Published online Mar 6, 2022. doi: 10.12998/wjcc.v10.i7.2216
Peer-review started: March 24, 2021
First decision: October 16, 2021
Revised: October 27, 2021
Accepted: January 22, 2022
Article in press: January 22, 2022
Published online: March 6, 2022
Processing time: 342 Days and 21.6 Hours
Quetiapine, known as a non-classical antipsychotic drug, is frequently used for the treatment of mental diseases, such as schizophrenia, bipolar disorder, and major depressive disorder. Acute lung injury, a rarely reported side effect of quetiapine, is described in this case report.
Due to terminal delirium, a 66-year-old man took a large dose of quetiapine and then developed severe pulmonary disease. His symptoms were not resolved after routine treatment, such as antibiotics, diuretic, and supportive therapies. Quetiapine-related acute lung injury was therefore suspected and hormonal therapy was initiated. Subsequently, his symptoms were alleviated and the radiological results improved dramatically.
Our findings in the present report highlight a potential adverse effect of quetiapine, drug-related acute lung injury, which deserves awareness in clinical practice.
Core Tip: Quetiapine is a non-classic antipsychotic drug. Acute lung injury, a rarely reported side effect of quetiapine, is described in this case report. Common etiologies were ruled out when the patient’s symptoms were not resolved after routine treatment. Finally, quetiapine-related acute lung injury was suspected and hormonal therapy was initiated. The patient’s symptoms were alleviated and the radiological results improved. The case report highlights this potential adverse effect of quetiapine, which deserves more awareness in clinical practice.
- Citation: Huang YX, He GX, Zhang WJ, Li BW, Weng HX, Luo WC. Quetiapine-related acute lung injury: A case report. World J Clin Cases 2022; 10(7): 2216-2221
- URL: https://www.wjgnet.com/2307-8960/full/v10/i7/2216.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i7.2216
Quetiapine is a commonly prescribed atypical antipsychotic drug used for the treatment of several mental diseases, such as schizophrenia, bipolar disorder, and major depressive disorder. It is also effective for patients with delirium, those with obsessive-compulsive disorder, etc. Due to its efficacy and few reported side effects, quetiapine is widely used in clinical practice[1].
The reported adverse effects of quetiapine are relatively rare and mild, such as extrapyramidal reaction, dizziness, drowsiness, abnormal liver function, postural hypotension, and tachycardia[2]. Quetiapine overdose is rarely reported and limited information is available regarding overuse cases. Therefore, a case of acute lung injury caused by a large dose of quetiapine is presented and awareness of this adverse reaction may improve patient outcomes.
On April 5, 2016, a 66-year-old man was admitted to our hospital for delirium lasting for 6 h.
The patient’s family found him to be delirious and a medicine bottle used for quetiapine storage [20 tablets (200 mg)] was empty. The patient was suspected of having taken a large dose of quetiapine. Gastric lavage was performed and he was admitted to the intensive care unit (ICU) for further management.
The patient had a history of mental illness, but the details were unclear. He had a medical history of quetiapine use during the past 6 mo.
No abnormalities were found in the patient's personal and family history.
The patient’s vital signs were as follows: Heart rate, 118 beats/min; respiratory rate, 13 breaths/min; systolic/diastolic blood pressure, 146/69 mmHg; and temperature, 36.6 ℃. The Glasgow Coma Score was calculated and estimated to be 5. Moist rale was heard on auscultation of the lungs. Both pupils were round and equal (3.5 mm) and the heart rhythm was normal.
Blood analysis revealed leukocytosis with a white blood cell count of 16.6 × 109/L, predominantly neutrophils (94.9%), and a normal platelet count. Prothrombin and partial thromboplastin times were prolonged, and D-dimers were slightly increased at 1.63 μg/mL. Serum C-reactive protein was elevated at 80.0 mg/L (normal range, < 8 mg/L) and procalcitonin was normal. The blood biochemistry results, as well as urine analysis, were normal.
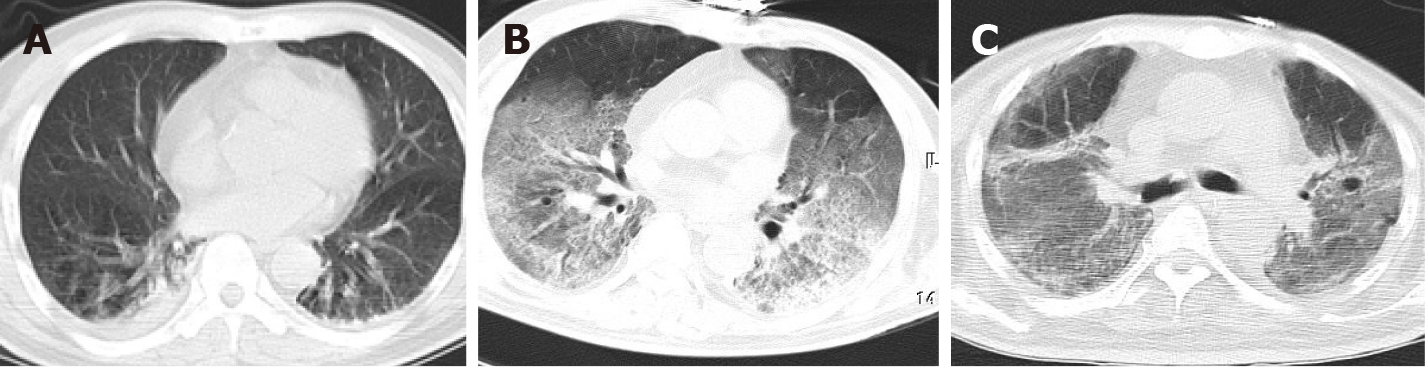
Abnormal radiological features such as lacunar cerebral infarction in the bilateral thalamus and left basal ganglia, consolidation in both lower lobes, and nodules in the dorsal segment of the left lower lung were suggested by computed tomography (CT) (Figure 1A).
Due to the suspicion of quetiapine intoxication, therapies such as oxygen inhalation, hemoperfusion (three times), hemofiltration, reduced glutathione, and naloxone were administered. Unfortunately, the patient’s blood oxygen saturation gradually decreased, reaching 83%-86% on the 3rd day even with an oxygen flow rate of 10 L/min. Emergency endotracheal intubation and mechanical ventilation were then used [ventilator parameters: Oxygen concentration fraction (FiO2), 80%; pressure support, 20 cm H2O; positive end-expiratory pressure, 10 cm H2O]. Similarly, blood pressure was measured and decreased to 90/52 mmHg during the ICU stay. After norepinephrine administration [0.1-0.3 g/(kg· min)] for 30 h, blood pressure was restored to 115-145/56-68 mmHg. The cardiac ultrasound examination was normal and B-type natriuretic peptide (BNP) was 184.6 ng/L. Chest radiography revealed more patchy shadows with increased density and blurred borders in the lungs. On the 4th day, the patient regained consciousness. For blood oxygen saturation, FiO2 was kept at 70% for ventilation. Additionally, antibiotic and diuretic treatments resulted in no improvements in the oxygenation index. On the 8th day, C-reactive protein had decreased to 47.4 mg/L, but chest CT (Figure 1B) was performed again and showed diffuse exudation and ground-glass shadows in the lungs. During the treatment period, the patient underwent sputum (n = 5), urine (n = 1), and blood (n = 1) cultures, with no evidence of infection.
Based on these observations, common diagnoses (such as pulmonary infection, congestive heart failure, and pulmonary embolism) were ruled out. Finally, the man was diagnosed with quetiapine-related acute lung injury.
On April 14, methylprednisolone was administrated as follows: 80 mg, intravenous drip every 8 h for 8 d; 80 mg, intra-venous infusion every 12 h for 7 d; 40 mg intravenous infusion every 12 h for 7 d; 40 mg intravenous drip every 8 h for 3 d; and 20 mg intravenous drip every 8 h. In addition, prone ventilation was performed.
FiO2 was kept stable at 60%-80% for ventilation between April 14 and April 22. On April 23, FiO2 was reduced to 55% and was gradually decreased due to the impro-vement of the oxygenation index. The patient’s radiological results improved dramatically (Figure 1C). Finally, on May 7, the endotracheal tube was removed and the patient required no further mechanical ventilatory support. The patient was discharged on June 3 after his condition improved. The patient’s condition and interventions during hospitalization are shown in Table 1.
| Timeline | April 5 | April 6 | April 7 | April 8 | April 14 | April 23 | May 7 |
| Condition | Delirium | Blood pressure1 | Blood oxygen saturation1 | Regained consciousness, blood oxygen saturation (unchanged) | Blood oxygen saturation (unchanged) | Blood oxygen saturation2 | Blood oxygen saturation2 |
| Intervention | Admission and hemoperfusion | Norepinephrine | Endotracheal intubation and mechanical ventilation | Antibiotic and diuretic treatments | Methylprednisolone | Methylprednisolone decrement | Intubation (removed) |
Quetiapine is a dibenzothiazepine derivative that shows affinity for a variety of neurotransmitter receptors including dopamine and 5-hydroxytryptamine receptors. In China, several studies have demonstrated that quetiapine is effective for many mental symptoms, such as schizophrenia, affective disorders, and mental disorders associated with organic brain diseases such as Alzheimer’s disease. Its efficacy in the control of delirium and obsessive-compulsive disorder was also observed and few side effects have been reported with its use. Therefore, quetiapine is widely used in developing countries[1].
Adverse reactions to quetiapine are infrequent in clinical practice. However, adverse reactions have been widely evaluated and the relevant information was often obtained from clinical trials involving patients or volunteers, or from datasets obtained from drug administration. As reported in the drug product information, the most common adverse reaction to quetiapine is nervous system damage, which usually presents with extrapyramidal reactions, dizziness, and drowsiness. Other adverse reactions include gastrointestinal disorders, hepatobiliary disorders, cardiac disorders, and blood and lymphatic system disorders[2,3]. In a systematic review, the data suggested that common adverse reactions to quetiapine included somnolence (25%-39%), dizziness (15%-27%), headache (10%-23%), postural hypotension (6%-18%), and weight gain (11%-30%)[4]. Additionally, quetiapine treatment can increase the risk of pneumonia among patients with schizophrenia[5], which has been confirmed in a case of quetiapine-induced interstitial pneumonia[6].
Clinical presentations of drug-related lung injuries are usually nonspecific, such as clinical symptoms, radiological features, and pathological evidence. Hence, it is difficult to make a definite diagnosis. Recently, a consensus statement on drug-related lung injury was issued by the Japanese Respiratory Society and several criteria for the diagnosis of drug-related lung injuries were addressed as follows: A drug which can induce lung injury and the corresponding clinical presentation was used; other causes for the injury may exist; the clinical presentation could improve after drug discontinuation and worsen if the drug is used again[7]. Identification of lung injuries caused by the drug is generally indirect. A combination of the medical history, laboratory examination, and response to treatment should be considered for clinical diagnosis. This is because objective diagnostic criteria are lacking and the diagnosis continues to rely on the presence or absence of a response to the drug. Drug-related lung injury usually stops progressing after drug discontinuation. The patient’s condition improves after hormone use, leading to recovery from the injury[8]. However, the radiological features of drug-related injury are similar to those of other diseases, such as interstitial pneumonitis, pulmonary fibrosis, hypersensitivity reaction, acute respiratory distress syndrome, and bronchiolitis obliterans organizing pneumonia. If the patient’s medical history suggests a potential risk of drug-related injury, further efforts may be required[9].
As an adverse reaction, respiratory disorders are rarely reported in patients with quetiapine use and the corresponding rate among total adverse events was reported to be 2.8%[3]. To date, few cases of drug poisoning that eventually resulted in quetiapine overdose have been reported in China. In a recent study, a case series of 12 patients who ingested 500-12000 mg quetiapine at once were reviewed, and several clinical characteristics associated with quetiapine use were identified, such as somnolence, slow pupillary light reflex, tachycardia, lethargy, excited agitation, hypokalemia, coma, slurred speech, pupil dilation, elevated white blood cells, and electrocardiogram abnormality[10]. The mechanism by which quetiapine induces drug-related lung injury remains unclear and requires further investigation. One possible explanation is that quetiapine is mainly metabolized by CYP3A4, which is found in lung tissues[11]. Afterward, toxic metabolites are generated, such as 7-hydroxyquetiapine, which contribute to the pulmonary impairment[12,13].
In terms of drug-related lung injury treatment, the most important factor is stopping the drug use, which usually leads to the alleviation of symptoms in most patients. Glucocorticoid therapy is subsequently administrated to patients who require further intervention. Most physicians recommend the administration of glucocorticoid at 1 mg/kg for several months (based on clinical manifestations and procedures), followed by a reduction[14]; however, the appropriate dose of hormones for the treatment of drug-related lung injuries remains unclear due to a lack of evidence. At present, quetiapine is widely used in China. Although there are few cases of lung injuries caused by quetiapine and the mechanism is unclear, studies are warranted to confirm the existence of a dose correlation. However, clinicians should be vigilant during the diagnosis and treatment, and should be aware of the possibility of drug-related lung injuries caused by quetiapine.
Quetiapine is an atypical antipsychotic drug commonly prescribed for the treatment of several mental diseases, but its side effects are concerning, even though they are not commonly seen in the clinic. In this case report, we describe a case of drug-related acute lung injury caused by high-dose quetiapine intoxication. Although there are few cases of lung injuries caused by quetiapine and the mechanism is unclear, clinicians should be vigilant during the diagnosis and treatment, and should be aware of the possibility of drug-related lung injuries caused by quetiapine.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Hassaan NA, Nakhleh A S-Editor: Wang JJ L-Editor: Wang TQ P-Editor: Wang JJ
| 1. | Feng ZY, Wang ZG. The clinical application of quetiapine in China. J Psychiat. 2010;23:475-477. [DOI] [Full Text] |
| 2. | Shen JW, Ma Y, Mao YM. Analysis of 149 Adverse Drug Reaction Reports Induced by Quetiapine. China Pharmacy. 2011;2011:3031-3033. [DOI] [Full Text] |
| 3. | Tapiainen V, Lavikainen P, Koponen M, Taipale H, Tanskanen A, Tiihonen J, Hartikainen S, Tolppanen AM. The Risk of Head Injuries Associated With Antipsychotic Use Among Persons With Alzheimer's disease. J Am Geriatr Soc. 2020;68:595-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | El-Saifi N, Moyle W, Jones C, Tuffaha H. Quetiapine safety in older adults: a systematic literature review. J Clin Pharm Ther. 2016;41:7-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 5. | Kuo CJ, Yang SY, Liao YT, Chen WJ, Lee WC, Shau WY, Chang YT, Tsai SY, Chen CC. Second-generation antipsychotic medications and risk of pneumonia in schizophrenia. Schizophr Bull. 2013;39:648-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 127] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 6. | Kim SJ, Han SD, Lee JY, Chon GR. A case of drug-induced interstitial pneumonia potentially related to quetiapine (seroquel) therapy for behavioral and psychological symptoms. Respir Care. 2014;59:e145-e148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Kubo K, Azuma A, Kanazawa M, Kameda H, Kusumoto M, Genma A, Saijo Y, Sakai F, Sugiyama Y, Tatsumi K, Dohi M, Tokuda H, Hashimoto S, Hattori N, Hanaoka M, Fukuda Y; Japanese Respiratory Society Committee for formulation of Consensus statement for the diagnosis and treatment of drug-induced lung injuries. Consensus statement for the diagnosis and treatment of drug-induced lung injuries. Respir Investig. 2013;51:260-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 193] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 8. | Shi JH, Yan XW, Xu WB, Liu HR, Zhu YY. Clinical diagnosis and treatment of drug-induced lung injury. Chin J Tuberc Respir Dis. 2007;30:161-166. [DOI] [Full Text] |
| 9. | Cleverley JR, Screaton NJ, Hiorns MP, Flint JD, Müller NL. Drug-induced lung disease: high-resolution CT and histological findings. Clin Radiol. 2002;57:292-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 110] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 10. | Bai R. Clinical manifestations of quetiapine overdose. Chinese Nursing Association 2009 National Nursing Management Academic Exchange and special Lecture Conference Chinese Nursing Association 2009 National Nursing New Theory, New Method, New Technology Seminar. 2009 Nov 12; Leeds, China. Haikou: Chinese Nursing Association, 2009: 133-136. |
| 11. | Wijnen PA, Bekers O, Drent M. Relationship between drug-induced interstitial lung diseases and cytochrome P450 polymorphisms. Curr Opin Pulm Med. 2010;16:496-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | DeVane CL, Nemeroff CB. Clinical pharmacokinetics of quetiapine: an atypical antipsychotic. Clin Pharmacokinet. 2001;40:509-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 272] [Cited by in RCA: 275] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 13. | Grimm SW, Stams KR, Bui K. In vitro prediction of potential metabolic drug interactions for seroquel. Schizophr Res. 1997;24:198-198. [DOI] [Full Text] |
| 14. | Cai BQ, Li LY. Concord respiration of Peking Union Medical College Beijing. China: Peking Union Medical College Press, 2011. |