Published online Mar 16, 2022. doi: 10.12998/wjcc.v10.i8.2622
Peer-review started: October 15, 2021
First decision: November 17, 2021
Revised: December 1, 2021
Accepted: February 10, 2022
Article in press: February 10, 2022
Published online: March 16, 2022
Processing time: 146 Days and 16.3 Hours
Teratoma is a common tumor, but rarely occurs in the parotid region. Only nine cases have been reported in the current literature. Although it is generally detected in infancy or childhood, it is commonly asymptomatic. Computed tomography (CT) and magnetic resonance imaging (MRI) have important roles in the diagnosis of teratoma.
A 36-year-old man developed a lump located below the left auricular lobule 3 years ago. Physical examination revealed a nearly-circular tumor in the left parotid gland region with a defined border, firm texture, and significant movement. Calcification, fat, keratinized substances, and typical fat-liquid levels was observed on CT and MRI. A diagnosis of cystic teratoma of the parotid gland was established preoperatively and confirmed by postoperative pathology. Following surgery, the patient developed temporary facial paralysis. There was no recurrence of teratoma during the 15-mo follow-up period.
When an asymptomatic mass in the parotid region is identified, parotid gland teratoma should be included in the differential diagnosis. Imaging examinations are helpful in the diagnosis.
Core Tip: We report an unusual case of teratoma in the parotid gland and review the related literature. The clinical characteristics and imaging features are described. Sufficient knowledge on teratoma, especially the computed tomography and magnetic resonance imaging characteristics, is essential for correct diagnosis and treatment.
- Citation: Liu HS, Zhang QY, Duan JF, Li G, Zhang J, Sun PF. Cystic teratoma of the parotid gland: A case report. World J Clin Cases 2022; 10(8): 2622-2628
- URL: https://www.wjgnet.com/2307-8960/full/v10/i8/2622.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i8.2622
Teratoma is a kind of tumor that develops from germ cells and is most usually found in the coccyx, ovaries, and testicles. Teratoma of the parotid gland, on the other hand, is uncommon. Shadid et al[1] reported the first incidence of teratoma in the parotid gland in 1975. Most parotid gland teratomas develop slowly and have clinical characteristics comparable to other benign parotid gland tumors. We report an unusual case of a giant cystic teratoma, which was located in the deep lobe of the left parotid gland extending into the parapharyngeal space. The diagnosis was made preoperatively by computed tomography (CT) and magnetic resonance imaging (MRI) and was further confirmed by postoperative pathology. The clinical and imaging findings are described. In order to further understand teratoma of the parotid gland, we also review the current literature, hoping to provide a basis for preoperative imaging diagnosis and differential diagnosis, and provide a reliable reference for clinical treatment planning.
A 36-year-old man developed a lump that was accidentally found below the left auricular lobule 3 years ago.
There was no sign of redness, swelling, suppuration, pain, or rupture. The patient had no fever or weight loss during this period. Ultrasonography suggested a cystic lesion of the parotid gland, while CT examination indicated a lipoma at a local hospital. The patient refused tumor excision recommended by the local hospital as the growth was not obvious. However, the lump had grown progressively over the last 6 mo and he occasionally experienced facial discomfort.
The patient denied other medical history.
The patient denied any history of personal or familial diseases.
A nearly-circular tumor with a clear boundary, hard texture, and high mobility was observed in the left parotid gland area. The temperature and color of the surface skin were normal. Facial nerve function was not weakened. No enlarged cervical lymph nodes were found.
No other abnormalities were found on laboratory examinations.
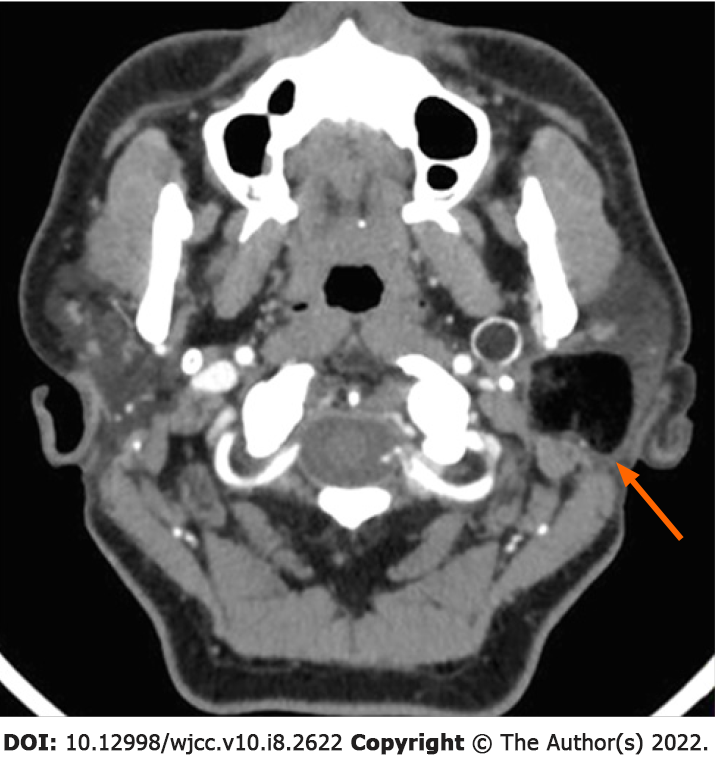
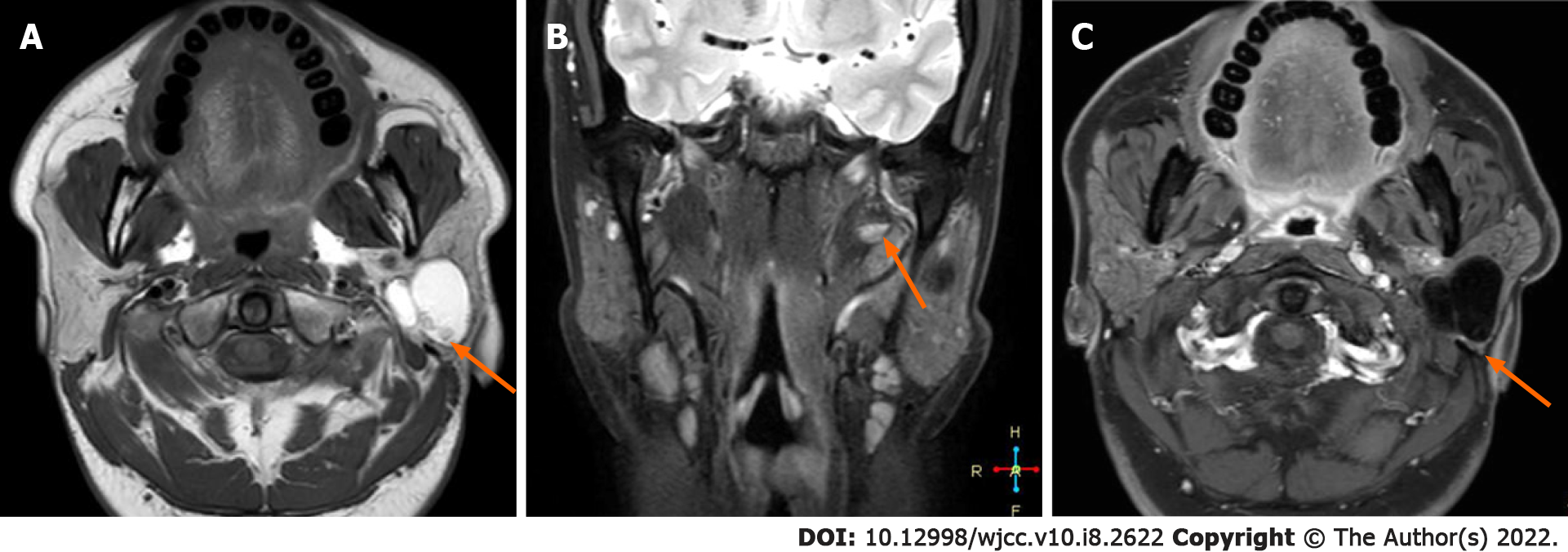
A tumor measuring approximately 3.0 cm x 2.8 cm x 2.9 cm was observed in the deep lobe of the left parotid gland on CT. The tumor was well-bounded and cystic. It comprised variable densities of substances, including a substantial amount of fat and a tiny amount of soft tissue-like parts that were perhaps keratinized. The medial part of the cyst wall was eggshell-like and extended into the parapharyngeal space (Figure 1). The mass on plain and enhanced MRI appeared as two "gourd"-like independent lesions, showing short T1 and long T2 signals, combined with medium T1 and T2 signals and line-like short T2 separation. In the fat saturation sequence, the mass had a complete capsule and a low signal. This was accompanied by lipid levels, which were not significantly enhanced (Figure 2A-C).
The preoperative imaging features suggested a benign lesion, which was further diagnosed as a teratoma of the parotid gland. And it was confirmed by the postoperative pathology.
The patient underwent tumor resection and facial nerve decompression. The tumor was located in the deep lobe of the parotid gland. The cystic wall of the tumor was thick and tough and it was filled with yellow fat-like keratinized substances. As the cyst was very large, some of the contents were extracted. The upper part of the tumor was tightly linked to the cartilage of the external auditory canal. The medial portion of tumor expanded into the deep of styloid process and the lateral skull base. To protect the facial nerve from pressure caused by the tumor, the trunk of the facial nerve was discovered at the root of the mastoid process.
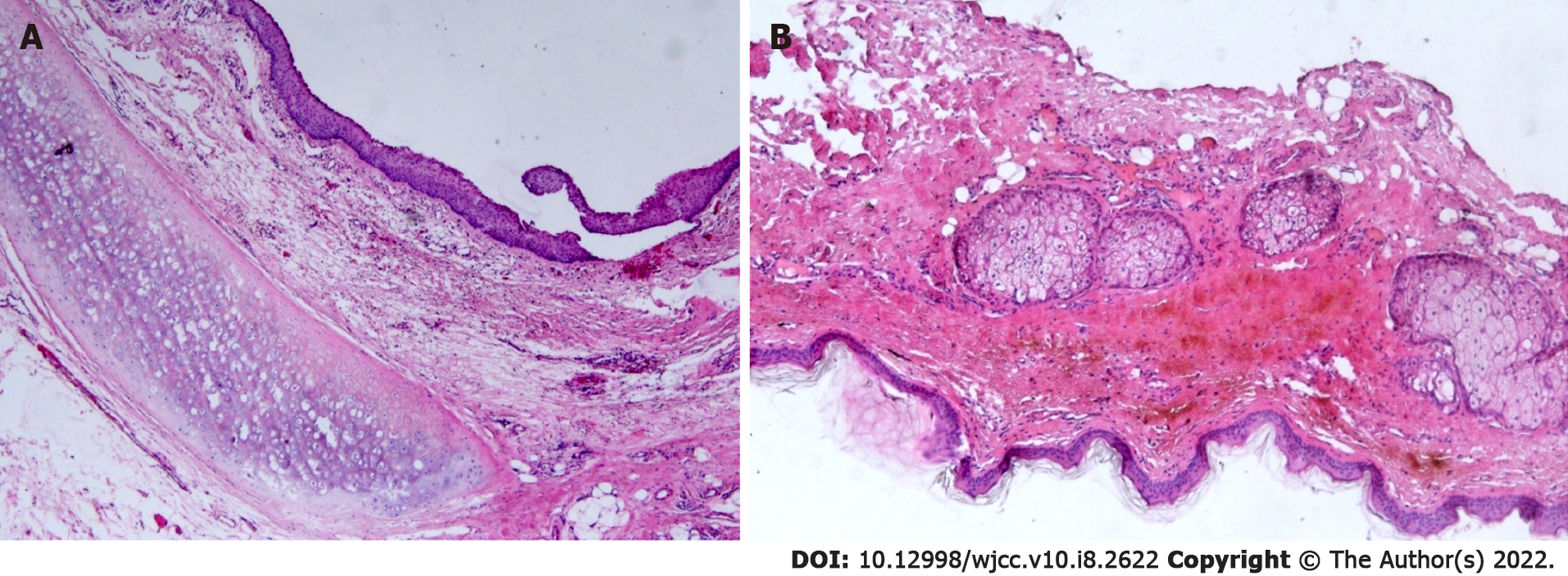
The tumor was completely removed after separation from the external auditory canal, facial nerve, and adjunct tissues. Neither the external auditory canal nor the facial nerve trunk was damaged. The tumor was then sent for pathological examination. In general, the tumor was comprised of sac liquid, and the thickness of the cystic wall was approximately 0.1 mm. The cyst was bordered with stratified squamous epithelium, superficial keratosis, and sebaceous gland cells under the microscope. The fibrous cyst wall contained sebaceous gland cells, cartilage, and adipose tissue. A small amount of keratinous material was found in the cyst cavity. There was no cellular atypia seen, and the surrounding parotid tissues were normal.
The ultimate diagnosis was a mature parotid cystic teratoma (Figure 3A and B). The patient complained of moderate facial paralysis postoperatively which recovered well within 4 mo. There was no recurrence of the teratoma during the 15-mo follow-up period.
Teratoma is a common germ cell tumor that most commonly affects the gonads. It also presents in extragonadal sites, including the sacrococcygeal, retroperitoneal, mediastinal, and pineal regions. In addition, 3% to 5% of teratomas are located in the head and neck[2,3]. However, it rarely occurs in the parotid gland. By reviewing the relevant literature, Only nine individuals with parotid gland teratoma were reported globally between 1975 and 2019 (Table 1)[1,4-11]. Although we made substantial efforts, we failed to access the detailed information of patients 2 and 6. Finally, only eight cases (including the present case) of teratoma in the parotid gland with complete information were analyzed.
| Ref. | Gender | Age (year) | Side/site | Tumor | Preoperative imaging finding | Operation | Postoperative complication | Follow-up/ recurrence |
| Size (cm) | ||||||||
| Shadid EA et al[1], 1975 | Female | 24 | Right, superficial lobe and involving the deep lobe | 1.5 | Cystic | Tumor resection, superficial lobectomy | NA | NA |
| Ayudhya NS et al[4], 1991 | Female | 35 | Left | NA | NA | NA | NA | NA |
| Pirodda A et al[5], 2001 | Female | 18 | Left, posteroinferior of the superficial lobe | 1 | Cystic | Parotidectomy | None | None |
| Wang G D et al[6], 2003 | Female | 21 | Right, superficial lobe | 3.0 × 2.0 | NA | Tumor resection | NA | NA |
| Yang D R et al[7], 2004 | Female | 26 | Right, | 2.0 × 1.5 | Cystic and fat | Tumor resection, parotidectomy | NA | NA |
| Superficial lobe, recurrent | ||||||||
| Oudidi A et al[8], 2007 | NA | NA | NA | NA | NA | NA | NA | NA |
| Ohta M et al[9], 2009 | Female | 17 | Left, superficial lobe | 3 | Cystic and fat | Parotidectomy | NA | 6 mo, none |
| Lenan SHAO et al[10], 2009 | Male | 28 | Right, anterior of the superficial lobe | 2 | Cystic | Tumor resection, parotidectomy | None | 2 years, none |
| Yin RJ et al[11], 2017 | Female | 9 | Left, inferior of the superficial lobe | 3.0 × 2.4 × 3.2 | Cystic | Parotidectomy | NA | NA |
| This report | Male | 36 | Left, deep lobe, extending into the parapharyngeal space | 3.0 × 2.8 × 2.9 | Cystic, fat and calcification | Tumor resection, partial parotidectomy | Moderate facial paralysis, recovered within 4 mo | 15 mo |
| None | ||||||||
Teratomas occur more frequently in females[12]. Approximately 90% of teratomas of the head and neck develop during children or infancy[13], while few develop in adulthood. Of the eight patients, six were female (75.0%), and two were male (25.0%), with a ratio of 3:1. The mean age was 22.3 years (range, 9-36 years). The patient in this case was a 36-year-old male, the oldest of these individuals with parotid gland teratoma to date. All of the individuals had unilateral lesions, with four (50.0%) on the left and four (50.0%) on the right sides. In this case, the lesion was found in the deep lobe of the parotid gland and extended into the parapharyngeal region. However, the superficial lobe of the parotid gland was involved in most cases and extended into the deep lobe in only one case. The maximum diameter of the lesions ranged from 1.0 cm to 3.2 cm. Onset of the lesion ranged from 2 wk to 4 years, with an average of 11 mo. All patients visited the hospital with a painless mass and did not have symptoms such as restricted mouth opening, hearing impairment, or facial nerve paralysis.
Teratomas have the potential to differentiate into somatic cells. According to Batsakis et al[14], most teratomas involve ectoderm, mesoderm, and endoderm components and may differentiate into skin, nerve, bone, and fat tissues. In addition, Teratomas are also either cystic (containing fluids, sebum debris, hair, and fat) or solid (including more complicated tissues). They consist of mature and immature components or both. This helps differentiate teratomas from epidermoid cysts and dermoid cysts. The majority of benign teratomas are cystic and are often referred to as mature cystic teratomas. Ohta et al[9] reported that a mature cystic teratoma might be identified by the presence of skin appendages and cartilage tissues in the cyst wall. In this case, the cyst wall featured a stratified squamous epithelial lining, sebaceous gland cells, hyaline cartilage, and well-differentiated fatty tissues, indicating that it was a mature cystic teratoma. The clinical manifestations of teratoma are usually not typical and the diagnosis mainly depends on imaging examinations, including ultrasonography, CT, and MRI. Ultrasonography commonly shows heterogeneous hyperechoic signals containing multiple components and with an uneven echo. However, it has limitations regarding teratomas located deep in the tissues. CT and MRI are essential for preoperative diagnosis.
On CT, calcification and fat elements are visualized in mature teratomas and the appearance of hypoattenuating fat within the cyst and calcifications in the cyst wall are strongly predictive of teratoma[15]. In addition, the presence of teeth, tufts of hair, and a fat-fluid level is also helpful in the diagnosis of teratoma. MRI allows better observation of soft tissues and is specific for fat signals. As fat contains more hydrogen protons, it shows a high signal on T1WI and T2WI and a low signal in the MRI sequence of fat suppression[16]. This helps to enhance tissue contrast and decrease artifacts, which is important for teratoma detection. The use of CT and MRI can offer a qualitative diagnosis as well as a good view of the lesion's location and scope, as well as its connection to nearby tissues. Calcification, fat, keratinized substances, and the typical fat-liquid levels were observed on CT and MRI in the present study. The lesion looked like a gourd on CT and MRI because it protruded into the parapharyngeal space. Lipoma, dermoid cyst, epidermoid cyst, branchial cleft cyst, vascular tumor, and pleomorphic adenoma must all be separated from teratoma in the parotid gland with atypical imaging features.
Similar to other benign tumors in the parotid gland, surgery is preferred for parotid teratomas. Surgery usually involves partial parotidectomy or total parotidectomy with facial nerve preservation. The extent of parotid resection depends on the location and size of the lesion[10,17]. Studies on postoperative complications are rare, and there was no mention of postoperative complications among the patients observed in previous studies. In the present study, the superficial lobe of the parotid gland was not involved and it was retained during surgery. The patient suffered from temporary moderate facial paralysis (he was not able to completely close his left eyelid) after decompression of the facial nerve. This recovered well postoperatively within 4 mo. Teratoma recurrence in the parotid gland is exceedingly rare. The teratoma recurred in situ in one case, according to the existing literature[7]. Incomplete resection of the tumor might lead to recurrence, which should be avoided. Our patient showed no sign of recurrence during the 15-mo follow-up period and is still being followed.
In summary, teratoma located in the parotid gland is extremely rare. The differential diagnosis of fat in the parotid gland tumor should prompt consideration of the possibility of teratoma. The presence of calcification, fat, and a fat-liquid level on preoperative CT and MRI scans may aid in the diagnosis and localization of a teratoma in the parotid gland. However, histopathological examination is required to confirm the final diagnosis. Surgical removal of a teratoma of the parotid gland is the recommended and successful treatment, and facial nerve function should be preserved. Patients with a parotid teratoma have a fair prognosis, but they should be monitored closely.
We are thankful to the patient and his family for their permission to publish this case report.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Ankrah AO, Ata F, Boscarelli A, Malekzadegan A S-Editor: Ma YJ L-Editor: Wang TQ P-Editor: Ma YJ
| 1. | Shadid EA, Engeron O, Glass RT. Benign teratoid tumor of the parotid; Case report. Plast Reconstr Surg. 1975;55:363-365. [PubMed] |
| 2. | Bergé SJ, von Lindern JJ, Appel T, Braumann B, Niederhagen B. Diagnosis and managementof cervical teratomas. Br J Oral Maxillofac Surg. 2004;41-45. [RCA] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Stricker TP, Kumar V, Neoplasia In, Abbas AK, Fausto N, Ster JC. Robbins and Cotran pathologic basis of disease. 8th ed. Philadelphia (PA): Elsevier Saunders. 2010. [DOI] [Full Text] |
| 4. | Ayudhya NS, Parichatikanond P, Chinda K. Benign cystic teratoma of the parotid salivary gland: report of the first case in Thailand. J Med Assoc Thai. 1991;74:478-480. [PubMed] |
| 5. | Pirodda A, Ferri GG, Truzzi M, Cavicchi O. Benign cystic teratoma of the parotid gland. Otolaryngol Head Neck Surg. 2001;125:429-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Wang GD, He Y. Teratoma of the parotid gland: a case report. Bengbu Yixueyuan Xuebao. 28:470. |
| 7. | Yang DR, Xu HM, Long QX. Mature cystic teratoma of the parotid gland: a case report. Zhenduan Binglixue Zazhi. 2004;11:237. |
| 8. | Oudidi A, Alami MN. [Teratoma of the parotid gland: a case report]. Rev Laryngol Otol Rhinol (Bord). 2007;128:125-127. [PubMed] |
| 9. | Ohta M, Imamura Y, Mori M, Maegawa H, Kojima A, Fujieda S. Benign cystic teratoma of the parotid gland: a case report. Acta Cytol. 2009;53:427-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Shao L, Guan H, Wan J. Mature cystic teratoma of the parotid gland: a case report and review of the literature. Frontiers of Med. 2009;3:503-506. [DOI] [Full Text] |
| 11. | Yin RJ, Zhao W, XJ S. A case of cystic teratoma in the parotid gland diagnosed by MRI. J Clin Radiol 2017; 36: 446. [DOI] [Full Text] |
| 12. | Li H, Zhao T, Wei Q, Yuan H, Cao D, Shen P, Liu L, Zeng H, Chen N. Laparoscopic resection of a huge mature cystic teratoma of the right adrenal gland through retroperitoneal approach: a case report and literature review. World J Surg Oncol. 2015;13:318. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Jordan RB, Gauderer MW. Cervical teratomas: an analysis. Literature review and proposed classification. J Pediatr Surg. 1988;23:583-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 99] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 14. | Batsakis JG. Teratomas of the head and neck. In: Tumors of the head and neck: clinical and pathological considerations. 2nd ed. Baltimore: Williams & Wilkins. 1979: 226-232. [DOI] [Full Text] |
| 15. | Yang DM, Jung DH, Kim H, Kang JH, Kim SH, Kim JH, Hwang HY. Retroperitoneal cystic masses: CT, clinical, and pathologic findings and literature review. Radiographics. 2004;24:1353-1365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 258] [Cited by in RCA: 242] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 16. | Chai J, Jin EH. Recent status on MRI chemical shift imaging in quantitative analysis of ectopic fat deposition in vivo. J Clin Exp Med. 2013;12: 2027-2230. [RCA] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Tapper D, Lack EE. Teratomas in infancy and childhood. A 54-year experience at the Children's Hospital Medical Center. Ann Surg. 1983;198:398-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 238] [Article Influence: 5.7] [Reference Citation Analysis (0)] |