Published online Mar 16, 2022. doi: 10.12998/wjcc.v10.i8.2584
Peer-review started: September 13, 2021
First decision: November 22, 2021
Revised: November 25, 2021
Accepted: February 10, 2022
Article in press: February 10, 2022
Published online: March 16, 2022
Processing time: 178 Days and 19.7 Hours
Atypical spindle cell lipomatous tumor (ASLT) is a rare soft tissue neoplasm with a low potential for malignancy. ASLT frequently occurs in the limb and limb girdles. However, large retroperitoneal ASLTs are extremely rare. There was no concrete case report of retroperitoneal ASLTs.
An 18-year-old woman presented with abdominal pain and a palpable mass. Abdominal computed tomography revealed a large fatty mass that was approximately 30 cm in size and filled the entire abdominal cavity. Surgical excision was indicated. The tumor did not invade the adjacent organs. The pelvic cavity was then too narrow to dissect smoothly. The mass was successfully excised without tumor rupture or adjacent organ injury. Microscopically, the neoplasm was a well-differentiated adipocytic neoplasm. Immunohistochemical staining showed that the spindle cells were positive for CD34 and desmin, in addition to multifocal positivity for S100 protein. These histological features were consistent with an ASLT. The patient’s postoperative course was uneventful. At the 12-mo follow-up, no evidence of recurrence or metastasis was observed.
To the best of our knowledge, our study is the first concrete report of a large retroperitoneal ASLT in the English literature. In the large retroperitoneal ASLT located in the pelvic cavity, which made it too narrow and tight to dissect, complete excision is difficult but very important because of recurrence risk. Although large retroperitoneal ASLTs are considered extremely rare, their detection is important for accurate evaluation and management. Owing to their significant rarity, retrospective multicenter case studies are required to determine the clinicopathologic characteristics.
Core Tip: To the best of our knowledge, our study is the first concrete report of a large retroperitoneal atypical spindle cell lipomatous tumor (ASLT) in the English literature. ASLT is a rare soft tissue neoplasm. Additionally, retroperitoneal ASLT is extremely rare. In the large retroperitoneal ASLT located in the pelvic cavity, which made it too narrow and tight to dissect, complete excision is difficult but very important because of recurrence risk.
- Citation: Bae JM, Jung CY, Yun WS, Choi JH. Large retroperitoneal atypical spindle cell lipomatous tumor, an extremely rare neoplasm: A case report. World J Clin Cases 2022; 10(8): 2584-2590
- URL: https://www.wjgnet.com/2307-8960/full/v10/i8/2584.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i8.2584
Atypical spindle cell lipomatous tumor (ASLT) is a rare soft tissue neoplasm with a low potential for malignancy or benign characteristics. To date, its etiology remains unknown. ASLT was first described in 1994[1], and for several decades, its diagnosis has been controversial and remains challenging. Recently, a diagnostic consensus has been reached[2].
According to a previous large case study, ASLT frequently occurs in the limb and limb girdles in two-thirds of cases, with a predilection for the hands and feet. However, large retroperitoneal ASLTs are extremely rare. Because of the tight pelvic cavity in the present case, surgical excision was very difficult.
In our study, we present the case of an 18-year-old woman diagnosed with a large retroperitoneal ASLT. Despite the surgical difficulty, the postoperative course was uneventful, and no evidence of recurrence or metastasis was observed at the 12-mo follow-up.
We also conducted a review of the literature. To the best of our knowledge, this is the first concrete report of a large retroperitoneal ASLT in the English literature.
This study was approved by the Institutional Review Board (IRB) of Yeungnam University Medical Center (IRB No. 2021-06-020). The patient provided written informed consent for the publication of the case details at admission.
An 18-year-old asian woman presented to our surgery department with abdominal pain, discomfort, and a palpable mass.
About several months previously, this patient felt abdominal discomfort. However, this patient did not further evaluation.
The patient had no other previous medical history.
The patient had no personal or family history of similar illnesses.
The initial blood pressure was 120/80 mmHg; heart rate, 86 beats/minute; respiratory rate, 14 breaths/minute; and body temperature, 36.9 °C at admission.
Her bowel sounds were normoactive and regular. Physical examination revealed non-specific tenderness throughout the abdomen. However, a very large mass was palpated from the epigastric area to the pelvic area.
The initial laboratory examination revealed normal levels of leukocytes and hemoglobin.
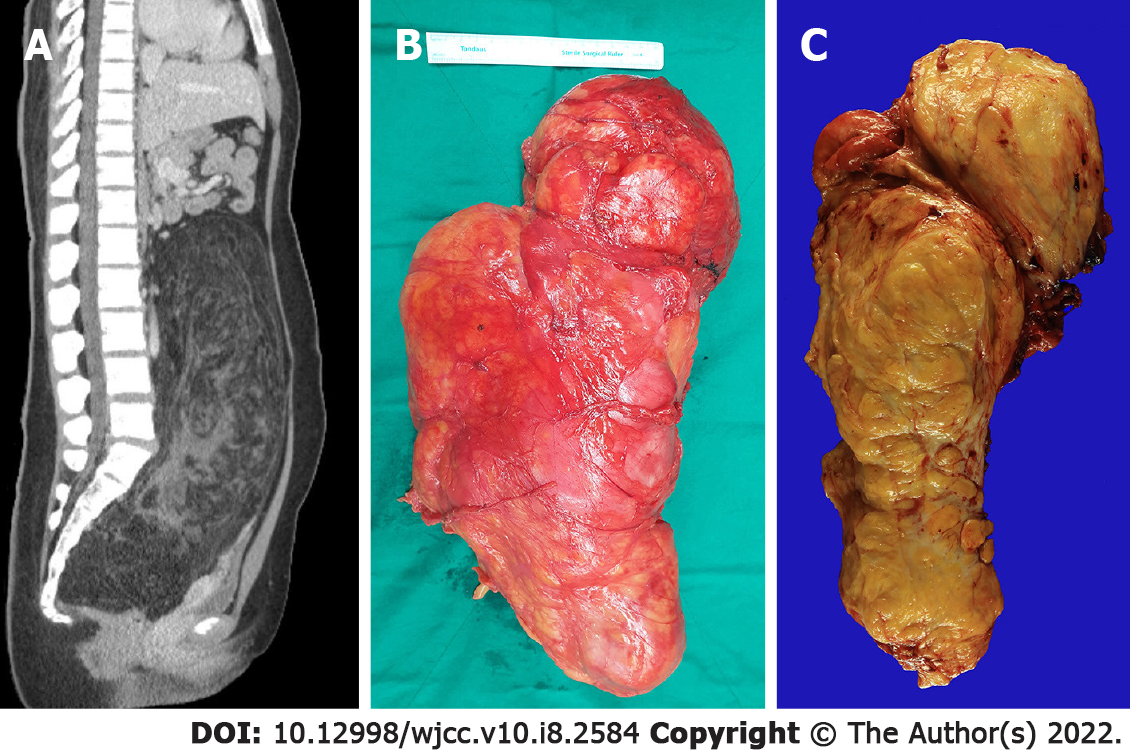
Abdominal computed tomography revealed a large fatty mass with a complex soft tissue component. The tumor was approximately 30 cm × 20 cm × 10 cm in size and filled the entire abdominal cavity (Figure 1A). The tumor pushed up the abdominal viscera from the pelvic cavity.
The results led us to consider retroperitoneal neoplasm, including retroperitoneal liposarcoma.
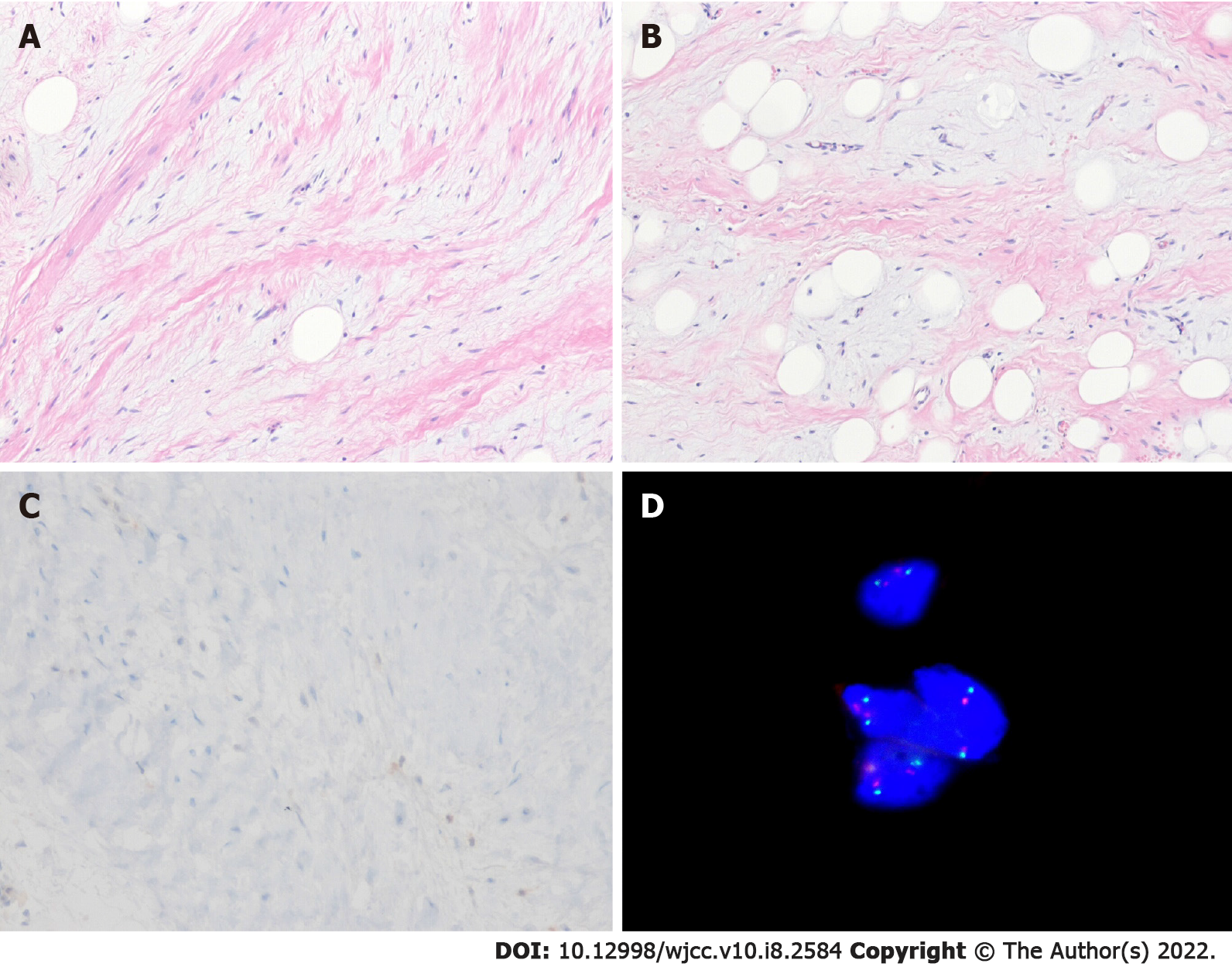
Microscopically, the neoplasm was a well-differentiated adipocytic neoplasm with a variable myxoid or collagenous stroma, and the pathologic margin was negative. Delicate and ropey collagen bundles were observed. There was an admixed spindle cell component that showed mild nuclear atypia and hyperchromatia, greater than that usually seen in a benign lipoma, but lesser than that usually seen in a well-differentiated liposarcoma. Immunohistochemical staining showed that the spindle cells were positive for CD34 and desmin, in addition to multifocal positivity for S100 protein, but were negative for MDM2. FISH analysis (fluorescence in situ hybridization) shows no MDM2 amplification (Figure 2). Rb staining revealed positive findings, that is, normal/retained status.
A final diagnosis is ASLT in retroperitoneum based on the immnohistocheminal staining and FISH analysis of the tumor tissue.
Surgical excision was indicated, and elective exploration was performed thereafter. Laparotomy revealed a huge retroperitoneal tumor. The abdominal organs were normal. The tumor did not invade the adjacent organs. However, it extended to the pelvic cavity and severely attached to the anterior surface of the coccyx and sacrum; the pelvic cavity was then too narrow to dissect smoothly. The peritumoral dissection in pelvic cavity was very difficult and the dissection was performed little by little dissection manner in both lateral pelvic wall surface, anterior coccyx surface and posterior pubic ramus surface. Intra-operative bleeding amount was about 700cc. However, no transfusion was performed in post-operative periods.
Therefore, the surgery was performed for 8 h. The mass was successfully excised without tumor rupture or adjacent organ injury. Gross and microscopic examinations in frozen section biopsy revealed negative surgical margins. The tumor weighed approximately 5000 g, had an egg-shaped appearance, and was 38 cm × 24 cm × 11.5 cm in size (Figure 1B).
The cut surface showed a large fatty mass with diffuse heterogeneous fibrotic change. No hemorrhage or necrosis was observed (Figure 1C).
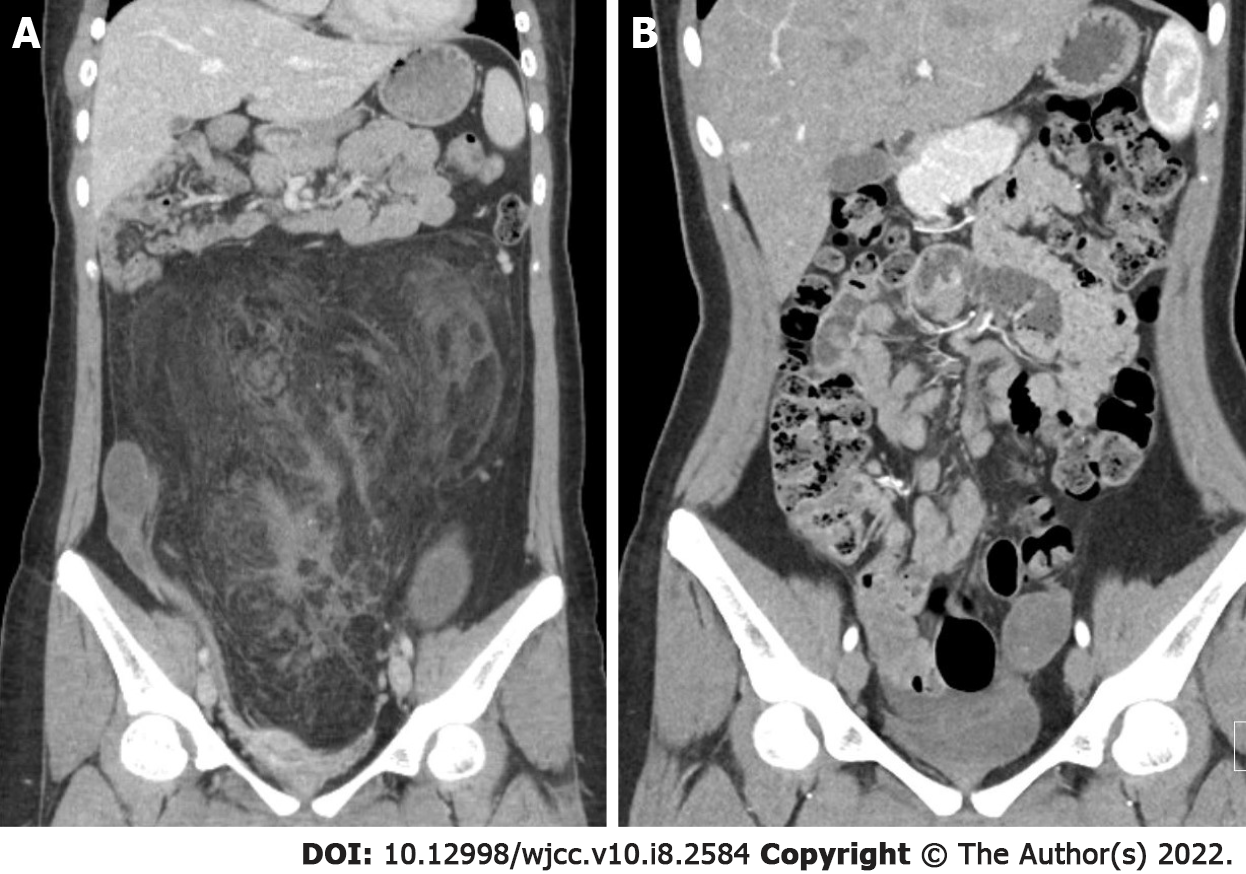
The patient’s postoperative course was uneventful, and recovery after surgery was satisfactory; at the 12-mo follow-up, no evidence of recurrence or metastasis was observed (Figure 3). At the time of preparation of this article, the patient is alive and well.
ASLT was first described in 1994[1]. It was previously called spindle cell liposarcoma, differentiated spindle cell liposarcoma, and atypical spindle cell lipoma. Although its diagnosis has been controversial and remains challenging for some time, consensus that ASLT is a subtype of spindle cell lipoma with features different from those of atypical lipoma-like tumor/well-differentiated liposarcoma has been reached[2]. In 2017, researchers suggested that ASLT and atypical pleomorphic lipomatous tumor (APLT) belong to the same morphologic spectrum, named atypical spindle cell/pleomorphic lipomatous tumor (ASPLT)[3]. Additionally, ASPLT is described in the 5th edition of the World Health Organization (WHO) classification of soft tissue and bone tumors in 2020[4]. Although ASPLT has similar clinicopathologic and biological features, ASLT and APLT have different morphological spectra[3].
According to the largest series on ASLTs, the male-to-female sex ratio was 3:2, and the median patient age was 54 years[2]. ASLT develops in the limb and limb girdles in two-thirds of cases, with a predilection for the hands and feet and an approximately equal distribution between superficial and deep sites. They less commonly occur in the head and neck, genitals, and trunk, with very rare retroperitoneal involvement[2].
The mean size of reported tumors ranges from 5 to 8.5 cm[5]. However, our case developed a tumor in the retroperitoneum with a size of 38 cm.
Interestingly, the clinical findings of our case, including the patient’s age and sex and tumor location and size, are different from the previously published characteristics of ASLT[2].
The frequent clinical manifestations of ASLT are persistent or enlarged soft tissue masses, nodules, or swelling, sometimes with tenderness. The rare clinical complaints include skin ulceration, local pain, cutaneous vascular markings, cough and hemoptysis, proptosis, night sweats, and abdominal discomfort[2].
Microscopically, the ASLT in our case consisted of a poorly marginated proliferation of mildly atypical spindle cells set in a fibrous or myxoid stroma, with a variably prominent admixed adipocytic component showing variation in adipocyte size and scattered nuclear atypia, frequently with univacuolated or multivacuolated lipoblasts. Tumor cellularity and the relative proportions of the different components highly varied[2].
Although the tumor margins in ASLT are often ill defined with invasion to the surrounding tissues[2], no such invasion was observed in our case.
The definite diagnosis of atypical adipocytic neoplasm with spindle cell features remains challenging for several decades. Recently, a diagnostic consensus has been reached owing to a better biological understanding with substantial contributions from cytogenetics, molecular genetics, and immunohistochemical correlates[2].
CD34 expression is often observed in ASLTs, which is helpful for diagnosis[2,3,5]. Rb protein expression loss is present in 57% of ASLT[2]. In a previous study, the diagnostic sensitivity of CD34 was 64%, and MDM2 expression was not observed in ASLT. Weak and/or focal expression of MDM2 or CDK4 is occasionally present but is always present in the absence of genomic amplification[2].
Molecular studies have shown deletions or losses of 13q14, including RB1 and its flanking genes RCBTB2, DLEU1, and ITM2B in a significant subset of atypical spindle cell/pleomorphic lipomatous tumors and a consistent absence of MDM2 amplification[2,3,6].
In addition, monosomy 7 has been reported in some cases[7].
In our case, MDM2 expression was negative, and amplification was absent. The negativity of MDM2, CDK4, and FISH for MDM2 amplification highlights critical biological differences between ASLT and dedifferentiated liposarcoma[2,5].
ASLTs can show a wide variety of microscopic features, and differential diagnosis is important and difficult. In our review, differential diagnosis of spindle cell-poor to spindle cell-rich variant of ASPLT was introduced[5]. The spindle cell-associated variants were spindle cell/pleomorphic lipoma, atypical lipomatous tumor/well-differentiated liposarcoma, dedifferentiated liposarcoma, pleomorphic liposarcoma, mammary-type myofibroblastoma, cellular angiofibroma, and solitary fibrous tumors.
The treatment of ASLT involves complete excision, similar to other soft tissue malignant neoplasms. In a large retrospective series, the local recurrence rate was approximately 12%. However, distant metastases were not observed. When complete excision was performed, further oncologic treatment was not required. In previous studies, preoperative or postoperative chemotherapy and radiotherapy were performed in several patients. However, the effectiveness or necessity of chemo
ASLT is classified as a benign neoplasm according to the 2020 WHO classification of tumors of soft tissue and bone[4]. However, several researchers believe that ASLT has a low potential for malignancy or has an intermediate biological potential[2]. Therefore, in our case of a large retroperitoneal ASLT located in the pelvic cavity, which made it too narrow and tight to dissect, complete excision is difficult but very important. Therefore, the surgeon should excise and dissect the tumor carefully without tumor spillage.
According to a large retrospective series, tumor recurrence may develop from 6 mo after the initial surgery; nevertheless, recurrence-related death may not be observed[2].
As mentioned above, large retroperitoneal ASLTs are extremely rare. In the largest series of ASLT cases, retroperitoneal ASLT was found in only two patients. However, the clinical data of these two retroperitoneal ASLT cases, including the patients’ age and sex, tumor size, and prognosis, were not available. Therefore, to the best of our knowledge, our study is the first concrete report of a large retroperitoneal ASLT in the English literature.
In conclusion, our study presents a case of a large retroperitoneal ASLT treated with complete excision. In the large retroperitoneal ASLT located in the pelvic cavity, which made it too narrow and tight to dissect, complete excision is difficult but very important. Although large retroperitoneal ASLTs are considered extremely rare, their detection is important for accurate evaluation and management. Owing to their significant rarity, retrospective multicenter case studies are required to determine the clinicopathologic characteristics.
Provenance and peer review: Unsolicited article; externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Higashida-Konishi M, Li BL, Liu C S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Dei Tos AP, Mentzel T, Newman PL, Fletcher CD. Spindle cell liposarcoma, a hitherto unrecognized variant of liposarcoma. Analysis of six cases. Am J Surg Pathol. 1994;18:913-921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 111] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 2. | Mariño-Enriquez A, Nascimento AF, Ligon AH, Liang C, Fletcher CD. Atypical Spindle Cell Lipomatous Tumor: Clinicopathologic Characterization of 232 Cases Demonstrating a Morphologic Spectrum. Am J Surg Pathol. 2017;41:234-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 111] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 3. | Creytens D, Mentzel T, Ferdinande L, Lecoutere E, van Gorp J, Atanesyan L, de Groot K, Savola S, Van Roy N, Van Dorpe J, Flucke U. "Atypical" Pleomorphic Lipomatous Tumor: A Clinicopathologic, Immunohistochemical and Molecular Study of 21 Cases, Emphasizing its Relationship to Atypical Spindle Cell Lipomatous Tumor and Suggesting a Morphologic Spectrum (Atypical Spindle Cell/Pleomorphic Lipomatous Tumor). Am J Surg Pathol. 2017;41:1443-1455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 86] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 4. | Sbaraglia M, Bellan E, Dei Tos AP. The 2020 WHO Classification of Soft Tissue Tumours: news and perspectives. Pathologica. 2021;113:70-84. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 554] [Article Influence: 110.8] [Reference Citation Analysis (0)] |
| 5. | Lecoutere E, Creytens D. Atypical spindle cell/pleomorphic lipomatous tumor. Histol Histopathol. 2020;35:769-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 6. | Creytens D, van Gorp J, Savola S, Ferdinande L, Mentzel T, Libbrecht L. Atypical spindle cell lipoma: a clinicopathologic, immunohistochemical, and molecular study emphasizing its relationship to classical spindle cell lipoma. Virchows Arch. 2014;465:97-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Italiano A, Chambonniere ML, Attias R, Chibon F, Coindre JM, Pedeutour F. Monosomy 7 and absence of 12q amplification in two cases of spindle cell liposarcomas. Cancer Genet Cytogenet. 2008;184:99-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.3] [Reference Citation Analysis (0)] |