Published online Apr 6, 2023. doi: 10.12998/wjcc.v11.i10.2123
Peer-review started: December 28, 2022
First decision: February 8, 2023
Revised: February 22, 2023
Accepted: March 15, 2023
Article in press: March 15, 2023
Published online: April 6, 2023
Processing time: 92 Days and 16.5 Hours
Hemodynamical evaluation of a coronary artery lesion is an important diagnostic step to assess its functional impact. Fractional flow reserve (FFR) received a class IA recommendation from the European Society of Cardiology for the assessment of angiographically moderate stenosis. FFR evaluation of coronary artery disease offers improvement of the therapeutic strategy, deferring unnecessary procedures for lesions with a FFR > 0.8, improving patients' management and clinical outcome. Post intervention, an optimal FFR > 0.9 post stenting should be reached and > 0.8 post drug eluting balloons. Non-hyperemic pressure ratio measure
Core Tip: Fractional flow reserve and non-hyperemic indices are the cornerstone for optimal percutaneous interventions. In this extensive review we discuss their rationale of use, indications guidelines, benefits and pitfalls. The comprehensive use of coronary artery physiology for the guidance of percutaneous interventions may be beneficial for every interventional cardiologist. Hence, we aimed to make a clear statement of physiology-guided percutaneous interventions to enhance coronary artery revascularization techniques.
- Citation: Boutaleb AM, Ghafari C, Ungureanu C, Carlier S. Fractional flow reserve and non-hyperemic indices: Essential tools for percutaneous coronary interventions. World J Clin Cases 2023; 11(10): 2123-2139
- URL: https://www.wjgnet.com/2307-8960/full/v11/i10/2123.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i10.2123
Coronary artery angiography remains the cornerstone for coronary artery disease (CAD) assessment confirming stenoses or occlusions of epicardial coronary arteries. These are often subjectively estimated by the operator who visually evaluates the percentage of intraluminal narrowing of the artery. Quantitative coronary angiography improves this guess work, optimizing devices sizing by accurately measuring the length and reference diameter of coronary stenoses[1]. However, this anatomic evaluation remains often insufficient requiring adjunctive information provided by a functional assessment. The presence of inducible ischemia in patients with CAD has been associated with adverse clinical outcome with risk stratification based on the extent of myocardial ischemia[2,3]. However, this was not confirmed in the more recent Ischemia trial where the severity of ischemia was not associated with an increased risk after adjustment for CAD severity[4].
Medical treatment is efficient in relieving anginal symptoms related to myocardial ischemia while revascularization improves downstream coronary blood flow and therefore relieves myocardial cells from the changes related to anaerobic metabolism[5].
Although current guidelines have implemented non-invasive stress testing prior to percutaneous interventions (PCI), the frequency of upstream testing remains low[6].
Fractional flow reserve (FFR) is used during coronary artery angiography to directly measure the pressure drop across an epicardial stenosis[7]. It is nowadays considered as the gold standard for the detection of myocardial ischemia and is recommended by the ESC 2018 myocardial revascularization guidelines[8]. This invasive diagnostic tool is the current standard of care for the functional assessment of lesion severity in patients with intermediate grade stenosis (40%-90%) without evidence of ischemia. FFR-guided PCI has been shown to be superior to angiographic guided PCI as well as its safety for PCI deferral of non-functionally significant stenosis[9-11].
With the increasing use of physiological assessment for CAD, new pressure-derived indices have emerged to guide PCI and to overcome some of the issues of FFR. Non-hyperemic pressure ratios (NHPR) are now an integral part of most current pressure wire systems and are widely used in the majority of catheterization laboratories. These indices evaluate coronary artery functional severity over either the diastolic phase or the whole cardiac cycle. A good correlation with FFR was found for the instantaneous wave free ratio (iFR), the first NHPR developed, with an 80% approximative accuracy[12-14]. Numerous NHPR are now available and are numerically equivalent with a common threshold[15].
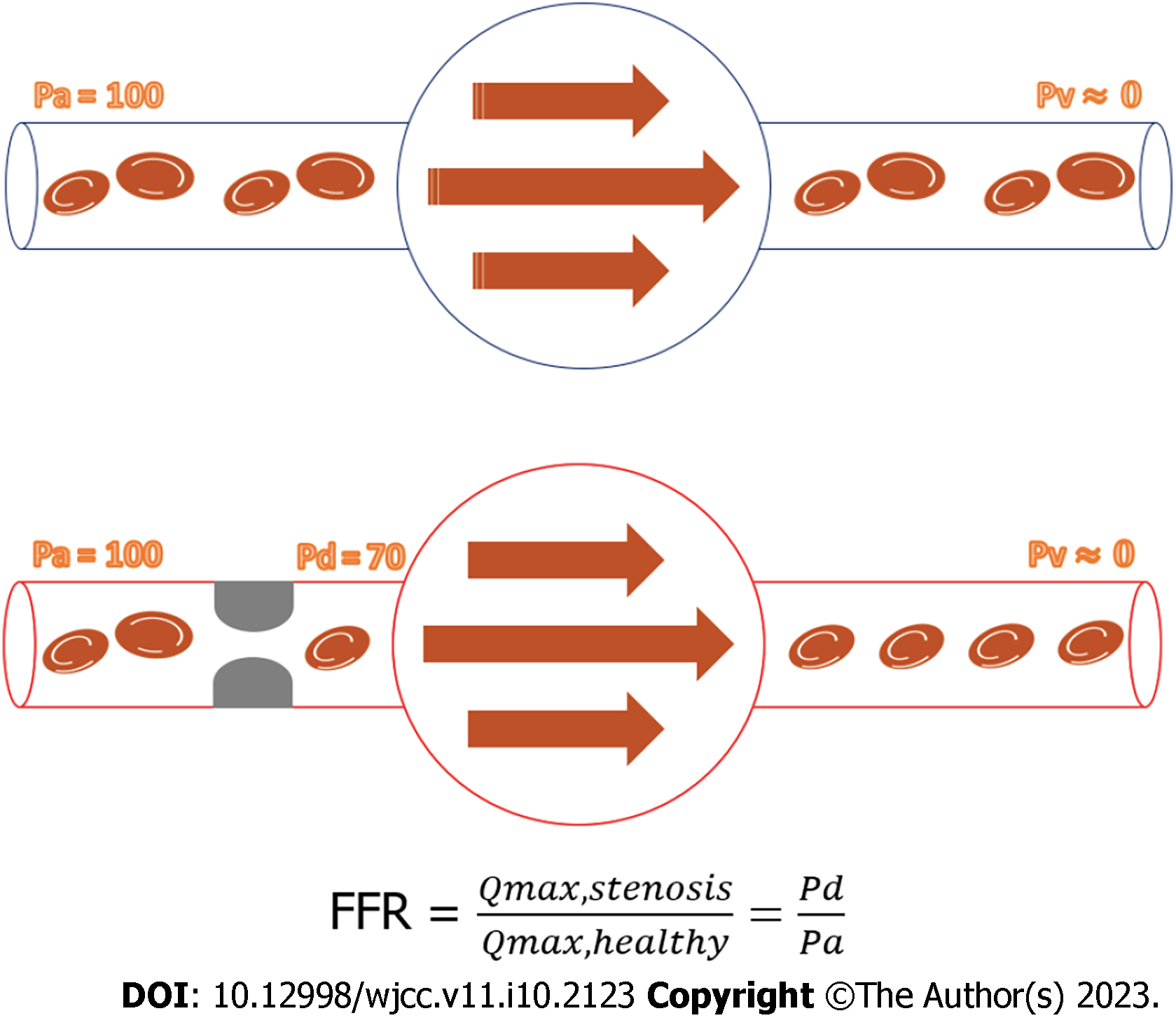
Fractional flow reserve is defined as the maximal achievable blood flow in the presence of an epicardial coronary stenosis divided by the maximum flow in the same healthy vessel if there was no obstructive epicardial disease[16]. It can be estimated by the simplified ratio of the coronary artery pressure downstream an epicardial stenosis over the aortic pressure during maximal hyperemia, taking into account the central venous pressure. Hence, FFR estimates the percentage of maximal blood flow limited by the presence of an epicardial stenosis. It is expressed by the following relationship, considering a constant and minimal coronary arterial bed resistance: FFR = (Pd-Pv)/(Pa-Pv), where Pd is the pressure recorded downstream the epicardial stenosis, Pa is the aortic pressure and Pv the central venous pressure (Figure 1).
Maximal hyperemia is generally obtained by intravenous or intracoronary perfusion of adenosine[17]. Other agents such as Regadenoson or Papaverine can also be used[18,19]. The coronary vasodilator agent dose and side effects perfusion are presented in Table 1[20].
| Agent | Dose | Side effects | |
| Adenosine | Intravenous | 140 µg/kg/min IV; > 40 µg RCA; > 80 µg LCA | Transient AV block, chest pain, shortness of breath, hypotension, headache, flushing |
| Intracoronary | |||
| Regadenoson | 400 µg singe bolus central or peripheral IV | Rhythm or conduction abnormalities, rare gastrointestinal side effects, less frequent chest pain and dyspnea | |
| Papaverine | 10-12 mg in RCA; 15-20 mg in LCA | Abdominal symptoms, headache, flushing of face, increase in heart rate, QTc prolongation, ventricular tachyarrhythmias | |
Intracoronary Adenosine is the preferred vasodilator agent inducing a quick (5-10 s) response to maximal hyperemia, however it may cause transient atrioventricular block, chest discomfort and shortness of breath and is contraindicated in patients presenting with chronic pulmonary obstructive disease. A more stable hyperemia is achieved using an intravenous perfusion[21]. Regadenoson (Rapiscan) is a selective agonist of the receptor A2 of adenosine with a 10-fold lower affinity for the A1 adenosine receptor. Its injection produces coronary vasodilatation and increases coronary blood flow. Given its selectivity for the A2 receptor, cardiac conduction sides effects are less frequently observed and is generally well tolerated in patients with chronic obstructive pulmonary disease (COPD)[22,23]. A good correlation between both agents has been reported in multiple trials[24,25].
The first proposed FFR threshold was 0.75. The issue of a grey-zone decision between 0.75 and 0.80 has been solved recommending now a threshold of 0.80[26]. An accuracy of 90% was reported in the FAME trial[10]. The revascularization between 0.75 and 0.80 remains debatable, but should be considered depending on the potential major adverse cardiovascular events (MACE) rates of the patients and coronary artery stenosis localization[27].
The cutoff threshold values have been validated in multiple trials comparing non-invasive measurements to FFR associated to the reversal of the presence of ischemia after PCI[7,26,28,29].
The majority of PCI are performed using 6 French guiding catheters (GC). All FFR systems are with a low profile allowing to use already 5 Fr GC but care must then be taken to optimize the quality of phasic pressure recordings, flushing the catheter with saline solution.
FFR systems are based either on a piezoelectrical or an optical sensor. Both types of pressure sensors generate a membrane deflection through the pressure, inducing either an electrical charge or a phase delay in a reflected light beam.
These systems have been well validated, with a reduction in pressure drift reported with the optical method[30,31]. Moreover, the latest versions of optical pressure guidewires enable its use as a workhorse guidewire for PCI by disconnecting and reconnecting the system.
The first step consists of zeroing the fluid-filled aortic pressure and the FFR pressure system ex vivo to the atmospheric one, ideally at the level of the right atrium. The pressure wire is then advanced few millimeters beyond the tip of the GC. Both pressure curves are equalized with the introducer needle off the Y connector[32]. Contrast may dampen the catheter waveform pressure, hence flushing the system with saline is mandatory before pressure measurements.
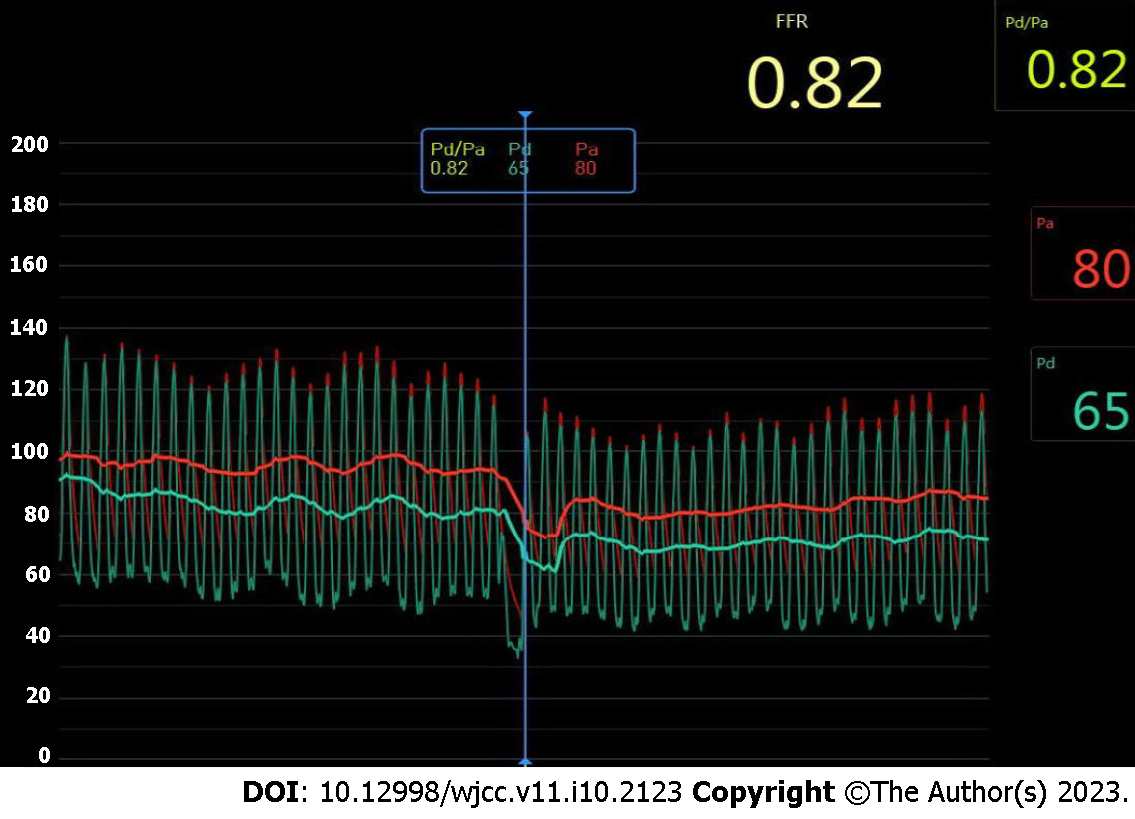
After intracoronary administration of isosorbide dinitrate, FFR and NHPR can be measured with the wire advanced at least 3 vessels diameters distal to the stenosis. In case of multiple stenosis and diffuse disease, a recording of the pressure during a pull back of the wire identifies spots with significant pressure changes where a PCI might be useful. At the end, a possible drift (significant if > 3 mmHg) of the FFR system is carried out[33]. Figure 2 represents the display screen of the POLARIS monitor (Boston Scientific, Marlborough, MA, United States) using the COMET™ wire, showing a non-significant FFR value of 0.82.
Several intracoronary pressure systems are currently available on the market: WaveWire™ (Philips Inc, Eindhoven, the Netherlands), COMET™ (Boston Scientific, Marlborough, MA, USA), PressureWire™ (St. Jude/Abbott, St. Paul, MN, United States), NAVVUS RXi® (ACIST Medical Systems, Inc, Eden Prairie, MN), TruePhysio™ (Insight Lifetech) and OptoWire Deux (Opsens medical, Quebec, Canada) with fewer drift[31]. The COMET trial comparing the COMET™ and the PressureWire™ found similar results in terms of safety and performance[34]. The RIPCORD 2 trial was a large prospective, multicenter study where investigators used the COMET™ wire to evaluate a FFR-guided revascularization strategy in patients presenting with stable CAD or NSTE-ACS.
In most guidewires, the pressure sensor is usually located at the proximal part of the radiopaque tip. In the case of the NAVVUS RXi®, the pressure sensor is located 5 mm above the distal tip of the microcatheter.
Conventional pressure wires have generally less torque control, flexibility and crossing ability than workhorse or specialized guidewires. Therefore, the NAVVUS RXi® and the TruePhysio™ are microcatheters to be used with any workhorse wire to overcome these issues, with debatable opinions. In vitro assessment of the novel 0.014’’ OptoWire™ showed improved pushability, steerability and torquability in comparison with regular PCI wires, offering reliable pre and post PCI hemodynamic assessment[35].
Myocardial ischemia is defined as a lack of coronary blood flow with electrical, functional, metabolic and structural consequences for the myocardium. The imbalance between oxygen supply and myocardial oxygen need is the central point of interest that should be improved with optimal medical therapy and/or coronary artery revascularization[36].
The FFR was first introduced by Pijls et al[7] who demonstrated the initial threshold of 0.75 demonstrating reversal of non-invasive stress tests after performing PCI.
The DEFER trial investigated the appropriateness of not stenting a functionally non-significant coronary stenosis and showed the safety to defer PCI when the FFR was > 0.75[37].
Tonino et al[10] showed in the FAME I trial that FFR-guided PCI is associated with fewer MACE and less resource utilization compared with angiography-guided PCI in patient with multivessel disease using a threshold of 0.80.
De Bruyne et al[9] proved in the FAME II trial that the addition of FFR measurements to optimal medical therapy in patients presenting stable CAD is superior to best medical therapy alone.
In the context of non ST-elevation acute coronary syndrome (NSTE-ACS) FFR guided revascularization of non-culprit lesions may be used during the index procedure to evaluate the need for further revascularization therapy[38].
The meta-analysis of Knuuti et al[39] evaluated the performance of non-invasive stress test to rule-in and rule-out significant CAD choosing as reference invasive coronary angiography with FFR measurements. They concluded that imaging methods are clearly superior to stress electrocardiogram. Functional imaging techniques including positron emission tomography, cardiac magnetic resonance and single-photon emission computerized tomography offer the best diagnostic performance even if the anatomical correlation is poor as shown in Table 2.
| Test | Anatomically Significant CAD | Functionally significant CAD | ||
| Specificity (95%CI) | Sensitivity (95%CI) | Specificity (95%CI) | Sensitivity (95%CI) | |
| Stress ECG | 62 (54-69) | 58 (46-69) | 73 (55-86) | 68 (60-75) |
| Stress echo | 82 (72-89) | 85 (80-89) | ||
| CCTA | 78 (67-86) | 97 (93-99) | 53 (37-68) | 93 (89-96) |
| SPECT | 70 (63-76) | 87 (83-90) | 83 (71-90) | 73 (62-82) |
| PET | 85 (78-90) | 90 (78-96) | 85 (81-88) | 89 (82-93) |
| Stress CMR | 80 (69-88) | 90 (83-94) | 87 (83-91) | 89 (85-92) |
All these major trials support the class IA recommendation to assess the hemodynamic relevance of intermediate coronary artery disease by FFR and as class IIB in multivessel disease evaluation[8]. In fact, both the European and American guidelines state that patients undergoing coronary angiography without prior ischemia assessment should have invasive hemodynamic test (FFR or NHPR) to optimize the revascularization strategy[40].
The theoretical value of FFR is 1 in a normal healthy epicardial coronary artery. FFR decreases with increasing epicardial stenosis severity. This index is not influenced by systemic hemodynamics and remain stable in case of systemic pressure, heart rate and left ventricular contractility changes[41]. In addition, Johnson et al[42] found a 98% reproducibility rates. Among its other advantages, FFR takes into account the contribution of collaterals by reflecting both antegrade and retrograde blood flow during maximal hyperemia[43].
Considering the critical prognostic importance of left main (LM) stem disease and its difficult angiographic assessment, the revascularization of intermediate LM should be guided by FFR or intravascular imaging[44]. Generally, LM disease is frequently associated with other stenoses of the coronary artery tree. FFR could therefore stratify patients for surgical or percutaneous revascularization taking into account downstream lesion implication[45,46].
FFR can guide revascularization of non-culprit lesions in patients presenting with acute coronary syndromes (ACS). The FAME trial demonstrated that the benefits of FFR-guided PCI were similar in patients with unstable angina or NSTEMI and chronic coronary syndrome[47]. However, controversial findings were reported by Liou et al[48] advocating in depth assessment of FFR guided PCI in ACS context.
Tandem lesions are defined by two 50% or more stenoses separated by an angiographically normal segment. In serial lesions, FFR measurements of all stenoses is carried out, followed by a slow pull back of the FFR wire under steady state hyperemia and fluoroscopic view to determine the exact drop of pressure localization[48]. These cases remain challenging to interpret considering the interaction of downstream coronary artery stenosis: the FFR value of the proximal lesion might be overestimated and equations to predict FFR for each stenosis have been reported using the coronary wedge pressure, measured with an inflated balloon[45-46,49]. For a tandem lesion, NHPR are easier and more precise in assessing the respective significance of each stenosis. Table 3 summarizes the major trials evaluating the outcomes of FFR in intermediate coronary lesions of LM and non LM lesions[9-11,50-53].
| Author or Study | Single or MVD CAD | Study design | FFR value defining ischemia | No. of patients | Survival % | Event-free survival % | Follow up, mo | Primary outcome rate % |
| DEFER[37] | Single | Randomized, prospective, multicenter | 0.75 | 91/144 | 93/91 | 80/63 | 60 | |
| FAME[10] | MVD | Randomized, prospective, multicenter | 0.80 | 509/1005 | 37/509 | 73 | 12 | |
| Hamilos et al[50] | LM | Prospective, single center | 0.80 | 136/73 | 89.8/85.4 | 74.2/82.8 | 35 | |
| FLOWER MI[51] | MVD | Randomized, prospective, multicenter | 0.80 | 590/1171 | 5.5/4.2 | 98.5/98.3 | 12.36 | |
| PHANTOM[52] | NR | Prospective, multicenter | 0.75 | 39/21 | 100/100 | 97/76 | 12 | |
| FAME 2[9] | Single + MVD | Randomized, prospective, multicenter | 0.80 | 447/1220 | 60 | 8.7 | ||
| FAME 3[53] | MVD | Randomized, prospective, multicenter | 0.80 | 757/1500 | 12 | 10.6 |
In an otherwise healthy vessel with only a short stenosis, the FFR after stenting should theoretically revert to 1. However, atherosclerosis affects diffusely most of the coronary vessels and FFR values will therefore be affected by a mix of potential sub-optimal stenting (e.g. a remaining sub-expansion of the stent in a calcified lesion), issues at the edges (e.g. a dissection), or a remaining stenosis outside the stented segment. In the DKCRUSH VII registry the only statistically significant predictor of target vessel failure (TVF) at 3-year was a post-PCI FFR < 0.88[54]. Hwang et al[55] reported an optimal cut-off post-PCI FFR predicting TVF of < 0.82, associated with a 10.9% rate of events while it was only 2.5% when the post-PCI FFR was ≥ 0.82 in the left anterior descending artery (LAD). Similarly, a FFR post PCI < 0.88 was associated with 8% of TVF, but 1.9% with a FFR ≥ 0.88 in a non-LAD vessel. Conversely, Diletti et al[56] more recently reported among 1000 patients that a sub-optimal FFR < 0.90 was measured in 38% of the treated vessels. At 2-year follow-up, in a patient level analysis, there were no increase in major adverse cardiac events. A vessel level analysis demonstrated a significant doubling of target vessel revascularization (P = 0.030) and a trend towards a higher stent thrombosis rate [HR, 2.89 (95%CI, 0.88–9.48), P = 0.08]. After balloon angioplasty without stenting, favorable outcomes have been associated with a final FFR ranging between 0.90 and 0.75. An optimal FFR cut-off of 0.80 was reported for drug eluting balloon angioplasty without stenting[57].
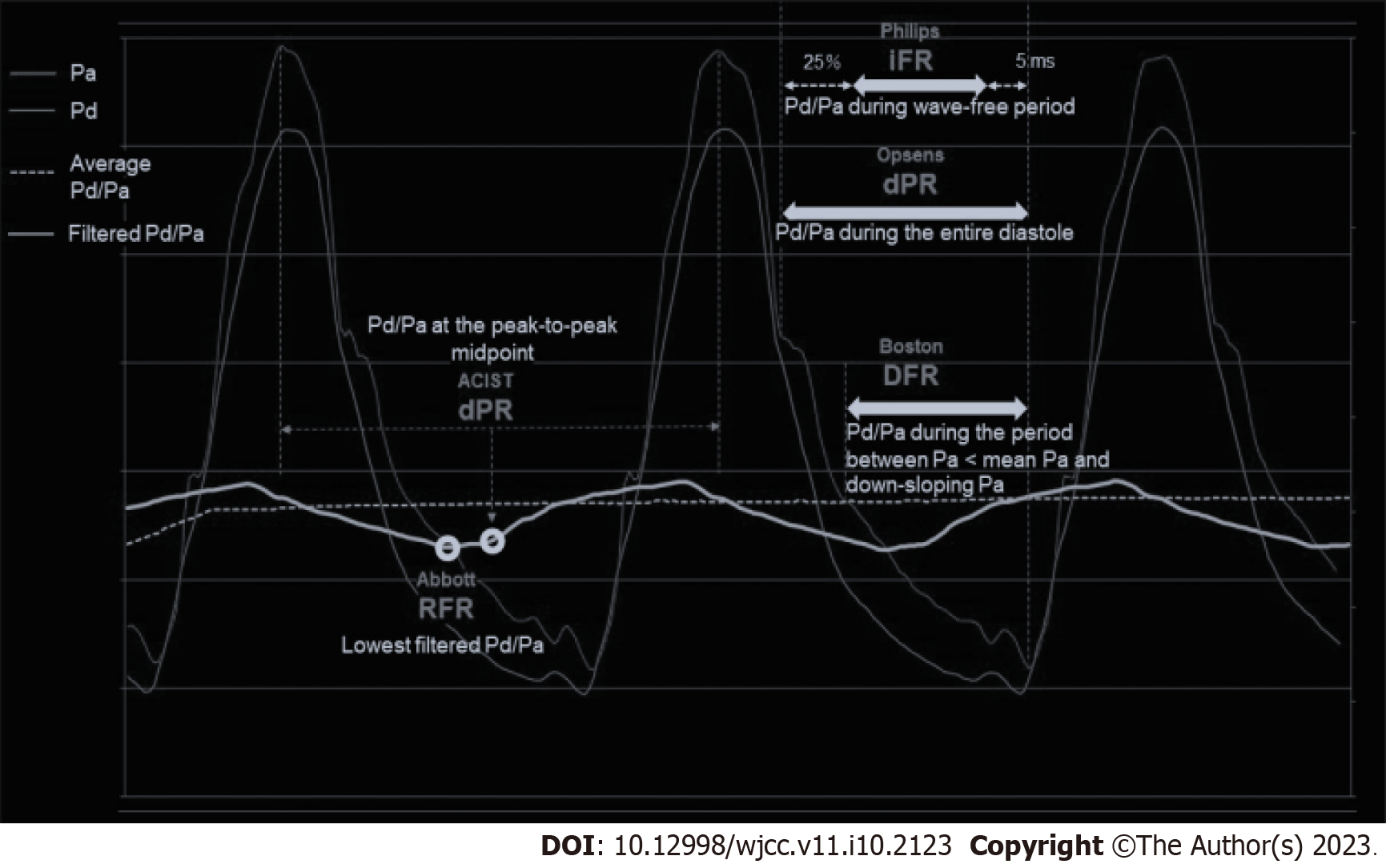
FFR has become the gold standard invasive diagnostic tool to guide coronary artery revascularization. Understanding the mechanisms of fractional flow measurement is essential before performing any physiological assessment of CAD. Coronary resistance fluctuates during the cardiac cycle in a phasic pattern, due to the compression and decompression of the myocardium. A specific period, not affected by forward and backward effects, named instantaneous wave free period, has been identified[58]. The iFR concept relies on the theory that intracoronary resistance is naturally low and constant during this wave free period allowing to compute a reliable pressure index. This particular cardiac window has been defined in the ADVISE (Adenosine vasodilator independent stenosis evaluation) trial to start 25% after the start of the diastolic phase and ends 5 ms before the systolic phase start. iFR is measured without the need of hyperemia/adenosine and the 0.89 threshold corresponding to ischemia has been validated vs FFR measurements[59].
The ADVISE study assessed the accuracy of iFR compared with FFR. A close correlation was found between both indices with good diagnostic performance (receiver-operating characteristic (ROC) area of 93%, at FFR< 0.8) with specificity, sensitivity, negative and positive predictive values respectively at 91%, 85%, 85% and 91%[59]. In the CLARIFY study, an agreement of 92% between iFR and FFR values was found. In the four lesions with mismatch between the two indices, the hyperemic stenosis resistance was correlated either to FFR or iFR[60]. In addition, the SWEDEHEART trial highlighted the noninferiority of iFR-guided PCI compared with a FFR-guided PCI[12]. The same finding were reported in the DEFINE FLAIR trial with a reduction in adverse procedural symptoms related to adenosine infusion and shorter time of procedures[13]. A better agreement between iFR than FFR and coronary flow velocity reserve was reported in JUSTIFY-CFR. In 4% of their non-significant iFR values (> 0.90) a significant drop in FFR value (< 0.75) was noted[61]. Multiple trials have reported an approximative 80% accuracy between iFR and FFR[14,59,62].
The ADIVSE II trial reported a strong correlation between iFR and FFR and identified 0.89 as the optimal iFR threshold with an area under the ROC curve of 0.90. This cut-off correctly classified 82.5% of coronary artery stenoses with a sensitivity and specificity of respectively 73% and 87.8%. The hybrid iFR-FFR approach based on a iFR treatment value below 0.85 and deferral above 0.94 showed a better correlation rate of 94.2%[63].
Using respectively 0.89 and 0.80 as cutoffs for iFR and FFR, Modi reported a 25% discordance rate, which is in line with the previous studies. This discrepancy can be lowered to 11% using respectively 0.86 and 0.75 cutoffs[64]. Table 4 presents these different studies.
| Trial | Study population | Mean FFR value +/-SD | Mean iFR-value +/-SD | iFR cut-off | P value for non-inferiority | Correlation | Sensitivity % | Specificity % |
| DEFINE-FLAIR[13] | 2492 | 0.83 +/-0.09 | 0.91+/- 0.09 | 0.89 | < 0.001 | |||
| iFR SWEDEHEART[12] | 2037 | 0.82 +/-0.10 | 0.91+/- 0.10 | 0.89 | 0.007 | |||
| ADVISE study[59] | 131 | 0.72+/- 0.2 | 0.83 | 0.9 (P < 0.001) | 85 | 91 | ||
| VERIFY[65] | 206 | 0.83 | 0.67 | 54 (49-60) | 96 (95-99) | |||
| JUSTIFY-CFR[61] | 186 | 0.74+/- 0.17 | 0.81+/- 0.21 | 0.89 | 0.68 0.60-0.76 | 73 | 74 |
In contrast, the VERIFY trial revealed only a moderate overall correlation between iFR and FFR with a weak correlation in the clinically important range for decision making, between 0.60 and 0.90. The authors do not recommend the use of iFR for clinical decision making for PCI[65]. We will also personally guide our clinical decisions to revascularize or defer an intervention in our patients using the results of their FFR that we will always assess in any doubtful result of a NHPR in a grey zone between 0.84 and 0.94.
With the increasing use of invasive hemodynamic assessment of CAD severity, novel NHPR have been proposed by different manufacturers. These indices have been compared to iFR and are summarized in Table 5.
| Acronym | Full name | Manufacturer | Method | Threshold | Evidence |
| iFR | Instantaneous wave-free ratio | Philips Heathcare | Mean five Pd/Pa during the WFP | 0.89 | DEFINE FLAIR[13], SWEDEHAEART TRIAL[12] |
| RFR | Resting full-cycle ratio | Abbott | Lowest value of Pd/Pa across the whole cardiac cycle | 0.89 | VALIDATE RFR[68], RE-VALIDATE RFR[69] |
| DFR | Diastolic hyperemia-free ratio | Boston Scientific | Average 5 consecutive cardiac cycles Pd/Pa ratio over the approximateda diastolic period | 0.89 | Comparison of different diastolic resting indexes to iFR[15] |
| dPR | Diastolic pressure ratio | ACIST/Opsens Medical | Average 5 beats Pd/Pa ratio at the pressure peak-to-peak midpoint | 0.89 | Diastolic pressure ratio: New approach and validation vs the iFR[69] |
| Resting Pd/Pa | Not proprietary technology | Pd/Pa averaged over the entire cardiac cycle | 0.91 |
Figure 3 shows the different periods used for NHPR calculation over the cardiac cycle. These indices can be separated into two groups, the ones using the whole cycle and the others using calculating diastolic indices.
The retrospective VALIDATE study showed the diagnostic comparability between resting full-cycle ratio (RFR) and iFR. It is important to note that 12.2% of RFR were measured outside the diastolic phase with a predominant discrepancy rate between both measurements when iFR was > 0.93. This difference was found to be more important in waveforms acquired in right coronary arteries (6.5%)[66]. The REVALIDATE RFR study had the same purpose using a prospective analysis methodology showing a 97.8% overall diagnostic accuracy, sensitivity and specificity. Thus, RFR is an alternative diagnostic tool for the guidance of PCI reducing time and cost procedures by avoiding hyperemic agents need[67].
The diastolic Pressure Ratio study found a strong linear correlation between the diastolic pressure ratio and iFR (r = 0,997, P < 0.001) on one hand and FFR (r = 0.77, P < 0.001) on the other[68,69]. The dPR measured with the Optowire (Opsens, Quebec City, Quebec, Canada) showed strong correlation with other NHPR (RFR, iFR) in the RPG study with an r = 0.84[70].
A novel Opsens dPR algorithm using the mean of 4 consecutive beats Pd/Pa ratio at diastole was highly correlated to iFR (R2 = 0.99) with high accuracy to predict iFR at 95.6%, with a sensitivity of 93.5% and specificity of 96.7%[71]. As reviewed by De Maria et al[72] among the major advantages of the resting indices is the hyperemia drug free evaluation.
The cut-off for these non-hyperemic indices is 0.89 with a proportion of discordance ranging between 15% to 20% particularly in proximal vessel subtending large myocardial areas[58]. Theses resting indices were not evaluated in randomized controlled trials but have only been compared in studies to support their clinical use[15,73].
Following the validation studies described above, NHPR share similar indications than FFR but additional specific clinical scenario’s have been investigated. For example, a retrospective study reported how to decide to perform a PCI with iFR in non-culprit lesions of patients presenting with ACS[74].
The iLITRO study found an agreement of 80% between iFR and FFR in left main intermediate stenosis. Intravascular ultrasound imaging (IVUS) was used in cases with discrepancy, using the threshold of 6 mm2 as a cut-off for revascularization. In discordant FFR/iFR measurements, IVUS showed an MLA < 6 mm2 in 69% of the cases of FFR+/iFR-, while in FFR-/iFR+ cases, 40% only had an MLA< 6 mm2. The patients deferred from revascularization with discordant hemodynamic measurements and a negative IVUS evaluation had a low incidence of MACE at follow-up, leading to an iFR-guided LMCA revascularization strategy combined with IVUS in the discordant cases (hybrid approach)[44].
An iFR pullback enables the operator to predict an iFR value after the treatment of a selected stenosis[75]. The comparison of functional PCI results using NHPR in the REFINE-RPG study showed comparable results between RFR, dPR and iFR while reducing the total length of treated lesions using NHPR pullback PCI-guided strategy compared to angiography-guided PCI. The correlation between predicted and actual post PCI NHPR was high (r = 0.73) with no difference among NHPR groups[70].
In multiple scenarios, the use of FFR or iFR alone may not suffice to take the proper therapeutic decision. Hence, a hybrid approach is useful in some clinical scenarios. Using FFR as the gold standard, NHPR has an average accuracy of 80% resulting in stenoses misclassifications. A combined physiological assessment without adenosine in the first line demonstrated a reduction of the need of intracoronary vasodilator in more than half of the CAD patients in need of functional assessment. Furthermore, the use a 0.86-0.93 cut-off range for iFR improve its positive and negative predictive value to respectively 92% and 91%[61].
The technical aspect of PCI optimization involves proper use of diagnostic and guidance imaging, equipment, techniques, and antithrombotic therapy to achieve optimal patient outcomes. Recently, the value of low post PCI FFR has been linked to poor outcomes related to suboptimal stent placement or remaining disease[76]. In this specific setting, intravascular imaging may be helpful to understand the mechanisms behind inadequate functional improvement. The FFR REACT trial used a post PCI threshold of 0.90 and randomized 291 patients for IVUS or traditional standard of care. This strategy resulted in the improvement of post PCI FFR in 20% of the vessels with a trend for lower target vessel revascularization in the IVUS guided arm (P = 0.06)[77].
Intermediate left main coronary artery lesions can be evaluated more thoroughly with either intracoronary imaging (using IVUS) or physiological assessment (using FFR pressure wire). These invasive tools can provide more detailed information on the anatomical severity and hemodynamic significance of the lesions to be discussed in the heart team to improve the decision of the revascularization strategy and its optimization. Park has reviewed in detail the role of pre and post PCI IVUS and FFR[78]. The ILITRO-EPIC07 study showed that FFR and iFR had an average agreement of 80%, while IVUS was more likely to match FFR’s classification of stenosis significance in discrepant cases. Therefore, from a clinician's viewpoint, the best approach for determining if revascularization can be safely deferred in intermediate left main coronary artery lesions is a combination of IVUS and physiology[44].
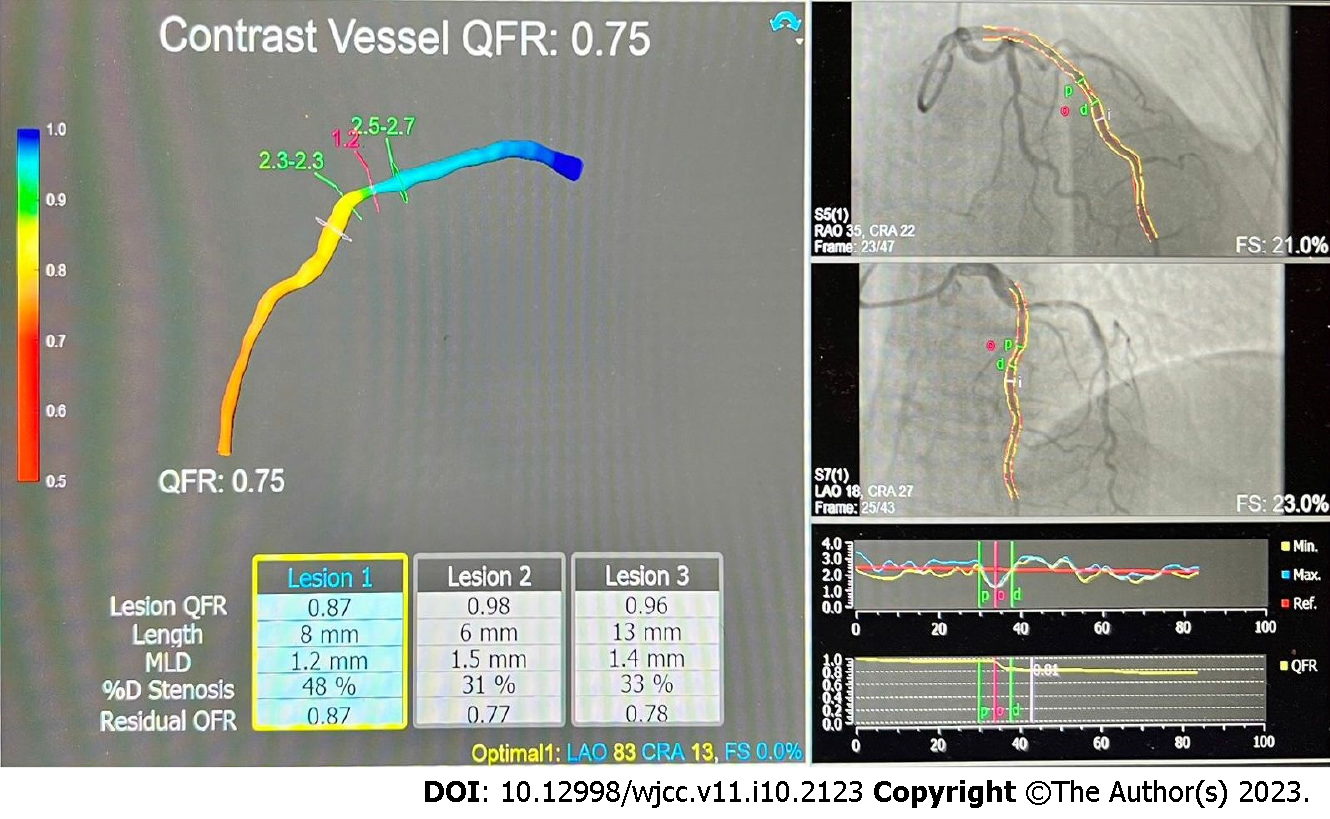
More recently, physiological coronary assessment has been evaluated with virtual tools computing the flow ratio. Quantitative flow ratio (QFR) is based on the analysis of two angiography views 25° apart at least with minimal superposition between the main and side branches. The QFR uses a mathematical model, the three-dimensional reconstruction and coronary contrast product progression in order to determine the coronary flow. The FAVOR trial was the first to assess this technique, and showed significant correlation with FFR (r = 0.77; P < 0.001) with an 80% accuracy using an FFR threshold of 0.80[79]. Along with these promising results, the FAVOR II Europe-Japan Study found that QFR is superior to angiographic assessment of intermediate coronary artery stenosis using FFR as standard reference[80]. Kasinadhuni et al[81] showed that QFR has a superior diagnostic performance compared to the benchmark FFR in evaluating intermediate lesions physiologically outperforming the anatomical percentage diameter stenosis with a significant difference (P < 0.001).
QFR and FFR have excellent consistency and alignment. The ability of QFR to determine the functional impact of coronary disease has been demonstrated in the meta-analysis and systematic review of Cortés et al[82]. This new tool, and a similar one, vFFR implemented in the CAAS Worstation (Pie Medical Imaging, Maastricht, the Netherlands) are independent predictors for MACE with beneficial effect of PCI for low QFR/vFFR values[83,84].
Finally non-invasively, The SYNTAX III REVOLUTION study showed that using computed coronary tomography angiography to decide between CABG and PCI for coronary artery disease, based on the predicted four-year mortality as indicated by the SYNTAX score II, resulted in high agreement (93%) in treatment decisions, with an "almost perfect kappa" of 0.82, compared to decisions made using ICA[85,86].
FFR-Computed Tomography (FFR-CT) allows for the measurement of flow across the entire coronary artery bed unlike the usual method which assess the functional significance of a specific coronary stenosis and its upstream segments[20,87].
These new concepts open new tracks for a better risk stratification and prognosis prediction of patients presenting with coronary artery disease. Their use is increasing in the context of stable CAD for the guidance of percutaneous interventions, but some authors have demonstrated the prognostic implication of a post interventional pan-coronary-QFR evaluation in patients with ACS[88].
We hypothesize that further improvement of these techniques might help the physicians to discriminate atherosclerotic NSTE-ACS from type II Myocardial infarction and myocardial infarction with non-obstructive coronary disease.
A hybrid approach, with a combined use of both anatomical (IVUS) and functional methods to determine the significance of coronary stenosis, could provide a more comprehensive and accurate assessment enabling the operators to take more targeted and individualized decisions. However, the hybrid approach does require additional imaging and testing, which can increase the cost and complexity of the evaluation. Using QFR and IVUS simultaneously, or FFR-CT before, seems appealing as they combine an invasive evaluation with a noninvasive one, lowering the cost.
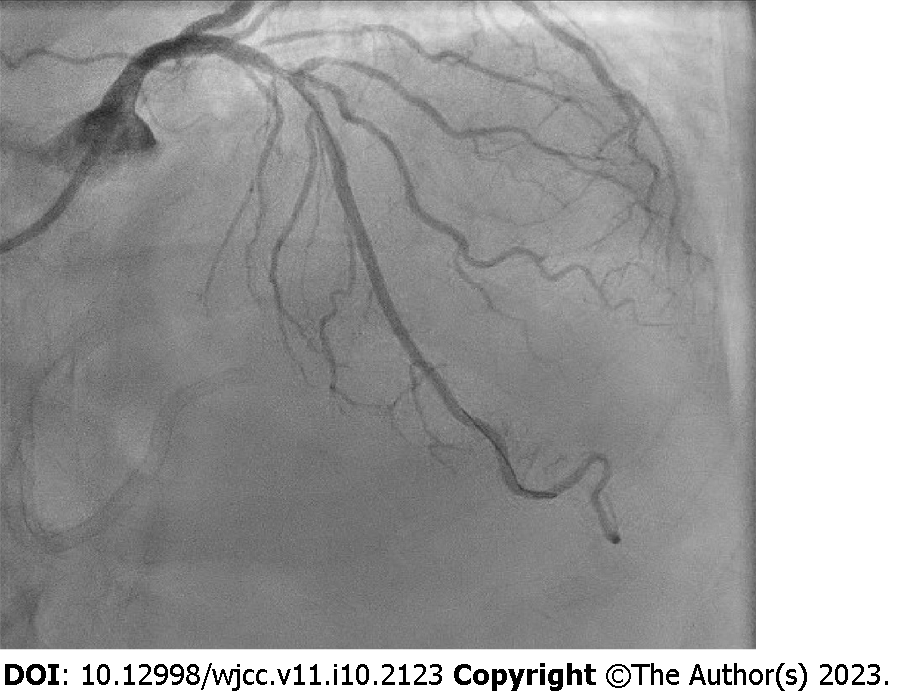
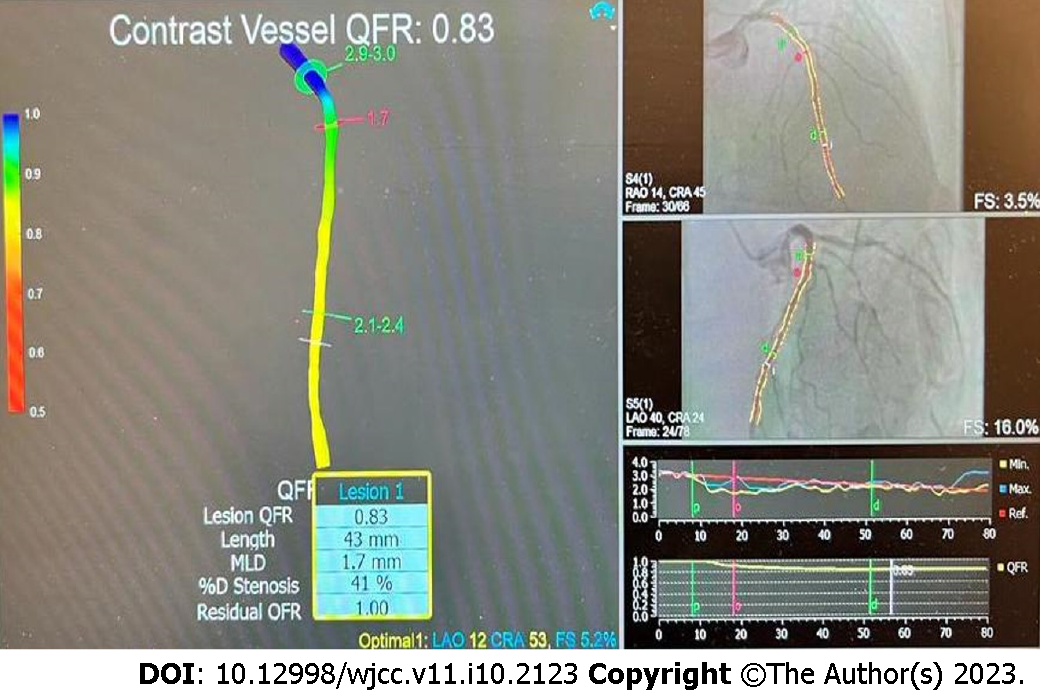
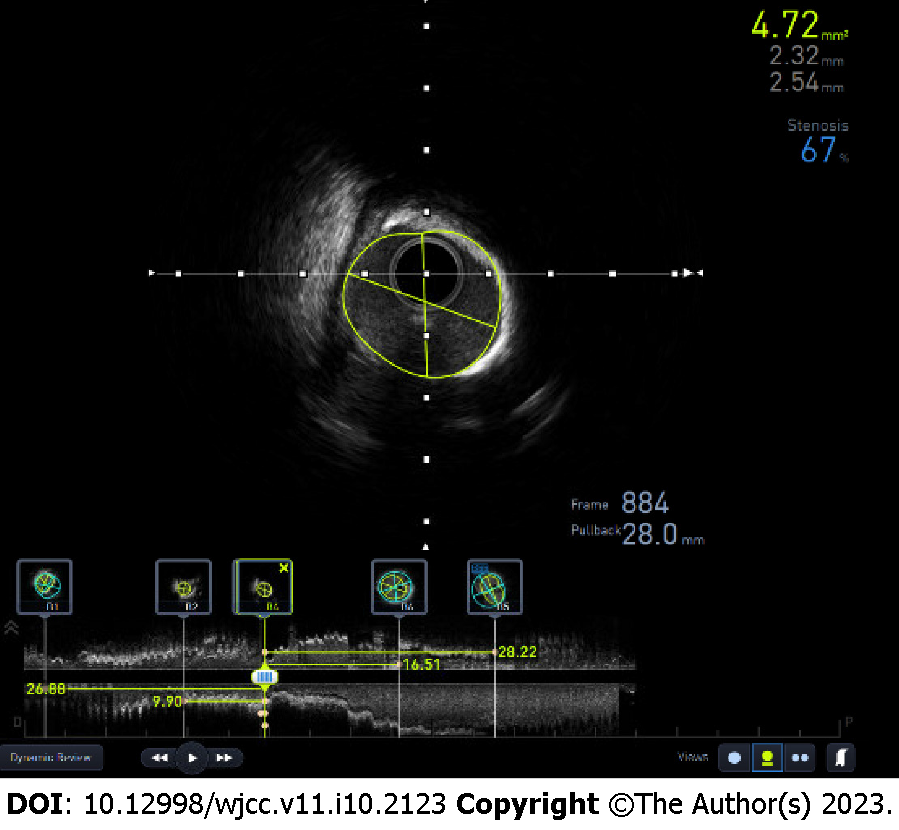
We will illustrate this concept in two recent clinical cases we performed. A stable patient with suspected myocardial ischemia after dobutamine stress test had a coronary angiogram demonstrating a LAD with a moderate long lesion in the proximal and mid part (Figure 4) that was evaluated by QFR at 0.83 (Figure 5). Regarding these intermediate values, a complementary IVUS evaluation was performed (Figure 6) showing a non-significant lesion with a minimal lumen area of was 4.7 mm².
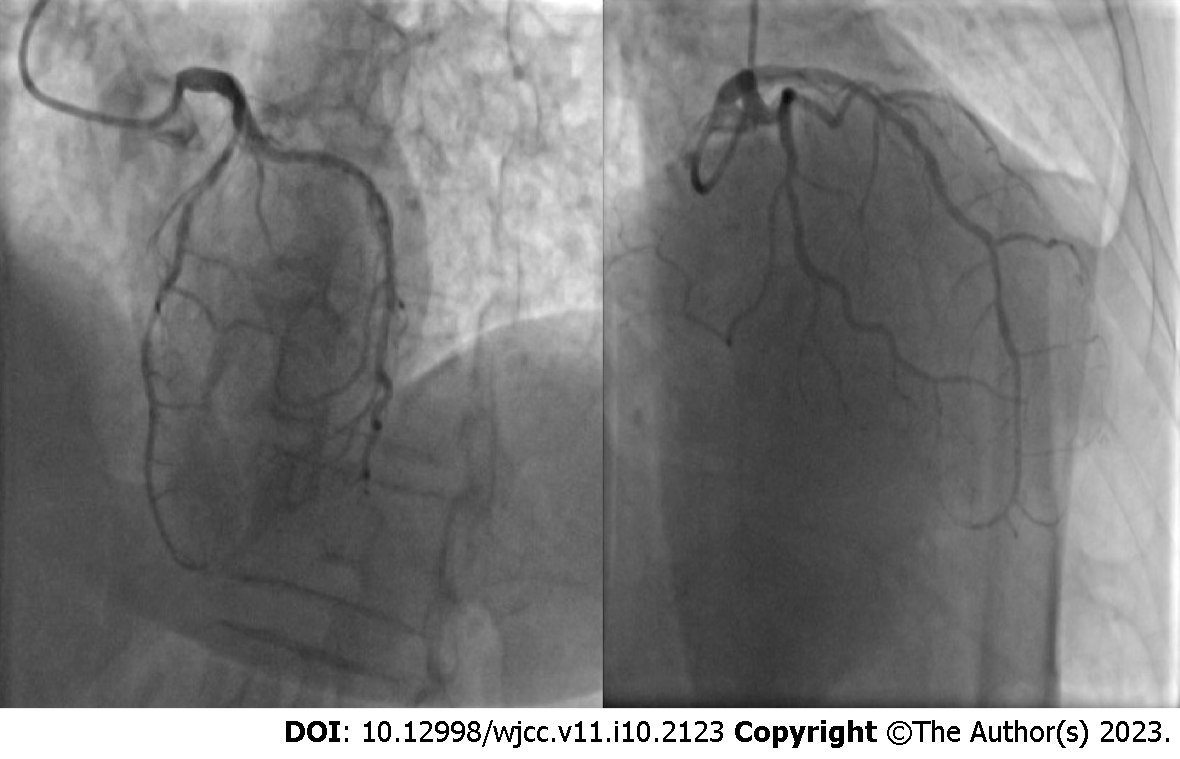
The good agreement between QFR and FFR is illustrated in another case summarized on Figures 7 to 9. On the coronary angiogram of a patient with recurrent clinical symptoms, we noticed multiple intermediate lesions in the proximal, mid, and distal LAD (Figure 7).
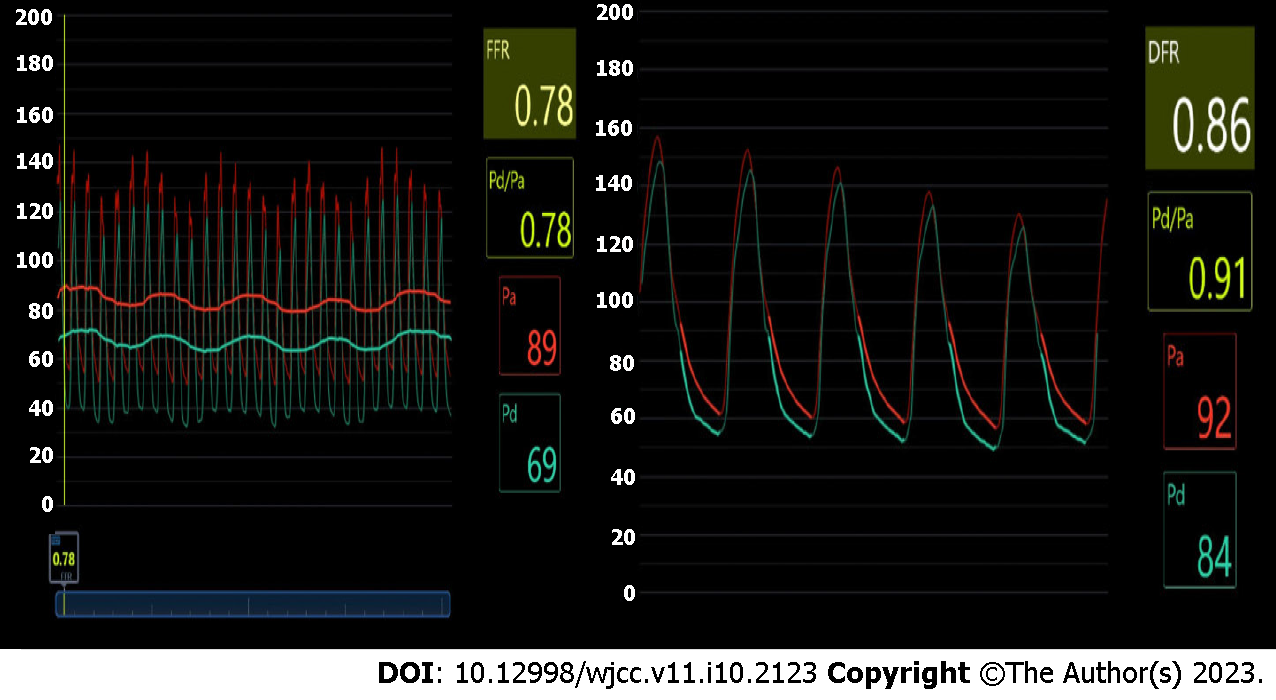
The FFR was positive in the distal LAD at 0.78 and also the DFR was 0.86 (Figure 8). The QFR of 0.75 was well aligned with these measurements (Figure 9). The relationship between QFR and clinical outcomes, and its cost-effectiveness, requires further prospective validation.
Invasive hemodynamic assessment of coronary artery disease is a critical component of a patient evaluation. Today, fractional flow reserve and non-hyperemic pressure ratios guide the physician in optimizing coronary artery tree revascularization therapy. Their development has been backed up by extensive validation studies and physiology and they obtained a class I indication during PCI. The possibility to assess the spatial distribution of epicardial resistances and determine the focal or diffuse characteristics of coronary artery disease is crucial for revascularization therapy decisions. In the case of a difference between the measured fractional flow reserve and any non-hyperemic pressure ratio, we recommend following the results of the FFR and defer an intervention when its value is superior to 0.80.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: Belgium
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Batta A, India; Hong X, China S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Suzuki N, Asano T, Nakazawa G, Aoki J, Tanabe K, Hibi K, Ikari Y, Kozuma K. Clinical expert consensus document on quantitative coronary angiography from the Japanese Association of Cardiovascular Intervention and Therapeutics. Cardiovasc Interv Ther. 2020;35:105-116. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 79] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 2. | Beller GA, Zaret BL. Contributions of nuclear cardiology to diagnosis and prognosis of patients with coronary artery disease. Circulation. 2000;101:1465-1478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 254] [Cited by in RCA: 256] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 3. | Hachamovitch R, Berman DS, Shaw LJ, Kiat H, Cohen I, Cabico JA, Friedman J, Diamond GA. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: differential stratification for risk of cardiac death and myocardial infarction. Circulation. 1998;97:535-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 848] [Cited by in RCA: 813] [Article Influence: 30.1] [Reference Citation Analysis (0)] |
| 4. | Reynolds HR, Shaw LJ, Min JK, Page CB, Berman DS, Chaitman BR, Picard MH, Kwong RY, O'Brien SM, Huang Z, Mark DB, Nath RK, Dwivedi SK, Smanio PEP, Stone PH, Held C, Keltai M, Bangalore S, Newman JD, Spertus JA, Stone GW, Maron DJ, Hochman JS. Outcomes in the ISCHEMIA Trial Based on Coronary Artery Disease and Ischemia Severity. Circulation. 2021;144:1024-1038. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 190] [Article Influence: 47.5] [Reference Citation Analysis (0)] |
| 5. | Jennings RB, Reimer KA. The cell biology of acute myocardial ischemia. Annu Rev Med. 1991;42:225-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 221] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 6. | Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck-Brentano C, Prescott E, Storey RF, Deaton C, Cuisset T, Agewall S, Dickstein K, Edvardsen T, Escaned J, Gersh BJ, Svitil P, Gilard M, Hasdai D, Hatala R, Mahfoud F, Masip J, Muneretto C, Valgimigli M, Achenbach S, Bax JJ; ESC Scientific Document Group. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41:407-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2791] [Cited by in RCA: 4488] [Article Influence: 897.6] [Reference Citation Analysis (0)] |
| 7. | Pijls NH, De Bruyne B, Peels K, Van Der Voort PH, Bonnier HJ, Bartunek J Koolen JJ, Koolen JJ. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med. 1996;334:1703-1708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1629] [Cited by in RCA: 1611] [Article Influence: 55.6] [Reference Citation Analysis (0)] |
| 8. | Neumann FJ, Sousa-Uva M. 'Ten commandments' for the 2018 ESC/EACTS Guidelines on Myocardial Revascularization. Eur Heart J. 2019;40:79-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 240] [Article Influence: 40.0] [Reference Citation Analysis (0)] |
| 9. | De Bruyne B, Pijls NH, Kalesan B, Barbato E, Tonino PA, Piroth Z, Jagic N, Möbius-Winkler S, Rioufol G, Witt N, Kala P, MacCarthy P, Engström T, Oldroyd KG, Mavromatis K, Manoharan G, Verlee P, Frobert O, Curzen N, Johnson JB, Jüni P, Fearon WF; FAME 2 Trial Investigators. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med. 2012;367:991-1001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1837] [Cited by in RCA: 1987] [Article Influence: 152.8] [Reference Citation Analysis (0)] |
| 10. | Tonino PA, De Bruyne B, Pijls NH, Siebert U, Ikeno F, van' t Veer M, Klauss V, Manoharan G, Engstrøm T, Oldroyd KG, Ver Lee PN, MacCarthy PA, Fearon WF; FAME Study Investigators. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360:213-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2974] [Cited by in RCA: 3050] [Article Influence: 190.6] [Reference Citation Analysis (0)] |
| 11. | Zimmermann FM, Ferrara A, Johnson NP, van Nunen LX, Escaned J, Albertsson P, Erbel R, Legrand V, Gwon HC, Remkes WS, Stella PR, van Schaardenburgh P, Bech GJ, De Bruyne B, Pijls NH. Deferral vs. performance of percutaneous coronary intervention of functionally non-significant coronary stenosis: 15-year follow-up of the DEFER trial. Eur Heart J. 2015;36:3182-3188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 315] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 12. | Götberg M, Christiansen EH, Gudmundsdottir IJ, Sandhall L, Danielewicz M, Jakobsen L, Olsson SE, Öhagen P, Olsson H, Omerovic E, Calais F, Lindroos P, Maeng M, Tödt T, Venetsanos D, James SK, Kåregren A, Nilsson M, Carlsson J, Hauer D, Jensen J, Karlsson AC, Panayi G, Erlinge D, Fröbert O; iFR-SWEDEHEART Investigators. Instantaneous Wave-free Ratio versus Fractional Flow Reserve to Guide PCI. N Engl J Med. 2017;376:1813-1823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 581] [Cited by in RCA: 702] [Article Influence: 87.8] [Reference Citation Analysis (1)] |
| 13. | Davies JE, Sen S, Dehbi HM, Al-Lamee R, Petraco R, Nijjer SS, Bhindi R, Lehman SJ, Walters D, Sapontis J, Janssens L, Vrints CJ, Khashaba A, Laine M, Van Belle E, Krackhardt F, Bojara W, Going O, Härle T, Indolfi C, Niccoli G, Ribichini F, Tanaka N, Yokoi H, Takashima H, Kikuta Y, Erglis A, Vinhas H, Canas Silva P, Baptista SB, Alghamdi A, Hellig F, Koo BK, Nam CW, Shin ES, Doh JH, Brugaletta S, Alegria-Barrero E, Meuwissen M, Piek JJ, van Royen N, Sezer M, Di Mario C, Gerber RT, Malik IS, Sharp ASP, Talwar S, Tang K, Samady H, Altman J, Seto AH, Singh J, Jeremias A, Matsuo H, Kharbanda RK, Patel MR, Serruys P, Escaned J. Use of the Instantaneous Wave-free Ratio or Fractional Flow Reserve in PCI. N Engl J Med. 2017;376:1824-1834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 679] [Cited by in RCA: 713] [Article Influence: 89.1] [Reference Citation Analysis (0)] |
| 14. | Jeremias A, Maehara A, Généreux P, Asrress KN, Berry C, De Bruyne B, Davies JE, Escaned J, Fearon WF, Gould KL, Johnson NP, Kirtane AJ, Koo BK, Marques KM, Nijjer S, Oldroyd KG, Petraco R, Piek JJ, Pijls NH, Redwood S, Siebes M, Spaan JAE, van 't Veer M, Mintz GS, Stone GW. Multicenter core laboratory comparison of the instantaneous wave-free ratio and resting Pd/Pa with fractional flow reserve: the RESOLVE study. J Am Coll Cardiol. 2014;63:1253-1261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 279] [Article Influence: 23.3] [Reference Citation Analysis (0)] |
| 15. | Van't Veer M, Pijls NHJ, Hennigan B, Watkins S, Ali ZA, De Bruyne B, Zimmermann FM, van Nunen LX, Barbato E, Berry C, Oldroyd KG. Comparison of Different Diastolic Resting Indexes to iFR: Are They All Equal? J Am Coll Cardiol. 2017;70:3088-3096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 163] [Article Influence: 27.2] [Reference Citation Analysis (0)] |
| 16. | Pijls NH, van Son JA, Kirkeeide RL, De Bruyne B, Gould KL. Experimental basis of determining maximum coronary, myocardial, and collateral blood flow by pressure measurements for assessing functional stenosis severity before and after percutaneous transluminal coronary angioplasty. Circulation. 1993;87:1354-1367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 807] [Cited by in RCA: 798] [Article Influence: 24.9] [Reference Citation Analysis (0)] |
| 17. | Mohdnazri SR, Keeble TR, Sharp AS. Fractional Flow Reserve: Does a Cut-off Value add Value? Interv Cardiol. 2016;11:17-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Warisawa T, Cook CM, Akashi YJ, Davies JE. Past, Present and Future of Coronary Physiology. Rev Esp Cardiol (Engl Ed). 2018;71:656-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 19. | van Nunen LX, Lenders GD, Schampaert S, van 't Veer M, Wijnbergen I, Brueren GR, Tonino PA, Pijls NH. Single bolus intravenous regadenoson injection versus central venous infusion of adenosine for maximum coronary hyperaemia in fractional flow reserve measurement. EuroIntervention. 2015;11:905-913. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 20. | Shantouf RS, Mehra A. Coronary fractional flow reserve. AJR Am J Roentgenol. 2015;204:W261-W265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Layland J, Carrick D, Lee M, Oldroyd K, Berry C. Adenosine: physiology, pharmacology, and clinical applications. JACC Cardiovasc Interv. 2014;7:581-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 215] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 22. | Andrikopoulou E, Hage FG. Adverse effects associated with regadenoson myocardial perfusion imaging. J Nucl Cardiol. 2018;25:1724-1731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Thomas GS, Tammelin BR, Schiffman GL, Marquez R, Rice DL, Milikien D, Mathur V. Safety of regadenoson, a selective adenosine A2A agonist, in patients with chronic obstructive pulmonary disease: A randomized, double-blind, placebo-controlled trial (RegCOPD trial). J Nucl Cardiol. 2008;15:319-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 83] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 24. | Arumugham P, Figueredo VM, Patel PB, Morris DL. Comparison of intravenous adenosine and intravenous regadenoson for the measurement of pressure-derived coronary fractional flow reserve. EuroIntervention. 2013;8:1166-1171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 25. | Nair PK, Marroquin OC, Mulukutla SR, Khandhar S, Gulati V, Schindler JT, Lee JS. Clinical utility of regadenoson for assessing fractional flow reserve. JACC Cardiovasc Interv. 2011;4:1085-1092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 58] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 26. | Pijls NH, Van Gelder B, Van der Voort P, Peels K, Bracke FA, Bonnier HJ, el Gamal MI. Fractional flow reserve. A useful index to evaluate the influence of an epicardial coronary stenosis on myocardial blood flow. Circulation. 1995;92:3183-3193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 589] [Cited by in RCA: 553] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 27. | Adjedj J, Flore V, Gioia GD, Ferrara A, Pellicano M, Toth G, Wijns W, de Bruyne B, Barbato E. 0043: FFR Gray zone and clinical outcome. Arch Cardiovasc Dis Suppl. 2016;8:8-9. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 28. | Watkins S, McGeoch R, Lyne J, Steedman T, Good R, McLaughlin MJ, Cunningham T, Bezlyak V, Ford I, Dargie HJ, Oldroyd KG. Validation of magnetic resonance myocardial perfusion imaging with fractional flow reserve for the detection of significant coronary heart disease. Circulation. 2009;120:2207-2213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 152] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 29. | Bartunek J, Van Schuerbeeck E, de Bruyne B. Comparison of exercise electrocardiography and dobutamine echocardiography with invasively assessed myocardial fractional flow reserve in evaluation of severity of coronary arterial narrowing. Am J Cardiol. 1997;79:478-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 63] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 30. | Fearon WF, Chambers JW, Seto AH, Sarembock IJ, Raveendran G, Sakarovitch C, Yang L, Desai M, Jeremias A, Price MJ; ACIST-FFR Study Investigators. ACIST-FFR Study (Assessment of Catheter-Based Interrogation and Standard Techniques for Fractional Flow Reserve Measurement). Circ Cardiovasc Interv. 2017;10:e005905. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 31. | Cottens D, Ferdinande B, Polad J, Vrolix M, Ameloot K, Hendrickx I, Poels E, Maeremans J, Dens J. FFR pressure wire comparative study for drift: piezo resistive versus optical sensor. Am J Cardiovasc Dis. 2022;12:42-52. [PubMed] |
| 32. | Vranckx P, Cutlip DE, McFadden EP, Kern MJ, Mehran R, Muller O. Coronary pressure-derived fractional flow reserve measurements: recommendations for standardization, recording, and reporting as a core laboratory technique. Proposals for integration in clinical trials. Circ Cardiovasc Interv. 2012;5:312-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 33. | Pijls NH, Bruyne BD. Fractional Flow Reserve, Coronary Pressure Wires, and Drift. Circ J. 2016;80:1704-1706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 34. | Stables RH, Elguindy M, Kemp I, Nicholas Z, Mars C, Mullen L, Curzen N. A randomised controlled trial to compare two coronary pressure wires using simultaneous measurements in human coronary arteries: the COMET trial. EuroIntervention. 2019;14:e1578-e1584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 35. | Ulacia P, Rimac G, Lalancette S, Belleville C, Mongrain R, Plante S, Rusza Z, Matsuo H, Bertrand OF. A novel fiber-optic based 0.014″ pressure wire: Designs of the OptoWire™, development phases, and the O(2) first-in-man results. Catheter Cardiovasc Interv. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 36. | Heusch G. Myocardial Ischemia: Lack of Coronary Blood Flow or Myocardial Oxygen Supply/Demand Imbalance? Circ Res. 2016;119:194-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 51] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 37. | Pijls NH, van Schaardenburgh P, Manoharan G, Boersma E, Bech JW, van't Veer M, Bär F, Hoorntje J, Koolen J, Wijns W, de Bruyne B. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER Study. J Am Coll Cardiol. 2007;49:2105-2111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1099] [Cited by in RCA: 1164] [Article Influence: 64.7] [Reference Citation Analysis (0)] |
| 38. | Collet JP, Thiele H, Barbato E, Barthélémy O, Bauersachs J, Bhatt DL, Dendale P, Dorobantu M, Edvardsen T, Folliguet T, Gale CP, Gilard M, Jobs A, Jüni P, Lambrinou E, Lewis BS, Mehilli J, Meliga E, Merkely B, Mueller C, Roffi M, Rutten FH, Sibbing D, Siontis GCM; ESC Scientific Document Group. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021;42:1289-1367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2569] [Cited by in RCA: 3115] [Article Influence: 778.8] [Reference Citation Analysis (0)] |
| 39. | Knuuti J, Ballo H, Juarez-Orozco LE, Saraste A, Kolh P, Rutjes AWS, Jüni P, Windecker S, Bax JJ, Wijns W. The performance of non-invasive tests to rule-in and rule-out significant coronary artery stenosis in patients with stable angina: a meta-analysis focused on post-test disease probability. Eur Heart J. 2018;39:3322-3330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 349] [Article Influence: 58.2] [Reference Citation Analysis (0)] |
| 40. | Fezzi S, Huang J, Lunardi M, Ding D, Ribichini FL, Tu S, Wijns W. Coronary physiology in the catheterisation laboratory: an A to Z practical guide. AsiaIntervention. 2022;8:86-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 41. | de Bruyne B, Bartunek J, Sys SU, Pijls NH, Heyndrickx GR, Wijns W. Simultaneous coronary pressure and flow velocity measurements in humans. Feasibility, reproducibility, and hemodynamic dependence of coronary flow velocity reserve, hyperemic flow versus pressure slope index, and fractional flow reserve. Circulation. 1996;94:1842-1849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 298] [Cited by in RCA: 281] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 42. | Johnson NP, Johnson DT, Kirkeeide RL, Berry C, De Bruyne B, Fearon WF, Oldroyd KG, Pijls NHJ, Gould KL. Repeatability of Fractional Flow Reserve Despite Variations in Systemic and Coronary Hemodynamics. JACC Cardiovasc Interv. 2015;8:1018-1027. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 81] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 43. | De Bruyne B, Sarma J. Fractional flow reserve: a review: invasive imaging. Heart. 2008;94:949-959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 132] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 44. | Rodriguez-Leor O, de la Torre Hernández JM, García-Camarero T, García Del Blanco B, López-Palop R, Fernández-Nofrerías E, Cuellas Ramón C, Jiménez-Kockar M, Jiménez-Mazuecos J, Fernández Salinas F, Gómez-Lara J, Brugaletta S, Alfonso F, Palma R, Gómez-Menchero AE, Millán R, Tejada Ponce D, Linares Vicente JA, Ojeda S, Pinar E, Fernández-Pelegrina E, Morales-Ponce FJ, Cid-Álvarez AB, Rama-Merchan JC, Molina Navarro E, Escaned J, Pérez de Prado A. Instantaneous Wave-Free Ratio for the Assessment of Intermediate Left Main Coronary Artery Stenosis: Correlations With Fractional Flow Reserve/Intravascular Ultrasound and Prognostic Implications: The iLITRO-EPIC07 Study. Circ Cardiovasc Interv. 2022;15:861-871. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 45. | Yong AS, Daniels D, De Bruyne B, Kim HS, Ikeno F, Lyons J, Pijls NH, Fearon WF. Fractional flow reserve assessment of left main stenosis in the presence of downstream coronary stenoses. Circ Cardiovasc Interv. 2013;6:161-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 67] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 46. | De Bruyne B, Pijls NH, Heyndrickx GR, Hodeige D, Kirkeeide R, Gould KL. Pressure-derived fractional flow reserve to assess serial epicardial stenoses: theoretical basis and animal validation. Circulation. 2000;101:1840-1847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 182] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 47. | Sels JW, Tonino PA, Siebert U, Fearon WF, Van't Veer M, De Bruyne B, Pijls NH. Fractional flow reserve in unstable angina and non-ST-segment elevation myocardial infarction experience from the FAME (Fractional flow reserve versus Angiography for Multivessel Evaluation) study. JACC Cardiovasc Interv. 2011;4:1183-1189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 139] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 48. | Liou KP, Ooi SM, Hoole SP, West NEJ. Fractional flow reserve in acute coronary syndrome: a meta-analysis and systematic review. Open Heart. 2019;6:e000934. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 49. | Liu LY, Wu HP, Lin PL. Fractional Flow Reserve Assessment of a Significant Coronary Stenosis Masked by a Downstream Serial Lesion. Case Rep Cardiol. 2016;2016:1987238. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 50. | Hamilos M, Muller O, Cuisset T, Ntalianis A, Chlouverakis G, Sarno G, Nelis O, Bartunek J, Vanderheyden M, Wyffels E, Barbato E, Heyndrickx GR, Wijns W, De Bruyne B. Long-term clinical outcome after fractional flow reserve-guided treatment in patients with angiographically equivocal left main coronary artery stenosis. Circulation. 2009;120:1505-1512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 294] [Cited by in RCA: 282] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 51. | Puymirat E, Cayla G, Simon T, Steg PG, Montalescot G, Durand-Zaleski I, le Bras A, Gallet R, Khalife K, Morelle JF, Motreff P, Lemesle G, Dillinger JG, Lhermusier T, Silvain J, Roule V, Labèque JN, Rangé G, Ducrocq G, Cottin Y, Blanchard D, Charles Nelson A, De Bruyne B, Chatellier G, Danchin N; FLOWER-MI Study Investigators. Multivessel PCI Guided by FFR or Angiography for Myocardial Infarction. N Engl J Med. 2021;385:297-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 223] [Article Influence: 55.8] [Reference Citation Analysis (0)] |
| 52. | Costa MA, Sabate M, Staico R, Alfonso F, Seixas AC, Albertal M, Crossman A, Angiolillo DJ, Zenni M, Sousa JE, Macaya C, Bass TA. Anatomical and physiologic assessments in patients with small coronary artery disease: final results of the Physiologic and Anatomical Evaluation Prior to and After Stent Implantation in Small Coronary Vessels (PHANTOM) trial. Am Heart J. 2007;153:296.e1-296.e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 46] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 53. | Fearon WF, Zimmermann FM, De Bruyne B, Piroth Z, van Straten AHM, Szekely L, Davidavičius G, Kalinauskas G, Mansour S, Kharbanda R, Östlund-Papadogeorgos N, Aminian A, Oldroyd KG, Al-Attar N, Jagic N, Dambrink JE, Kala P, Angerås O, MacCarthy P, Wendler O, Casselman F, Witt N, Mavromatis K, Miner SES, Sarma J, Engstrøm T, Christiansen EH, Tonino PAL, Reardon MJ, Lu D, Ding VY, Kobayashi Y, Hlatky MA, Mahaffey KW, Desai M, Woo YJ, Yeung AC, Pijls NHJ; FAME 3 Investigators. Fractional Flow Reserve-Guided PCI as Compared with Coronary Bypass Surgery. N Engl J Med. 2022;386:128-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 215] [Article Influence: 71.7] [Reference Citation Analysis (0)] |
| 54. | Li SJ, Ge Z, Kan J, Zhang JJ, Ye F, Kwan TW, Santoso T, Yang S, Sheiban I, Qian XS, Tian NL, Rab TS, Tao L, Chen SL. Cutoff Value and Long-Term Prediction of Clinical Events by FFR Measured Immediately After Implantation of a Drug-Eluting Stent in Patients With Coronary Artery Disease: 1- to 3-Year Results From the DKCRUSH VII Registry Study. JACC Cardiovasc Interv. 2017;10:986-995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 113] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 55. | Hwang D, Lee JM, Lee HJ, Kim SH, Nam CW, Hahn JY, Shin ES, Matsuo A, Tanaka N, Matsuo H, Lee SY, Doh JH, Koo BK. Influence of target vessel on prognostic relevance of fractional flow reserve after coronary stenting. EuroIntervention. 2019;15:457-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 56. | Diletti R, Masdjedi K, Daemen J, van Zandvoort LJC, Neleman T, Wilschut J, Den Dekker WK, van Bommel RJ, Lemmert M, Kardys I, Cummins P, de Jaegere P, Zijlstra F, Van Mieghem NM. Impact of Poststenting Fractional Flow Reserve on Long-Term Clinical Outcomes: The FFR-SEARCH Study. Circ Cardiovasc Interv. 2021;14:e009681. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 46] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 57. | Jeger RV, Eccleshall S, Wan Ahmad WA, Ge J, Poerner TC, Shin ES, Alfonso F, Latib A, Ong PJ, Rissanen TT, Saucedo J, Scheller B, Kleber FX; International DCB Consensus Group. Drug-Coated Balloons for Coronary Artery Disease: Third Report of the International DCB Consensus Group. JACC Cardiovasc Interv. 2020;13:1391-1402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 306] [Article Influence: 61.2] [Reference Citation Analysis (0)] |
| 58. | Michail M, Thakur U, Mehta O, Ramzy JM, Comella A, Ihdayhid AR, Cameron JD, Nicholls SJ, Hoole SP, Brown AJ. Non-hyperaemic pressure ratios to guide percutaneous coronary intervention. Open Heart. 2020;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 59. | Sen S, Escaned J, Malik IS, Mikhail GW, Foale RA, Mila R, Tarkin J, Petraco R, Broyd C, Jabbour R, Sethi A, Baker CS, Bellamy M, Al-Bustami M, Hackett D, Khan M, Lefroy D, Parker KH, Hughes AD, Francis DP, Di Mario C, Mayet J, Davies JE. Development and validation of a new adenosine-independent index of stenosis severity from coronary wave-intensity analysis: results of the ADVISE (ADenosine Vasodilator Independent Stenosis Evaluation) study. J Am Coll Cardiol. 2012;59:1392-1402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 485] [Cited by in RCA: 532] [Article Influence: 38.0] [Reference Citation Analysis (0)] |
| 60. | Sen S, Asrress KN, Nijjer S, Petraco R, Malik IS, Foale RA, Mikhail GW, Foin N, Broyd C, Hadjiloizou N, Sethi A, Al-Bustami M, Hackett D, Khan MA, Khawaja MZ, Baker CS, Bellamy M, Parker KH, Hughes AD, Francis DP, Mayet J, Di Mario C, Escaned J, Redwood S, Davies JE. Diagnostic classification of the instantaneous wave-free ratio is equivalent to fractional flow reserve and is not improved with adenosine administration. Results of CLARIFY (Classification Accuracy of Pressure-Only Ratios Against Indices Using Flow Study). J Am Coll Cardiol. 2013;61:1409-1420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 187] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 61. | Petraco R, van de Hoef TP, Nijjer S, Sen S, van Lavieren MA, Foale RA, Meuwissen M, Broyd C, Echavarria-Pinto M, Foin N, Malik IS, Mikhail GW, Hughes AD, Francis DP, Mayet J, Di Mario C, Escaned J, Piek JJ, Davies JE. Baseline instantaneous wave-free ratio as a pressure-only estimation of underlying coronary flow reserve: results of the JUSTIFY-CFR Study (Joined Coronary Pressure and Flow Analysis to Determine Diagnostic Characteristics of Basal and Hyperemic Indices of Functional Lesion Severity-Coronary Flow Reserve). Circ Cardiovasc Interv. 2014;7:492-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 141] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 62. | Park JJ, Petraco R, Nam CW, Doh JH, Davies J, Escaned J, Koo BK. Clinical validation of the resting pressure parameters in the assessment of functionally significant coronary stenosis; results of an independent, blinded comparison with fractional flow reserve. Int J Cardiol. 2013;168:4070-4075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 63. | Escaned J, Echavarría-Pinto M, Garcia-Garcia HM, van de Hoef TP, de Vries T, Kaul P, Raveendran G, Altman JD, Kurz HI, Brechtken J, Tulli M, Von Birgelen C, Schneider JE, Khashaba AA, Jeremias A, Baucum J, Moreno R, Meuwissen M, Mishkel G, van Geuns RJ, Levite H, Lopez-Palop R, Mayhew M, Serruys PW, Samady H, Piek JJ, Lerman A; ADVISE II Study Group. Prospective Assessment of the Diagnostic Accuracy of Instantaneous Wave-Free Ratio to Assess Coronary Stenosis Relevance: Results of ADVISE II International, Multicenter Study (ADenosine Vasodilator Independent Stenosis Evaluation II). JACC Cardiovasc Interv. 2015;8:824-833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 161] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 64. | Modi BN, Rahman H, Kaier T, Ryan M, Williams R, Briceno N, Ellis H, Pavlidis A, Redwood S, Clapp B, Perera D. Revisiting the Optimal Fractional Flow Reserve and Instantaneous Wave-Free Ratio Thresholds for Predicting the Physiological Significance of Coronary Artery Disease. Circ Cardiovasc Interv. 2018;11:e007041. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 65. | Berry C, van 't Veer M, Witt N, Kala P, Bocek O, Pyxaras SA, McClure JD, Fearon WF, Barbato E, Tonino PA, De Bruyne B, Pijls NH, Oldroyd KG. VERIFY (VERification of Instantaneous Wave-Free Ratio and Fractional Flow Reserve for the Assessment of Coronary Artery Stenosis Severity in EverydaY Practice): a multicenter study in consecutive patients. J Am Coll Cardiol. 2013;61:1421-1427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 181] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 66. | Svanerud J, Ahn JM, Jeremias A, van 't Veer M, Gore A, Maehara A, Crowley A, Pijls NHJ, De Bruyne B, Johnson NP, Hennigan B, Watkins S, Berry C, Oldroyd KG, Park SJ, Ali ZA. Validation of a novel non-hyperaemic index of coronary artery stenosis severity: the Resting Full-cycle Ratio (VALIDATE RFR) study. EuroIntervention. 2018;14:806-814. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 158] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 67. | Kumar G, Desai R, Gore A, Rahim H, Maehara A, Matsumura M, Kirtane A, Jeremias A, Ali Z. Real world validation of the nonhyperemic index of coronary artery stenosis severity-Resting full-cycle ratio-RE-VALIDATE. Catheter Cardiovasc Interv. 2020;96:E53-E58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 68. | Ligthart J, Masdjedi K, Witberg K, Mastik F, van Zandvoort L, Lemmert ME, Wilschut J, Diletti R, de Jaegere P, Zijlstra F, Kardys I, Van Mieghem NM, Daemen J. Validation of Resting Diastolic Pressure Ratio Calculated by a Novel Algorithm and Its Correlation With Distal Coronary Artery Pressure to Aortic Pressure, Instantaneous Wave-Free Ratio, and Fractional Flow Reserve. Circ Cardiovasc Interv. 2018;11:e006911. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 69. | Johnson NP, Li W, Chen X, Hennigan B, Watkins S, Berry C, Fearon WF, Oldroyd KG. Diastolic pressure ratio: new approach and validation vs. the instantaneous wave-free ratio. Eur Heart J. 2019;40:2585-2594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 70. | Omori H, Kawase Y, Mizukami T, Tanigaki T, Hirata T, Kikuchi J, Ota H, Sobue Y, Miyake T, Kawamura I, Okubo M, Kamiya H, Hirakawa A, Kawasaki M, Nakagawa M, Tsuchiya K, Suzuki Y, Ito T, Terashima M, Kondo T, Suzuki T, Escaned J, Matsuo H. Comparisons of Nonhyperemic Pressure Ratios: Predicting Functional Results of Coronary Revascularization Using Longitudinal Vessel Interrogation. JACC Cardiovasc Interv. 2020;13:2688-2698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 71. | Versaci F, Conte M, Van't Veer M, Lalancette S, Oldroyd K, Calcagno S, Biondi Zoccai G. A novel algorithm for the computation of the diastolic pressure ratio in the invasive assessment of the functional significance of coronary artery disease. Panminerva Med. 2021;63:206-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 72. | De Maria GL, Garcia-Garcia HM, Scarsini R, Hideo-Kajita A, Gonzalo López N, Leone AM, Sarno G, Daemen J, Shlofmitz E, Jeremias A, Tebaldi M, Bezerra HG, Tu S, Lemos PA, Ozaki Y, Dan K, Collet C, Banning AP, Barbato E, Johnson NP, Waksman R. Novel Indices of Coronary Physiology: Do We Need Alternatives to Fractional Flow Reserve? Circ Cardiovasc Interv. 2020;13:e008487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 49] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 73. | Lee JM, Choi KH, Park J, Hwang D, Rhee TM, Kim J, Kim HY, Jung HW, Cho YK, Yoon HJ, Song YB, Hahn JY, Nam CW, Shin ES, Doh JH, Hur SH, Koo BK. Physiological and Clinical Assessment of Resting Physiological Indexes. Circulation. 2019;139:889-900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 97] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 74. | Hidalgo F, Gonzalez-Manzanares R, Ojeda S, Benito-González T, Gutiérrez-Barrios A, De la Torre Hernández JM, Minguito-Carazo C, Izaga-Torralba E, Cabrera-Rubio I, Flores-Vergara G, de Lezo JS, Romero-Moreno M, de Prado AP, Pan M. Instantaneous wave-free ratio for guiding treatment of nonculprit lesions in patients with acute coronary syndrome: A retrospective study. Catheter Cardiovasc Interv. 2022;99:489-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 75. | Nijjer SS, Sen S, Petraco R, Mayet J, Francis DP, Davies JE. The Instantaneous wave-Free Ratio (iFR) pullback: a novel innovation using baseline physiology to optimise coronary angioplasty in tandem lesions. Cardiovasc Revasc Med. 2015;16:167-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 59] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 76. | Wolfrum M, Fahrni G, de Maria GL, Knapp G, Curzen N, Kharbanda RK, Fröhlich GM, Banning AP. Impact of impaired fractional flow reserve after coronary interventions on outcomes: a systematic review and meta-analysis. BMC Cardiovasc Disord. 2016;16:177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 77. | Neleman T, van Zandvoort LJC, Tovar Forero MN, Masdjedi K, Ligthart JMR, Witberg KT, Groenland FTW, Cummins P, Lenzen MJ, Boersma E, Nuis RJ, den Dekker WK, Diletti R, Wilschut J, Zijlstra F, Van Mieghem NM, Daemen J. FFR-Guided PCI Optimization Directed by High-Definition IVUS Versus Standard of Care: The FFR REACT Trial. JACC Cardiovasc Interv. 2022;15:1595-1607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 36] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 78. | Park S, Park SJ, Park DW. Percutaneous Coronary Intervention for Left Main Coronary Artery Disease: Present Status and Future Perspectives. JACC Asia. 2022;2:119-138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 25] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 79. | Tu S, Westra J, Yang J, von Birgelen C, Ferrara A, Pellicano M, Nef H, Tebaldi M, Murasato Y, Lansky A, Barbato E, van der Heijden LC, Reiber JHC, Holm NR, Wijns W; FAVOR Pilot Trial Study Group. Diagnostic Accuracy of Fast Computational Approaches to Derive Fractional Flow Reserve From Diagnostic Coronary Angiography: The International Multicenter FAVOR Pilot Study. JACC Cardiovasc Interv. 2016;9:2024-2035. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 429] [Article Influence: 53.6] [Reference Citation Analysis (0)] |
| 80. | Westra J, Andersen BK, Campo G, Matsuo H, Koltowski L, Eftekhari A, Liu T, Di Serafino L, Di Girolamo D, Escaned J, Nef H, Naber C, Barbierato M, Tu S, Neghabat O, Madsen M, Tebaldi M, Tanigaki T, Kochman J, Somi S, Esposito G, Mercone G, Mejia-Renteria H, Ronco F, Bøtker HE, Wijns W, Christiansen EH, Holm NR. Diagnostic Performance of In-Procedure Angiography-Derived Quantitative Flow Reserve Compared to Pressure-Derived Fractional Flow Reserve: The FAVOR II Europe-Japan Study. J Am Heart Assoc. 2018;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 141] [Cited by in RCA: 287] [Article Influence: 41.0] [Reference Citation Analysis (0)] |
| 81. | Kasinadhuni G, Batta A, Gawalkar AA, Budakoty S, Gupta A, Vijayvergiya R. Validity and correlation of quantitative flow ratio with fractional flow reserve for assessment of intermediate coronary lesions. Acta Cardiol. 2023;78:91-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 82. | Cortés C, Carrasco-Moraleja M, Aparisi A, Rodriguez-Gabella T, Campo A, Gutiérrez H, Julca F, Gómez I, San Román JA, Amat-Santos IJ. Quantitative flow ratio-Meta-analysis and systematic review. Catheter Cardiovasc Interv. 2021;97:807-814. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 83. | Hamaya R, Hoshino M, Kanno Y, Yamaguchi M, Ohya H, Sumino Y, Kanaji Y, Usui E, Murai T, Lee T, Yonetsu T, Hirao K, Kakuta T. Prognostic implication of three-vessel contrast-flow quantitative flow ratio in patients with stable coronary artery disease. EuroIntervention. 2019;15:180-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 84. | Masdjedi K, van Zandvoort LJC, Balbi MM, Gijsen FJH, Ligthart JMR, Rutten MCM, Lemmert ME, Wilschut JM, Diletti R, de Jaegere P, Zijlstra F, Van Mieghem NM, Daemen J. Validation of a three-dimensional quantitative coronary angiography-based software to calculate fractional flow reserve: the FAST study. EuroIntervention. 2020;16:591-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 54] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 85. | Andreini D, Modolo R, Katagiri Y, Mushtaq S, Sonck J, Collet C, De Martini S, Roberto M, Tanaka K, Miyazaki Y, Czapla J, Schoors D, Plass A, Maisano F, Kaufmann P, Orry X, Metzdorf PA, Folliguet T, Färber G, Diamantis I, Schönweiß M, Bonalumi G, Guglielmo M, Ferrari C, Olivares P, Cavallotti L, Leal I, Lindeboom W, Onuma Y, Serruys PW, Bartorelli AL; SYNTAX III REVOLUTION Investigators. Impact of Fractional Flow Reserve Derived From Coronary Computed Tomography Angiography on Heart Team Treatment Decision-Making in Patients With Multivessel Coronary Artery Disease: Insights From the SYNTAX III REVOLUTION Trial. Circ Cardiovasc Interv. 2019;12:e007607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 81] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 86. | Serruys PW, Hara H, Garg S, Kawashima H, Nørgaard BL, Dweck MR, Bax JJ, Knuuti J, Nieman K, Leipsic JA, Mushtaq S, Andreini D, Onuma Y. Coronary Computed Tomographic Angiography for Complete Assessment of Coronary Artery Disease: JACC State-of-the-Art Review. J Am Coll Cardiol. 2021;78:713-736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 97] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 87. | Nørgaard BL, Fairbairn TA, Safian RD, Rabbat MG, Ko B, Jensen JM, Nieman K, Chinnaiyan KM, Sand NP, Matsuo H, Leipsic J, Raff G. Coronary CT Angiography-derived Fractional Flow Reserve Testing in Patients with Stable Coronary Artery Disease: Recommendations on Interpretation and Reporting. Radiol Cardiothorac Imaging. 2019;1:e190050. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 81] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 88. | Erbay A, Penzel L, Abdelwahed YS, Klotsche J, Heuberger A, Schatz AS, Steiner J, Haghikia A, Sinning D, Fröhlich GM, Landmesser U, Stähli BE, Leistner DM. Prognostic Impact of Pancoronary Quantitative Flow Ratio Assessment in Patients Undergoing Percutaneous Coronary Intervention for Acute Coronary Syndromes. Circ Cardiovasc Interv. 2021;14:e010698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |