herniation positively correlates with the symptoms of LIDH[7].
Disc prolapse can cause lumbar and leg pain. For prolapsed lumbar discs, surgery is a common treatment[8]. However, negative effects can accompany the treatment effects achieved with surgery[9,10]. Consequently, non-surgical treatment options have been more frequently considered. Hong and Ball[7] reported a 29-year-old female patient with a prolapsed lumbar 4/5 intervertebral disc who underwent physical therapy and epidural injections of glucocorticoids for treatment[7]. After five months, the protruding nucleus pulposus was gradually absorbed[7]. Herniated nucleus pulposus reabsorption has become an active and engaging topic in both clinical and basic research. It also represents a new direction in conservative treatment. In the present case, the patient exhibited a much more serious prolapse than previously reported cases, with the lumbar disc extending 1.0 cm beyond the vertebral edge and hanging along the posterior vertebral edge. Nevertheless, the prolapsed lumbar disc was reabsorbed after applying a treatment regimen that included TCM, acupuncture, and massage.
Massage is widely used in China and can have a significant effect. Massage as used in TCM involves an acupoint massage manipulation that is based on the meridian theory. Briefly, massage mediates a dredging of the meridians, thereby promoting blood circulation, invigorating qi, removing cold, and relieving pain[11,12]. Modern medicine has ascribed three functions to massage of the waist area. First, it can reduce pressure in an intervertebral disc, concomitantly it increases the pressure outside the disc, and it promotes reinstatement of the protrusion and creates favorable conditions for repair of the fibrous ring. Second, massage changes the position of the protrusion to release adhesions between the protrusion and the nerve root, relieves or reduces compression, stimulates the nerve root affected by the protrusion, and relieves symptoms[13]. Third, massage relaxes muscles in the waist and buttocks[14], strengthens circulation of local qi and blood, and facilitates recovery of normal function in diseased nerve roots[12]. However, the biological mechanisms mediating the effects of massage treatment of LIDH and reabsorption of prolapsed intervertebral discs remain unclear and require further investigation.
The present case demonstrates that it is possible for a prolapsed disc to be reabsorbed with application of acupuncture and massage therapy in combination with TCM. Generally, prolapse is an indication for surgical treatment. However, the present case expands the scope of non-surgical treatment and provides an example of successful conservative treatment of LIDH with TCM. It remains for the possibility and probability of prolapsed intervertebral disc absorption to be evaluated in order to ensure the effectiveness and safety of this type of conservative treatment. Further study is also needed to provide a theoretical basis for this type of non-surgical treatment of a prolapsed lumbar disc. A large sample epidemiological investigation could demonstrate the likelihood of disc reabsorption, while a randomized controlled clinical trial could evaluate the effectiveness and safety of acupuncture and massage as a conservative therapy.
In the present case report, conservative treatment including TCM, acupuncture and massage were able to relieve a patient’s LIDH symptoms of waist and leg pain and numbness. The TCM regimen applied also promoted significant reabsorption of the prolapsed intervertebral disc to its normal position. Thus, TCM may represent an alternative non-surgical treatment for ruptured giant prolapse of an intervertebral disc that patients should consider.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cheng TH, Taiwan; Li J, China S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Ropper AH, Zafonte RD. Sciatica. N Engl J Med. 2015;372:1240-1248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 191] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 2. | Abou-Elroos DA, El-Toukhy MAE, Nageeb GS, Dawood EA, Abouhashem S. Prolonged Physiotherapy versus Early Surgical Intervention in Patients with Lumbar Disk Herniation: Short-term Outcomes of Clinical Randomized Trial. Asian Spine J. 2017;11:531-537. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Guinto FC Jr, Hashim H, Stumer M. CT demonstration of disk regression after conservative therapy. AJNR Am J Neuroradiol. 1984;5:632-633. [PubMed] |
| 4. | Zhong M, Liu JT, Jiang H, Mo W, Yu PF, Li XC, Xue RR. Incidence of Spontaneous Resorption of Lumbar Disc Herniation: A Meta-Analysis. Pain Physician. 2017;20:E45-E52. [PubMed] |
| 5. | Tsarouhas A, Soufla G, Tsarouhas K, Katonis P, Pasku D, Vakis A, Tsatsakis AM, Spandidos DA. Molecular profile of major growth factors in lumbar intervertebral disc herniation: Correlation with patient clinical and epidemiological characteristics. Mol Med Rep. 2017;15:2195-2203. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Zhang B, Xu H, Wang J, Liu B, Sun G. A narrative review of non-operative treatment, especially traditional Chinese medicine therapy, for lumbar intervertebral disc herniation. Biosci Trends. 2017;11:406-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 61] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 7. | Hong J, Ball PA. IMAGES IN CLINICAL MEDICINE. Resolution of Lumbar Disk Herniation without Surgery. N Engl J Med. 2016;374:1564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Kapoor S, Amarouche M, Al-Obeidi F, U-King-Im JM, Thomas N, Bell D. Giant thoracic discs: treatment, outcome, and follow-up of 33 patients in a single centre. Eur Spine J. 2018;27:1555-1566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Wilson CA, Roffey DM, Chow D, Alkherayf F, Wai EK. A systematic review of preoperative predictors for postoperative clinical outcomes following lumbar discectomy. Spine J. 2016;16:1413-1422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 71] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 10. | Dorow M, Löbner M, Stein J, Pabst A, Konnopka A, Meisel HJ, Günther L, Meixensberger J, Stengler K, König HH, Riedel-Heller SG. The Course of Pain Intensity in Patients Undergoing Herniated Disc Surgery: A 5-Year Longitudinal Observational Study. PLoS One. 2016;11:e0156647. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Niu JF, Zhao XF, Hu HT, Wang JJ, Liu YL, Lu DH. Should acupuncture, biofeedback, massage, Qi gong, relaxation therapy, device-guided breathing, yoga and tai chi be used to reduce blood pressure? Complement Ther Med. 2019;42:322-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Mei L, Miao X, Chen H, Huang X, Zheng G. Effectiveness of Chinese Hand Massage on Anxiety Among Patients Awaiting Coronary Angiography: A Randomized Controlled Trial. J Cardiovasc Nurs. 2017;32:196-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Kukimoto Y, Ooe N, Ideguchi N. The Effects of Massage Therapy on Pain and Anxiety after Surgery: A Systematic Review and Meta-Analysis. Pain Manag Nurs. 2017;18:378-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 14. | Weerapong P, Hume PA, Kolt GS. The mechanisms of massage and effects on performance, muscle recovery and injury prevention. Sports Med. 2005;35:235-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 354] [Cited by in RCA: 401] [Article Influence: 20.1] [Reference Citation Analysis (0)] |