Published online Apr 6, 2023. doi: 10.12998/wjcc.v11.i10.2237
Peer-review started: October 20, 2022
First decision: December 26, 2022
Revised: January 3, 2023
Accepted: March 15, 2023
Article in press: March 15, 2023
Published online: April 6, 2023
Processing time: 161 Days and 3.7 Hours
Coronavirus disease 2019 (COVID-19) is a major and costly public health emergency.
To investigate the impact of China’s lockdown policies during the COVID-19 outbreak on the level I trauma center of a tertiary comprehensive hospital of Traditional Chinese Medicine.
All patients admitted to our trauma center during a lockdown in 2020 and the same period in 2019 were enrolled. We collected data on demographics, daily visits, injury type, injury mechanism, injury severity score, and patient management for comparative analysis.
The total number of patients in the trauma center of our hospital decreased by 50.38% during the COVID-19 Lockdown in 2020 compared to the same period in 2019. The average number of trauma visits per day in 2019 was 47.94, compared to 23.79 in 2020. Comparing the patients’ demographic data, loss of employment was the most predominate characteristic in 2020 compared to 2019, while there was no significant difference in gender, age, and marital status between both periods. During the lockdown period, the proportion of traffic accident-related injuries, injuries due to falls greater than 1.5 m, and mechanical injuries decreased significantly, whereas the proportion of injuries caused by falls less than 1.5 m, cuts, assault, bites, and suicidal tendencies and other injuries increased relatively. In addition, the proportion of patients with minor injuries increased and serious injuries decreased during the lockdown. The hospitalization rate increased significantly, and there was no significant difference in emergency surgery and death rates.
The lockdown policies during the COVID-19 outbreak significantly altered the number and mechanism of traumatic events in our hospital, which can be monitored regularly. Our results suggest that mandatory public health prevention and control measures by the government can reduce the incidence of traumatic events and the severity of traumatic injuries. Emergency surgery and mortality rates remain high, increased because of factors such as family injury and penetrating injury, and hospitalization rates have increased significantly. Therefore, our trauma center still needs to be fully staffed. Finally, from the perspective of the injury mechanism, indoor trauma is a major risk during a lockdown, and it is particularly important to develop prevention strategies for such trauma to reduce the medical burden of the next catastrophic epidemic.
Core Tip: First of all, during the coronavirus disease 2019 pandemic, the incidence of traumatic events in our city has been greatly reduced thanks to effective government control. In addition, from the perspective of injury mechanism, indoor trauma is a major risk during lockdown periods; therefore, it is particularly important to develop prevention strategies for such trauma to reduce the medical burden of the next catastrophic epidemic.
- Citation: Shen BS, Cheng WY, Liang ZR, Tang Q, Li KY. Impact of lockdown policies during the COVID-19 outbreak on a trauma center of a tertiary hospital in China. World J Clin Cases 2023; 11(10): 2237-2245
- URL: https://www.wjgnet.com/2307-8960/full/v11/i10/2237.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i10.2237
Coronavirus disease 2019 (COVID-19) was first detected in Wuhan, China[1], which spread rapidly worldwide and emerged as a pandemic[2-3], posing a major threat to the health of all populations[4]. The Chinese government adopted a series of unprecedented restrictions to contain the COVID-19 pandemic, including community lockdown, transportation restrictions, work cessation, school closures, home quarantine, and bans on all types of social activities. Guangdong province initiated a level I special major public health emergency response from January 23 to February 24, 2020, which marked the official start of a total lockdown. During this period, many major hospitals globally showed an overall decrease in the number of patients admitted and the admission rates for unrelated COVID-19 infections[5-6], as well as corresponding changes in trauma patterns and mechanisms[7-10]. It is unknown whether these lockdown policies reduced the demand on the health care system and the occurrence of trauma injuries. As a result, we conducted a study to investigate the impact of the lockdown policies on the level I trauma center of a tertiary comprehensive hospital of traditional Chinese medicine (TCM).
It should be noted that our hospital did not admit any COVID-19 patients during this period. Therefore, we believe that this study objectively presents accurate evidence of traumatic conditions unrelated to COVID-19, as the impact of visits attrition due to COVID-19 patients was excluded.
We conducted a retrospective study of all trauma patients admitted to the trauma center of a tertiary comprehensive Hospital of TCM. This is a comprehensive tertiary hospital located in the center of Foshan City, Guangdong Province, and it is famous for its orthopedics department. Its comprehensive strength has been ranked first among TCM hospitals in prefecture-level cities for many years in China, and the trauma center of the emergency department is particularly prominent. This study enrolled all patients who visited the emergency trauma center from January 23 to February 24 in 2019 and 2020. All data were obtained from the Electronic Registration Database of Trauma Institutions in the emergency department of our hospital. There were 1582 cases in 2019 and only 785 cases in 2020. The study was approved by the Institutional Review Board of our hospital, and the need for informed consent was waived.
We collected data on demographics, daily visits, injury type, injury mechanism, injury severity score (ISS), and patient management. Demographic characteristics included gender, age, occupation, and marital status. The injury type was defined to include blunt, penetrating, burns, and others. The injury mechanisms were divided into the following categories: (1) Traffic accident-related, including motor vehicle collisions, motorcycle collisions, and other pedestrian accidents; (2) falls greater than or less than 1.5 m; (3) machine-related; (4) cuts; (5) assault; (6) bites, including bee stings and animal and snake bites; (7) suicidal tendencies; and (8) reasons other than those mentioned above. The severity of the injury was set according to the international ISS scoring standard. Patient management included emergency surgery, hospitalization, leave granted, death, and others. We obtained complete data for all patients, and no one was excluded from the analysis.
Categorical data were described as number (percentage) and compared using Chi-squared and Fisher’s Exact test, as appropriate. Continuous variables were expressed as mean (standard deviation, SD) and compared using the two-sample t-test. p < 0.05 was considered statistically significant. Statistical Package for the Social Sciences version 22.0 was used for statistical analysis.
As shown in Table 1, our hospital enrolled a total of 2367 trauma patients in both phases, none of whom had been diagnosed with COVID-19. There were 1582 trauma cases in 2019 and only 785 in 2020, indicating a 50.38% overall decline in trauma cases in 2020 compared to the same period in 2019. Besides the significant difference in employment status in the occupational classification between 2020 and 2019 (21.81% and 18.22%, p = 0.042), there was no significant difference in the remaining demographic characteristics (p > 0.05).
| 2019, n = 1582 | 2020, n = 785 | P value | ||
| Age, mean (SD) | 34.01 (22.13) | 32.84 (23.57) | 0.236 | |
| Age groups | < 18 | 396 (25.03) | 195 (24.84) | 0.92 |
| 18–45 | 712 (45.01) | 348 (44.33) | 0.756 | |
| 46–60 | 237 (14.98) | 107 (13.63) | 0.38 | |
| > 60 | 237 (14.98) | 135 (17.20) | 0.163 | |
| Gender | Male | 1052 (66.50) | 505 (64.33) | 0.296 |
| Female | 530 (33.50) | 280 (35.67) | ||
| Occupation | Employed | 345 (21.81) | 143 (18.22) | 0.042a |
| Unemployed | 759 (47.98) | 377 (48.02) | 0.982 | |
| Not recorded | 478 (30.21) | 265 (33.76) | 0.08 | |
| Marital status | Married | 554 (35.02) | 282 (35.92) | 0.665 |
| Unmarried | 727 (45.95) | 368 (46.88) | 0.671 | |
| Minor | 301 (19.03) | 135 (17.20) | 0.28 |
As shown in Figure 1, the data were combined into the total number of cases over 3 d. The daily intake of trauma patients in our hospital during the lockdown phase in 2020 was less than that in 2019, with an average of 47.94 trauma patient visits per day in 2019 compared to 23.79 in 2020.
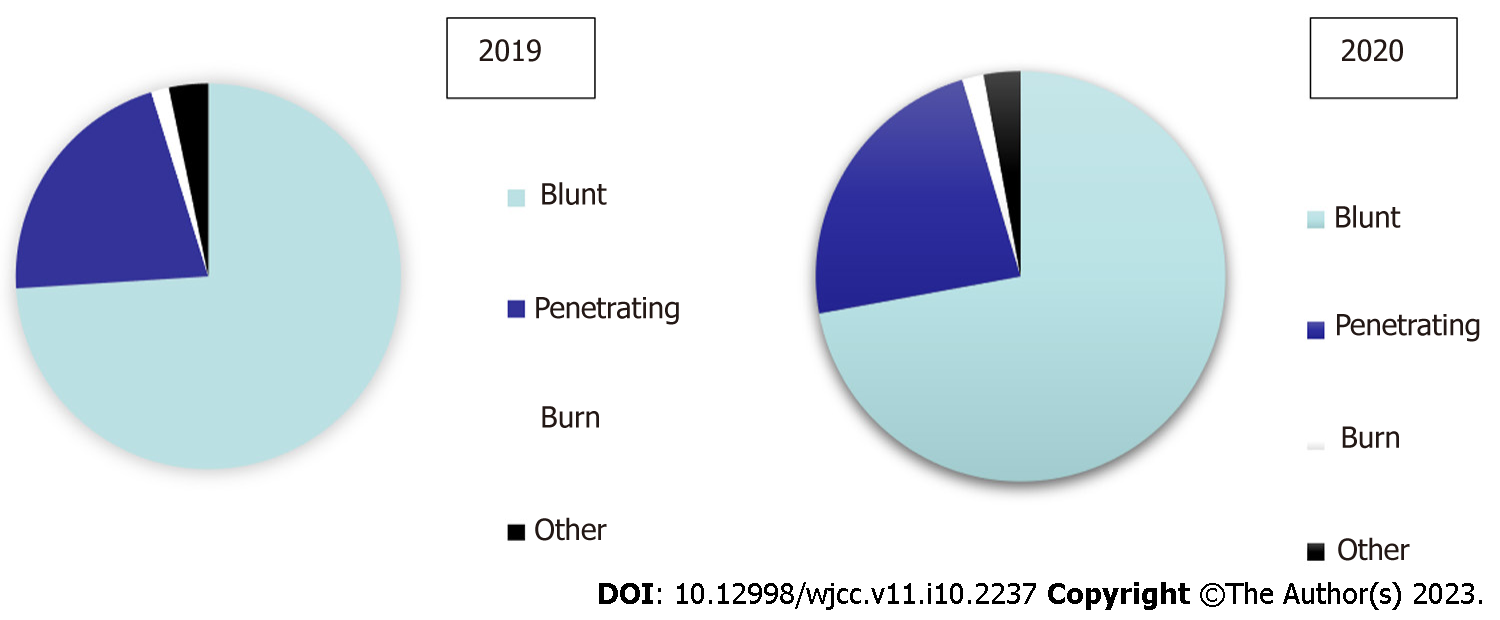
As shown in Figure 2, there was not significant difference in injury type, including blunt injury (74.02% vs 72.10%, p = 0.320), penetrating injury (21.18% vs 23.31%, p = 0.237), burns (1.52% vs 1.66%, p = 0.797), and others (3.29% vs 2.93%, p = 0.641), between the 2020 and 2019 periods, and there was no association between injury type and the government blockade policy in 2020 (all p > 0.05).
As shown in Table 2, the number of all injury mechanisms decreased in 2020 compared with 2019, but their proportions varied in the same period. The proportion of traffic accident-related injury (20.51% vs 24.72%, p = 0.023), fall (> 1.5 m) injury (6.75% vs 9.73%, p = 0.016), and mechanical injury (18.09% vs 22.06%, p = 0.025) showed a significant decreasing trend from 2019 to 2020. However, the proportion of fall (< 1.5 m) (18.34% vs 15.04%, p = 0.040), cut (14.90% vs 10.81%, p = 0.004), assault (3.69% vs 2.28%, p = 0.047), bites (3.18% vs 2.28%, p = 0.189), suicidal tendencies (1.66% vs 1.52%, p = 0.797), and other injury mechanisms (12.87% vs 11.57%, p = 0.360) all increased. Among them, there was a significant difference in fall (< 1.5 m), cut, and assault (p < 0.05), but there was no significant difference in the other three injury mechanisms (p > 0.05).
| 2019, n = 1582 | 2020, n = 785 | P value | |
| Traffic accident-related | 391 (24.72) | 161 (20.51) | 0.023a |
| Fall-greater than 1.5 m | 154 (9.73) | 53 (6.75) | 0.016a |
| Fall-less than 1.5 m | 238 (15.04) | 144 (18.34) | 0.040a |
| Machine-related | 349 (22.06) | 142 (18.09) | 0.025a |
| Cut | 171 (10.81) | 117 (14.90) | 0.004a |
| Assault | 36 (2.28) | 29 (3.69) | 0.047a |
| Bites | 36 (2.28) | 25 (3.18) | 0.189 |
| Suicidal tendencies | 24 (1.52) | 13 (1.66) | 0.797 |
| Other | 183 (11.57) | 101 (12.87) | 0.36 |
Regarding the assessment of trauma severity (shown in Table 3), the overall mean ISS level in 2020 was lower than that in 2019, and the difference was statistically significant (p < 0.05). Further division of ISS according into degrees showed that the proportion of patients with ISS score < 15 (81.91% vs 78.13%, p = 0.032) in 2020 was significantly higher than that in 2019, while the proportion of patients with ISS score > 25 (1.40% vs 2.72%, p = 0.043) was significantly higher in 2019 compared with 2020. There was no difference in the proportion of patients with ISS score between 15 and 25 (p > 0.05).
In terms of disposal methods (shown in Table 4), the rates of emergency surgery (37.07% vs 33.63%, p = 0.098) and hospitalization (18.47% vs 12.20%, p < 0.01) in 2020 were both higher than those in 2019, but with no statistical difference in the former (p > 0.05). However, there was a decrease in the proportion of leave granted (41.27% vs 50.63%, p < 0.01), death (0.25% vs 0.38%, p = 0.908), and others (2.93% vs 3.16%, p = 0.760) in 2020 compared with 2019, with a significant difference only in the rate of leave granted (p < 0.05).
It is well known that trauma places a heavy burden on global healthcare systems[11]. The COVID-19 pandemic poses an even more serious challenge to trauma centers, similar to a relentless mass casualty event[12]. In addition, the morbidity and mortality caused by COVID-19 prompted the government to institute an unprecedented and severe lockdown policy to control the spread of the virus[13]. Some scholars reported that the COVID-19 outbreak has increased the pressure of medical care, and that many facilities have exceeded their original resource capacity load and will be exhausted[14]. Another study suggested that the burden of trauma during COVID-19 can be reduced by social distancing and the advice to stay at home[15]. Based on the above findings, it is unclear how these lockdown policies have affected our trauma center.
Our study showed an overall decline of 50.38% in the number of trauma patients treated in the trauma center of our hospital during the lockdown period from January 23 to February 24, 2020, compared to the same period in 2019. Both daily and total visits decreased, which is similar to the results in most countries[16-20]. Young and middle-aged individuals accounted for the highest proportion of the trauma patients, and the injuries were observed mainly among males. In addition, we found that the number of employed patients declined significantly during the COVID-19 outbreak. This may be due to the disproportionate combined influence of various socioeconomic factors. For instance, most high-income individuals have transitioned to working at home, while most unemployed persons may continue to work outside due to economic pressure[21]. Such employees include taxi drivers, construction workers, teachers, technicians, and civil servants. However, our study did not make this comparison.
Although the injury types in these two periods were similar to those in other studies[22], there was no significant difference after analysis of the results. However, there are certain rules in the mechanism of injury. We found that the lockdown period significantly reduced injuries due to traffic accident, falls greater than 1.5 m, and machine-related injuries, whereas other injury mechanisms such as falls less than 1.5 m, cuts, and assault increased. The Chinese government’s lockdown policy reduced travel, construction works, and manufacturing operations, while home quarantine measures were implemented to limit the spread of the virus. As a result, traffic accidents, high fall injury, mechanical injury, and other types of injury were greatly reduced. Global studies have similarly shown a significant decrease in the number of transportation-related traumas during the COVID-19 pandemic[23-24]. However, the risk of indoor injury did not decrease[8]. For instance, some studies[25-26] showed that injuries caused by falling from a height and using tools at home increased during the lockdown period. The incidence of domestic violence caused by economic pressure, loneliness, and psychological pressure was also much higher during the COVID-19 pandemic than before[27-29]. Regarding trauma severity, we observed that the mean ISS score during the lockdown period was lower than that of the same period in 2019, with the main significant difference being an increase in the proportion of low scores (< 15) and a decrease in the proportion of high scores (> 25). This is consistent with the studies of Andreozzi et al[30] and Qasim et al[12], considering that factors such as family injury and penetrating injury increase the proportion of emergency surgery, but the risk of death is also small due to the low severity of this type of injuries[12,30]. The proportions of emergency surgery and mortality in the two periods were not significantly different. However, the hospital’s demand for emergency surgery and inpatient wards remained unchanged[31]. This indicates that a lockdown period can indeed reduce the overall severity of injuries, and that mainly minor injuries occur during such periods[32,33]. Moreover, our study found that hospitalization rates increased significantly during lockdown periods. Trauma is still an important cause of many hospitalizations[11].
Our study has some limitations. First, the data were only from the trauma center of one hospital, and the sample size was small, which did not satisfy the needs of other regions in China. Second, results of retrospective studies based on electronic medical records have a certain degree of subjectivity, which may increase the information error. However, we believe that COVID-19 Lockdown regularly has a negative impact on humans, and this study certainly adds to existing evidence. It is hoped that we can conduct a national multi-center study to confirm similar findings and further evaluate the impact of the Chinese government’s lockdown policy on hospital trauma centers to provide information and allocate trauma medical resources for the prevention of the next catastrophic infectious disease.
The lockdown policy during the COVID-19 outbreak significantly changed the number and mechanism of traumatic events in our hospital, which can be monitored regularly. Mandatory prevention and control measures by the government can reduce the occurrence and severity of traumatic events and significantly reduce the incidence of traffic accidents, falling injuries, and machine injuries. However, high rates of emergency surgery, mortality, and hospitalizations have led to the need for better staffing of health care personnel. Finally, there is a need to focus on indoor trauma, which is particularly important in terms of prevention strategies, to reduce the medical burden of the next catastrophic epidemic.
Coronavirus disease 2019 (COVID-19) was spread rapidly worldwide and emerged as a pandemic, posing a major threat to the health of all populations.
It is unknown whether these lockdown policies reduced the demand on the health care system and the occurrence of trauma injuries. As a result, we conducted a study to investigate the impact of the lockdown policies on the level I trauma center of a tertiary comprehensive hospital of traditional Chinese medicine (TCM).
This study aimed to investigate the impact of China’s lockdown policies during the COVID-19 outbreak on the level I trauma center of a tertiary comprehensive hospital of TCM.
All patients admitted to our trauma center during a lockdown in 2020 and the same period in 2019 were enrolled. We collected data on demographics, daily visits, injury type, injury mechanism, injury severity score, and patient management for comparative analysis.
The total number of patients in the trauma center of our hospital decreased by 50.38% during the COVID-19 Lockdown in 2020 compared to the same period in 2019. The average number of trauma visits per day in 2019 was 47.94, compared to 23.79 in 2020. Comparing the patients’ demographic data, loss of employment was the most predominate characteristic in 2020 compared to 2019, while there was no significant difference in gender, age, and marital status between both periods. During the lockdown period, the proportion of traffic accident-related injuries, injuries due to falls greater than 1.5 m, and mechanical injuries decreased significantly, whereas the proportion of injuries caused by falls less than 1.5 m, cuts, assault, bites, and suicidal tendencies and other injuries increased relatively. In addition, the proportion of patients with minor injuries increased and serious injuries decreased during the lockdown. The hospitalization rate increased significantly, and there was no significant difference in emergency surgery and death rates.
The lockdown policies during the COVID-19 outbreak significantly altered the number and mechanism of traumatic events in our hospital, which can be monitored regularly. Our results suggest that mandatory public health prevention and control measures by the government can reduce the incidence of traumatic events and the severity of traumatic injuries. Increased due to factors such as family injury and penetrating injury, emergency surgery and death rates remain high, and hospitalization rates have increased significantly.
Therefore, our trauma center still needs to be fully staffed. Finally, from the perspective of the injury mechanism, indoor trauma is a major risk during a lockdown, and it is particularly important to develop prevention strategies for such trauma to reduce the medical burden of the next catastrophic epidemic.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Aseni P, Italy; Pantelis AG, Greece; Taghizadeh-Hesary F, Iran S-Editor: Li L L-Editor: A P-Editor: Li L
| 1. | Huang H, Zhang M, Chen C, Zhang H, Wei Y, Tian J, Shang J, Deng Y, Du A, Dai H. Clinical characteristics of COVID-19 in patients with preexisting ILD: A retrospective study in a single center in Wuhan, China. J Med Virol. 2020;92:2742-2750. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 50] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 2. | World Health Organization. WHO Director-General's opening remarks at the media briefing on COVID-19. Mar 11, 2020. [cited April 24, 2020]. Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-may-2020. |
| 3. | Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ; COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395:1973-1987. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2542] [Cited by in RCA: 2387] [Article Influence: 477.4] [Reference Citation Analysis (0)] |
| 4. | Rakhsha A, Azghandi S, Taghizadeh-Hesary F. Decision on Chemotherapy Amidst COVID-19 Pandemic: a Review and a Practical Approach from Iran. Infect Chemother. 2020;52:496-502. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 5. | Williams CH, Scott EM, Dorfman JD, Simon BJ. Traumatic Injury Under COVID-19 Stay-at-Home Advisory: Experience of a New England Trauma Center. J Surg Res. 2022;269:165-170. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Meara JG, Leather AJ, Hagander L, Alkire BC, Alonso N, Ameh EA, Bickler SW, Conteh L, Dare AJ, Davies J, Mérisier ED, El-Halabi S, Farmer PE, Gawande A, Gillies R, Greenberg SL, Grimes CE, Gruen RL, Ismail EA, Kamara TB, Lavy C, Lundeg G, Mkandawire NC, Raykar NP, Riesel JN, Rodas E, Rose J, Roy N, Shrime MG, Sullivan R, Verguet S, Watters D, Weiser TG, Wilson IH, Yamey G, Yip W. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Int J Obstet Anesth. 2016;25:75-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 214] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 7. | Rhodes HX, Petersen K, Biswas S. Trauma Trends During the Initial Peak of the COVID-19 Pandemic in the Midst of Lockdown: Experiences From a Rural Trauma Center. Cureus. 2020;12:e9811. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 8. | Hakeem FF, Alshahrani SM, Ghobain MA, Albabtain I, Aldibasi O, Alghnam S. The Impact of COVID-19 Lockdown on Injuries in Saudi Arabia: Results From a Level-I Trauma Center. Front Public Health. 2021;9:704294. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 9. | Kreis CA, Ortmann B, Freistuehler M, Hartensuer R, Van Aken H, Raschke MJ, Schliemann B. Impact of the first COVID-19 shutdown on patient volumes and surgical procedures of a Level I trauma center. Eur J Trauma Emerg Surg. 2021;47:665-675. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 10. | Nia A, Popp D, Diendorfer C, Apprich S, Munteanu A, Hajdu S, Widhalm HK. Impact of lockdown during the COVID-19 pandemic on number of patients and patterns of injuries at a level I trauma center. Wien Klin Wochenschr. 2021;133:336-343. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 11. | Aljuboori Z, Sieg E. The early effects of social distancing resultant from COVID-19 on admissions to a Level I trauma center. Injury. 2020;51:2332. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Qasim Z, Sjoholm LO, Volgraf J, Sailes S, Nance ML, Perks DH, Grewal H, Meyer LK, Walker J, Koenig GJ, Donnelly J, Gallagher J, Kaufman E, Kaplan MJ, Cannon JW. Trauma center activity and surge response during the early phase of the COVID-19 pandemic-the Philadelphia story. J Trauma Acute Care Surg. 2020;89:821-828. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 59] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 13. | Xie J, Tong Z, Guan X, Du B, Qiu H, Slutsky AS. Critical care crisis and some recommendations during the COVID-19 epidemic in China. Intensive Care Med. 2020;46:837-840. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 320] [Cited by in RCA: 368] [Article Influence: 73.6] [Reference Citation Analysis (0)] |
| 14. | Jackson SE, Garnett C, Shahab L, Oldham M, Brown J. Association of the COVID-19 lockdown with smoking, drinking and attempts to quit in England: an analysis of 2019-20 data. Addiction. 2021;116:1233-1244. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 160] [Cited by in RCA: 184] [Article Influence: 46.0] [Reference Citation Analysis (0)] |
| 15. | Stinner DJ, Lebrun C, Hsu JR, Jahangir AA, Mir HR. The Orthopaedic Trauma Service and COVID-19: Practice Considerations to Optimize Outcomes and Limit Exposure. J Orthop Trauma. 2020;34:333-340. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 60] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 16. | McGuinness MJ, Harmston C; Northern Region Trauma Network. Association between COVID-19 public health interventions and major trauma presentation in the northern region of New Zealand. ANZ J Surg. 2021;91:633-638. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 17. | Morris D, Rogers M, Kissmer N, Du Preez A, Dufourq N. Impact of lockdown measures implemented during the Covid-19 pandemic on the burden of trauma presentations to a regional emergency department in Kwa-Zulu Natal, South Africa. Afr J Emerg Med. 2020;10:193-196. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 18. | van Aert GJJ, van der Laan L, Boonman-de Winter LJM, Berende CAS, de Groot HGW, Boele van Hensbroek P, Schormans PMJ, Winkes MB, Vos DI. Effect of the COVID-19 pandemic during the first lockdown in the Netherlands on the number of trauma-related admissions, trauma severity and treatment: the results of a retrospective cohort study in a level 2 trauma centre. BMJ Open. 2021;11:e045015. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 19. | Venter A, Lewis CM, Saffy P, Chadinha LP. Locked down: Impact of COVID-19 restrictions on trauma presentations to the emergency department. S Afr Med J. 2020;111:52-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 20. | Harris D, Ellis DY, Gorman D, Foo N, Haustead D. Impact of COVID-19 social restrictions on trauma presentations in South Australia. Emerg Med Australas. 2021;33:152-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 21. | Talev M. Axios-Ipsos Coronavirus Index: rich sheltered, poor shafted amid virus. 2020. [cited May 2020]. Available from: https://www.i-com.org/news-articles/axios-ipsos-coronavirus-index-rich-sheltered-poor-shafted-amid-virus. |
| 22. | Devarakonda AK, Wehrle CJ, Chibane FL, Drevets PD, Fox ED, Lawson AG. The Effects of the COVID-19 Pandemic on Trauma Presentations in a Level One Trauma Center. Am Surg. 2021;87:686-689. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 23. | Poggetti A, Del Chiaro A, Nucci AM, Suardi C, Pfanner S. How hand and wrist trauma has changed during covid-19 emergency in Italy: Incidence and distribution of acute injuries. What to learn? J Clin Orthop Trauma. 2021;12:22-26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 24. | Keays G, Friedman D, Gagnon I. Injuries in the time of COVID-19. Health Promot Chronic Dis Prev Can. 2020;40:336-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 79] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 25. | Ruiz-Medina PE, Ramos-Meléndez EO, Cruz-De La Rosa KX, Arrieta-Alicea A, Guerrios-Rivera L, Nieves-Plaza M, Rodríguez-Ortiz P. The effect of the lockdown executive order during the COVID-19 pandemic in recent trauma admissions in Puerto Rico. Inj Epidemiol. 2021;8:22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 26. | Garude K, Natalwala I, Hughes B, West C, Bhat W. Patterns of Adult and Paediatric Hand Trauma During the COVID-19 Lockdown. J Plast Reconstr Aesthet Surg. 2020;73:1575-1592. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 27. | Mackolil J, Mackolil J. Addressing psychosocial problems associated with the COVID-19 lockdown. Asian J Psychiatr. 2020;51:102156. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 56] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 28. | Boserup B, McKenney M, Elkbuli A. Alarming trends in US domestic violence during the COVID-19 pandemic. Am J Emerg Med. 2020;38:2753-2755. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 460] [Cited by in RCA: 372] [Article Influence: 74.4] [Reference Citation Analysis (0)] |
| 29. | Bradbury-Jones C, Isham L. The pandemic paradox: The consequences of COVID-19 on domestic violence. J Clin Nurs. 2020;29:2047-2049. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 507] [Cited by in RCA: 495] [Article Influence: 99.0] [Reference Citation Analysis (0)] |
| 30. | Andreozzi V, Marzilli F, Muselli M, Previ L, Cantagalli MR, Princi G, Ferretti A. The impact of COVID-19 on orthopaedic trauma: A retrospective comparative study from a single university hospital in Italy. Orthop Rev (Pavia). 2020;12:8941. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 31. | İlhan B, Bozdereli Berikol G, Aydın H, Arslan Erduhan M, Doğan H. COVID-19 outbreak impact on emergency trauma visits and trauma surgery in a level 3 trauma center. Ir J Med Sci. 2022;191:2319-2324. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 32. | Christey G, Amey J, Campbell A, Smith A. Variation in volumes and characteristics of trauma patients admitted to a level one trauma centre during national level 4 lockdown for COVID-19 in New Zealand. N Z Med J. 2020;133:81-88. [PubMed] |
| 33. | Trier F, Fjølner J, Raaber N, Sørensen AH, Kirkegaard H. Effect of the COVID-19 pandemic at a major Danish trauma center in 2020 compared with 2018-2019: A retrospective cohort study. Acta Anaesthesiol Scand. 2022;66:265-272. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |