Published online Feb 26, 2022. doi: 10.12998/wjcc.v10.i6.1863
Peer-review started: June 4, 2021
First decision: September 1, 2021
Revised: September 14, 2021
Accepted: January 13, 2022
Article in press: January 13, 2022
Published online: February 26, 2022
Processing time: 264 Days and 10.5 Hours
Epidural hematoma is one of the common postoperative complications after craniotomy. However, multiple remote epidural hematomas in different sites, including supratentorial and infratentorial regions, are exceedingly rare.
We present a rare case in which three remote epidural hematomas occurred after craniotomy. A 21-year-old woman was admitted with a headache for 1 mo, vomiting, and rapid vision loss for 1 wk. Brian magnetic resonance imaging indicated a right thalamic tumor. The intraoperative diagnosis was a cystic tumor, posterior cerebral artery aneurysm, and vascular malformation. The operation was successful. Unfortunately, the patient developed three extradural hematomas within 48 h. Family members consented to the first two hematoma evacuations but refused the third.
More attention should be paid to this kind of rare complication. Adequate preoperative evaluation is important, especially for acute patients. Monitoring neural function and early computed tomography scanning of the brain after surgery should be highlighted.
Core Tip: We report a 21-year-old emergency woman who developed three remote epidural hematomas in different sites after craniotomy.
- Citation: He Q, Tao CY, Fu RH, You C. Multiple different remote epidural hematomas after craniotomy: A case report. World J Clin Cases 2022; 10(6): 1863-1868
- URL: https://www.wjgnet.com/2307-8960/full/v10/i6/1863.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i6.1863
Postoperative hemorrhage includes intracerebral hematoma (ICH), subdural hematoma, and extradural hematoma (EDH), which are serious complications after craniotomy. EDH is one of the most frequent and devastating complications. It may occur in supratentorial, infratentorial, ipsilateral, and even contralateral sites of the operative area[1,2]. As a specific subset of EDH after craniotomy, multiple remote EDHs are very rare. In this study, we present a 21-year-old woman who developed three remote EDHs in different sites after craniotomy.
A 21-year-old woman visited the emergency department and was admitted to the Neurosurgery Department. She complained of headache and vomiting for 1 mo, and rapid vision loss for 1 wk.
The patient had a headache and recurrent vomiting, along with rapid vision loss.
The patient had no significant medical history.
Neither the patient nor her family members had special medical history.
The patient was conscious. The extremities were moved as instructed. General sensory was normal. The positive sign was blurred binocular vision.
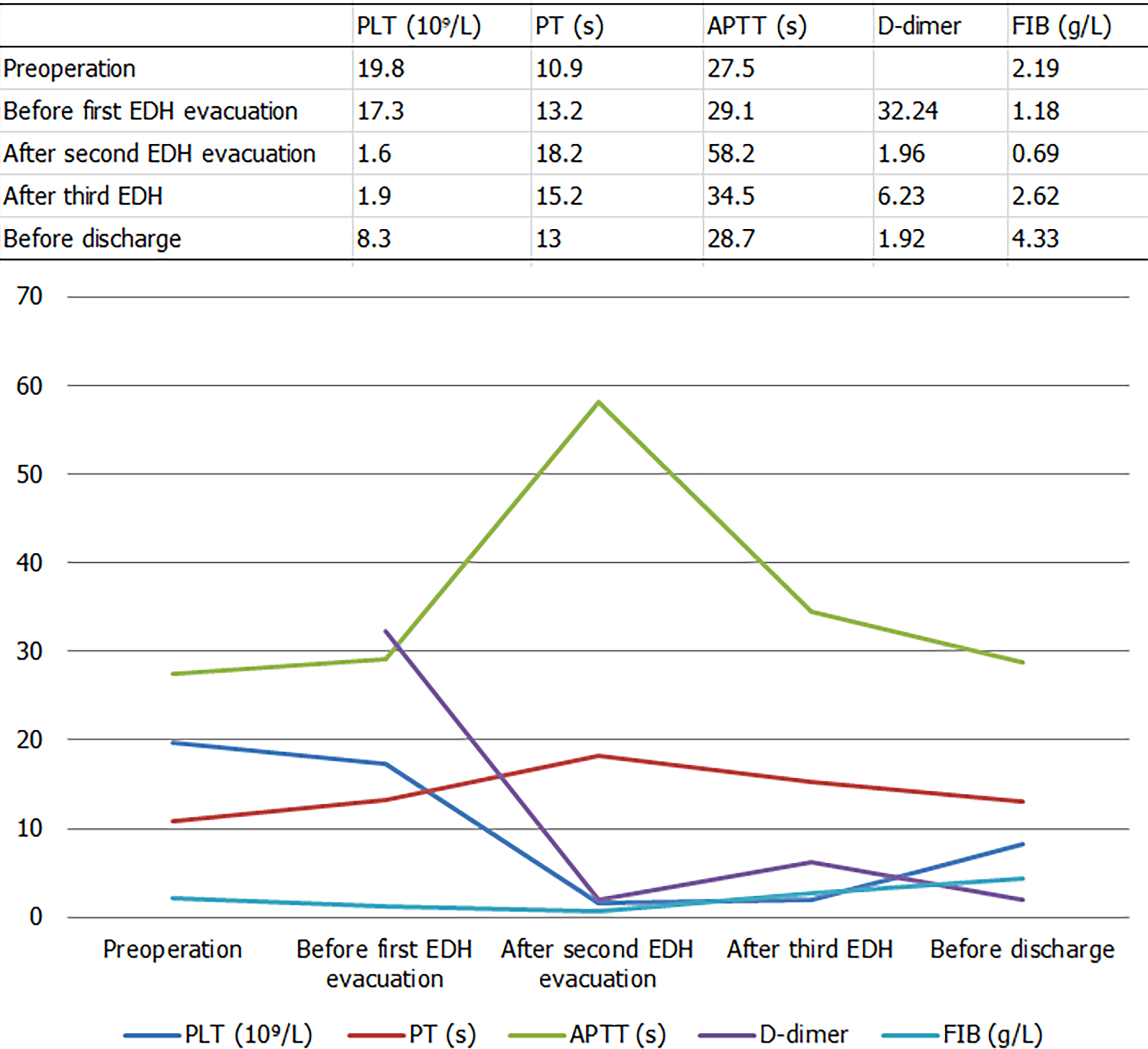
The blood test results were within normal limits before surgery. The laboratory examination results in the whole treatment process are shown in Figure 1 and Table 1.
| Item | PLT (109/L) | PT (s) | APTT (s) | D-dimer (mg/L) | Fibrinogen (g/L) |
| Normal value | 100-300 | 9.6-12.8 | 24.8-33.8 | < 0.55 | 2.0-4.0 |
| Preoperation | 19.8 | 10.9 | 27.5 | - | 2.19 |
| Before first EDH evacuation (3 h postoperatively) | 17.3 | 13.2 | 29.1 | 32.24 | 1.18 |
| After second EDH evacuation (22 h after operation) | 1.6 | 18.2 | 58.2 | 1.96 | 0.69 |
| After third EDH (41 h postoperatively) | 1.9 | 15.2 | 34.5 | 6.23 | 2.62 |
| Before discharge | 8.3 | 13 | 28.7 | 1.92 | 4.33 |
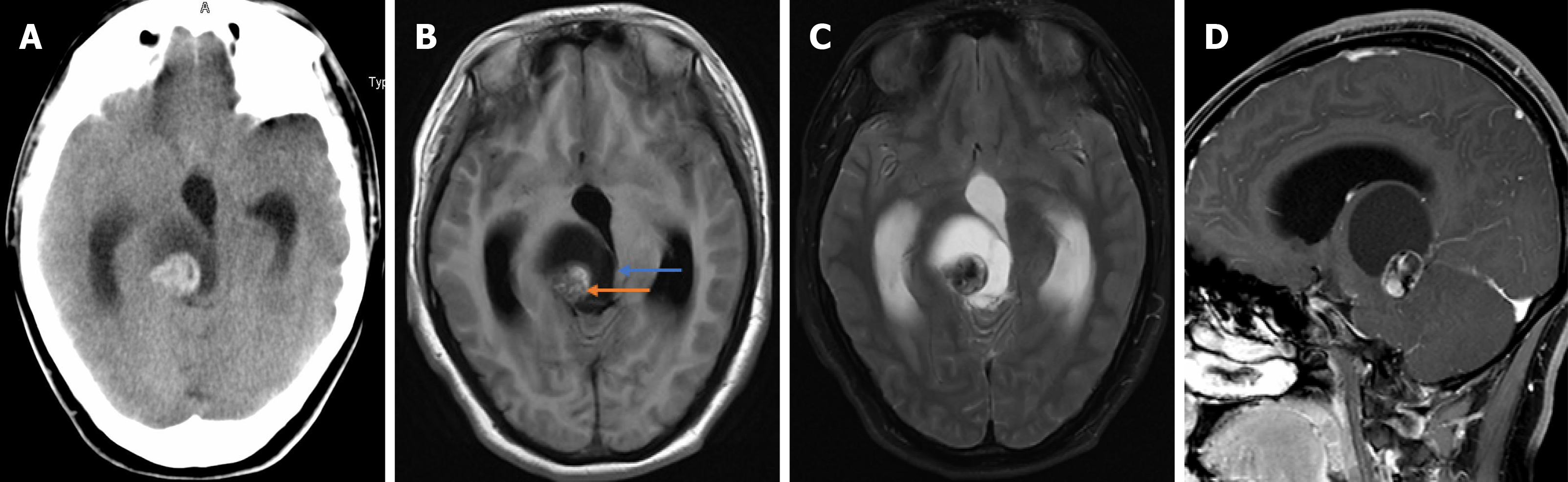
Computerized tomography (CT) revealed a solid cystic tumor in the right thalamus (Figure 2A). Brian magnetic resonance imaging (MRI) showed a solid cystic tumor in the right thalamus and midbrain (Figure 2B-D).
The patient was diagnosed with a right thalamic tumor before surgery.
The final diagnosis was a solid cystic tumor, right posterior cerebral artery aneurysm, vascular malformation in the thalamus, and multiple remote EDHs.
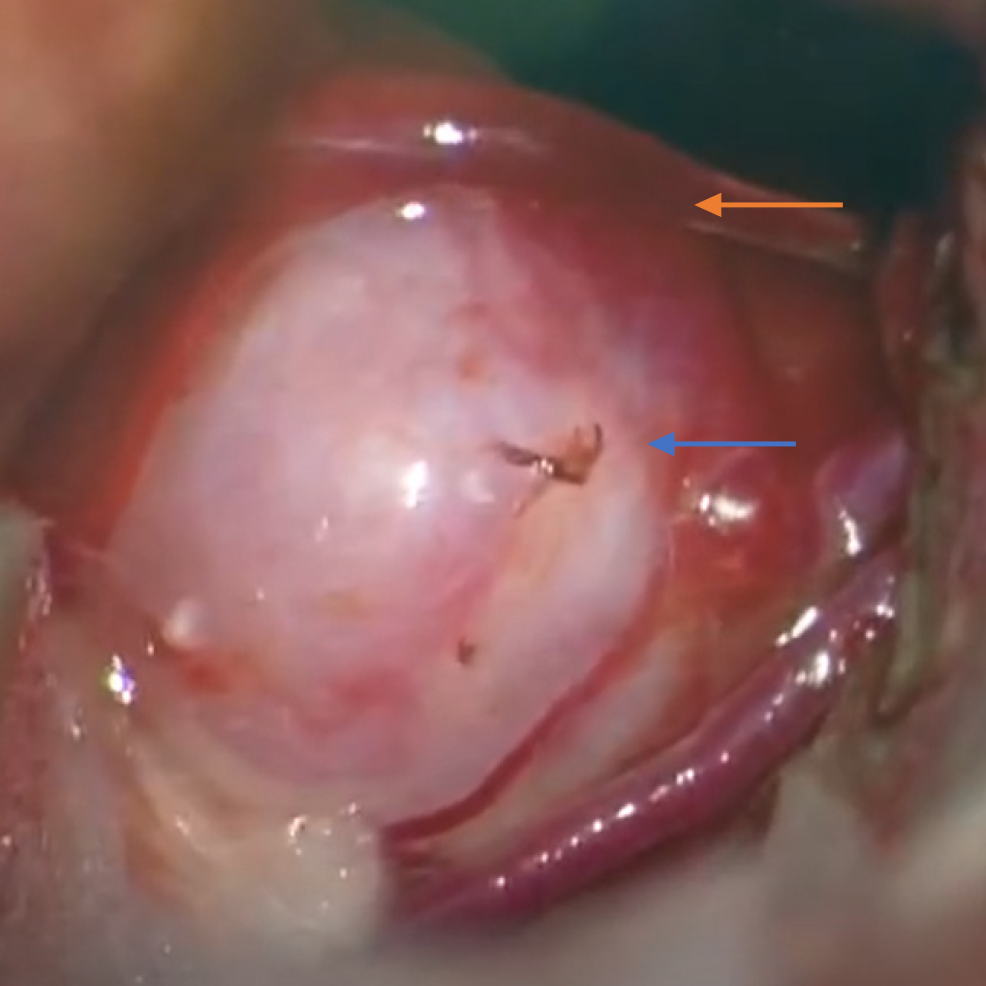
Under the neuro-electrophysiological monitoring, a triangular approach was performed. The cystic mass was dissected, and then yellow fluid was released from the cyst. However, a small artery was observed below the cyst cavity. In addition, a red bulge was observed and considered an aneurysm, which had a drainage vein (Figure 3). Therefore, aneurysm clipping and vascular malformation resection were performed. Neuro-electrophysiological monitoring revealed a decline in the left lower limb. The entire procedure lasted 6.5 h.
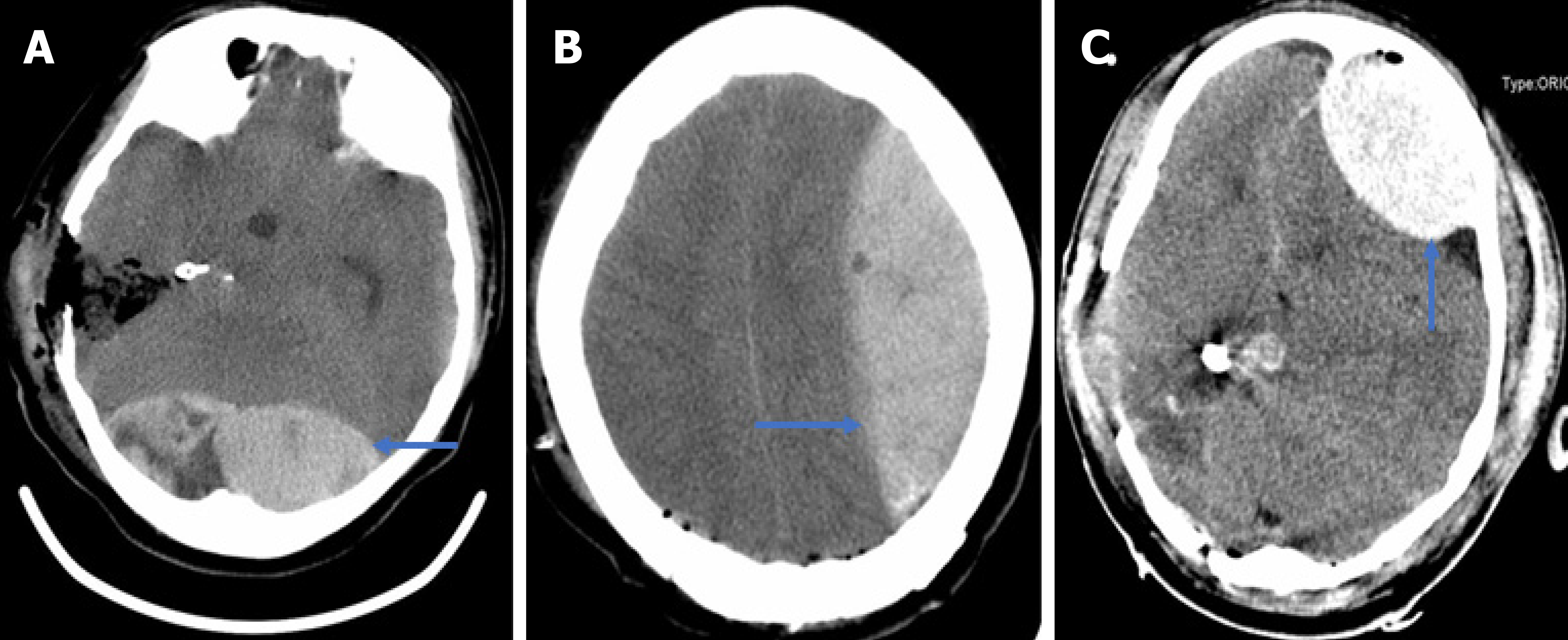
Because the patient did not wake up from anesthesia after 3 h, CT confirmed the first EDH of about 130 mL in the occipital (Figure 4A). Hematoma evacuation was performed. However, the second EDH after 22 h and the third EDH after 41 h developed in the left frontotemporal and the frontal regions (Figure 4B and C). Familial members consented to the second hematoma evacuation but refused the third.
The patient’s family members refused further treatment and asked for discharging. The patient died.
Remote EDH is defined as EDH at a site away from the primary surgical site. Although EDH accounts for 20%[1] among remote site bleeding[3,4], only 12% required surgical intervention[2]. According to published articles, only three cases of multiple postoperative EDHs were reported. Wolfsberger et al[5] presented a patient with four EDHs in the supratentorial area after surgery for the fourth ventricular choroid plexus papilloma. Lim et al[6] and Gaurav Tyagi et al[7] reported two EDHs in the supratentorial area after posterior fossa surgery. However, our patient had three remote EDHs in different locations, including supratentorial and infratentorial regions.
The drastic fluctuation of ICP is a trigger point of postoperative remote ICH[4,8,9]. The fluctuation may result from tumor resection and/or rapid release of cerebrospinal fluid (CSF) and sac fluid. Patients with ventricular drainage systems have a higher incidence of remote ICH than those without[10]. The fast decline of ICP results in negative pressure in a distant area. This fluctuation causes the rupture of blood vessels. With the increasing hematoma caused by vessel rupture, the dura and skull are separated. The phenomenon aggravates hematoma expansion. The above points are a vicious cycle. In our case, the lesion was in the thalamus and midbrain with a posterior cerebral artery. Angiographic assessment should be necessary but was not performed. Because the acute onset occurred and the lesion compressed the aqueduct, the patient had acute obstructive hydrocephalus. Those are special factors for the first occipital EDH.
The pins of a Mayfield head holder may be a reason[11], which may damage the transverse sinus. However, no evidence of fracture was found at the pin sites. Therefore, the cause was ruled out. Age may be a factor for the first EDH because the not-tight adhesion between the dura and skull is more frequent in young people[12,13]. Our patient was a 21-year-old woman. EDH may also result from jugular vein compression because of the extended neck position and intraoperative rotation[14,15]. The patient was positioned in a supine gesture with the head rotation about 65 degrees during surgery, which could lead to obstruction of cerebral venous return.
Coagulopathy is a possible explanation. Our patient had a normal coagulation function before surgery. For the second EDH, consumptive coagulopathy after tumor resection and first EDH might disturb coagulation. The disturbance presented increasing prothrombin time, activated partial thromboplastin time, and international normalized ratio and decreasing fibrinogen, combining with drastically declining platelets. The volume of the first EDH was 130 mL. After the first EDH hematoma evacuation, changes in ICP between the supratentorial and infratentorial regions led to the second left supratentorial EDH. The third EDH could also be attributed to those hypotheses. Thrombocytopenia may play an important role in the third bleeding. Platelet counts in our patients decreased drastically, although the patient was infused with platelets. Unfortunately, a thromboelastogram test was not performed. Decreased factor XIII activity and factor X deficiency may result in EDH[16-18], but the patient and her family did not have this medical history.
We noticed that no definitive source of ooze could be identified during the two hematoma evacuations. There was no visible bleeding on the edge of the dura mater. In the first EDH, the pupil change was noted in time. CT confirmed the EDH. In the third and second EDH, the assessment of CT scan was also a matter of time. Accordingly, early computed tomography scanning of the brain after surgery should be highlighted. Postoperative pupil changes and not waking up from anesthesia are indications for early CT scanning.
Although multiple remote EDH is an uncommon complication, attention should be paid to it. Understanding the mechanism of the complication, sufficient preparation and evaluation before an operation, and meticulous operation during surgery are the keys to preventing postoperative EDH, especially for acute onset. Intraoperative administration of ICP should be meticulous. It is important to monitor the ICP and nerve function after the operation. When the pupil change and the patient cannot recover from anesthesia in time, early CT scanning of the brain should be a priority.
We appreciate the patient and her family members contributing to this medical study.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Neurosciences
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bakar KA, Chan SM S-Editor: Ma YJ L-Editor: Wang TQ P-Editor: Ma YJ
| 1. | Kalfas IH, Little JR. Postoperative hemorrhage: a survey of 4992 intracranial procedures. Neurosurgery. 1988;23:343-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 174] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 2. | Desai VR, Grossman R, Sparrow H. Incidence of Intracranial Hemorrhage After a Cranial Operation. Cureus. 2016;8:e616. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Fukamachi A, Koizumi H, Nagaseki Y, Nukui H. Postoperative extradural hematomas: computed tomographic survey of 1105 intracranial operations. Neurosurgery. 1986;19:589-593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 65] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Yu J, Yang H, Cui D, Li Y. Retrospective analysis of 14 cases of remote epidural hematoma as a postoperative complication after intracranial tumor resection. World J Surg Oncol. 2016;14:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 5. | Wolfsberger S, Gruber A, Czech T. Multiple supratentorial epidural haematomas after posterior fossa surgery. Neurosurg Rev. 2004;27:128-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Lim JW, Yang SH, Lee JS, Song SH. Multiple remote epidural hematomas following pineal gland tumor resection. J Pediatr Neurosci. 2010;5:79-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Tyagi G, Bhat DI, Devi BI, Shukla D. Multiple Remote Sequential Supratentorial Epidural Hematomas-An Unusual and Rare Complication After Posterior Fossa Surgery. World Neurosurg. 2019;128:83-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Garg K, Tandon V, Sinha S, Suri A, Mahapatra AK, Sharma BS. Remote site intracranial hemorrhage: our experience and review of literature. Neurol India. 2014;62:296-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Chung HJ, Park JS, Park JH, Jeun SS. Remote Postoperative Epidural Hematoma after Brain Tumor Surgery. Brain Tumor Res Treat. 2015;3:132-137. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Xu T, Zhang S, Zhang X, Guo L. Remote Intracranial Hemorrhage Secondary to Brain Tumor Surgery. J Craniofac Surg. 2020;31:e53-e57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Naik V, Goyal N, Agrawal D. Pin site bilateral epidural hematoma - a rare complication of using Mayfield clamp in neurosurgery. Neurol India. 2011;59:649-651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Eom KS, Kim TY, Park JT. Contralateral acute interdural haematoma occurring after burr hole drainage of chronic subdural haematoma. Br J Neurosurg. 2009;23:213-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Cui Z, Zhong C, Zhang M, Wu Z, Xu S, Zheng Y, Luo Q, Jiang J. Remote epidural haematoma and severe basal ganglia oedema complicating the removal of a central neurocytoma in the lateral ventricle: a case report and lessons learned. Clin Neurol Neurosurg. 2013;115:365-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Maruyama T, Ishii K, Isono M, Abe T, Fujiki M, Kobayashi H. Remote cerebellar hemorrhage following supratentorial craniotomy--case report. Neurol Med Chir (Tokyo). 2004;44:294-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Honegger J, Zentner J, Spreer J, Carmona H, Schulze-Bonhage A. Cerebellar hemorrhage arising postoperatively as a complication of supratentorial surgery: a retrospective study. J Neurosurg. 2002;96:248-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 71] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 16. | Vrettou CS, Stavrinou LC, Halikias S, Kyriakopoulou M, Kollias S, Stranjalis G, Koutsoukou A. Factor XIII deficiency as a potential cause of supratentorial haemorrhage after posterior fossa surgery. Acta Neurochir (Wien). 2010;152:529-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Gerlach R, Tölle F, Raabe A, Zimmermann M, Siegemund A, Seifert V. Increased risk for postoperative hemorrhage after intracranial surgery in patients with decreased factor XIII activity: implications of a prospective study. Stroke. 2002;33:1618-1623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 139] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 18. | Fujimoto Y, Aguiar PH, Carneiro JD, Martins RS, Ciquini O Jr, de Andrade AF, Manreza LA. Spontaneous epidural hematoma following a shunt in an infant with congenital factor X deficiency. Case report and literature review. Neurosurg Rev. 1999;22:226-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |