Published online Mar 26, 2022. doi: 10.12998/wjcc.v10.i9.2710
Peer-review started: August 24, 2021
First decision: November 17, 2021
Revised: November 26, 2021
Accepted: February 12, 2022
Article in press: February 12, 2022
Published online: March 26, 2022
Processing time: 210 Days and 1.5 Hours
Endoscopic removal with forceps/baskets is favored in treating submandibular stones due to its minimal invasiveness. However, recent studies have found that endoscopic removal failure (ERF) is not unusual, and stones in such cases still need to be removed with other surgical methods. If the risk of ERF can be predicted preoperatively, it could be helpful for surgeons when choosing the appropriate therapy.
To develop a predictive nomogram for the risk of ERF when treating sub
A total of 180 patients with 211 submandibular stones treated from January 2012 to December 2020 were included in the current study. Based on the preoperative clinical features of the stones, independent risk factors for ERF were identified by logistic regression analysis. The stones were then randomly divided into training and testing sets. A nomogram was constructed to predict the risk of ERF using the training set and then validated using both sets. The predictive performance of the nomogram was assessed by calibration curves and the concordance index (C-index).
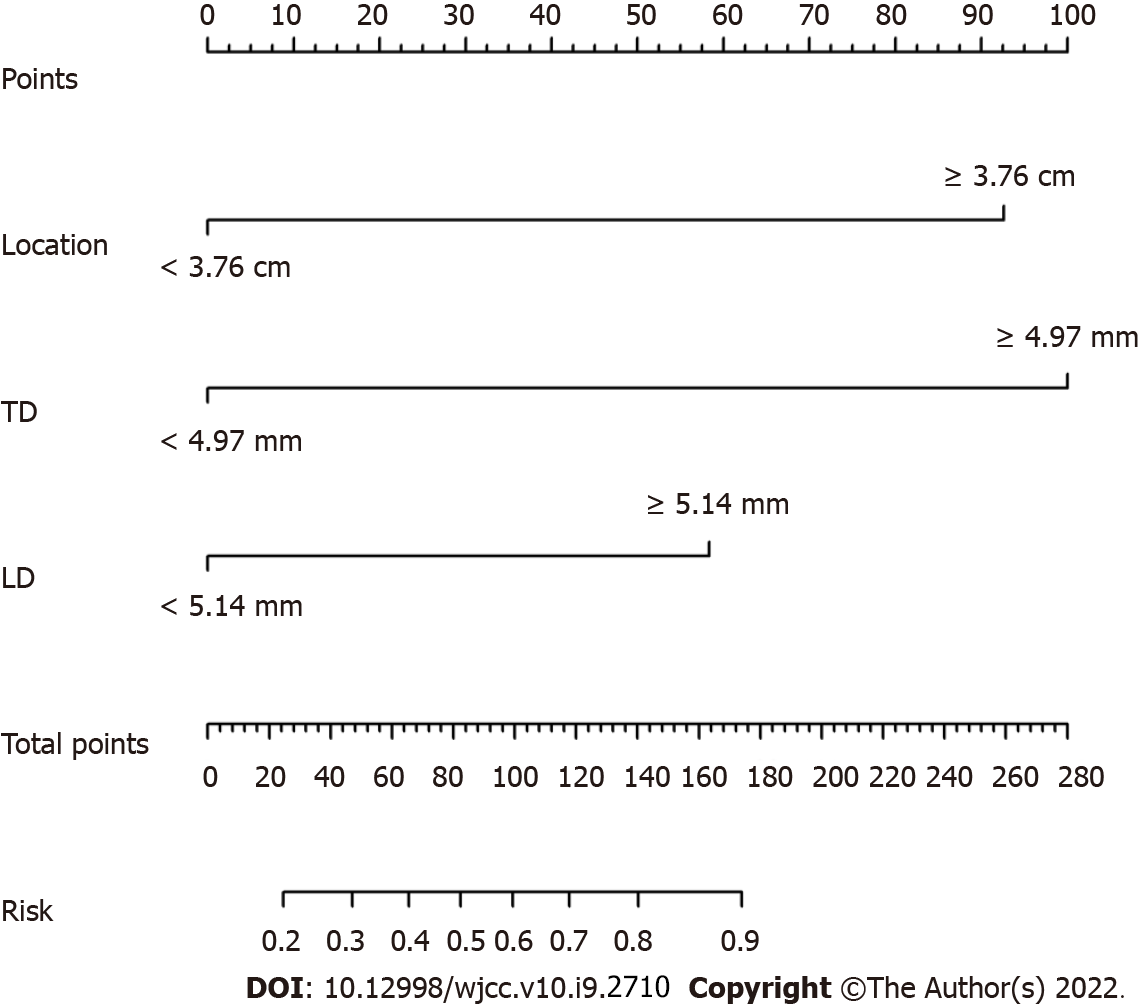
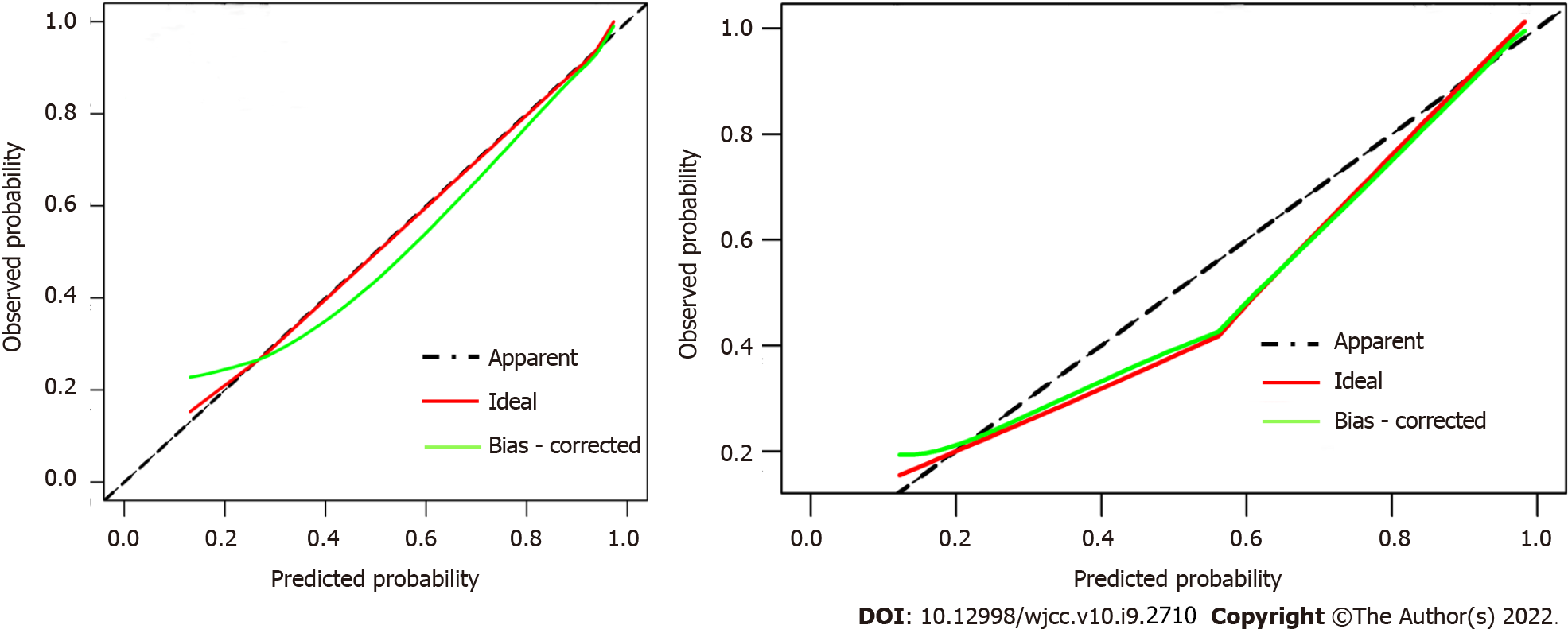
Three independent predictors, location (P = 0.040), transverse diameter (P < 0.001) and longitudinal diameter (P < 0.001) measured on the cone beam computed tomography (CBCT) images of the submandibular stones, were identified and included in the predictive nomogram. Calibration curves of the nomogram showed good agreement between the predicted and observed probabilities in both sets. The C-index in the training set was 0.917 (95%CI, 0.875-0.959) and that in the testing set was 0.925 (95%CI, 0.862-0.989).
A nomogram based on the location, transverse and longitudinal diameters on CBCT images of submandibular stones showed satisfactory efficacy in predicting the risk of ERF preoperatively when treating submandibular stones.
Core Tip: A predictive nomogram based on the objective and measurable preoperative clinical features of submandibular stones was constructed in the present study; the nomogram helps to determine the risk of endoscopic removal failure preoperatively and aids in the selection of appropriate surgical methods.
- Citation: Huang Y, Liang PS, Yang YC, Cai WX, Tao Q. Nomogram to predict the risk of endoscopic removal failure with forceps/baskets for treating submandibular stones. World J Clin Cases 2022; 10(9): 2710-2720
- URL: https://www.wjgnet.com/2307-8960/full/v10/i9/2710.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i9.2710
Endoscopic stone removal, in which stones are removed with forceps/baskets during endoscopy, plays an important role in treating salivary lithiasis[1-5]. For most surgeons and patients, endoscopic stone removal is favored because of its high visibility and minimal invasiveness. However, studies in recent years have found that many submandibular stones fail to be removed by the forceps/baskets under endoscopy, which means endoscopic removal failure (ERF) in treating submandibular stones is not unusual[6-8]. Fruitless attempts to repeatedly perform endoscopic removal with forceps/baskets will greatly prolong the operation time and increase the risk of severe postoperative complications, such as ductal avulsion and perforation[5,9]. Therefore, the clinical features of the stones should be carefully considered when selecting endoscopic removal, which has pros and cons[2,3,10]. Currently, however, a broad consensus has not been reached regarding the indications of endoscopic removal for submandibular stones, leading to improper surgical choice in some cases[7,8].
Therefore, in this study, we aimed to identify the risk factors for ERF and construct and validate a predictive nomogram, a useful statistical tool, to identify the risk of ERF preoperatively when treating submandibular stones and to aid in clinical therapeutic decision making.
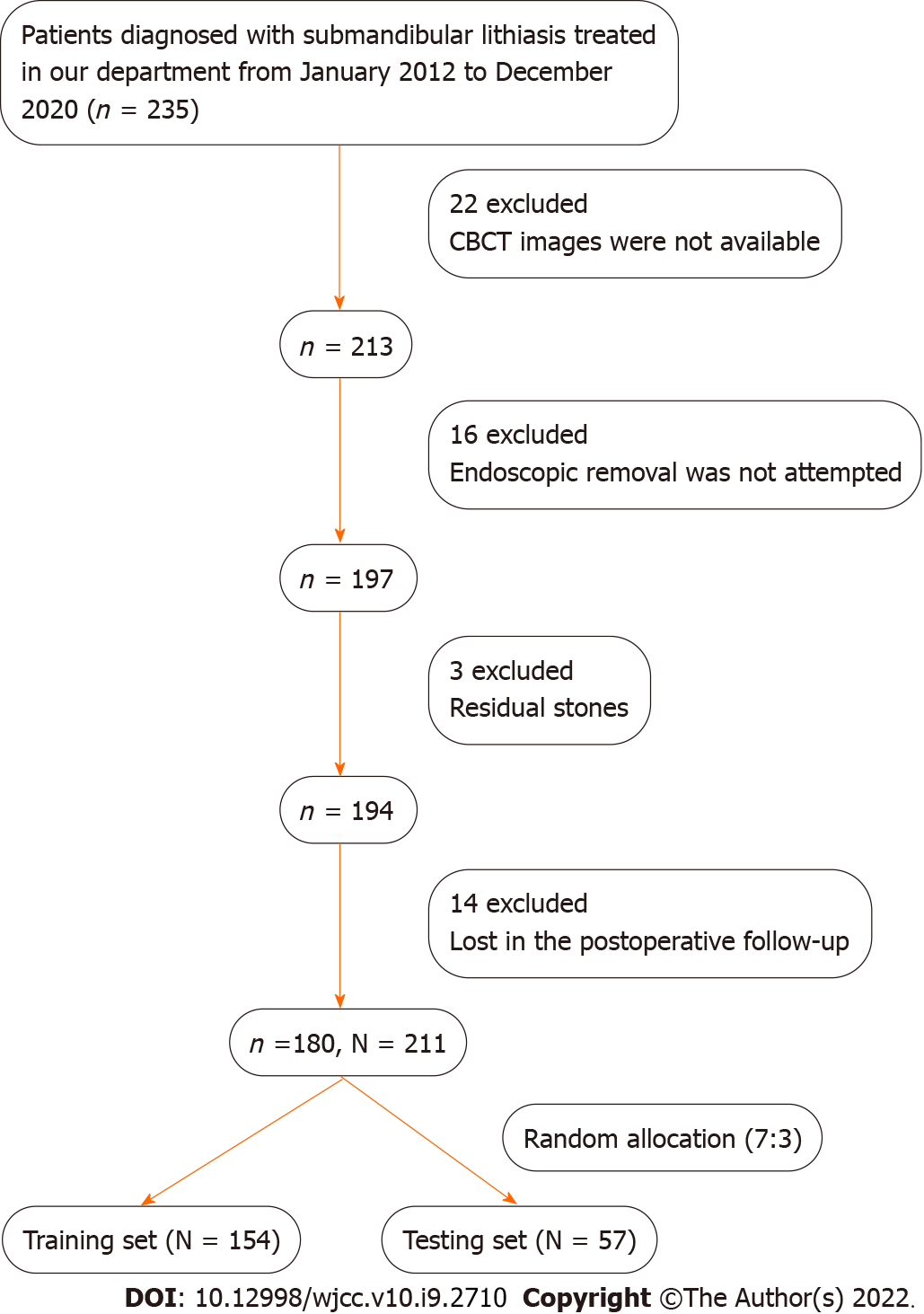
This retrospective study enrolled patients with submandibular stones treated at the Hospital of Stomatology, Sun Yat-Sen University, from January 2012 to December 2020. The inclusion criteria were as follows: (1) availability of complete clinical information and CBCT images; (2) attempted stone localization by introducing an endoscope through the ductal orifice and removal with forceps or baskets under the endoscope; and (3) satisfactory surgical outcomes without residual stones. The detailed exclusion criteria and data screening process are shown in Figure 1.
The study was approved by the Medical Ethics Committee of Hospital of Stomatology, Sun Yat-Sen University (No. KQEC-2019-41) and was performed in accordance with the Declaration of Helsinki in regard to medical protocols and ethics.
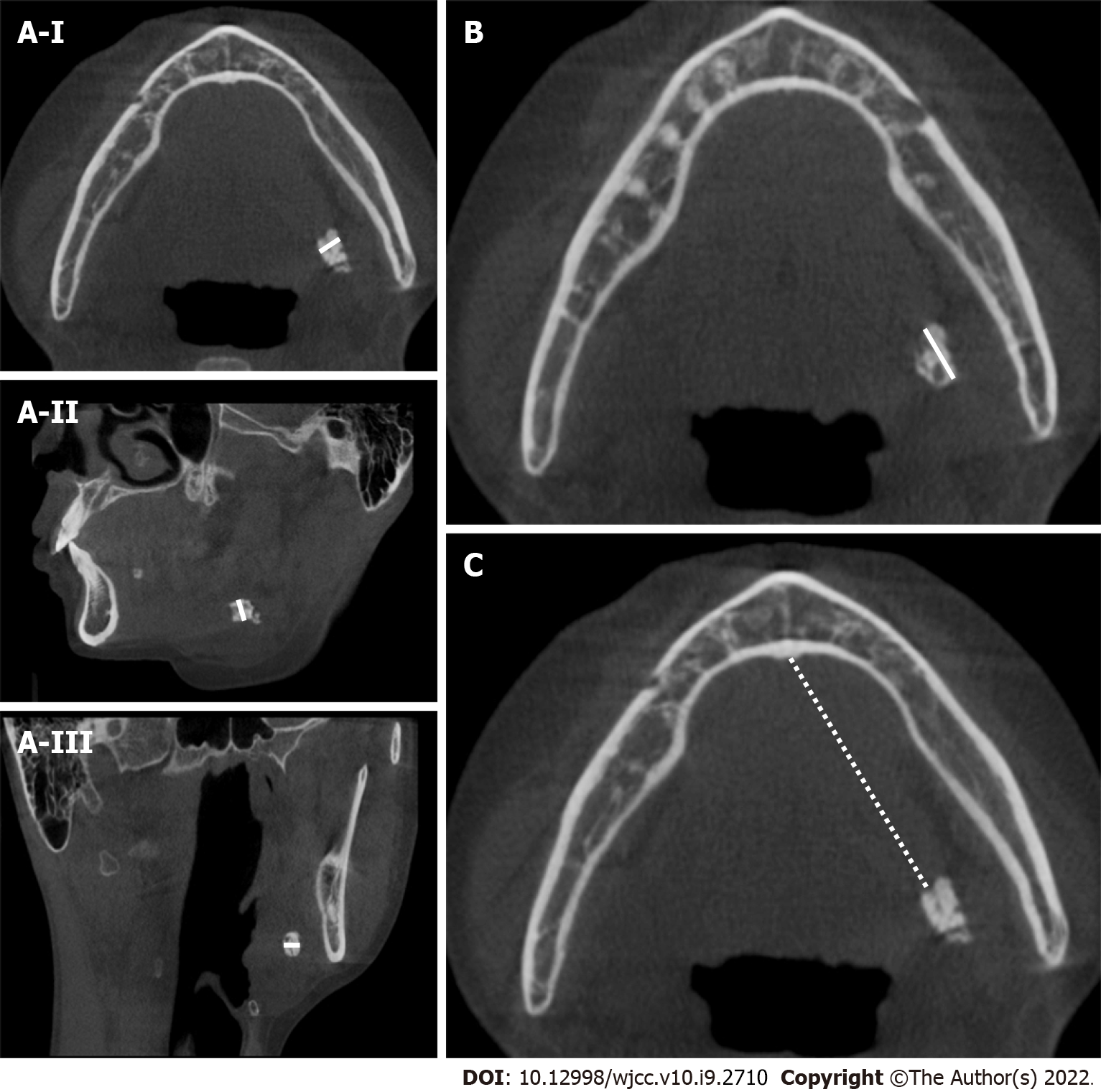
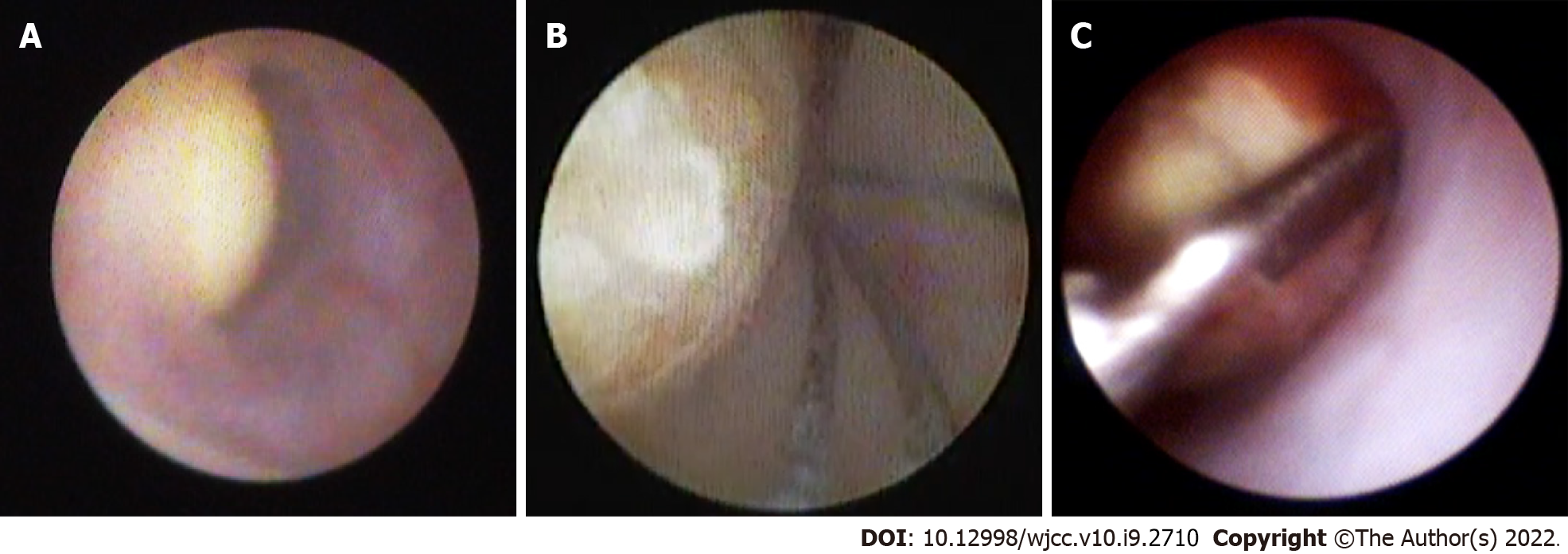
Clinical data, including sex, age, intraductal stone treatment history, involved sides, number of stones in the same gland, palpation, CBCT images (New Tom Inc., Italy), and results of endoscopic removal were collected for the patients who met the criteria. The average location, transverse diameter (TD) and longitudinal diameter (LD) of all the stones on CBCT images were recorded after evaluation by 3 blinded experienced surgeons. As demonstrated in Figure 2, the location of the stone was defined as the distance between its anterior edge and the midpoint of the glossal bony cortex of the mandible in axial CBCT views. The TD of the stone was defined as the maximum width on its axial, coronal and sagittal sections. The LD of the stone was defined as its maximum length on the axial CBCT views. We attempted to remove all of the stones included in our study with forceps or baskets after locating them with an endoscope (Karl Storz Inc., Germany), as shown in Figure 3. All endoscopic removals were performed by the same three experienced surgeons (Q.T., G.L., and H.L.).
Statistical analyses were performed with SPSS 25.0 software (SPSS Inc., Chicago), and the statistical methods of this study were reviewed by Zhi-Wei Li from the Department of Medical Statistics and Epidemiology, Sun Yat-Sen University.
Receiver operating characteristic (ROC) curve analysis was performed, and Youden’s index was calculated to determine the optimal cutoff points for the location, TD and LD of the stones. According to the new classification criteria of the World Health Organization, 44 years was considered the cutoff value for age.
Pearson’s chi-squared test was used to explore the correlations between the clinical variables of the stones and ERF. Next, univariate and multivariate logistic regression analyses were used to identify the independent risk factors. Then, ROC curve analysis was carried out, and the area under the curve (AUC) was calculated to assess the predictive performance of the univariate and multivariate combined models. For the model with the best predictive performance, Youden's index was calculated to determine the optimal cutoff value, and the accuracy, sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were calculated to evaluate the model.
All stones were randomly divided into the training and testing sets at a ratio of 7:3 using an R-generated random number (random seeds of 123). With the ‘rms’ package in R software (version 4.0.3) and based on the training set, a nomogram was constructed using the independent factors from the best model above to identify the risk of ERF. The predictive performance of the nomogram was evaluated by calibration curves and the C-index.
A total of 180 patients with 211 stones who underwent endoscopic removal attempts were finally included in further analyses; 100 of the patients were female. The average age of the patients was 41.4 ± 13.5 years old (17-75 years old).
Thirty-four stones were confirmed to have an intraductal stone treatment history, such as intraductal irrigation and intraductal dilatation, which might result in ductal stenosis after the treatment. A total of 52.6% of the stones involved the glands on the right side. Thirty-one stones were found to be multiple, and 77 were unpalpable. The average location, TD and LD of the stones were 3.48 ± 1.51 cm, 5.17 ± 2.01 mm and 4.97 ± 1.48 mm, respectively. Endoscopic removal was successful in 89 cases but failed in 122 attempts. The preoperative clinical variables of all the enrolled stones are shown in Table 1.
| Variables | |
| Sex | |
| Male | 99 (46.9%) |
| Female | 112 (53.1%) |
| Age of the patient | |
| < 44 yr | 123 (58.3%) |
| ≥ 44 yr | 88 (41.7%) |
| Intraductal stone treatment history | |
| Yes | 34 (16.1%) |
| No | 177 (83.9%) |
| Involved side | |
| Left | 100 (47.4%) |
| Right | 111 (52.6%) |
| Amounts of stones | |
| Single | 180 (85.3%) |
| Multiple | 31 (14.7%) |
| Palpation | |
| Positive | 134 (63.6%) |
| Negative | 77 (36.4%) |
| Location/cm | |
| Range | 0.42-5.69 |
| Mean | 3.48 ± 1.51 |
| TD/mm | |
| Range | 1.23-12.00 |
| Mean | 5.17 ± 2.01 |
| LD/mm | |
| Range | 0.57-9.26 |
| Mean | 4.97 ± 1.48 |
| Surgical methods | |
| Endoscopic removal | 89 (42.2%) |
| ERF | 122 (57.8%) |
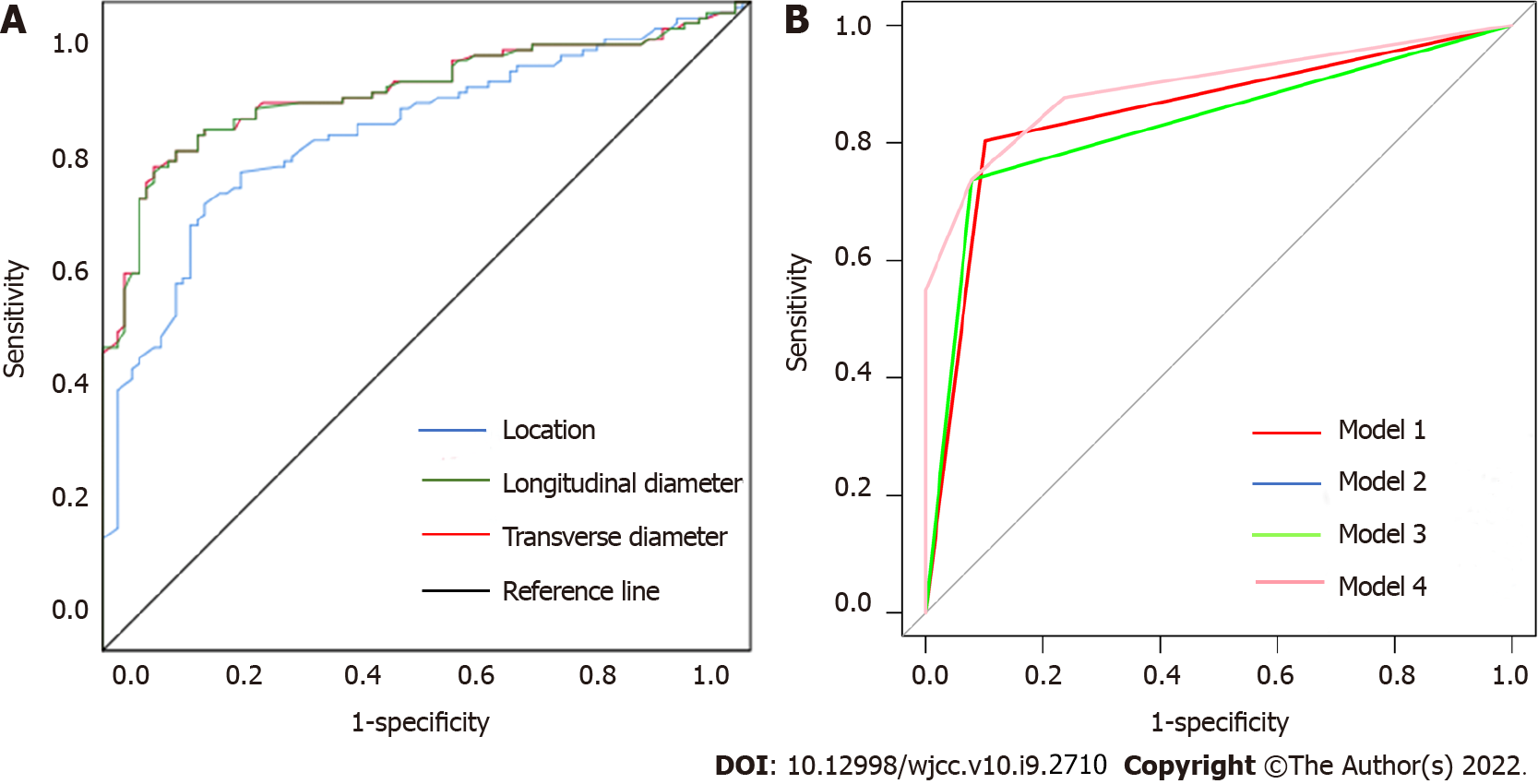
The optimal cutoff points for the location, TD and LD were 3.76 cm, 4.97 mm and 5.14 mm, respectively, as demonstrated in Figure 4A and Table 2. These three factors, together with the age of patients, were then used to divide patients into subgroups according to the cutoff values in further statistical analysis. Correlations between the clinical features of the stones and ERF are shown in Table 3; palpation (P < 0.001), location (P < 0.001), TD (P < 0.001) and LD (P < 0.001) were significantly associated with ERF.
| Variables | Cutoff | Youden’s index | Sensitivity | Specificity |
| Location/cm | 3.76 | 0.581 | 0.719 | 0.862 |
| TD/mm | 4.97 | 0.675 | 0.787 | 0.877 |
| LD/mm | 5.14 | 0.638 | 0.730 | 0.908 |
| Variables | Endoscopic removal | ERF | χ2 | P value | |
| Sex | Male | 42 | 57 | 0.005 | 0.946 |
| Female | 47 | 65 | |||
| Age of the patient | < 44 | 54 | 69 | 0.359 | 0.549 |
| ≥ 44 | 35 | 53 | |||
| Intraductal stone treatment history | Yes | 12 | 22 | 0.788 | 0.244 |
| No | 77 | 100 | |||
| Involved side | Left | 43 | 57 | 0.052 | 0.819 |
| Right | 46 | 65 | |||
| Amounts of stones | Single | 74 | 106 | 0.005 | 0.945 |
| Multiple | 15 | 16 | |||
| Palpation | Positive | 38 | 96 | 28.764 | < 0.001a |
| Negative | 51 | 26 | |||
| Location | < 3.76 cm | 75 | 38 | 58.382 | < 0.001a |
| ≥ 3.76 cm | 14 | 84 | |||
| TD | < 4.97 mm | 76 | 28 | 80.274 | < 0.001a |
| ≥ 4.97 mm | 13 | 94 | |||
| LD | < 5.14 mm | 82 | 32 | 34.586 | < 0.001a |
| ≥ 5.14 mm | 7 | 90 | |||
As demonstrated in Table 4, three independent risk factors were identified by univariate and multivariate logistic regression analyses, including the location (OR = 8.796, 95%CI, 3.673-22.661, P = 0.040), TD (OR = 10.287, 95%CI, 3.301-35.269, P < 0.001) and LD (OR = 4.412, 95%CI, 1.256-15.575, P < 0.001) of the stones.
| Variables | Univariate | Multivariate | ||||
| Odds ratio | 95%CI | P value | Odds ratio | 95%CI | P value | |
| Sex | 1.288 | 0.745-2.228 | 0.366 | - | - | - |
| Age of the patient | 1.185 | 0.680-2.066 | 0.549 | - | - | - |
| Intraductal stone treatment history | 1.412 | 0.658-3.029 | 0.376 | - | - | - |
| Involved side | 1.066 | 0.617-1.842 | 0.819 | - | - | - |
| Amounts of stones | 1.026 | 0.496-2.123 | 0.945 | - | - | - |
| Palpation | 4.955 | 2.710-9.061 | < 0.001a | - | - | - |
| Location/cm | 11.842 | 5.956-23.547 | < 0.001a | 8.796 | 3.672-22.661 | 0.040a |
| TD/mm | 19.626 | 9.516-40.481 | < 0.001a | 10.287 | 3.301-35.269 | < 0.001a |
| LD/mm | 32.946 | 13.791-78.106 | < 0.001a | 4.412 | 1.256-15.575 | < 0.001a |
Comparisons of the predictive performance of the univariate models and multivariate combined model are shown in Figure 4B. The multivariate combined model, based on the three independent risk factors, had the best predictive performance with an AUC of 0.920, accuracy of 84.8%, sensitivity of 77.9%, specificity of 94.3%, PPV of 95.0% and NPV of 75.7%.
A total of 154 stones were selected randomly for the training set, while the remaining 57 were included in the testing set. Based on the data from the training set, the location, TD and LD of the stones were incorporated when constructing the nomogram model for predicting the risk of ERF, as shown in Figure 5. Calibration curves of the nomogram are shown in Figure 6; good agreement was found between the predicted and observed probabilities in both sets. The C-index of the model in the training set was 0.917 (95%CI, 0.875-0.959), and that in the testing set was 0.925 (95%CI, 0.862-0.989).
At present, the preservation of glandular functions and minimal invasiveness have become the focuses of treating submandibular stones[8,11,12]. Endoscopic stone removal with forceps/baskets has allowed the incision-free treatment of submandibular stones and has been favored due to its ability to be directly visualized endoscopically and its minimally invasive nature. The procedure not only avoids the need for an incision but also helps with stone positioning, ductal expansion, plug removal, and tiny stone clearance. However, studies in recent years have found that endoscopic removal with forceps/baskets failed to achieve satisfactory therapeutic effects in some cases of submandibular stones[10,13]. It has been reported that the procedure might have limitations when removing the submandibular stones in the following cases[2,6,14,15]: (1) Posteriorly located stones; (2) very large stones; (3) irregular stones and (4) stones trapped by ductal stenosis. After repeatedly fruitless attempts at endoscopic removal, such submandibular stones still need to be removed with other surgical methods, such as transoral incision and even gland excision[7,8,16]. Under these circumstances, repeated fruitless attempts with endoscopy and forceps/baskets will greatly prolong the operation time and increase the risk of ductal perforation, resulting in severe swelling of the submaxillary area and even postoperative airway obstruction.
If the risk of ERF can be predicted before the surgery, unsuccessful endoscopic removal can be avoided to a large extent, and the patients will be able to truly benefit from this minimally invasive procedure. Based on the clinical records of 211 stones at our institution, all preoperative factors that can fully and objectively reflect the clinical features of submandibular stones were collected. According to the results of Pearson’s chi-squared test and univariate logistic regression analysis, the palpation, location, TD and LD of the stones were associated with the outcomes of endoscopic removal. Multivariate logistic regression analysis finally identified stone location, TD and LD on cone beam computed tomography images as independent risk factors for ERF.
The results of our study are consistent with those of previous studies[6,8,10,17]. Cox et al[18] pointed out that the location and size of the stones significantly affected the success rate of endoscopic removal for submandibular stones. Kondo et al[10] found that the success rate of endoscopic removal for anterior stones was higher than that for stones located in the posterior segment of the duct, and the transverse diameter of the stones was significantly correlated with successful endoscopic removal. Foletti et al[6] reported that submandibular stones located in the middle or posterior third of the duct with a transverse diameter less than 4 mm could be removed by forceps/baskets under endoscopy. Koch et al[17] believed that endoscopic removal could be adopted for anterior submandibular stones with transverse diameters less than 5 mm. Marchal et al[19] found that endoscopic removal could be selected when the transverse diameter of the stones was less than 3 mm. Fabie et al[8] believed that the benefits of applying other surgical methods to remove submandibular stones increased when the transverse diameter was greater than 6 mm. In the opinion of Walveka et al[15], the shapes and locations of the stones were the main factors that affected the success rate of endoscopic removal. However, previous studies have not proposed specific methods for measuring the preoperative location and size of submandibular stones and have not reached a broad consensus on the indications for endoscopic removal.
In contrast to previous studies, our current study first defined the specific methods for the preoperative measurement of stone location and size and used these measurable and objective independent risk factors to construct an effective nomogram for quantifying the indications for endoscopic stone removal. The midpoint of the glossal bony cortex of the mandible is regarded as the marker for measuring the stone location because it is close to the ductal orifice and can be clearly visualized on CBCT images. The distance between this point and the anterior edge of stones also represents the depth to which the endoscope and forceps/baskets should be lowered into the ductal system, providing guidance during the process of endoscopic removal.
Nevertheless, there are some limitations to our current study. Due to its retrospective nature, information bias may have been present during the data collection procedure. Additionally, this study was a single-center analysis, and a limited number of samples were included. It is essential to assess the nomogram at multiple institutes with a larger population. Moreover, our present model does not include anatomical variations of the Wharton duct, which can also affect the success rate of endoscopic removal but are difficult to inspect with preoperative examinations. Despite these disadvantages, this was the first study to construct a noninvasive predictive nomogram to predict ERF when treating submandibular stones preoperatively and that could serve as a reference for surgeons to personalize treatment plans for patients.
The location, transverse diameter and longitudinal diameter of submandibular stones on CBCT images are independent risk factors for ERF. A nomogram based on these three factors helps to predict the risk of ERF for submandibular stones.
Recent studies have found that the favored minimally invasive endoscopic removal, in which clear stones with forceps/baskets, failed to remove submandibular stones in most cases.
To predict the risk of endoscopic removal failure (ERF) for submandibular stones based on their preoperative clinical features.
In the current study, we aimed to construct a predictive model to figure out the risk of ERF for treating submandibular stones before the surgery.
The preoperative clinical data of submandibular stones attempted to be treated by endoscopic removal with forceps/baskets in our department from January 2012 to December 2020 were collected. Correlations between clinical variables of the stones and ERF were explored by Pearson’s chi-squared test. Univariate and multivariate logistic regression analyses were then used to identify the independent risk factors of ERF. Finally, the nomogram based on the independent risk factors was constructed and validated to predict the risk of ERF for individual submandibular stone.
The palpation, location, transverse diameter and longitudinal diameter of submandibular stones were significantly associated with ERF. And the location, transverse diameter and longitudinal diameter of submandibular stones on cone beam computed tomography images were independent factors for ERF with forceps/baskets. A nomogram based on these three factors had satisfying predictive efficiency.
A nomogram based on the location, transverse diameter and longitudinal diameter helps to predict the risk of ERF with forceps/baskets for submandibular stones.
Feasible preoperative measurements of anatomical variations of the Wharton duct are needed to be included in the further study. Also, it is essential to assess the predictive nomogram at multiple institutes with a larger population.
We thank Zhi-Wei Li for his help in statistical analyses.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Dentistry, oral surgery and medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Aoun G, Dawasaz AA S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Nahlieli O, Nakar LH, Nazarian Y, Turner MD. Sialoendoscopy: A new approach to salivary gland obstructive pathology. J Am Dent Assoc. 2006;137:1394-1400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 96] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 2. | Walvekar RR, Bomeli SR, Carrau RL, Schaitkin B. Combined approach technique for the management of large salivary stones. Laryngoscope. 2009;119:1125-1129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 45] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 3. | Zenk J, Koch M, Klintworth N, König B, Konz K, Gillespie MB, Iro H. Sialendoscopy in the diagnosis and treatment of sialolithiasis: a study on more than 1000 patients. Otolaryngol Head Neck Surg. 2012;147:858-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 117] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 4. | Schwartz N, Hazkani I, Goshen S. Combined approach sialendoscopy for management of submandibular gland sialolithiasis. Am J Otolaryngol. 2015;36:632-635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Wolf G, Langer C, Wittekindt C. [Sialolithiasis: Current Diagnostics and Therapy]. Laryngorhinootologie. 2019;98:815-823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Foletti JM, Graillon N, Avignon S, Guyot L, Chossegros C. Salivary Calculi Removal by Minimally Invasive Techniques: A Decision Tree Based on the Diameter of the Calculi and Their Position in the Excretory Duct. J Oral Maxillofac Surg. 2018;76:112-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 7. | Sigismund PE, Zenk J, Koch M, Schapher M, Rudes M, Iro H. Nearly 3,000 salivary stones: some clinical and epidemiologic aspects. Laryngoscope. 2015;125:1879-1882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 84] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 8. | Fabie JE, Kompelli AR, Naylor TM, Nguyen SA, Lentsch EJ, Gillespie MB. Gland-preserving surgery for salivary stones and the utility of sialendoscopes. Head Neck. 2019;41:1320-1327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Nahlieli O. Complications of sialendoscopy: personal experience, literature analysis, and suggestions. J Oral Maxillofac Surg. 2015;73:75-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 40] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 10. | Kondo N, Yoshihara T, Yamamura Y, Kusama K, Sakitani E, Seo Y, Tachikawa M, Kujirai K, Ono E, Maeda Y, Nojima T, Tamiya A, Sato E, Nonaka M. Treatment outcomes of sialendoscopy for submandibular gland sialolithiasis: The minor axis of the sialolith is a regulative factor for the removal of sialoliths in the hilum of the submandibular gland using sialendoscopy alone. Auris Nasus Larynx. 2018;45:772-776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Harrison JD. Causes, natural history, and incidence of salivary stones and obstructions. Otolaryngol Clin North Am. 2009;42:927-947, Table of Contents. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 127] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 12. | Yoshimura Y, Morishita T, Sugihara T. Salivary gland function after sialolithiasis: scintigraphic examination of submandibular glands with 99mTc-pertechnetate. J Oral Maxillofac Surg. 1989;47:704-10; discussion 710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 52] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Walvekar RR, Carrau RL, Schaitkin B. Endoscopic sialolith removal: orientation and shape as predictors of success. Am J Otolaryngol. 2009;30:153-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 24] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Singh PP, Gupta V. Sialendoscopy: introduction, indications and technique. Indian J Otolaryngol Head Neck Surg. 2014;66:74-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Kopeć T, Wierzbicka M, Kałużny J, Młodkowska A, Szyfter W. Sialendoscopy and sialendoscopically-assisted operations in the treatment of lithiasis of the submandibular and parotid glands: our experience of 239 cases. Br J Oral Maxillofac Surg. 2016;54:767-771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Turner MD. Combined Surgical Approaches for the Removal of Submandibular Gland Sialoliths. Atlas Oral Maxillofac Surg Clin North Am. 2018;26:145-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Koch M, Zenk J, Iro H. Algorithms for treatment of salivary gland obstructions. Otolaryngol Clin North Am. 2009;42:1173-1192, Table of Contents. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 103] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 18. | Cox D, Chan L, Veivers D. Prognostic factors for therapeutic sialendoscopy. J Laryngol Otol. 2018;132:275-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Marchal F, Dulguerov P. Sialolithiasis management: the state of the art. Arch Otolaryngol Head Neck Surg. 2003;129:951-956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 233] [Article Influence: 10.6] [Reference Citation Analysis (0)] |