Published online Mar 16, 2022. doi: 10.12998/wjcc.v10.i8.2447
Peer-review started: September 6, 2021
First decision: October 27, 2021
Revised: December 2, 2021
Accepted: February 10, 2022
Article in press: February 10, 2022
Published online: March 16, 2022
Processing time: 185 Days and 23.4 Hours
Tube indwelling is a key procedure in modern medicine. Careful tube setup is necessary to prevent unplanned extubation. The training for tube fixation is time- and resource-consuming, and optimal modes of training are currently being sought. Previous studies have compared workshops and flipped classroom models separately using conventional teaching strategies, but no study has examined a combination of both teaching models in nursing training.
To compare the effectiveness of workshops vs workshops combined with the flipped classroom model for improving tube fixation training for nursing students.
This was a prospective cohort study. In this study, 149 nurses who joined our hospital in 2019 underwent training using workshops combined with the flipped classroom model (experimental group), while 159 nurses who joined the hospital in 2018 received only workshop-based training (control group). The combination of workshops with the flipped classroom training model was divided into two modules: pre-class and in-class training. The participation of nurses in the training activities, on-site assessment of training, nurses’ evaluation of their training, and related indicators of tube quality management were evaluated.
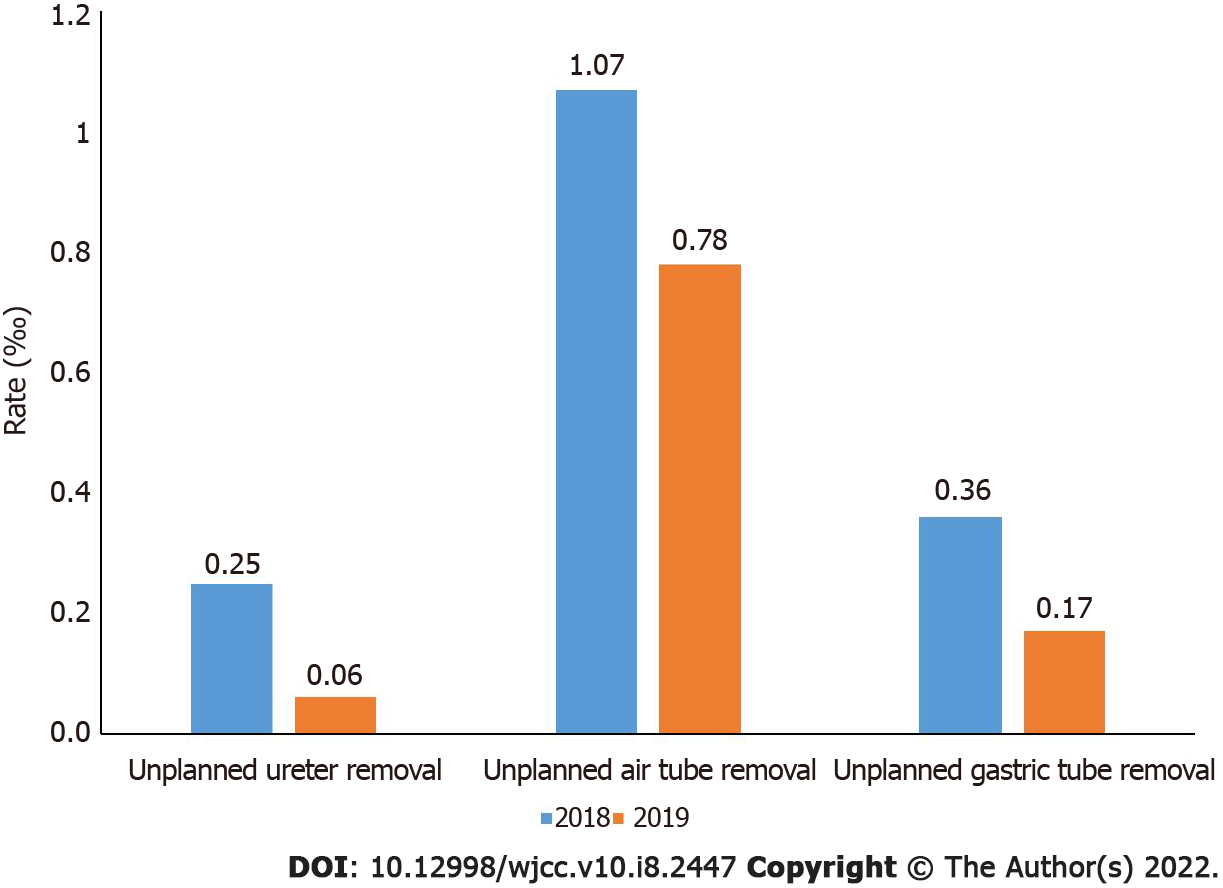
The average age of nurses in the control group was 22.94 ± 0.94 years and that of nurses in the experimental group was 25.42 ± 3.23 years (P < 0.01). The qualified rate of after-class assessments for the experimental and control groups was 100.00% (average score: 94.01 ± 2.78 points) and 91.82% (average score: 84.24 ± 2.94 points), respectively (P < 0.01). Most nurses in the experimental group completely agreed that the combined training was helpful to cultivate clinical thinking and independent learning ability and to master knowledge of tube fixation. In addition, the training content within the pre-class teaching video, pre-class tube atlas, pre-class main instructor guidance, in-class demonstration, and in-class practice was very informative. The experimental group had higher evaluation scores than the control group (4.88 ± 0.38 vs 4.67 ± 0.64; P < 0.01). Comparison of tube quality management before and after training in 2018 to 2019 revealed that the unplanned ureteral tube removal rate dropped from 0.25‰ to 0.06‰, the unplanned chest tube removal rate dropped from 1.07‰ to 0.78‰, and the unplanned gastric tube removal rate dropped from 0.36‰ to 0.17‰. The incidence rate of pressure ulcers caused by the tube decreased from 0.78‰ to 0.45‰.
The combination of workshop and flipped classroom training is effective in improving tube fixation training of nurses, cultivating nurses’ active learning abilities and clinical thinking, and improving the safety of the procedure.
Core Tip: This was a prospective study, in which 149 nurses participated in a new skill-training method for tube fixation training. The workshop combined with flipped classroom training was helpful in improving tube fixation training, cultivating nurses’ active learning abilities and clinical thinking, and improving the safety of the procedure.
- Citation: Wang YC, Cheng HL, Deng YM, Li BQ, Zhou XZ. Effectiveness of the combination of workshops and flipped classroom model to improve tube fixation training for nursing students. World J Clin Cases 2022; 10(8): 2447-2456
- URL: https://www.wjgnet.com/2307-8960/full/v10/i8/2447.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i8.2447
Tube indwelling is a key and complex procedure in modern medicine. It is a vital means and basis for treatment, observation, and prognosis of patients[1,2]. Unplanned extubation (UEX) refers to extubation intentionally caused by patients or by accident and one that is not planned by a healthcare worker[1-3]. Careful tube setup is necessary to prevent UEX[1,2], which requires appropriate training. Proper training is time- and resource-consuming, because tube indwelling is an invasive procedure and cannot be performed without adequate practice by student nurses or healthcare workers. Hence, optimal training models are being currently sought.
At present, the most effective approaches for learning medical techniques are eagerness of the trainees to learn the material, active participation of the students in class, and collaboration with classmates and instructors[4-6]. The workshop model first appeared during research in the field of education and psychology. It is a participatory, experiential, and interactive training model that can enhance the interest and enthusiasm of the participants to learn techniques through skill practice, which is essential to improve their ability to perform operations[7-10]. Another training model that is gaining popularity in healthcare is the flipped classroom model, in which the trainees are provided with learning resources (including paper materials, video, or audio lecture content, etc.) before attending the class, dedicating the classroom time for engaging and interactive discussion and experiential practices[11-16]. In workshop or teacher-focused training, trainers should stimulate learners’ interest from multiple perspectives. The training effect largely depends on nurses' interest and participation. As shown in several previous studies in the field of nursing, appropriate training methods can have a positive effect on nurses' participation in training. Several studies have explored the application of the flipped classroom model alone in nursing training. For example, Yi and Ding[17] implemented flipped classroom teaching in nursing management, and 96.8% of the students believed that it could promote learning and recognized this teaching mode. Yang et al[18] applied the flipped classroom model in geriatric nursing courses, and the results showed that there was no significant difference in the scores of comprehension and memory questions between groups, but the case analysis ability and autonomous learning ability were significantly improved. Liu et al[19] found that implementing the flipped classroom mode in nursing teaching in higher vocational colleges can improve students' autonomous learning ability, and their theoretical and operational assessment scores are significantly improved.
Previous studies have compared using workshops and flipped classroom models separately with conventional teaching methods[20-22]; however, to date, no study has examined the effectiveness of the combination of workshops and flipped classroom teaching techniques in medical education, although the concept theoretically exists in education[23]. The only literature on such an approach was a report that was published in the context of a flipped classroom workshop, during a conference[24]. It has been suggested that the flipped classroom technique engages trainees for a longer period and improves knowledge retention as well as performance of trainees, compared to more conventional teaching methods that are usually teacher-focused and theory-centered[25-27].
Our hospital set up a tube nurse specialist team in 2018. The workshop model was used to train 159 nurses who joined the hospital in 2018. After comprehensively evaluating the effectiveness of the workshop, the structure of the training model was reformed and the nurses who joined the hospital in 2019 received training based on a blended learning approach involving, a combination of the workshop with the flipped classroom model; this model was based on the hypothesis that the combination of the two methods could enhance the effectiveness of the training. Therefore, our study aimed to compare the effectiveness of workshop-only training with the combination of workshop and flipped classroom training on improving the teaching technique of tube fixation for nursing students. The findings of our study could provide new teaching methods to improve the effectiveness and safety of tube indwelling in clinical nursing.
This was a prospective cohort study involving 149 newly graduated trainee nurses who joined the Sun Yat-Sen Memorial Hospital of Sun Yat-Sen University in 2019 and received blended training, based on the combination of the workshop and flipped classroom (experimental group), and 159 nurses who joined the hospital in 2018 and received only workshop-based training (control group). All trainees were newly graduated nurses and were in their first year of working as registered nurses; they had no previous work experience or tube-related training. Biostatistics is not covered in this manuscript.
Tube fixation training is part of the standardized training course for new nurses at Sun Yat-Sen Memorial Hospital. The student nurses are required to complete the training and assessment course of this technique before working independently, in order to safely perform the procedure as well as meet the needs of clinical nursing work.
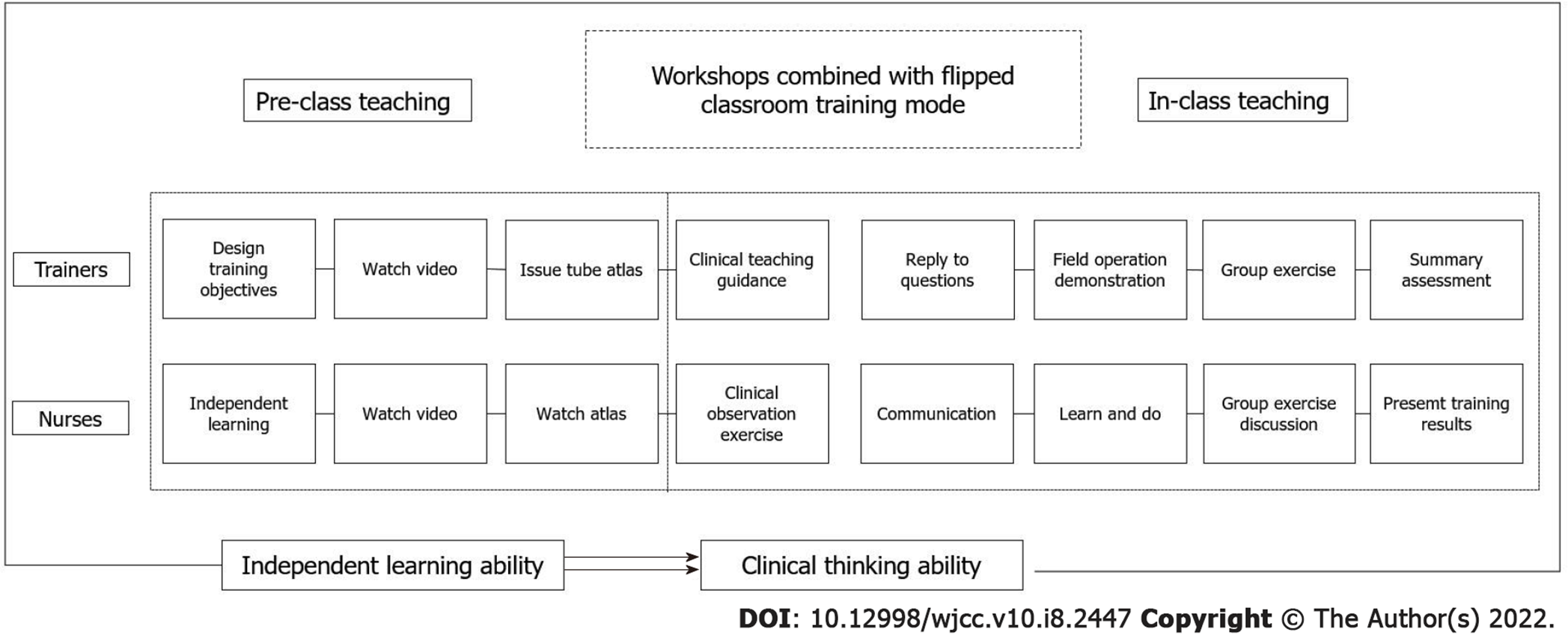
The control group received only in-class training using the traditional workshop model, including on-site explanation, on-site demonstration, group exercises, and summary assessments. The experimental group received tube fixation training using workshops in combination with a flipped classroom approach. The workshop combined with the flipped classroom model was led by a group of tube specialists from the hospital and was designed as two modules: Pre-class teaching and in-class training (Figure 1).
The pre-class training content was divided into three components.
Training design and requirements: Before the lecture, the training instructors designed the overall training objectives and content. The resources were then provided to the newly recruited nurses to study in advance. Furthermore, the instructors briefed the nurses on the combined approach that would be used for the tube fixation training and explained the study content and importance of pre-class training to facilitate independent learning. The training instructors regularly sent the trainees learning notices every week through a network communication platform, to encourage them to complete the pre-class self-study, following which they collected feedback.
Design and distribution of the pre-class training content: The training instructors sent the nurses pre-class training content that included a video operation guide of tube fixation and the fixation chart. The commonly used clinical tubes are divided into two categories: venous tubes and non-venous tubes. Non-venous tube fixation methods are further subdivided into gastric tube fixation, tracheal intubation fixation, I-shaped fixation, one-shaped fixation, and knot fixation methods. There are a total of seven tube fixation methods, and seven videos were recorded by the tube specialist group, each being 3-6 min in length. The nurses were required to watch the videos and were encouraged to engage in group discussions and ask questions in class. The tube fixation guide atlas was compiled by the tube specialist group, printed in large color pages, and distributed as a reference to the new nurses.
Observation and practice: The chief clinical instructor who approved the training and assessment designed by the tube specialist group provided guidance to the new nurses while they observed and practiced the tube fixation technique in a clinical setting.
The in-class training of the newly graduated nurses from the control and experimental groups was divided into two sessions, each session being 4 h long. After the training, each nurse was assessed for 0.5 h, totaling 4.5 h. The assessment mainly included three modules for the control group, including on-site demonstration, independent group practice and Q&A guidance, and on-the-spot examination. For the experimental group, a summary module was added.
On-site demonstration: The tube specialist group demonstrated the abovementioned seven fixation methods with physical projection equipment. The time to demonstrate each method was limited to 10-20 min, and the instructors simultaneously explained the methods. The key points, difficulties, and details of the methods were focused on. For the experimental group, theory and knowledge were supplemented based on actual cases.
Independent group exercise and Q&A guidance: The new nurses were organized in groups of 8-10. The instructors provided the trainees with tube models and exercise consumables. All nurses participated in the exercise and were encouraged to discuss the key difficulties and problems. The instructors answered any questions that the nurses had and guided each of them to practice independently.
Summary: The instructors answered any queries that the nurses had and summarized the advantages and disadvantages experienced during the practical application.
On-the-spot examination: All new nurses participating in the training had to complete the assessment by performing all seven fixation methods. The instructors worked in groups of two, and each group was responsible for the assessment and scoring of a fixation method.
The participation of the new nurses in the training activities, on-site assessment of the training, nurses’ evaluation of the training, and related indicators of tube quality management were evaluated. The nurses in the control group only participated in the on-site assessment of tube fixation methods and training satisfaction surveys.
Participation of nurses in training activities: For pre-class training, based on the observations of the chief instructors in each ward, the understanding of the nurses when learning to use the tube fixation atlas, the methods of tube fixation, and the participation of the nurses in the actual practice of tube fixation were recorded. For in-class training, the participation of the nurses was recorded through their participation in group exercises and discussions.
On-site assessment of the training: The assessment was conducted immediately after completing the on-site training and independent exercises. Instructors worked in teams of two and were responsible for the assessment of a fixation method. The nurses were required to complete the assessment and scoring of all fixation methods. The methods were scored using the percentile system, with ≥ 80 points indicating that the methods qualified; the fixation methods were deemed qualified only if they met the standards.
Evaluation of the training by the nurses: After class, a self-designed questionnaire was used to understand the evaluation of the training models by the trainee nurses. The questionnaire included the evaluation of the training models and the training content. Likert’s 5-level scoring scale was used to evaluate the training models. The responses were scored on a scale of 1-5, ranging from “completely disagree” to “completely agree” and “very bad” to “very good.” The questionnaire was completed on-site after training.
The standard clinical tube fixation rate, UEX rate, and incidence of tube-related pressure ulcers were recorded after the training. The standard clinical tube fixation rate was calculated as the number of fixed standard tubes/total number of tubes × 100%[1-3]. The UEX rate refers to the proportion of UEX of catheters occurring in hospitalized patients to the total number of days of indwelling of a catheter or to the total number of cases of catheter insertion during the same study period. The incidence of pressure ulcers is equal to the number of new cases of pressure injuries in hospitalized patients in the same period/total number of hospitalized patients in the same period × 100%.
All analyses were performed using the SPSS 20.0 software (IBM, Armonk, NY, United States). Continuous variables are presented as means ± SD and were analyzed using the Student’s t-test. Categorical data were presented as n (%) and were compared using a chi-square test. Ordinal data were presented as n (%) and were compared using the Mann–Whitney U-test. P values of < 0.05 were considered to be statistically significant.
The average age of nurses in the control group was 22.94 ± 0.94 years and that of those in the experimental group was 25.42 ± 3.23 years (P < 0.01). There were no significant differences in sex and educational background between the two groups (Table 1).
| Characteristics | Control group (n = 159) | Experimental group (n = 149) | P value |
| Age, years (mean ± SD) | 22.94 ± 0.94 | 25.42 ± 3.23 | < 0.01 |
| Sex (male/female), n (%) | 17/142 (10.69/89.31) | 21/128 (14.09/85.91) | 0.36 |
| Education background, n | |||
| Masters/Undergraduate | 1/158 (0.63/99.37) | 2/147 (1.34/98.66) | 0.52 |
The qualified rate of the after-class assessment for the experimental group was 100.00%, with an average score of 94.01 ± 2.78 points, compared to a qualified rate of 91.82% for the control group, with an average score of 84.24 ± 2.94 points (both P < 0.01; Table 2).
| Characteristics | Control group (n = 159) | Experimental group (n = 149) | P value |
| Assessment scoring (mean ± SD) | 84.24 ± 2.94 | 94.01 ± 2.78 | < 0.01 |
| Evaluation scoring (mean ± SD) | 4.67 ± 0.64 | 4.88 ± 0.38 | < 0.01 |
| Number of up-to-standard patients, n (%) | 146 (91.82) | 149 (100.00) | < 0.01 |
All 149 nurses in the experimental group completed the evaluation questionnaire. Most nurses completely agreed that the training model based on the combination of workshops and a flipped classroom was beneficial for cultivating clinical thinking (59.73%, score of 4.50 ± 0.68), encouraging independent learning ability (62.41%, score of 4.56 ± 0.62), and mastering knowledge (66.44%, score of 4.52 ± 0.76) (Table 3). In the experimental group, 52.35% nurses found that the pre-class training video helpful (score of 4.28 ± 0.89), 72.48% nurses found the pre-class tube atlas helpful (score of 4.68 ± 0.54), 59.06% nurses found the pre-class chief-instructor guidance helpful (score of 4.51 ± 0.65), 88.59% nurses found the in-class demonstration helpful (score of 4.87 ± 0.37), and 84.56% nurses found the in-class practice helpful (score of 4.84 ± 0.39) (Table 4). The evaluation score of the tube fixation training was higher in the experimental group compared to that in the control group (4.88 ± 0.38 vs 4.67 ± 0.64, P < 0.01; Table 2).
| Items | Score (mean ± SD) | Completely agree (%) | Mostly agree (%) | Basically agree (%) | Not agree (%) |
| Good for cultivating clinical thinking | 4.50 ± 0.68 | 89 (59.73) | 46 (30.87) | 13 (8.72) | 1 (0.67) |
| Good for cultivating independent learning ability | 4.56 ± 0.62 | 93 (62.41) | 48 (32.21) | 7 (4.69) | 1 (0.67) |
| Good for mastering knowledge | 4.52 ± 0.76 | 99 (66.44) | 32 (21.47) | 15 (10.06) | 3 (2.01) |
| Item | Score (mean ± SD) | Great (%) | Good (%) | General (%) | Bad (%) | Terrible (%) |
| Pre-class teaching video | 4.28 ± 0.89 | 78 (52.35) | 42 (28.19) | 23 (15.44) | 5 (3.36) | 1 (0.67) |
| Pre-class tube atlas | 4.68 ± 0.54 | 108 (72.48) | 35 (23.49) | 6 (4.03) | 0 | 0 |
| Pre-class main instructor guidance | 4.51 ± 0.65 | 88 (59.06) | 52 (34.90) | 7 (4.70) | 2 (1.34) | 0 |
| In-class demonstration | 4.87 ± 0.37 | 132 (88.59) | 15 (10.07) | 2 (1.34) | 0 | 0 |
| In-class practice | 4.84 ± 0.39 | 126 (84.56) | 22 (14.77) | 1 (0.67) | 0 | 0 |
After analysis and training, the clinical tube fixation methods were retrospectively analyzed at the end of 2019, and the standard fixation compliance rate was 96.03%. On comparing the rate of UEX events at our hospital in 2018 and 2019, we observed that the rate of unplanned ureteral tube removal decreased from 0.25‰ to 0.06‰, the rate of unplanned chest tube removal decreased from 1.07‰ to 0.78‰, and the rate of unplanned gastric tube removal decreased from 0.36‰ to 0.17‰ (Figure 2). Retrospective analysis of the pressure ulcers in the 2 years before and after training revealed that they mainly occurred with gastric tubes. The number of cases of pressure ulcers decreased from 33 to 22, and the incidence decreased from 0.78‰ to 0.45‰.
In this study, we compared the effectiveness of workshop-only training and the combined training model for improving the tube fixation training of nursing students. Our results strongly demonstrate that a blended learning approach using the combination of the workshop training and the flipped classroom training models was effective in improving the quality of teaching and learning the tube fixation methods. In addition, using this model encouraged the nurses’ enthusiasm and eagerness for interactive and independent learning and clinical thinking as well as improved the safety of the procedure.
The instructors should stimulate the nurses’ interest from multiple perspectives in order to influence as many trainees as possible[24]. The effectiveness of the training depends, to a large extent, on the training methods along with interest and participation of the nurses, which can have a positive effect on the quality of their participation in training. Some studies showed that the workshop training model could more effectively stimulate the nurses’ interest in learning compared to traditional teaching methods[28,29]. The flipped classroom model is focused on the students, and a large number of studies have shown that flipped classrooms can effectively improve the independent learning ability of students[19,25-27,30-31]. In this study, using the combination of the two learning models, the nurses were required to self-study before the class by watching videos and an atlas. Then, while in class, they were required to observe and practice the operations, find problems and solutions, and seek advice and clarifications regarding doubts from the clinical guidance teachers. The tube specialists then conducted practical ability training for all nurses through the workshop and finally completed the assessment. During the entire training process, as the main body of learning, not only did the nurses develop an interest in learning and cultivate the ability of independent learning, they also ensured the final effect of training. After completing the training course, some nurses commented the following: “this form of training is different from the inflexible classroom theoretical study. It enables us to learn on our own, has more opportunities for practical practice, engages in more exchanges and discussions, and improves our ability to think about clinical problems.” This response is reflected by the high satisfaction scores of the experimental group with regard to the training course.
In addition, as a result of the high quality of training, our study shows that combining the workshop and flipped classroom training models helps in improving the safety of using tubes in clinical practice. The nurses in our study provided good evaluation scores for the content of the training model, especially its ease of use, operation demonstration, and operation practice with the guidance of the tube fixation atlas; this proved to greatly improve the enthusiasm and eagerness of the nurses during training as well as the outcomes of training. Furthermore, analysis of clinical data after training showed that the fixation rate of clinical tubes reached 96.03%, and the busy work schedules of the nurses did not hamper their understanding and the effectiveness of tube fixation. When analyzing the UEX events at our hospital 1 year before and after the training, tube UEX rates decreased and the incidence of pressure ulcers caused by tubes decreased from 0.78‰ to 0.45‰; these rates indicate a better understanding of clinical tube fixation, which ensures that the tubes do not cause harm to the patients while playing effective roles in their treatment.
Despite the improvements observed with the novel combined training model, our study has some limitations. The participants in our study were inexperienced, newly graduated nurses, and this training model should be applied to assess the continuous education of experienced nurses as well.
Although good training results have been achieved using the combined training model for tube fixation, several problems need to be addressed. First, the inadequate training conditions cannot be ignored, and access to basic training equipment must be considered[32]. Due to the lack of literature on tube fixation training, this study has a theoretical and exploratory disadvantage. Furthermore, the number of nurses are higher than the number of trainers, and training efficacy cannot be guaranteed. Second, it is necessary to understand the adaptability of the trainers and nurses to the flipped classroom approach. To smoothly apply the flipped classroom model, it is necessary to encourage the nurses to become the main body of learning; change the traditional teacher-student relationship; and encourage nurses to find problems, raise issues, and think about problems that may be encountered during learning. Third, attention should be paid to effectively combine and promote the two training models. This study suggests that the pre-class training on tube fixation can be adequately conducted by using the flipped classroom model, but the in-class training should be conducted using the workshop model to ensure that the nurses have enough time to practice their skills. Further studies are required to refine and optimize the training content.
One limitation of this study is that the combined training model was in its first year of implementation. Similarly, the instructors responsible for designing the training were themselves exploring the course whilst conducting it. Moreover, the research scheme was immature. Due to the limitation of information technology, the pre-class contents could not be well mastered, and the pre-class training could not be effectively conducted. Furthermore, we did not record the observation of the instructors, so there was no effective evaluation of the differences in the training models by supervisors. Information from only the nurses was obtained by individually talking to them at the training site. Therefore, our study lacks robust quantitative results. The two groups in our study comprised nurses of different ages, and the training sessions were conducted at two different periods, which may have led to biases. Additional studies are necessary to address these limitations.
In conclusion, our results prove that a combined approach using workshop along with flipped classroom training is helpful in improving tube fixation training for student nurses. This novel combined model of a workshop and flipped classroom is in line with the development of modern informatization and innovation in sciences. Using the flipped classroom approach is particularly helpful to encourage nurses to become the main body of learning by active and interactive participation. In addition, it ensures the integration of theory with practical application, so as to achieve optimum effective training.
Nurse training for tube fixation is necessary to prevent unplanned extubation.
No study has examined a combination of both workshop and flipped classroom models in tube fixation training for nurses.
This study aimed to compare workshops plus flipped classroom model with workshops alone to deliver tube fixation training for nurses.
Nurses were trained according to the two models, and the quality indicators of the training were then evaluated.
Nurses in the combined training group scored higher than nurses who received workshop training alone.
Workshop plus flipped classroom models are effective in improving tube fixation training in nurses.
Future studies can investigate class content, record trainers’ observations, and devise an effective method to evaluate the training model.
The authors thank all the study participants who were enrolled in this study.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Nursing
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Joseph MA, NG DTK S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Astle BJ, Duggleby W. Canadian Fundamentals of Nursing, 6th edition. Toronto: Elsevier Canada, 2018. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (1)] |
| 2. | Potter PA, Perry AG, Stockert P, Hall A. Fundamentals of Nursing, ninth edition. Toronto: Elsevier Canada, 2016. [DOI] [Full Text] |
| 3. | National Institute of Hospital Administration. Handbook of Nursing Sensitive Quality Indicators (2016 Edition). Beijing: People's Medical Publishing House, 2016. [RCA] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Freeman S, Eddy SL, McDonough M, Smith MK, Okoroafor N, Jordt H, Wenderoth MP. Active learning increases student performance in science, engineering, and mathematics. Proc Natl Acad Sci U S A. 2014;111:8410-8415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3461] [Cited by in RCA: 1613] [Article Influence: 146.6] [Reference Citation Analysis (0)] |
| 5. | Prober CG, Heath C. Lecture halls without lectures--a proposal for medical education. N Engl J Med. 2012;366:1657-1659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 365] [Cited by in RCA: 327] [Article Influence: 25.2] [Reference Citation Analysis (0)] |
| 6. | Mehta NB, Hull AL, Young JB, Stoller JK. Just imagine: new paradigms for medical education. Acad Med. 2013;88:1418-1423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 196] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 7. | Catling C, Hogan R, Fox D, Cummins A, Kelly M, Sheehan A. Simulation workshops with first year midwifery students. Nurse Educ Pract. 2016;17:109-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Fischer F, Helmer S, Rogge A, Arraras JI, Buchholz A, Hannawa A, Horneber M, Kiss A, Rose M, Söllner W, Stein B, Weis J, Schofield P, Witt CM. Outcomes and outcome measures used in evaluation of communication training in oncology - a systematic literature review, an expert workshop, and recommendations for future research. BMC Cancer. 2019;19:808. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 9. | Honeyman CS. Course Review: North East Microsurgery Training Course and Workshop: A New Two Day Microsurgery Course for Trainees in Plastic Surgery, Otolaryngology and Oral and Maxillofacial Surgery. Ann Plast Surg. 2016;77:262-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Walters ST, Matson SA, Baer JS, Ziedonis DM. Effectiveness of workshop training for psychosocial addiction treatments: a systematic review. J Subst Abuse Treat. 2005;29:283-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 119] [Article Influence: 6.0] [Reference Citation Analysis (1)] |
| 11. | Betihavas V, Bridgman H, Kornhaber R, Cross M. The evidence for 'flipping out': A systematic review of the flipped classroom in nursing education. Nurse Educ Today. 2016;38:15-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 395] [Cited by in RCA: 236] [Article Influence: 26.2] [Reference Citation Analysis (0)] |
| 12. | Leung JY, Kumta SM, Jin Y, Yung AL. Short review of the flipped classroom approach. Med Educ. 2014;48:1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Lo CK, Hew KF. A critical review of flipped classroom challenges in K-12 education: possible solutions and recommendations for future research. Res Pract Technol Enhanc Learn. 2017;12:4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 14. | Njie-Carr VP, Ludeman E, Lee MC, Dordunoo D, Trocky NM, Jenkins LS. An Integrative Review of Flipped Classroom Teaching Models in Nursing Education. J Prof Nurs. 2017;33:133-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 61] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 15. | Vanka A, Vanka S, Wali O. Flipped classroom in dental education: A scoping review. Eur J Dent Educ. 2020;24:213-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 16. | Xu P, Chen Y, Nie W, Wang Y, Song T, Li H, Li J, Yi J, Zhao L. The effectiveness of a flipped classroom on the development of Chinese nursing students' skill competence: A systematic review and meta-analysis. Nurse Educ Today. 2019;80:67-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 17. | Yi Y, Ding F. Research on the application of workshop in nurses' standardized pipe fixation training. China Nurs Educ. 2018;15:5. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Yang M, Zhang J, Gao L, Kun L. Application and effect of flipped classroom in nursing management teaching. Chin Nurs Educ. 2017;14:4. [DOI] [Full Text] |
| 19. | Liu P, Xue M, Ma L, Jing L. The influence of flipped classroom teaching on the autonomous learning ability of nursing students in Vocational colleges. Chin Nurs Educ. 2016;2016:109-112. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Pawelczak D. Comparison of traditional lecture and flipped classroom for teaching programming. 3rd International Conference on Higher Education Advances, HEAd'17. Valencia, 2017. [DOI] [Full Text] |
| 21. | Tang F, Chen C, Zhu Y, Zuo C, Zhong Y, Wang N, Zhou L, Zou Y, Liang D. Comparison between flipped classroom and lecture-based classroom in ophthalmology clerkship. Med Educ Online. 2017;22:1395679. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 102] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 22. | Chen F, Lui AM, Martinelli SM. A systematic review of the effectiveness of flipped classrooms in medical education. Med Educ. 2017;51:585-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 341] [Cited by in RCA: 354] [Article Influence: 44.3] [Reference Citation Analysis (0)] |
| 23. | Pugsee P. Using of the Flipped Classroom Learning with a Workshop Activity in Object-oriented Analysis and Design Course. Adv Sci Technol Engin Syst J. 2018;3:52-63. [DOI] [Full Text] |
| 24. | Musunuru K, Haspel RL; Innovative Approaches to Education Working Group of the Inter-Society Coordinating Committee for Practitioner Education in Genomics. Improving Genomic Literacy Among Cardiovascular Practitioners via a Flipped-Classroom Workshop at a National Meeting. Circ Cardiovasc Genet. 2016;9:287-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 25. | Lew EK. Creating a contemporary clerkship curriculum: the flipped classroom model in emergency medicine. Int J Emerg Med. 2016;9:25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 26. | Tune JD, Sturek M, Basile DP. Flipped classroom model improves graduate student performance in cardiovascular, respiratory, and renal physiology. Adv Physiol Educ. 2013;37:316-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 291] [Cited by in RCA: 163] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 27. | Heitz C, Prusakowski M, Willis G, Franck C. Does the Concept of the "Flipped Classroom" Extend to the Emergency Medicine Clinical Clerkship? West J Emerg Med. 2015;16:851-855. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 44] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 28. | Yi Y, Ding F. Study on the Application of Workshop in the Training of Standardized Tube Fixation for Nurses. China J Nurs Educ. 2018;15:424-428. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 29. | Karim HM, Yunus M, Bhattacharyya P, Ahmed G. Comparison of effectiveness of class lecture vs workshop-based teaching of basic life support on acquiring practice skills among the health care providers. Int J Crit Illn Inj Sci. 2016;6:61-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 30. | Yang M, Zhang J, Gao L. Application and Effect of Flipped Classroom in Nursing Management Teaching. China J Nurs Educ. 2017;2017. [RCA] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |