Published online Mar 26, 2022. doi: 10.12998/wjcc.v10.i9.2764
Peer-review started: August 26, 2021
First decision: November 17, 2021
Revised: November 26, 2021
Accepted: February 19, 2022
Article in press: February 19, 2022
Published online: March 26, 2022
Processing time: 208 Days and 12.4 Hours
The odontogenic jaw cyst is a cavity containing liquid, semifluid or gaseous components, with the development of the disease. In recent years, with the rapid development of oral materials and the transformation of treatment of jaw cysts, more options are available for treatment of postoperative bone defect of jaw cysts. Guided bone regeneration (GBR) places biomaterials in the bone defect, and then uses biofilm to separate the proliferative soft tissue and the slow-growing bone tissue to maintain the space for bone regeneration, which is widely used in the field of implantology.
To observe the clinical effect of GBR in repairing bone defect after enucleation of small and medium-sized odontogenic jaw cysts.
From June 2018 to September 2020, 13 patients (7 male, 6 female) with odontogenic jaw cysts were treated in the Department of Oral Surgery, Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine. Adults without hypertension, heart disease, diabetes or other systemic diseases were selected. The diagnosis was based on the final pathological results: 11 cases were diagnosed as apical cysts, one as primordial cyst, and one as dentigerous cyst. The lesions were located in the maxilla in seven cases, and in the mandible in six cases. All cases were treated with the same method of enucleation combined with GBR.
Three to four months after the operation, the boundary between the implant site and the surrounding normal stroma was not obvious in patients with small-sized odontogenic jaw cysts. The patients with tooth defects were treated with implant after 6 mo. For the patients with medium-sized odontogenic jaw cysts, the density of the center of the implant area was close to the normal mass at 6 mo after surgery, and there was a clear boundary between the periphery of the implant area and the normal mass. The boundary between the periphery of the implant area and the normal mass was blurred at 8-9 mo after surgery. Patients with tooth defects were treated with implants at > 6 mo after the operation.
Enucleation combined with guided bone regeneration in small and medium-sized odontogenic jaw cysts can shorten the time of osteogenesis, increase the amount of new bone formation, reduce complications, and improve quality of life.
Core Tip: This was a retrospective study to observe the clinical effect of guided bone regeneration (GBR) in repairing bone defect after enucleation of small and medium-sized odontogenic jaw cysts. The application of odontogenic jaw cysts extraction combined with GBR can shorten the time of osteogenesis, increase the amount of new bone formation, reduce complications, and improve quality of life. GBR has good prospects for application in the treatment of small and medium-sized odontogenic jaw cysts.
- Citation: Cao YT, Gu QH, Wang YW, Jiang Q. Enucleation combined with guided bone regeneration in small and medium-sized odontogenic jaw cysts . World J Clin Cases 2022; 10(9): 2764-2772
- URL: https://www.wjgnet.com/2307-8960/full/v10/i9/2764.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i9.2764
The odontogenic jaw cyst is a cavity containing liquid, semi-fluid or gaseous components, which is usually derived from odontogenic tissue or epithelium or residual epithelium[1]. The incidence rate of odontogenic jaw cysts was 10.7% in a US study on oral biopsies from a dental school[2]. Development of the disease can lead to bone destruction, absorption or displacement of adjacent teeth[3]. Clinically, odontogenic jaw cysts can be divided into root, primary, dentigerous and calcification cysts[4]. Conventional surgical curettage is mostly used clinically, and cysts are removed at one time. The disadvantage is that it may cause pathological fracture or damage of adjacent tissues[5]. For larger jaw cysts (more than 4 cm), fenestration and decompression should be performed first, and the second stage curettage should be performed when the cyst cavity has shrunk, in order to reduce the recurrence rate[6,7]. The mechanism of healing after enucleation of jaw cysts is autogenous blood filling of the bone cavity, coagulation. However, it takes a long time to heal. Some studies have shown that the average healing time of the defect caused by small jaw cysts is 1 year, while that of larger jaw cysts is 2-5 years[7,8]. In recent years, with the rapid development of oral materials and transformation of treatment of jaw cysts, more options[9,10] are available for treatment of postoperative bone defect of jaw cysts, such as autogenous bone graft[9], β-tricalcium phosphate for bone substitution[10]. Guided bone regeneration (GBR) involves placing biomaterials in the bone defect, and using biofilms to separate the proliferative soft tissue and the slow-growing bone tissue to maintain the space for bone regeneration, which is widely used in the field of implantology[11]. In view of increasing bone width and height with GBR, the purpose of this study was to observe the clinical effect of GBR in repairing bone defect after enucleation of small and medium-sized odontogenic jaw cysts (the maximum diameter: 1.0 cm-4.0 cm)[6,7].
From June 2018 to September 2020, 13 patients with odontogenic jaw cysts were treated in the Department of Oral Surgery, Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine. Adults without hypertension, heart disease, diabetes or other systemic diseases were selected. The diagnosis was based on the final pathological results: 11 cases were diagnosed as apical cysts, one as primordial cyst, and one as dentigerous cyst. The lesions were located in the maxilla in seven cases, and in the mandible in six cases. There were seven men and six women, aged 25-61 years (mean 37.2 ± 11.1 years) (Supplementary Table 1).
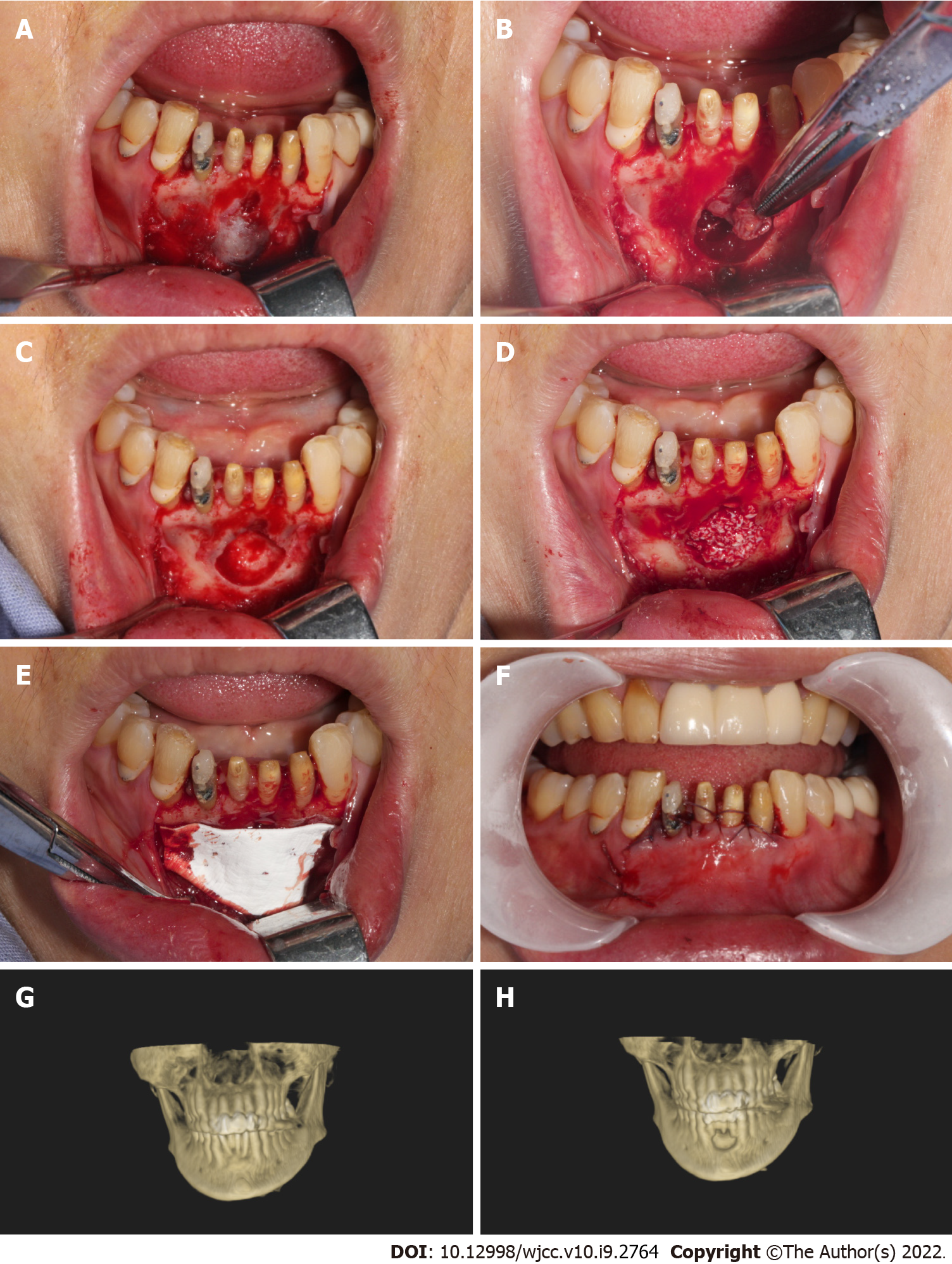
(1) Cyst enucleation: trapezoidal or triangular flap gingival sulcus incision was used. After mucoperiosteal flap elevation, an anterior vertical releasing incision was provided for optimum visualization. Sharp dissection using a pair of scissors was done superficial to the cyst wall in order to separate the mucoperiosteal flap without compromising its integrity. While the cystic lesion was identified and enucleated in total, mild adhesions to the lingual mucoperiosteum were released through blunt dissection using the surgical curette. The cyst was enucleated and sent to pathology during surgery; (2) Treatment of bone cavity: cyst tissue was scraped off completely, the cavity was washed with a large amount of normal saline, and the cavity was ground intermittently with a planter at 3000 r/min; and (3) GBR: The residual defect left behind by the cystic lesion was filled with a xenograft bone (Bio-Oss, Geistlich Pharma, Princeton, NJ, United States) soaked in sterile normal saline and covered by a resorbable collagen membrane (Bio-Gide, Geistlich Pharma, Princeton, NJ, United States). The coverage was about 3 mm from the cyst surface to the defect area. The mucoperiosteal flap was re-approximated and closed with Vicryl 4-0 interrupted sutures (Polyglactin 910, ETHICON, Somerville, NJ, United States) (Figure 1A-F).
Antibiotics were given intravenously to prevent infection for 1-2 d after the operation. Gargling was used to maintain oral hygiene. The suture was removed 10 d later. After 1, 3-4, 6, 8-9 and 12 mo, CBCT (i-CAT, Imaging Sciences International, Hatfield, PA, United States) was performed to check the healing of the defect area.
The range of incision should be determined according to preoperative imaging examination, combined with imaging and clinical conditions. All patients had destruction of the bone plate. Twelve of the 13 patients were operated upon through the maxillobuccal gingiva (CBCT showed that the labial or buccal plate was damaged), and one was operated upon through the palatal median mucinous membrane (CBCT showed that the palatal plate was damaged and the labial plate was intact). Trapezoidal incision was used in 11 cases, and angular-shaped incision was used in two because the lesion was located in the posterior molar area.
Before the operation, 11 patients underwent root canal therapy for the diseased teeth and their apices in the cystic cavity; three patients without root canal treatment; and eight diseased teeth were not worth extracting. There were two cases of root canal therapy after the operation. So far, four cases have completed implant restoration of missing teeth.
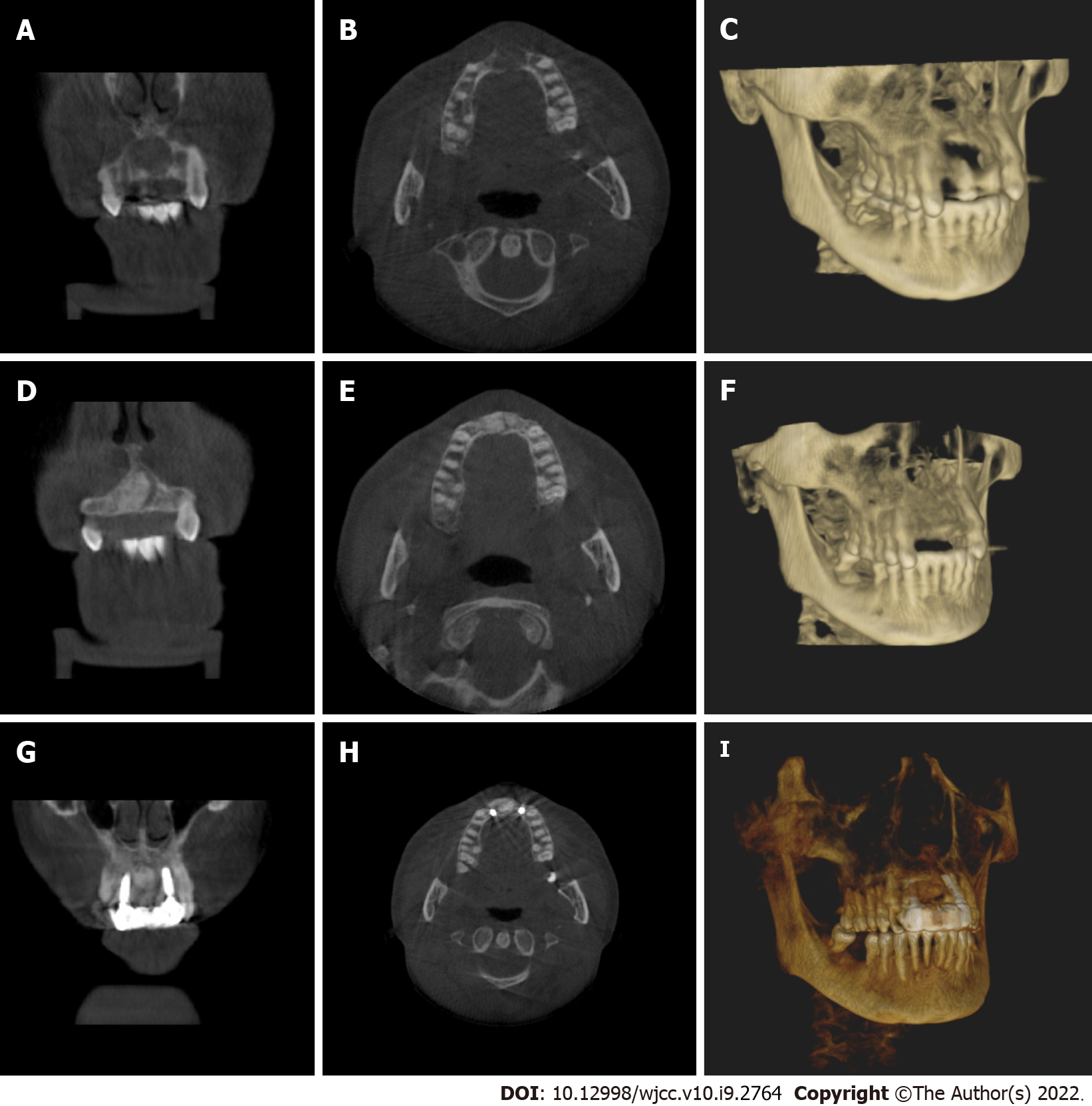
The maxillofacial cysts caused destruction of the labial (buccal) or palatal plates; the maximum diameter of which was 1.0 cm-4.0 cm. Small-sized lesions (≥ 1.0 cm, ≤ 2.5 cm) were found in six cases, and medium-sized lesions (> 2.5 cm, < 4.0 cm) in seven. Three to four months after the operation, the boundary between the implant site and the surrounding normal stroma was not obvious in patients with small-sized lesions (Figure 1G and H). The patients with tooth defects were treated with implants. For the patients with median-sized lesions, the density of the center of the implant area was close to the normal mass at 6 mo after the operation, and there was a clear boundary between the periphery of the implant area and the normal mass. The boundary between the periphery of the implant area and the normal mass was blurred at 8-9 mo after the operation. For medium-sized lesions, the patients with dentition defect were treated with implant repair for 8-9 mo (Figure 2A-I).
The immediate postoperative period was uneventful, and the surgical wound healed remarkably well. The patients were satisfied with the operation. Pathological examination supported the preoperative diagnosis. Follow-up examinations at 1, 3, 6, 9 and 12 mo after cyst enucleation and GBR revealed no clinical recurrence of the lesion (Supplementary Table 2).
Odontogenic jaw cyst is a common cause of jaw defect. For jaw defect after odontogenic jaw cyst enucleation, there is no universal treatment. In the past, most of the methods used were tissue self-healing. Chiapasco et al[12] evaluated spontaneous bone healing after enucleation of large mandibular cysts with a computerized analysis of postoperative panoramic radiographs, which showed mean reduction in size of the residual cavity of 12.34% after 6 mo, 43.46% after 1 year, and 81.30% after 2 years, and increase in bone density was 37% after 6 mo, 48.27% after 12 mo, and 91.01% after 24 mo. Rabin Chacko et al[7] evaluated spontaneous bone regeneration after enucleation of odontogenic jaw cysts (diameter 1.4 cm-15 cm) with a computerized analysis of postoperative panoramic radiographs, which showed mean reduction in size of the residual cavity of 25.85% after 6 mo, 57.13% after 9 mo, 81.03% after 1 year and 100% after 2 years. Li[13] used CBCT to explore the natural outcome of jaw defect after curettage of odontogenic jaw cysts. CBCT images showed that the cytoplasm around the cyst was regenerated and reconstructed, and the cyst cavity was gradually reduced. The formation rate differed with the size of the original capsule, which was maintained at about 50% and 80% at 6 mo and 12 mo, respectively, after the operation.
In recent years, with the emergence of high-quality biomaterials, a large number of studies have been carried out on the treatment of jaw lesions with exogenous implants as filling materials. At present, the commonly used xenogeneic bone meal mainly comes from cattle, such as Geistlich Bio-Oss®. Kim et al[14] conducted a follow-up observation of 20 patients with cysts filled with xenogeneic bone meal materials after curettage, and found that there was more new bone formation 3 mo after the operation. Tonetti et al[15] applied the material to the treatment of alveolar defect caused by periodontal disease, and showed that the xenogeneic bone meal had good bone-forming ability. Although these allogeneic materials lack active components, such as osteoblasts, which do not have the ability to induce bone formation, their porous structure can guide bone tissue regeneration. Yin et al[16] found that after curettage of cysts with Geistlich Bio-Oss®, new bone formation was found in the defect area 1 and 3 mo after the operation, and bone integration occurred 6 mo later. Our study also found that after curettage combined with GBR for the treatment of odontogenic jaw cysts with small lesion area, the defect area healed well 3-4 mo after the operation, which was similar to the surrounding normal density, and the boundary between the two was not clear. After enucleation combined with GBR, the defect area healed well 6-8 mo after the operation, which was similar to the surrounding normal density. It is suggested that this treatment method has a definite effect on promoting the healing of maxillofacial cysts after surgery. Compared with the simple enucleation method, the time of osteogenesis was significantly shortened. For patients with simultaneous cyst and tooth extraction, this treatment method can shorten the time of tooth formation, implant the missing teeth as soon as possible, and shorten the disease course. This is particularly important for patients with anterior teeth cysts. Maxillary anterior tooth area is an important oral aesthetic area, which is exposed by lip tissue in the maximum movement state. The loss of teeth in this area not only causes the loss of function of the missing tooth area, but also has a significant impact on the facial appearance, language, pronunciation and mental health of patients. Studies have shown that the natural healing time of large bone defects after cyst surgery takes 2-5 years, and there may be insufficient bone height and width, which brings challenges for later implantation. Therefore, how to shorten the time of missing teeth and provide sufficient bone for implant has become an urgent problem. In our study, a 50-year-old female patient presented with residual roots of 12, 11, 12, 22. CBCT showed that the size of the cyst in the area of #12-22 was 29.8 mm × 21.3 mm, and the buccal and lingual bone walls were absorbed. At the follow-up visit 6 mo after #12,11,21,22 extraction + cyst enucleation + GBR, it was found that the bone mass in the edentulous area and the buccal alveolar bone fullness were well recovered. CBCT showed that the width of alveolar bone and the height were adequate. An implant operation was performed at #12 and #22 sites, and the initial stability of the implants was greater than 35N, so immediate repair was carried out (Figures 2 and 3). This shortened the time of missing teeth and patient satisfaction was high. At present, five cases of missing teeth in the cyst area have been repaired by implants, which significantly shortened the time of missing teeth, and the patients were satisfied.
All 13 patients were treated with surgical enucleation and primary bone defect repair using GBR with xenograft and resorbable collagen membrane, along with a recurrence-free follow-up period. There was no infection after bone grafting. The possible reasons may be the following. (1) After bone grafting, biomaterial scaffolds play an important role in mandibular regeneration. Complete filling of biomaterial scaffolds in the capsule cavity is conducive to blood clotting to stabilize the defect area, and then promote mandibular regeneration; (2) intact biofilm is also important, which can block the influence of extraluminal soft tissue on bone regeneration; and (3) when the wound was closed, the base of the soft tissue valve was supported by biological scaffold and biofilm, and sutured tightly to avoid infection in the surgical area.
This study had some limitations, including small sample size and short follow-up time. In the future, we need to expand the sample size and continue to delay the return visit time. In addition, a reasonable control group should be set up for prospective comparison.
The application of odontogenic jaw cysts extraction combined with GBR can shorten the time of osteogenesis, increase the amount of new bone formation, reduce complications, and improve quality of life. It has good prospects for application in the treatment of odontogenic jaw cysts. However, this study also has some limits, such as insufficient sample size and short follow-up time, we needs further to increase the sample size, the results obtained will be more persuasive.
The odontogenic jaw cyst is a cavity containing liquid, semifluid or gaseous components, with the development of the disease. In recent years, with the rapid development of oral materials and the transformation of treatment of jaw cysts, more options are available for treatment of postoperative bone defect of jaw cysts. Guided bone regeneration (GBR) places biomaterials in the bone defect, and then uses biofilm to separate the proliferative soft tissue and the slow-growing bone tissue to maintain the space for bone regeneration, which is widely used in the field of implantology.
This was a retrospective study to observe the clinical effect of guided bone regeneration (GBR) in repairing bone defect after enucleation of small and medium-sized odontogenic jaw cysts. The application of odontogenic jaw cysts extraction combined with GBR can shorten the time of osteogenesis, increase the amount of new bone formation, reduce complications, and improve quality of life. GBR has good prospects for application in the treatment of small and medium-sized odontogenic jaw cysts.
To observe the clinical effect of GBR in repairing bone defect after enucleation of small and medium-sized odontogenic jaw cysts.
From June 2018 to September 2020, 13 patients (7 male, 6 female) with odontogenic jaw cysts were treated in the Department of Oral Surgery, Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine. Adults without hypertension, heart disease, diabetes or other systemic diseases were selected. The diagnosis was based on the final pathological results: 11 cases were diagnosed as apical cysts, one as primordial cyst, and one as dentigerous cyst. The lesions were located in the maxilla in seven cases, and in the mandible in six cases. All cases were treated with the same method of enucleation combined with GBR.
Three to four months after the operation, the boundary between the implant site and the surrounding normal stroma was not obvious in patients with small-sized odontogenic jaw cysts. The patients with tooth defects were treated with implant after 6 mo. For the patients with medium-sized odontogenic jaw cysts, the density of the center of the implant area was close to the normal mass at 6 mo after surgery, and there was a clear boundary between the periphery of the implant area and the normal mass. The boundary between the periphery of the implant area and the normal mass was blurred at 8-9 mo after surgery. Patients with tooth defects were treated with implants at > 6 mo after the operation.
Enucleation combined with guided bone regeneration in small and medium-sized odontogenic jaw cysts can shorten the time of osteogenesis, increase the amount of new bone formation, reduce complications, and improve quality of life.
The application of odontogenic jaw cysts extraction combined with GBR can shorten the time of osteogenesis, increase the amount of new bone formation, reduce complications, and improve quality of life. It has good prospects for application in the treatment of odontogenic jaw cysts.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zhu H S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Rajendra Santosh AB, Boyd D, Laxminarayana KK. Clinical Outline of Oral Diseases. Dent Clin North Am. 2020;64:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Rajendra Santosh AB. Odontogenic Cysts. Dent Clin North Am. 2020;64:105-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 61] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 3. | Zhao Y, Liu B, Zhao YF. Controversies Regarding the Management of Teeth Associated with Cystic Lesions of the Jaws. Chin J Dent Res. 2019;22:81-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 4. | Speight PM, Takata T. New tumour entities in the 4th edition of the World Health Organization Classification of Head and Neck tumours: odontogenic and maxillofacial bone tumours. Virchows Arch. 2018;472:331-339. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 147] [Cited by in RCA: 185] [Article Influence: 23.1] [Reference Citation Analysis (6)] |
| 5. | de Moraes ATL, Soares HA, Viana Pinheiro JJ, Ribeiro Ribeiro AL. Marsupialization before enucleation as a treatment strategy for a large calcifying odontogenic cyst: Case report. Int J Surg Case Rep. 2020;67:239-244. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Shah N, Logani A, Kumar V. A minimally invasive surgical approach for large cyst-like periapical lesions: a case series. Gen Dent. 2014;62:e1-e5. [PubMed] |
| 7. | Chacko R, Kumar S, Paul A, Arvind. Spontaneous Bone Regeneration After Enucleation of Large Jaw Cysts: A Digital Radiographic Analysis of 44 Consecutive Cases. J Clin Diagn Res. 2015;9:ZC84-ZC89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Rubio ED, Mombrú CM. Spontaneous Bone Healing after Cysts Enucleation without Bone Grafting Materials: A Randomized Clinical Study. Craniomaxillofac Trauma Reconstr. 2015;8:14-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Aludden HC, Mordenfeld A, Hallman M, Dahlin C, Jensen T. Lateral ridge augmentation with Bio-Oss alone or Bio-Oss mixed with particulate autogenous bone graft: a systematic review. Int J Oral Maxillofac Surg. 2017;46:1030-1038. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 67] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 10. | Bohner M, Santoni BLG, Döbelin N. β-tricalcium phosphate for bone substitution: Synthesis and properties. Acta Biomater. 2020;113:23-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 319] [Article Influence: 63.8] [Reference Citation Analysis (0)] |
| 11. | Mordini L, Hur Y, Ogata Y, Finkelman M, Cavani F, Steffensen B. Volumetric Changes Following Lateral Guided Bone Regeneration. Int J Oral Maxillofac Implants. 2020;35:e77-e85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Chiapasco M, Rossi A, Motta JJ, Crescentini M. Spontaneous bone regeneration after enucleation of large mandibular cysts: a radiographic computed analysis of 27 consecutive cases. J Oral Maxillofac Surg. 2000;58:942-8; discussion 949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 105] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 13. | Li X. The study of bone tissue repair after curettage of mandibular cyst by CBCT. Qingdao Daxue. 2018;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Kim YK, Yun PY, Lee HJ, Ahn JY, Kim SG. Ridge preservation of the molar extraction socket using collagen sponge and xenogeneic bone grafts. Implant Dent. 2011;20:267-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 53] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 15. | Tonetti MS, Cortellini P, Lang NP, Suvan JE, Adriaens P, Dubravec D, Fonzar A, Fourmousis I, Rasperini G, Rossi R, Silvestri M, Topoll H, Wallkamm B, Zybutz M. Clinical outcomes following treatment of human intrabony defects with GTR/bone replacement material or access flap alone. A multicenter randomized controlled clinical trial. J Clin Periodontol. 2004;31:770-776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 97] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 16. | Yin XN, Wang XM. Application of Bio-Oss® in bone repair after jaw cyst operation. Quankeyixue linchuang yu Jiaoyu. 2011;6:677-678. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |