Published online Mar 16, 2022. doi: 10.12998/wjcc.v10.i8.2516
Peer-review started: July 25, 2021
First decision: October 25, 2021
Revised: November 25, 2021
Accepted: January 29, 2021
Article in press: January 29, 2022
Published online: March 16, 2022
Processing time: 228 Days and 11.2 Hours
There are few reports of a fractured esophageal self-expanding metallic stent (SEMS) and the lasso retrieval technique, forming a guidewire loop by directing the guidewire back up the external stent for retrieval.
A 74-year-old man complained of dysphagia approximately 6 mo after radical resection of esophageal cancer. Benign anastomotic stenosis was diagnosed, and a 20 mm in diameter and 60 mm in length esophageal covered SEMS was inserted after repeated balloon dilatation. About 13.5 mo after stenting, dysphagia recurred and esophagography showed severe stenosis above the proximal stent and stent removal was performed. One-third of the stent was removed and the fractured stent remained in the proximal esophagus. A suction tube was introduced through the guidewire and then the guidewire was grabbed, acting like a “lasso” on tightening. The remaining fractured stent was successfully removed by slowly pulling back the guidewire, with no fragments of stent wires retained.
The guidewire lasso technique is a simple, effective method of removing esophageal SEMS in rare cases of stent fracture.
Core Tip: We present a case in which the guidewire lasso technique was used to remove a fractured esophageal Z-stent. A 74-year-old man developed dysphagia approximately 6 mo after resection for esophageal cancer and a Z stent was inserted. After 13.5 mo, esophagography showed severe stenosis above the proximal stent. One-third of the stent was removed and the fractured stent remained in the proximal esophagus. A suction tube was introduced through the guidewire and then the guidewire was grabbed, acting like a “lasso” on tightening. The fractured stent was successfully removed by slowly pulling back the guidewire, with no fragments of stent wires retained.
- Citation: Bi YH, Ren JZ, Li JD, Han XW. Fluoroscopic removal of fractured, retained, embedded Z self-expanding metal stent using a guidewire lasso technique: A case report. World J Clin Cases 2022; 10(8): 2516-2521
- URL: https://www.wjgnet.com/2307-8960/full/v10/i8/2516.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i8.2516
Covered esophageal stents are mainly reserved for malignant indications, such as esophageal stricture or fistula caused by esophageal cancer. Self-expanding metallic stent (SEMSs) have not been widely used in patients with benign dysphagia due to their expected long-term complications[1,2]. SEMSs may serve as a routine option for the management of refractory benign stenosis if they can be timely and safely retrieved within 2 to 3 mo[3] or before excessive epithelial hyperplasia develops[1]. There are few reports of a fractured esophageal SEMS and the lasso retrieval technique, in which a guidewire loop is formed by directing the guidewire back up the external stent for retrieval. We present a case in which this technique was used to remove a fractured esophageal Z-stent.
A 74-year-old man developed aggravation of dysphagia approximately 13.5 mo after stent insertion following resection of esophageal cancer 6 mo previously.
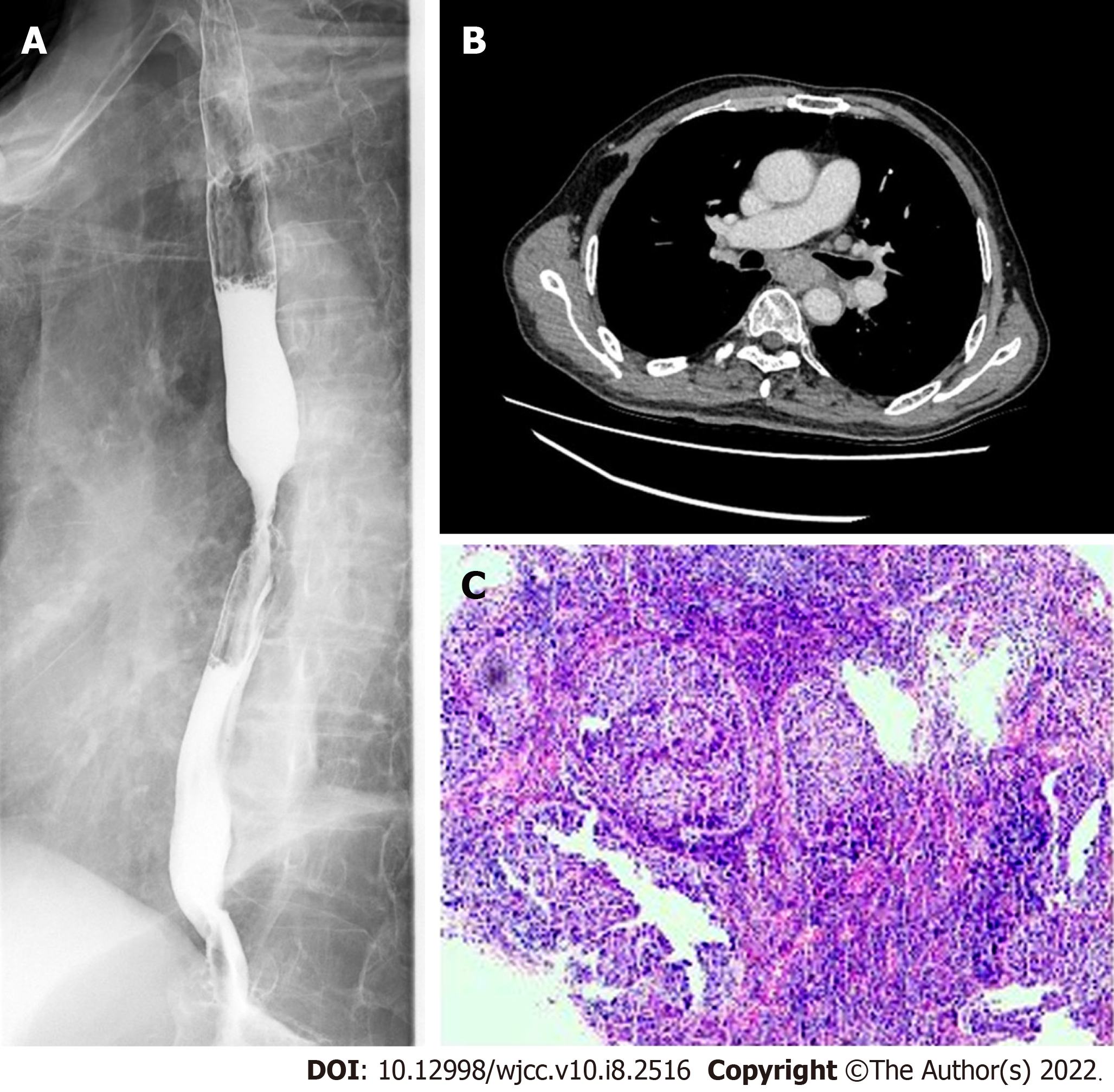
The patient gradually developed dysphagia 21 mo ago. Esophagography and a chest contrast-enhanced computed tomography (CT) scan showed a tumor located in the middle and lower part of the esophagus (Figure 1A and B). Esophageal gastroscopy examination was performed and biopsy pathology confirmed esophageal squamous cell carcinoma (Figure 1C). Radical resection of esophageal cancer was performed 19.5 mo ago under general anesthesia. The patient complained again of dysphagia about 13.5 mo ago and benign anastomotic stenosis was diagnosed. A 20 mm in diameter and 60 mm in length esophageal covered SEMS was inserted after repeated balloon dilatation. The retrievable Z-stents are made of stainless steel and coated with silicon (Sigma Medical Industry Co., Ltd., Huaian, Jiangsu Province, China). Two weeks ago, the symptoms of dysphagia were significantly aggravated and esophagography showed severe stenosis above the proximal stent.
The patient had mild coronary heart disease for 15 years, but did not take medication.
The patient had no history of smoking, drinking, or familial cancers.
Vital signs were as follows: Body temperature 36 ℃, pulse 88 bpm, respiration 22 breaths/min, blood pressure 99/69 mmHg, height 169 cm, and body weight 50.0 kg. Oxygen saturation in room air was 99%.
Routine blood tests showed the following: Leukocyte count 4.73 × 109/L, erythrocyte count 3.80↓ × 1012/L, hemoglobin 117.0 g/L↓↓, Platelet count 202 × 109/L, neutrophil percentage 75.6%↑, and lymphocyte percentage 15.7%.
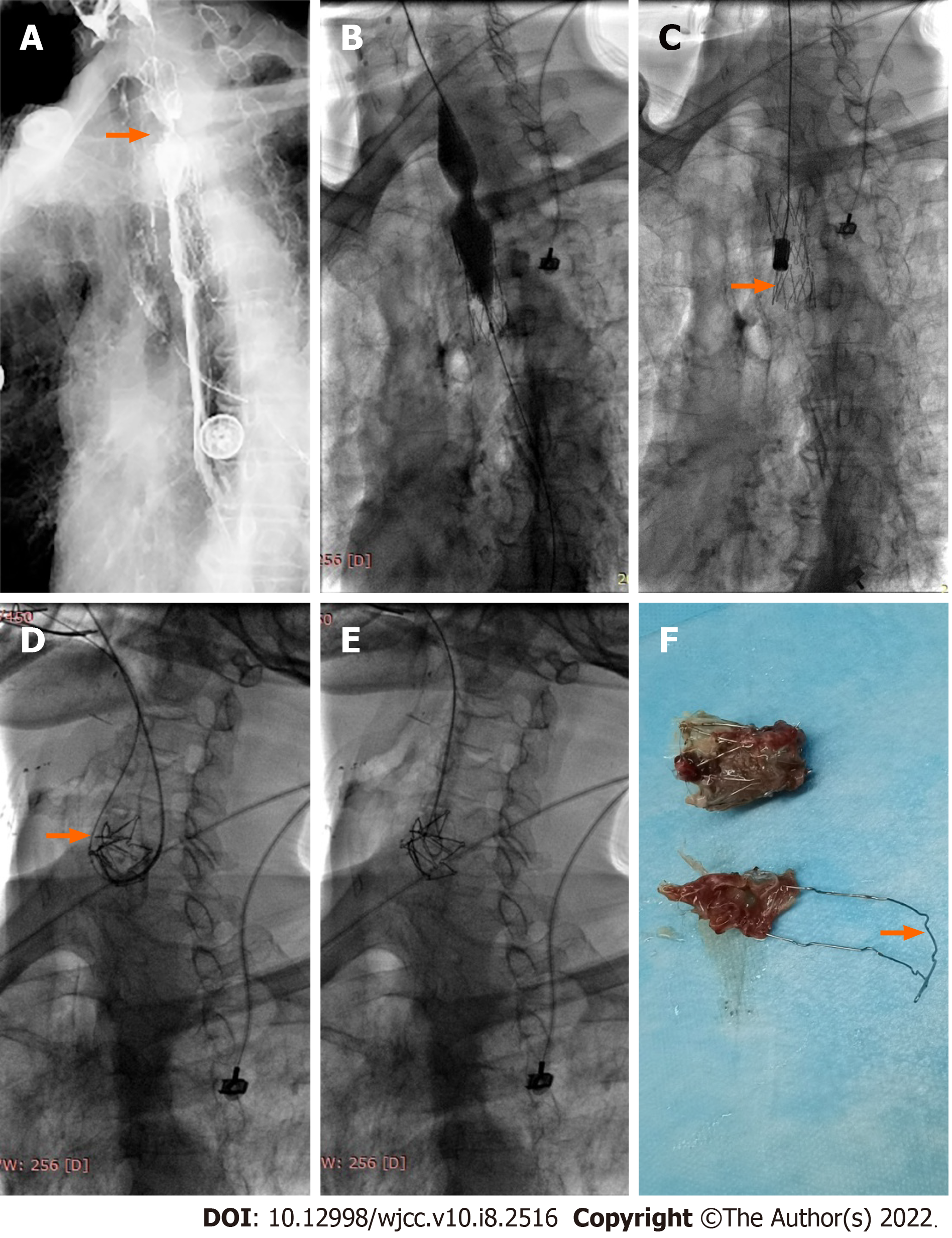
Severe stenosis above the proximal stent was diagnosed by esophagography (Figure 2A). Removal of the stent was decided due to aggravated dysphagia after repeated balloon dilation.
The final diagnosis of the case presented was severe benign anastomotic stenosis above the proximal stent.
Two days after admission, esophageal balloon dilatation and stent removal was performed under fluoroscopy. The procedure was as follows: The patient lay supine on the operating table; 10 mL of iodine contrast agent was administered orally. After local mucosal anesthesia, an opener was placed in the mouth. A 5F single curved catheter and 0.035-inch guidewire was introduced and passed through the esophageal stent. An AMPLAZ stiff guidewire was exchanged and a 20 mm in diameter and 40 mm in length balloon catheter (Cook Medical, Bloomington, IN, United States) was introduced to dilate the stenotic segment (Figure 2B). After withdrawing the catheter, the stent removal sheath was introduced and then the removal hook was placed in the lower part of the stent in order to remove the whole stent (Figure 2C).
Because the stent was embedded in proliferative tissue, it fractured during the removal process. After the application of considerable traction to the distal end of the stent, only one-third of the stent was removed and the fractured stent remained in the proximal esophagus. We failed to remove the retained stent using the same method again.
A 0.035-inch guidewire was introduced and passed over the retained stent and looped back from the stent to the mouth (Figure 2D). A suction tube was introduced through the guidewire and then the guidewire was grabbed, acting like a “lasso” on tightening (Figure 2E). Under fluoroscopy, the fractured stent was successfully removed by slowly pulling back the guidewire, with no fragments of stent wires retained. Proliferative tissue could be seen in the removed stent and the strut was deformed (Figure 2F). Mild bleeding occurred during the procedure, and epinephrine was administered orally for hemostasis.
Reexamination showed that stenosis was no longer present and there was no overflow of contrast agent. The patient complained of mild postoperative pharyngeal pain which did not require treatment, and dysphagia symptoms disappeared so that he could eat. After a total of 4-d of hospitalization the patient was discharged.
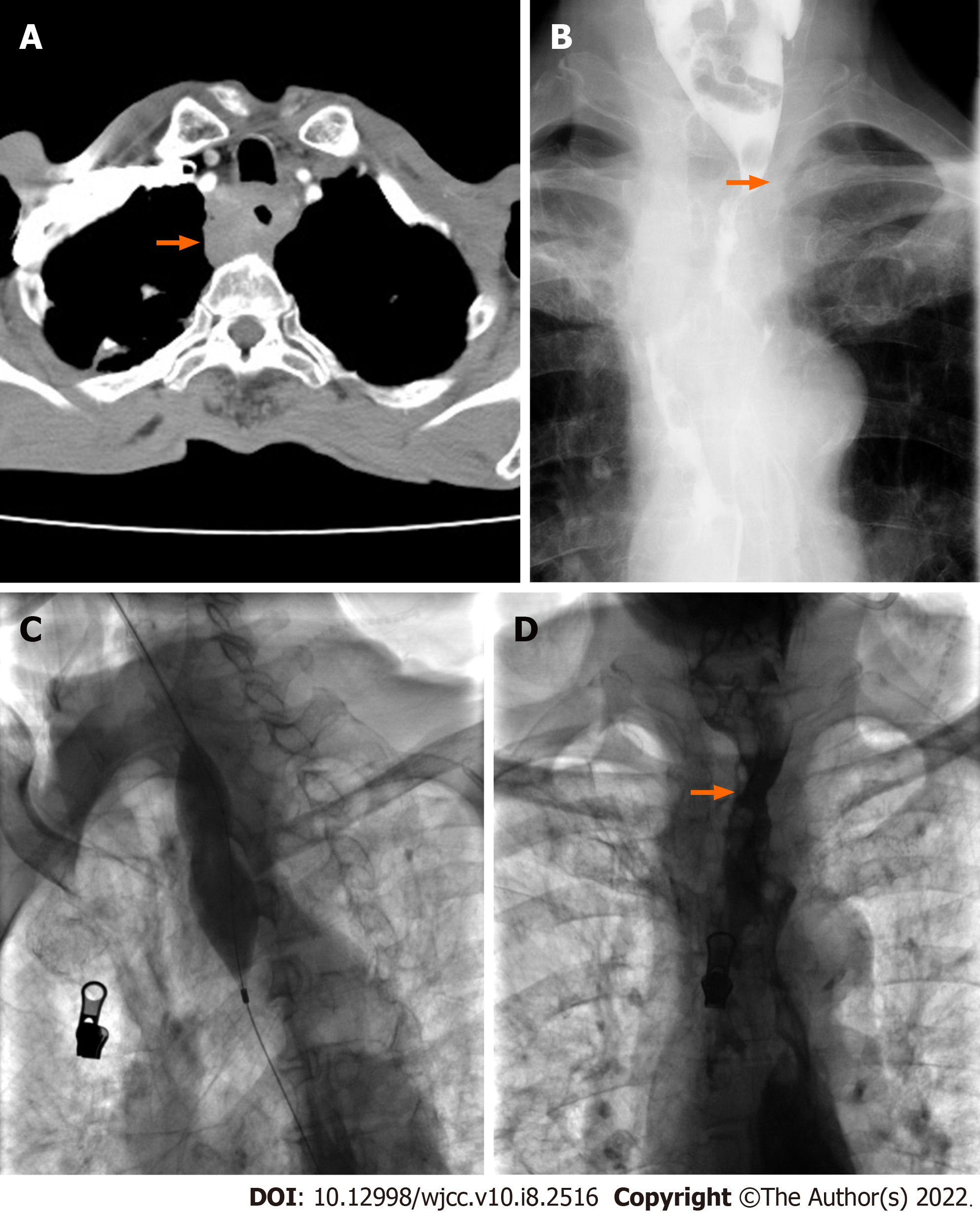
The patient complained of dysphagia again about 40 d later. A chest contrast-enhanced CT examination and esophagography showed severe stenosis in the proximal part of the esophagus (Figure 3A and B). A 28 mm in diameter and 40 mm in length big balloon catheter (Cook) was used to dilate the stenotic section (Figure 3C). Esophagography showed that the stenosis disappeared after dilation (Figure 3D) and the patient did not complain of dysphagia thereafter.
Covered esophageal stents are mainly reserved for malignant indications, such as esophageal stricture or fistula caused by esophageal cancer. The ability of SEMSs to relieve dysphagia effectively in patients with malignancy is accepted generally. SEMSs have not been widely used in patients with benign dysphagia due to their expected long-term complications. Due to pressure necrosis caused by SEMS expansion, the bare ends are routinely incorporated into the esophageal mucosa and then covered by pseudomembrane[1]. Benign granulation tissue hyperplasia may extend into the deeper layers of the esophageal wall and increase the possibility of formation of secondary obstruction formation[1,2]. Esophageal resection may be required due to severe stricture after stent placement in benign disease[3]. Additional stent placement or laser ablation are routine management options if granulation tissue overgrowth occurs in patients with malignancy. However, other options can be used in patients with benign disease[4].
A SEMS may serve as a routine option for the management of refractory benign stenosis if the retrievable stents can be safely retrieved within 2 to 3 mo[4] or before excessive epithelial hyperplasia develops[1]. Esophageal stent removal methods should be varied according to the different types of SEMS, including the endoscopic removal technique of multiple SEMS in certain cases, such as both Z-stents and Ultraflex stents. Previous studies have reported the removal of SEMSs for inappropriate insertion or stent migration. For example, Mallery and Freeman[5] removed an Ultraflex stent with distal-to-proximal invagination into an overtube. However, this method was unable to extract a similar stent one month after deployment. The Ultraflex stent is more flexible than other brands including the Gianturco and Wallstent stents; thus, this removal technique may not be applicable for various types of SEMSs.
Fragments of stent wires are commonly retrieved endoscopically with grasping forceps. There are few reports of a fractured esophageal SEMS and the lasso retrieval technique in which a guidewire loop is formed by directing the guidewire back up the external stent for retrieval. This technique has been used successfully to extract a migrated colonic stent[6], as well as an esophageal SEMS that had migrated into the stomach[7]. The Z stents may be best removed by polyp snare rather than invagination removal from distal to proximal ends. Our report describes a stent retrieval method that can be performed in selected cases of benign disease in which stent fracture has occurred.
This case validates that the guidewire lasso technique is a simple and effective method of removing esophageal SEMSs in rare cases in which stent fracture occurs. The ability to retrieve fractured and retained Z-stents may facilitate broader stent applications.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ozdemir HI S-Editor: Xing YX L-Editor: Webster JR P-Editor: Xing YX
| 1. | Vakil N, Gross U, Bethge N. Human tissue responses to metal stents. Gastrointest Endosc Clin N Am. 1999;9:359-365. [PubMed] |
| 2. | Karras PJ, Barawi M, Webb B, Michalos A. Squamous cell papillomatosis of esophagus following placement of a self-expanding metal stent. Dig Dis Sci. 1999;44:457-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Chen JS, Luh SP, Lee F, Tsai CI, Lee JM, Lee YC. Use of esophagectomy to treat recurrent hyperplastic tissue obstruction caused by multiple metallic stent insertion for corrosive stricture. Endoscopy. 2000;32:542-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Song HY, Park SI, Do YS, Yoon HK, Sung KB, Sohn KH, Min YI. Expandable metallic stent placement in patients with benign esophageal strictures: results of long-term follow-up. Radiology. 1997;203:131-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 101] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Mallery S, Freeman ML. Removal of an incompletely expanded ultraflex esophageal stent. Gastrointest Endosc. 1996;43:163-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Stone CD, Lichtenstein DR. A novel technique for endoscopic removal of a migrated colonic stent. Gastrointest Endosc. 2001;54:522-524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Weickert U, Jakobs R, Siegel E, Schilling D, Riemann JF. Lasso technique for retrieval of a dislocated and impacted esophageal stent. Endoscopy. 2004;36:575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |