Published online Mar 16, 2022. doi: 10.12998/wjcc.v10.i8.2504
Peer-review started: July 26, 2021
First decision: October 22, 2021
Revised: October 30, 2021
Accepted: January 29, 2022
Article in press: January 29, 2022
Published online: March 16, 2022
Processing time: 229 Days and 16.4 Hours
Retroperitoneal cysts are rare and usually asymptomatic abdominal lesions. Epidermoid cysts are frequent benign cutaneous tumors, but retroperitoneal localization of these cysts does not occur very often.
We report a case report of a 25-year-old woman with a giant mass in the abdominal cavity. Because imaging examination indicated that the mass probably originated from the pancreas, the mass was considered a solid pseudopapillary tumor of the pancreas (SPTP). However, surgery revealed a retroperitoneal epidermoid cyst located behind the pancreas neck and the root of the superior mesenteric artery (SMA). We performed complete resection of the tumor. Postoperative pathology showed an epidermoid cyst. The patient fared well after two months of follow-up.
Surgery is the gold standard for the diagnosis and treatment of retroperitoneal epidermoid cysts. Retroperitoneal epidermoid cysts around the pancreas are easily misdiagnosed as cystic SPTPs. Surgeons should pay particular attention to preoperative diagnosis to reduce severe surgical complications and improve the quality of life of patients.
Core Tip: Retroperitoneal cysts are rare and usually asymptomatic abdominal lesions. Epidermoid cysts are frequent benign cutaneous tumors, but retroperitoneal localization of these cysts does not occur very often. Surgery is the gold standard for the diagnosis and treatment of retroperitoneal epidermoid cysts. Epidermoid cysts around the pancreas are easily misdiagnosed as cystic solid pseudopapillary tumors of the pancreas (SPTPs). Because of the different biological characteristics of retroperitoneal epidermoid cysts and SPTPs and the different surgical methods used for their treatment, surgeons should pay particular attention to preoperative diagnosis to reduce severe surgical complications and improve the quality of life of patients.
- Citation: Ma J, Zhang YM, Zhou CP, Zhu L. Retroperitoneal congenital epidermoid cyst misdiagnosed as a solid pseudopapillary tumor of the pancreas: A case report. World J Clin Cases 2022; 10(8): 2504-2509
- URL: https://www.wjgnet.com/2307-8960/full/v10/i8/2504.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i8.2504
Epidermoid cysts are tumor-like benign lesions that can be divided into congenital and acquired lesions. Congenital tumors often occur in the central nervous system and reproductive system and originate from the ectoderm of the skin at an early stage of the embryo. Acquired tumors are mostly caused by trauma and surgery wherein the epidermis is introduced into deep tissue. Epidermoid cysts are commonly found in the brain, trunk and neck and less commonly reported in the testis, penis, spleen and kidney[1,2].
The incidence of retroperitoneal epidermoid cysts is less than 1/40000, and most of them grow in the presacral region[3]. Retroperitoneal epidermoid cysts are less common at the back of the pancreatic neck or the root of mesenteric vessels. Because of the atypical location in this case, the cyst was misdiagnosed as a solid pseudopapillary tumor of the pancreas (SPTP) before laparotomy.
A 25-year-old Chinese woman experienced a one-month history of upper abdominal pain, abdominal distension and vomiting.
The patient developed epigastric pain without obvious cause one month prior, and she had symptoms of nausea and vomiting. She experienced no hematemesis or bloody stool, no chills or fever, and no significant weight loss.
The patient had no previous history of pancreatitis, trauma, surgery or a malignant tumor.
The patient had her menarche at the age of 14, and her menstrual cycle was regular. Her parents had no related diseases.
The physical examination revealed a firm abdominal mass reaching the navel, and the rest of the examination revealed no abnormalities.
Laboratory tests were normal.
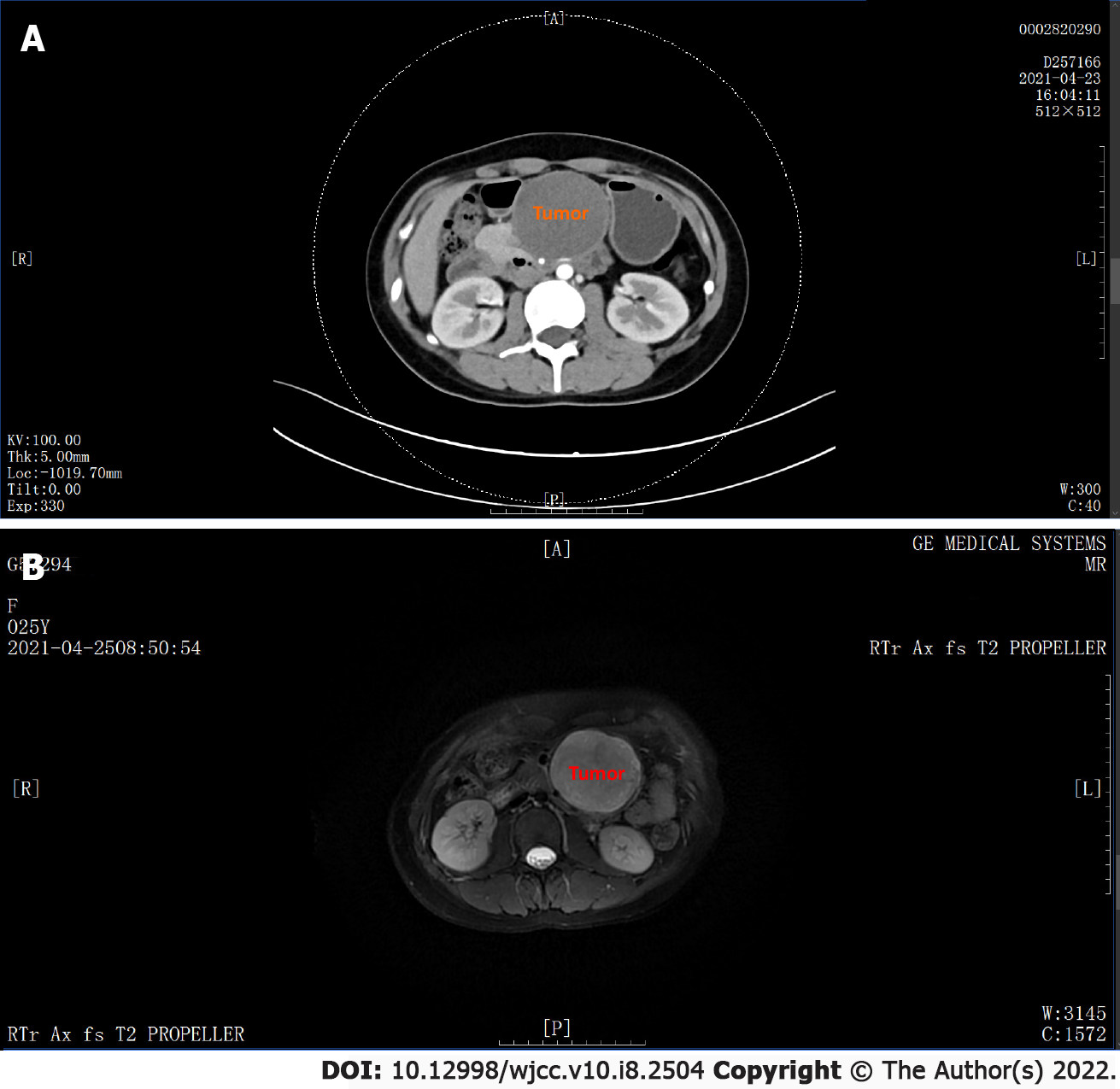
Computed tomography (CT) detected a 98 mm × 63 mm × 54 mm subcircular mass in the uncinate process of the pancreas; the boundary was clear, and the adjacent tissue was pressed upon, with multiple spots and granular dense shadows observed. The dual-phase CT values were approximately 30 to 36 HU, and the density of the mass (which was considered to be an SPTP) was inhomogeneous (Figure 1A).
Magnetic resonance imaging (MRI) detected one 91 mm × 72 mm × 63 mm mass below the pancreas, which appeared hypointense on T1-weighted imaging and hyperintense on T2-weighted imaging, T2-weighted fat suppression imaging, and diffusion-weighted imaging (DWI; b1200). The wall of the mass showed progressive enhancement. The tumor was adjacent to the pancreas, and the uncinate process was suspected to be the initial site of the tumor (which was considered to be an SPTP) (Figure 1B).
Postoperative pathology showed an epidermoid cyst.
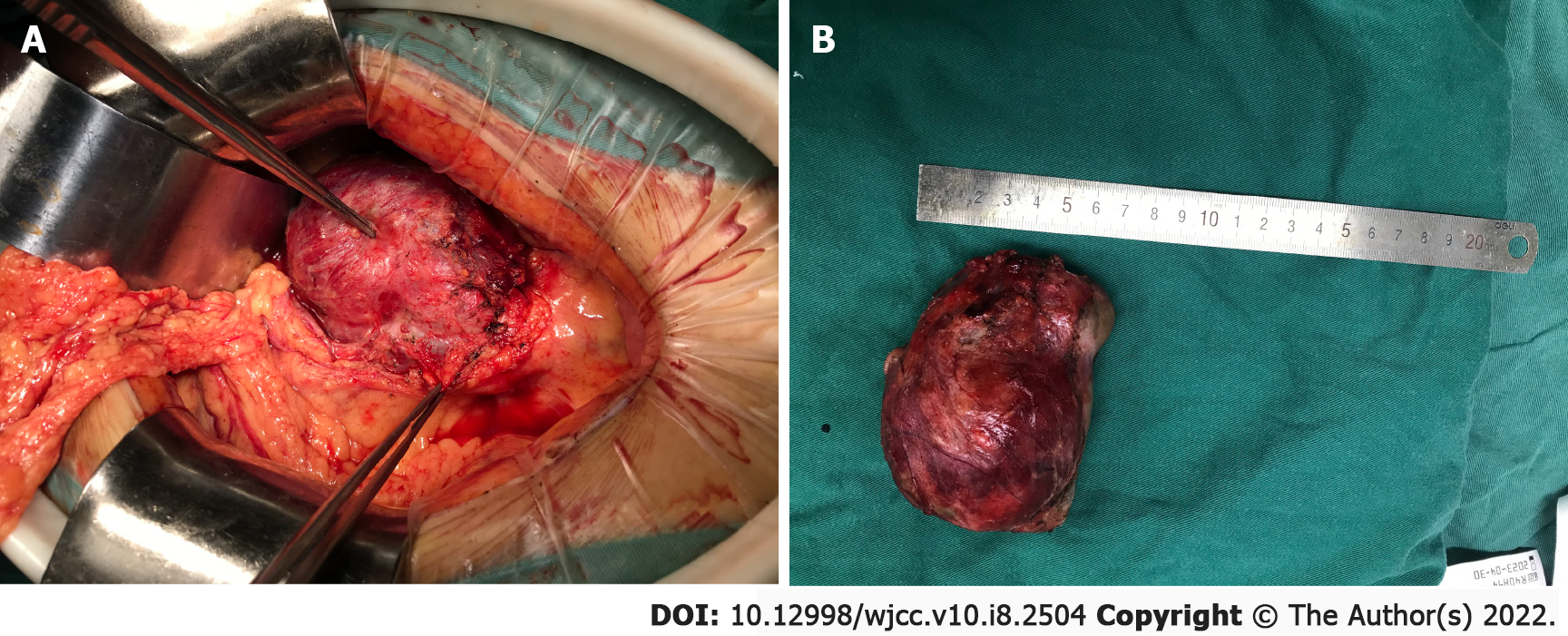
The patient underwent a median incision of the upper abdomen under general anesthesia. When the transverse colon was lifted upward, we observed a large cystic mass of approximately 100 mm × 70 mm × 60 mm with an intact wall. The lesion was located behind the pancreas neck, with the superior mesenteric artery (SMA) and horizontal part of the duodenum under compression; the right margin adhered closely to the superior mesenteric vein (SMV), and the left margin was close to the inferior mesenteric vein (IMV), caudally extending to separate the SMV and SMA (Figure 2A). We performed complete resection of the tumor. The cyst was excised after mobilization of the SMV and splenic vein (SV), which were found on the right side and cephalic side, respectively, of the tumor. During surgery, special attention was given to the connection between the lesion and the pancreas. The incidence of recurrence for retroperitoneal cysts is higher than that of other forms of cysts, as their proximity to major blood vessels and vital structures can make retroperitoneal cysts difficult to completely excise. Grossly, the cyst was approximately 10 cm in the largest dimension (Figure 2B).
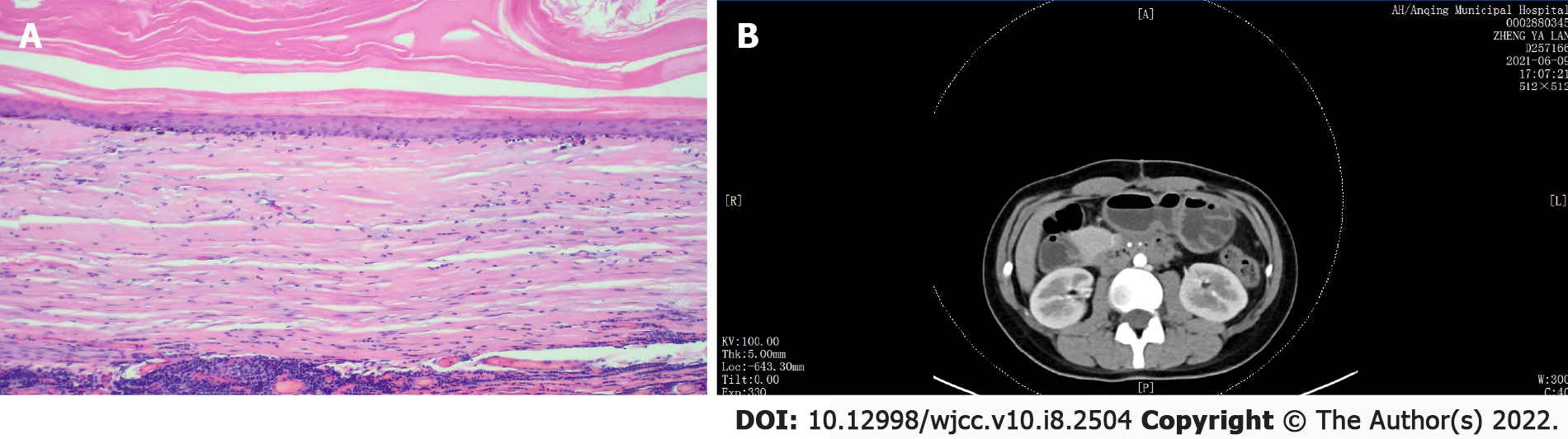
The patient recovered well and was discharged one week after the operation. Postoperative pathology showed an epidermoid cyst (Figure 3A). Two months later, enhanced CT revealed a normal shape of the SMV and SMA, no intravascular thrombus, no pseudoaneurysm, no obvious peripancreatic effusion, and no tumor recurrence or metastasis (Figure 3B).
The case was diagnosed as a retroperitoneal congenital epidermoid cyst for several reasons. First, the tumor was located at the back of the neck of the pancreas and the root of the SMA; second, the patient had no history of trauma or surgery.
The wall of the epidermoid cyst was composed of stratified squamous cells. The keratin and cholesterol that filled the cyst were gray–white, caseous, keratinized substances mixed with shed, broken epidermal cells. Epidermoid cysts are slow-growing benign tumors composed of epithelial cells[4].
The incidence of retroperitoneal congenital cysts is approximately 1/40000-1/63000. The main types of these cysts are epidermoid cysts, dermoid cysts, cystic hamartomas, teratomas and malignant teratomas[5].
Patients with retroperitoneal epidermoid cysts may have related symptoms, such as abdominal distension, abdominal pain, vomiting and constipation, depending on the location and volume of the tumor. Female patients are easily misdiagnosed with gynecological diseases. Some patients without clinical symptoms are diagnosed as a result of imaging examination.
CT features of epidermoid cysts include discrete lesions, thin and smooth cystic walls and homogeneous liquid density shadows[6]. On MRI, these cysts appear hypointense on T1-weighted imaging and hyperintense on T2-weighted imaging. However, some scattered low-density foci can be observed on T2-weighted imaging, which may be related to keratin in the cyst[6]. Because there are no vessels in the cysts, the masses are not enhanced by contrast medium. Retroperitoneal epidermoid cysts are rare and lack imaging specificity; therefore, it is difficult to distinguish them from other cystic tumors.
The first report of SPTP was by Frantz in 1959. SPTPs are mostly benign or low-grade malignant tumors and often occur in women, mainly between the ages of 20 and 30 years[7,8]. SPTPs are mostly circular or subcircular and can be located in any position on the pancreas[9]. SPTPs can be divided into three types: Solid, cystic-solid and cystic. On CT, the cystic type appears as an area of low density and is not enhanced by contrast medium. On MRI, the cystic type is hypointense on T1-weighted imaging, hyperintense on T2-weighted imaging, somewhat hyperintense on DWI imaging, and marginally strengthened on enhanced imaging.
There were several reasons for the mass to have been misdiagnosed as an SPTP. First, the patient was a young woman. Second, the mass was mainly located on the left side of the pancreatic head and behind the pancreatic neck, which led us to believe that the cyst may have originated from the pancreas. Third, preoperative images of retroperitoneal epidermoid cysts are similar to those of SPTPs.
Surgery is the main method of treatment for retroperitoneal epidermoid cysts. Because this disease is rare, it is easily confused with other types of tumors of the abdominal cavity. Misdiagnosis can lead to inappropriate surgery, increasing the risks of postoperative complications and mortality and thereby leading to significantly worse quality of life of patients. In the present case, careful exploration during the operation revealed that the tumor originated from the root of the SMA and failed to invade the pancreas; thus, fortunately, the woman avoided pancreaticoduodenectomy or middle pancreatectomy. In addition, with the continuous growth of lesions, inflammatory adhesion occurs around vital vessels and organs, which makes the lesions difficult to completely excise.
In summary, retroperitoneal epidermoid cysts around the pancreas are easily misdiagnosed as a cystic SPTP. Because of their different biological characteristics and surgical methods used for retroperitoneal epidermoid cysts and SPTP, surgeons should pay more attention to preoperative diagnosis to reduce severe surgical complications and improve the quality of life of patients.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Koustas E, Singh I, Villa E S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
| 1. | Kumar S, Sahana D, Rathore L, Sahu RK, Jain A, Borde P, Tawari M, Madhariya SN. Fourth Ventricular Epidermoid Cyst - Case Series, Systematic Review and Analysis. Asian J Neurosurg. 2021;16:470-482. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Bhasker N. Review of Head and Neck Masses in the Indian Population Based on Prevalence and Etiology With an Emphasis on Primary Diagnostic Modalities. Cureus. 2021;13:e16249. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | Fdili Alaoui FZ, Oussaden A, Bouguern H, El Fatemi H, Melhouf MA, Amarti A, Ait Taleb K. Giant pelvic retroperitoneal epidermoid cyst: a rare case report. Case Rep Med. 2012;2012:981387. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (1)] |
| 4. | Liu D, Zhou EY, Chen D, Tuan H, Zhao Y. Epidermoid cyst removal with CO2 laser fenestration: A retrospective cohort study. J Cosmet Dermatol. 2021;20:1709-1713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Kesici U, Sakman G, Mataraci E. Retrorectal/Presacral epidermoid cyst: report of a case. Eurasian J Med. 2013;45:207-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Hoang VT, Trinh CT, Nguyen CH, Chansomphou V, Tran TTT. Overview of epidermoid cyst. Eur J Radiol Open. 2019;6:291-301. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 100] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 7. | Coelho JCU, da Costa MAR, Ramos EJB, Torres AR, Savio MC, Claus CMP. Surgical Management of Solid Pseudopapillary Tumor of the Pancreas. JSLS. 2018;22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 8. | Gurzu S, Bara T, Sincu M, Gabos S, Vlad DM, Bara T Jr, Beres H, Jung I. Solid pseudopapillary neoplasm of pancreas: Two case reports. Medicine (Baltimore). 2019;98:e16455. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | Yao J, Song H. A Review of Clinicopathological Characteristics and Treatment of Solid Pseudopapillary Tumor of the Pancreas with 2450 Cases in Chinese Population. Biomed Res Int. 2020;2020:2829647. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |